Abstract
Background
Transvaginal video-assisted cholecystectomy (TVC) has so far not been prospectively evaluated using an internationally recognized health-related quality of life (HRQoL) assessment. We report the results of a prospectively studied cohort of patients with clinical and quality of life data.
Methods
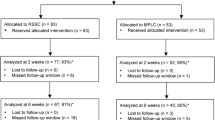
Prospectively controlled study of 128 patients undergoing TVC and 147 patients with conventional laparoscopic cholecystectomy (CLC). Data reported include patient demography, body mass index, anesthetic risk score (ASA), laboratory data, surgical times, length of hospital stay, pain score, analgesic medication used, complications, and quality of life scores using the combined method of SF-36 and GIQoL.
Results
Ninety-five TVC and 96 CLC patients fully completed pre- and postoperative HRQoL questionnaires. Patients with incomplete or missing questionnaires were excluded as well as patients with signs of acute cholecystitis. Differences included cardiovascular comorbidity and previous surgical procedures, but there was no difference in age (p = 0.4), body mass index (p = 0.4), ASA grade (p = 0.4), or preoperative quality of life. No difference was seen in laboratory data, surgical times, or length of hospital stay. Pain score and analgesic medication showed a clear trend and significant differences in favor of TVC. There was no difference in complications. Quality of life and postoperative sexual function did not show any differences between the two groups.
Conclusions
This is the first study to report HRQoL outcomes after TVC using a recognized combined HRQoL assessment method. Although differences do exist in patient comorbidity and previous surgical experience, both groups were comparable. Less postoperative pain and no difference in HRQoL in TVC patients underlines this new procedure as a feasible standard approach in female patients. This study also is the first to differentiate between acute cholecystitis and symptomatic cholecystolithiasis in patients undergoing TVC.

Similar content being viewed by others
References
Federlein M, Borchert D, Muller V, Atas Y, Fritze F, Burghardt J, Elling D, Gellert K (2010) Transvaginal video-assisted cholecystectomy in clinical practice. Surg Endosc 24:2444–2452
Linke GR, Tarantino I, Hoetzel R, Warschkow R, Lange J, Lachat R, Zerz A (2010) Transvaginal rigid-hybrid NOTES cholecystectomy: evaluation in routine clinical practice. Endoscopy 42:571–575
Eypasch E, Wood-Dauphinee S, Williams JI, Ure B, Neugebauer E, Troidl H (1993) The gastrointestinal quality of life index. A clinical index for measuring patient status in gastroenterologic surgery. Chirurg 64:264–274
Korolija D, Sauerland S, Wood-Dauphinee S, Abbou CC, Eypasch E, Caballero MG, Lumsden MA, Millat B, Monson JR, Nilsson G, Pointner R, Schwenk W, Shamiyeh A, Szold A, Targarona E, Ure B, Neugebauer E (2004) Evaluation of quality of life after laparoscopic surgery: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc 18:879–897
Keus F, de VJ, Gooszen HG, Van Laarhoven CJ (2008) Laparoscopic versus small-incision cholecystectomy: health status in a blind randomised trial. Surg Endosc 22:1649–1659
Bullinger M (1995) German translation and psychometric testing of the SF-36 Health Survey: preliminary results from the IQOLA Project. International quality of life assessment. Soc Sci Med 41:1359–1366
Lehmann KS, Ritz JP, Wibmer A, Gellert K, Zornig C, Burghardt J, Busing M, Runkel N, Kohlhaw K, Albrecht R, Kirchner TG, Arlt G, Mall JW, Butters M, Bulian DR, Bretschneider J, Holmer C, Buhr HJ (2010) The German registry for natural orifice translumenal endoscopic surgery: report of the first 551 patients. Ann Surg 252:263–270
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de SE, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Powers JR, Mishra G, Young AF (2005) Differences in mail and telephone responses to self-rated health: use of multiple imputation in correcting for response bias. Aust N Z J Public Health 29:149–154
Bitzer EM, Lorenz C, Nickel S, Dorning H, Trojan A (2008) Assessing patient-reported outcomes of cholecystectomy in short-stay surgery. Surg Endosc 22:2712–2719
Quintana JM, Cabriada J, Arostegui I, Lopez dT I, Bilbao A (2003) Quality-of-life outcomes with laparoscopic vs open cholecystectomy. Surg Endosc 17:1129–1134
Mantha S, Thisted R, Foss J, Ellis JE, Roizen MF (1993) A proposal to use confidence intervals for visual analog scale data for pain measurement to determine clinical significance. Anesth Analg 77:1041–1047
Burghardt J, Federlein M, Elling D, Gellert K, Borchert D (2008) Transvaginale Cholezystektomie—Erfahrungen mit einem neuen Zugangsweg. Chirugische Allgemeine Zeitung für Klinik und Praxis 9(1):23–26 Kaden Verlag
Burghardt J, Federlein M, Borchert D, Lippowski A, Elling D, Gellert K (2008) Transvaginale cholezystektomie: die etablierung und nutzung eines neuen zuganges zur Bauchhöhle für die Viszeralchirurgie. Caduceus News 5:19–25 Covidien
Auyang ED, Santos BF, Enter DH, Hungness ES, Soper NJ (2011) Natural orifice translumenal endoscopic surgery (NOTES®): a technical review. Surg Endosc 25:3135–3148
Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, Goresky CA, Meakins JL (1992) Randomised controlled trial of laparoscopic versus mini cholecystectomy. The McGill gallstone treatment Group. Lancet 340:1116–1119
Hackethal A, Sucke J, Oehmke F, Munstedt K, Padberg W, Tinneberg HR (2010) Establishing transvaginal NOTES for gynecological and surgical indications: benefits, limits, and patient experience. Endoscopy 42:875–878
Hensel M, Schernikau U, Schmidt A, Arlt G (2012) Comparison between transvaginal and laparoscopic cholecystectomy: a retrospective case-control study. Zentralbl Chir 137:48–54
Kilian M, Raue W, Menenakos C, Wassersleben B, Hartmann J (2011) Transvaginal-hybrid vs. single-port-access vs. ‘conventional’ laparoscopic cholecystectomy: a prospective observational study. Langenbecks Arch Surg 396:709–715
Zornig C, Siemssen L, Emmermann A, Alm M, von Waldenfels HA, Felixmuller C, Mofid H (2011) NOTES cholecystectomy: matched-pair analysis comparing the transvaginal hybrid and conventional laparoscopic techniques in a series of 216 patients. Surg Endosc 25:1822–1826
Bisgaard T, Kehlet H, Rosenberg J (2001) Pain and convalescence after laparoscopic cholecystectomy. Eur J Surg 167:84–96
Solomon D, Lentz R, Duffy AJ, Bell RL, Roberts KE (2012) Female sexual function after pure transvaginal appendectomy: a cohort study. J Gastrointest Surg 16:183–186
Hildebrand P, Roblick UJ, Keller R, Kleemann M, Mirow L, Bruch HP (2007) What is the value of minimizing access trauma for patients? Chirurg 78:494, 496–494, 500
Shi HY, Lee KT, Lee HH, Uen YH, Chiu CC (2011) Response shift effect on gastrointestinal quality of life index after laparoscopic cholecystectomy. Qual Life Res 20:335–341
Disclosures
All authors submitted the Surgical Endoscopy disclosure form individually. Drs D. Borchert, O. Rückbeil and Prof. K. Gellert have no conflicts of interest of financial ties to disclose. M. Federlein and Dr. F. Fritze give lectures organized by HCx Consulting. These lectures are sponsored by the companies Storz, Erbe, Nycomed and Ethicon. M. Federlein received grants for surgical courses from Ethicon and LifeCell. Dr. F. Fritze received grants for taking part in medical conferences from KCI and Novartis. Dr. J. Burghardt lectures in surgical courses on behalf of Covidien and is co-owner of a patent with Storz.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dietmar Borchert and Matthias Federlein share first authorship. This publication contributes to the thesis work of M. Federlein. Sana Hospital Berlin is a teaching hospital of the medical faculty Charité, Humboldt University Berlin, Germany.
Rights and permissions
About this article
Cite this article
Borchert, D., Federlein, M., Rückbeil, O. et al. Prospective evaluation of transvaginal assisted cholecystectomy. Surg Endosc 26, 3597–3604 (2012). https://doi.org/10.1007/s00464-012-2378-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2378-1