Abstract
Background
Biological scaffolds must support a complex balance of resisting enzymatic degradation while promoting tissue remodeling. Thus, the purpose of this study was to evaluate the effects of in vitro enzymatic exposure on the mechanical properties of biological scaffolds. It was hypothesized that exposure to an enzyme solution would result in decreased tensile strength and that crosslinked scaffolds would resist enzymatic degradation more effectively than noncrosslinked scaffolds.
Methods
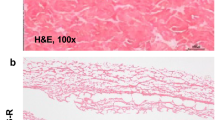
Nine scaffolds were evaluated (four porcine dermis: Permacol™, CollaMend™, Strattice™, XenMatrix™; two human dermis: AlloMax™, FlexHD®; two bovine pericardium: Veritas®, PeriGuard®; and one porcine small intestine submucosa: Surgisis™). Ten specimens (n = 10) were hydrated in saline at 37 °C and subjected to uniaxial testing to establish baseline properties. 50 specimens (n = 50) were incubated in collagenase solution at 37 °C for 2, 6, 12, 24, or 30 h (n = 10 each group) followed by uniaxial tensile testing.
Results
Tensile strength was significantly reduced after 30 h for CollaMend™, AlloMax™, Veritas®, Strattice™, XenMatrix™, Permacol™, and FlexHD® (p < 0.01), while PeriGuard® demonstrated a slight increase in tensile strength (p = 0.0188). Crosslinked bovine pericardium (PeriGuard®) maintained greater tensile strength than noncrosslinked bovine pericardium (Veritas®) throughout all exposure periods (p < 0.0001). Similarly, crosslinked porcine dermis (Permacol™) maintained greater tensile strength than noncrosslinked porcine dermis (Strattice™ and XenMatrix™) throughout all exposure periods (p < 0.0001).
Conclusions
Materials that deteriorate rapidly after in vitro enzymatic exposure may also deteriorate rapidly in vivo, particularly when exposed to a wound environment with elevated levels of matrix metalloproteinases. Permacol™, CollaMend™, Strattice™, FlexHD®, and PeriGuard® survived the longest incubation period (30 h) and withstood mechanical testing. XenMatrix™, AlloMax™, Veritas®, and Surgisis™ degraded more quickly and did not survive the longer exposure periods. Scaffolds that maintain strength characteristics after in vitro collagenase exposure may be advantageous for long-term hernia repair scenarios where elevated enzyme levels are expected.




Similar content being viewed by others
References
Earle DB, Mark LA (2008) Prosthetic material in inguinal hernia repair: how do I choose? Surg Clin N Am 88:179–201
Coda A, Botto-Micca F, Quaglino F, Ramellini G (2000) In vivo tissue reaction to different prosthetic materials in abdominal wall hernia repair. Hernia 4:206–211
Jakus SM, Shapiro A, Hall CD (2008) Biologic and synthetic graft use in pelvic surgery: a review. Obstet Gynecol Surv 63:253–266
Klinge U, Klosterhalfen B, Muller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165:665–673
Badylak SF (2004) Xenogeneic extracellular matrix as a scaffold for tissue reconstruction. Transpl Immunol 12:367–377
Badylak SF (2007) The extracellular matrix as a biologic scaffold material. Biomaterials 28:3587–3593
Cook JL, Fox DB, Kuroki K, Jayo M, De Deyne PG (2008) In vitro and in vivo comparison of five biomaterials used for orthopedic soft tissue augmentation. Am J Vet Res 69:148–156
Charulatha V, Rajaram A (2003) Influence of different crosslinking treatments on the physical properties of collagen membranes. Biomaterials 24:759–767
Milburn ML, Holton LH, Chung TL, Li EN, Bochicchio GV, Goldberg NH, Silverman RP (2008) Acellular dermal matrix compared with synthetic implant material for repair of ventral hernia in the setting of peri-operative Staphylococcus aureus implant contamination: a rabbit model. Surg Infect (Larchmt) 9:433–442
Blatnik J, Jin J, Rosen M (2008) Abdominal hernia repair with bridging acellular dermal matrix—an expensive hernia sac. Am J Surg 196:47–50
Wright JB, Lam K, Buret AG, Olson ME, Burrell RE (2002) Early healing events in a porcine model of contaminated wounds: effects of nanocrystalline silver on matrix metalloproteinases, cell apoptosis, and healing. Wound Repair Regen 10:141–151
Nwomeh BC, Liang HX, Cohen IK, Yager DR (1999) MMP-8 is the predominant collagenase in healing wounds and nonhealing ulcers. J Surg Res 81:189–195
Sternlicht MD, Werb Z (2001) How matrix metalloproteinases regulate cell behavior. Annu Rev Cell Dev Biol 17:463–516
Nwomeh BC, Liang HX, Diegelmann RF, Cohen IK, Yager DR (1998) Dynamics of the matrix metalloproteinases MMP-1 and MMP-8 in acute open human dermal wounds. Wound Repair Regen 6:127–134
Corbel M, Boichot E, Lagente V (2000) Role of gelatinases MMP-2 and MMP-9 in tissue remodeling following acute lung injury. Braz J Med Biol Res 33:749–754
Harper E (1980) Collagenases. Annu Rev Biochem 49:1063–1078
van der Veen V, van der Wal MB, van Leeuwen MC, Ulrich MM, Middelkoop E (2010) Biological background of dermal substitutes. Burns 36:305–321
Deeken CR, Eliason BJ, Pichert MD, Grant SA, Frisella MM, Matthews BD (2012) Differentiation of biologic scaffold materials through physicomechanical, thermal, and enzymatic degradation techniques. Ann Surg 255(3):595–604
Pui CL, Tang ME, Annor AH, Ebersole GC, Frisella MM, Matthews BD, Deeken CR (2012) Effect of repetitive loading on the mechanical properties of biological scaffold materials. J Am Coll Surg (in press)
Gilbert TW, Sellaro TL, Badylak SF (2006) Decellularization of tissues and organs. Biomaterials 27:3675–3683
Damink LHHO, Dijkstra PJ, vanLuyn MJA, vanWachem PB, Nieuwenhuis P, Feijen J (1996) Cross-linking of dermal sheep collagen using a water-soluble carbodiimide. Biomaterials 17:765–773
Billiar K, Murray J, Laude D, Abraham G, Bachrach N (2001) Effects of carbodiimide crosslinking conditions on the physical properties of laminated intestinal submucosa. J Biomed Mater Res 56:101–108
Olde Damink LH, Dijkstra PJ, van Luyn MJ, van Wachem PB, Nieuwenhuis P, Feijen J (1996) In vitro degradation of dermal sheep collagen cross-linked using a water-soluble carbodiimide. Biomaterials 17:679–684
Abraham GA, Murray J, Billiar K, Sullivan SJ (2000) Evaluation of the porcine intestinal collagen layer as a biomaterial. J Biomed Mater Res 51:442–452
Khor E (1997) Methods for the treatment of collagenous tissues for bioprostheses. Biomaterials 18:95–105
HardinYoung J, Carr RM, Downing GJ, Condon KD, Termin PL (1996) Modification of native collagen reduces antigenicity but preserves cell compatibility. Biotechnol Bioeng 49:675–682
Courtman DW, Errett BF, Wilson GJ (2001) The role of crosslinking in modification of the immune response elicited against xenogenic vascular acellular matrices. J Biomed Mater Res 55:576–586
Acknowledgments
This research was supported by research grants from Covidien (Norwalk, CT), the Musculoskeletal Transplant Foundation (Edison, NJ), the Washington University Institute for Minimally Invasive Surgery (St. Louis, MO), and an NIH/NHLBI Training Grant (5 T35 HL007815-16). Permacol™ scaffolds were donated by Covidien (Norwalk, CT). The authors also acknowledge the contributions of Evan G. Buettmann to this study.
Disclosures
Dr. Deeken is a consultant for Atrium Medical Corporation and C.R. Bard/Davol, Inc., and has received honoraria from Covidien and Musculoskeletal Transplant Foundation, as well as grant support from Atrium Medical Corporation, Covidien, Kensey Nash Corporation, and Musculoskeletal Transplant Foundation. Dr. Matthews is a consultant for Atrium Medical Corporation and Ethicon, Inc. He also receives honoraria and research/equipment support from Atrium Medical Corporation, Ethicon Endo-Surgery, Karl Storz Endoscopy, Stryker Endoscopy, and W.L. Gore & Associates, Inc. Margaret M. Frisella is a consultant for Atrium Medical Corporation and receives honoraria from W.L. Gore & Associates. Afua H. Annor, Michael E. Tang, Chi Lun Pui, and Gregory C. Ebersole have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Annor, A.H., Tang, M.E., Pui, C.L. et al. Effect of enzymatic degradation on the mechanical properties of biological scaffold materials. Surg Endosc 26, 2767–2778 (2012). https://doi.org/10.1007/s00464-012-2277-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2277-5