Abstract
Background
The aim of this study was to compare the effects of LigaSure™ versus conventional bipolar techniques on operating time and blood loss during laparoscopic salpingo-oophorectomy in a randomized controlled trial.
Methods
In three teaching hospitals, 100 women undergoing a laparoscopic salpingo-oophorectomy were randomized for LigaSure or conventional bipolar instruments. Primary outcome was operating time (from initial skin incision to removal of the specimen). Secondary outcome measures were total operating time (from initial skin incision to skin closure), time to dissect the ovarian and infundibulopelvic ligaments, intraoperative blood loss, and subjective judgment of the instrument used.
Results
There were no differences in operating time and total operating time using LigaSure versus conventional bipolar instruments: 41.0 vs. 39.2 min (p = 0.78; 95 % CI = −10.9 to 14.5) and 54.6 vs. 58.6 min (p = 0.46; 95 % CI = −14.8 to 6.8), respectively. The mean blood loss using LigaSure versus conventional bipolar instruments was 38 vs. 33 mL (p = 0.73; 95 % CI = −22.7 to 32.2). Various subjective efficacy and instrument handling parameters of the two instruments varied among participating centers.
Conclusion
There were no significant differences in operating time and blood loss with the use of LigaSure compared to conventional bipolar instruments during laparoscopic salpingo-oophorectomy, even after correction for potential confounders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since hemorrhage is one of the most frequent complications that occurs during surgery, adequate hemostatic techniques are essential during surgical procedures. Excessive bleeding during laparoscopic surgery increases the risk of complications since it diminishes the view of the operation field. Additional hemostatic actions under these conditions may increase the risk of bowel- and ureter-related complications.
After the introduction of laparoscopic surgery, different hemostatic instruments have been developed. In laparoscopic surgery, conventional mechanical hemostatic techniques, using sutures or clips, have almost completely been replaced by coagulation techniques, using monopolar or bipolar coagulation or ultrasonic instruments. LigaSure™ (Valleylab, Boulder, CO, USA) is an instrument that desiccates vascular tissues using a feedback-programmed amount of bipolar diathermy [1]. This method of vessel sealing relies on the application of a precise amount of bipolar electrocoagulation and pressure to the tissue, leading to the denaturation of the collagen and elastin in vessel walls, resulting in a hemostatic seal [2]. The technique is able to seal vessels of up to 7 mm in diameter and the seal can withstand a maximum of three times the normal systolic pressure [3]. In addition, compared with conventional bipolar instruments, this vessel-sealing mechanism has a reduced thermal spread profile [3], potentially decreasing the risk of injury to adjacent structures.
One of the gynecological procedures in which bipolar coagulation is used very frequently is the laparoscopic salpingo-oophorectomy. The use of a feedback-controlled bipolar cutting device (vessel-sealing device) has been assessed for a range of procedures, including abdominal and vaginal hysterectomy, hemorrhoidectomy, and bowel surgery [4–12]. Several studies reported a decrease in operating time or operative blood loss using vessel-sealing devices in comparison to other hemostatic devices [5–8, 12]. However, evaluation of its efficacy compared to other hemostatic techniques for laparoscopic salpingo-oophorectomy for benign disorders is lacking. The aim of this randomized controlled trial was to compare the effect of using LigaSure (the 5-mm vessel-sealing instrument with pointed tip: LS1500 V) versus the conventional bipolar technique on operating time and blood loss during laparoscopic salpingo-oophorectomy.
Materials and methods
Design and population
A single-blinded multicenter randomized controlled trial was conducted in two teaching hospitals and one university hospital in the Netherlands, after receiving approval from the local ethical committees concerned. All patients over 18 years old who were scheduled for a laparoscopic salpingo-oophorectomy for a benign disorder in one of the participating centers between June 2006 and October 2009 and who did not meet any of the exclusion criteria were asked to participate and were included in the study after giving written informed consent. Patients were excluded if a pregnancy or malignancy was suspected, if one of the ovaries exceeded a diameter of 10 cm, or if additional surgical procedures during the same operation were planned. All patient data, including the registration of complications during a follow-up period of 6 weeks, were recorded in an electronic database for further analysis.
Randomization
Consenting patients were randomized to surgery with LigaSure (intervention group) or a conventional bipolar instrument (control group) from 1 day to several hours before surgery. Randomization was stratified according to the participating center and type of laparoscopic salpingo-oophorectomy: unilateral (USO) or bilateral (BSO). A web-based central computer system generated the study numbers and the randomization outcome. The randomization outcome was communicated to only the surgeon and the theater team, not to the patient.
Surgical procedures
All laparoscopic salpingo-oophorectomies were performed with the patient under endotracheal general anesthesia, and were performed or supervised by an expert laparoscopic gynecologist. All centers performed the procedure following the standard steps for laparoscopic unilateral or bilateral salpingo-oophorectomy: (1) preoperative thrombosis prophylaxis is given; (2) place the patient in the lithotomy position; (3) insufflation with CO2 and placement of the trocars; (4) suction of 5-mL ascites for cytological pathology; (5) dissection and bipolar coagulation/sealing and transection of the ovarian vessels; (6) dissection and bipolar coagulation/sealing and transection of the utero-ovarian ligament; (7) repeat the preceding two steps for the contralateral side (in case of a bilateral procedure); (8) remove the specimen and close the abdominal skin incisions. In the intervention group, LigaSure™ Lap5 (LS1500 V, Valleylab, Boulder, CO, USA) was used for dissection and hemostasis. In the control group, a conventional bipolar instrument with integrated knife was used. This was either a Seitzinger or a Cutting forceps (both formerly produced by ACMI Corp., Southborough, MA, USA), with respectively an Erbe or a Valleylab generator. The bipolar settings ranged between 30 and 40 W.
Outcome measures
The primary end point was operating time, defined as the time from first incision to removal of the specimen, to reduce variation due to variation in time necessary for removal of the specimen. The exact start and end times were registered by theater staff. Secondary end points were total operating time (time from first incision to last closure of the incision), time to transect the ovarian and infundibulopelvic ligaments, intra- and postoperative complications, length of hospital stay, and intraoperative blood loss. To calculate the amount of blood lost during surgery, we subtracted the total volume of irrigated fluid used from amount measured in the irrigation bottle. For this calculation we weighed the residual fluid in the bags used for irrigation and the total volume in the suction containers at the end of the procedure. To ensure removal of all intra-abdominal fluid, we positioned the patient with the feet down before suction (reverse Trendelenburg position). Differences in hematocrit and hemoglobin levels on the first postoperative day and baseline values before surgery were calculated. Other secondary end points were the surgeon’s subjective evaluation of efficacy and handling characteristics of the instruments used. After each procedure, surgeons were asked to grade the instrument used with respect to dissection, cutting, level of carbonization, and maneuverability, and give their subjective opinion of the sealing, grasping and coagulation abilities of the instrument. Numeric rating scales were used for grading, with 1 being very poor and 5 very good.
The mean time to transect the ovarian and infundibulopelvic ligaments was calculated for the entire group, including both BSO and USO procedures. However, the fastest time to transect the ovarian and infundibulopelvic ligaments was calculated only when both ovaries were removed, thus USO procedures were excluded for this analysis.
Statistical analyses
For the comparison of patient characteristics, analyses of variance were used for normally distributed variables. In all other cases the Mann–Whitney U test was used. χ2 tests were used to compare dichotomous and ordinal variables, and in case the five expected numbers in some cells were lower than five, Fisher’s exact test was used. Multivariable linear regression analyses were used to study the relationship between the intervention group and the outcomes operating time and blood loss and to identify and correct for potential confounders. The confounding variables, indication for surgery, center, age of the patient, and first surgeon, affecting the relationship between instrument used and operating time or blood loss were included in the linear regression models. Based on the residual plots, we decided to natural log transform the outcomes operating time and blood loss before the statistical analyses were performed. As a result of this approach, the regression coefficient had to be back-transformed using the exponential function in order to allow correct interpretation. All analyses were performed according to the intention-to-treat principle using the SPSS ver. 16.0 statistical software package (SPSS, Inc., Chicago, IL, USA). Two-sided p values below 0.05 were considered statistically significant. The results are presented for the total group and by subgroups of laparoscopic salpingo-oophorectomy, i.e., USO and BSO.
Power calculation
The sample size calculation was based on the operating time (defined as the time from first incision to removal of the specimen). We considered a difference of 15 min in operating time to be clinically relevant. We assumed a standard deviation of 25 min, as earlier reported standard deviations varied between 17 and 35 min [13, 14]. Using Student’s t-test, two-sided, and considering a dropout rate of 10 %, 97 patients should be randomized to achieve a power of 80 % at a 5 % significance level.
Results
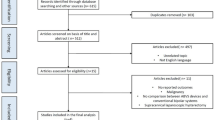
Between June 2006 and October 2009, 100 patients were included; 92 underwent a bilateral laparoscopic salpingo-oophorectomy (BSO) and 8 a unilateral laparoscopic salpingo-oophorectomy (USO) (Fig. 1). Fifty-one patients were randomized to feedback-controlled bipolar cutting device (LigaSure) group and 49 to the conventional bipolar device (28 cases with the Cutting forceps and 21 with the Seitzinger instrument) group. No protocol violation occurred.
Baseline characteristics
Baseline characteristics of the patients are presented in Table 1 and were well balanced between the two study groups. The number of residents performing the procedure as the first surgeon, under close supervision of a gynecologist, was also equally distributed in both arms. The procedures were mainly performed by residents as a first surgeon.
Surgical outcome
Mean operating time (both from initial skin incision to removal of the specimen and from initial skin incision to final skin closure), blood loss, and length of hospital stay did not differ between the groups (Fig. 2; Table 2). Mean time needed to dissect the ovarian and infundibulopelvic ligaments was not different using LigaSure compared to the conventional bipolar instruments (5.44 vs. 6.20 min, p = 0.42). The reductions in hemoglobin and hematocrit levels postoperatively were similar in both study groups. No differences could be observed in the outcomes of BSO and USO. Multivariable analyses were performed to identify any potential confounders. Adjusted analysis did not change the effect between the instruments used on the operating time or the blood loss, i.e., results remained not statistically significantly different between both study groups (Table 3). In the control group, either the Seitzinger or the Cutting forceps could be used. Within this control group, no significant differences could be observed in any of the outcome parameters between these two conventional bipolar instruments.
Complications
During surgery and the study follow-up period of 6 weeks, five complications were recorded in three patients. No statistically significant differences could be observed between the two randomization arms. In one patient fever occurred in combination with a wound hematoma (conventional bipolar instrument was used), in the second patient fever was combined with temporary urine retention (LigaSure was used), and in the third patient postoperative temporary urine retention occurred without fever (conventional bipolar instrument used).
Subjective evaluation of the characteristics and abilities of the used instruments
Statistically significant association in the subjective evaluation was observed only for the level of carbonization, in favor of LigaSure (p = 0.04). However, there was a large variation in the surgeon’s judgment among the participating centers.
Discussion
To our knowledge, our study is the first randomized clinical trial designed to study the effect of two hemostatic instruments used during laparoscopic salpingo-oophorectomy on operating time and blood loss. We could not identify a significant difference in mean operating time or perioperative blood loss between the feedback-controlled bipolar cutting device and the conventional bipolar devices, even after correction for possible confounding parameters. Two different types of conventional bipolar instruments were used in the control group: the Cutting forceps with a Valley lab generator or a Seitzinger with an Erbe generator with a standard setting between 30 and 40 W. In theory there might be a difference in outcome parameters between these two instruments. However, in our study we did not find statistically significant differences between these instruments, therefore we did not perform subgroup analyses.
The mean operating time for the entire procedure, from initial skin incision to removal of the specimen, was 41.0 vs. 39.2 min, which is relatively long. This may be explained by the fact that most procedures were performed by a resident as the first surgeon under supervision of an experienced surgeon. Thus, some of the surgeons may have been in their learning curve, which might cause the variation in operating time. However, our multivariable analyses could not identify experience of the first surgeon as a confounder. In addition, we could not observe any significant effects of the instrument used on the mean or fastest transection time of the ligaments.
There have been only a few studies on laparoscopic salpingo-oophorectomy and the use of different hemostatic techniques, including bipolar cautery, laparoscopic stapler, and extracorporeal knot. Reported mean operating time varied between 60 and 70 min and mean reported blood loss was 50 mL [13, 14]. These studies did not take into account the level of experience of the first surgeon. However, their main outcome with respect to operating time and blood loss were comparable to our findings.
In general, the combination of pressure used in the vessel-sealing technique and bipolar coagulation has two main advantages: it requires less electronic energy thus reducing the thermal spread, and it is more effective due to the formation of a translucent seal of partially denatured protein [2]. In vitro studies comparing feedback-controlled bipolar cutting devices to conventional bipolar electrosurgery, harmonic scalpel, clips, and staples in porcine vessels proved that a feedback-controlled bipolar cutting device was inferior to clip and staple technology and required more time to effect vessel occlusion. However, in regard to other electrosurgical modalities, a feedback-controlled bipolar cutting device was superior to standard bipolar energy [3].
Based on these laboratory results it can be assumed that feedback-controlled bipolar cutting devices, compared to other devices, may have better hemostatic control in vivo and will be more effective in terms of operating time and reduction in blood loss. However, we were not able to confirm these favorable results as reported in previous published studies [5, 8, 15–24]. Most of these laparoscopic studies involved bowel surgery and compared LigaSure with ultrasonic devices [8, 16, 19, 20]. The reduction in blood loss with the LigaSure in those studies may be explained by the less effective hemostasis in large vessels by ultrasonic devices [25–27]. One other study that compared LigaSure with conventional bipolar instruments in a random way in laparoscopic hysterectomy was also not able to detect any significant differences with respect to operating time or blood loss [28].
Because a feedback-controlled bipolar cutting device reduces thermal spread, the risk of injury to adjacent structures may be reduced. However, our study was not designed to identify differences in complications, such as ureter or bowel injuries. Only minor complications occurred in the current study and they were judged by the surgeons as probably not related to the device used.
Given the low incidence of ureter injuries, from 0 to 2.9 %, during salpingo-oophorectomy [29–31], it will be very difficult to perform studies of sufficient power that would show the effect of different hemostatic instruments on these complications. In addition, knowledge of the anatomy and visual perception may have an even larger impact on the risk of ureter injuries than the thermal spread only [32].
There was a clear variation among the three participating centers in the subjective evaluation of the characteristics and abilities of the instruments used. The instrument preferred by the surgeons in each participating center probably reflects bias toward personal preferences. Unfortunately, blinding the surgeon with respect to instrument used is not possible. Despite the variation, the grasping abilities and level of carbonization were consistently evaluated among the different surgeons during this study. The level of carbonization was in favor of the LigaSure and the grasping ability was more in favor of the conventional bipolar instruments. The lower grasping ability of the LigaSure was probably the result of the smooth surface of the LigaSure Lap5 instrument used. There is currently a second-generation 5-mm LigaSure device with better grasping and cutting abilities due to a longer pointed knife with a blunt tip, which is expected to improve dissection and the earlier less positive subjective handling parameters. This was not the instrument tested in this study, however.
A reduction in operating time is required in order to overcome the increased instrument costs in the case of the LigaSure Lap5 compared to the conventional bipolar instruments. Although the mean costs of instruments used vary among hospitals, it is estimated that in the Netherlands the mean cost of a LigaSure Lap5 is approximately €100 higher than conventional bipolar instruments (Seitzinger and Cutting forceps). The OR costs are estimated to be €3.12/min [33] or 4.09 £/min (i.e., €4.8/min) [34]. Thus, the mean required reduction in OR time to overcome the increased costs of approximately €100 varies between 20 and 33 min. Such a reduction is hard to achieve in a procedure which usually takes less than 60 min of OR time. So, in terms of cost-saving, the use of a conventional bipolar instrument should be considered during relatively short procedures such as laparoscopic salpingo-oophorectomy.
In summary, our data indicate that a feedback-controlled bipolar cutting device is as effective in terms of operating time and blood loss as conventional bipolar hemostatic instruments. There is an inconsistent personal preference for either the first-generation LigaSure Lap5 or the conventional bipolar instruments which might be due to personal preference and experiences with one of the instruments rather than technical performance. In terms of cost reduction, taking the instruments’ and OR time costs into account, we cannot claim a preference for LigaSure use in laparoscopic salpingo-oophorectomy.
References
Heniford BT, Matthews BD, Sing RF, Backus C, Pratt B, Greene FL (2001) Initial results with an electrothermal bipolar vessel sealer. Surg Endosc 15(8):799–801
Kennedy JS, Stranahan PL, Taylor KD, Chandler JG (1998) High-burst-strength, feedback-controlled bipolar vessel sealing. Surg Endosc 12(6):876–878
Landman J, Kerbl K, Rehman J, Andreoni C, Humphrey PA, Collyer W et al (2003) Evaluation of a vessel sealing system, bipolar electrosurgery, harmonic scalpel, titanium clips, endoscopic gastrointestinal anastomosis vascular staples and sutures for arterial and venous ligation in a porcine model. J Urol 169(2):697–700
Levy B, Emery L (2003) Randomized trial of suture versus electrosurgical bipolar vessel sealing in vaginal hysterectomy. Obstet Gynecol 102(1):147–151
Franklin EJ, Seetharam S, Lowney J, Horgan PG (2003) Randomized, clinical trial of Ligasure vs conventional diathermy in hemorrhoidectomy. Dis Colon Rectum 46(10):1380–1383
Jayne DG, Botterill I, Ambrose NS, Brennan TG, Guillou PJ, O’Riordain DS (2002) Randomized clinical trial of Ligasure versus conventional diathermy for day-case haemorrhoidectomy. Br J Surg 89(4):428–432
Palazzo FF, Francis DL, Clifton MA (2002) Randomized clinical trial of Ligasure versus open haemorrhoidectomy. Br J Surg 89(2):154–157
Takada M, Ichihara T, Kuroda Y (2005) Comparative study of electrothermal bipolar vessel sealer and ultrasonic coagulating shears in laparoscopic colectomy. Surg Endosc 19(2):226–228
Hagen B, Eriksson N, Sundset M (2005) Randomised controlled trial of LigaSure versus conventional suture ligature for abdominal hysterectomy. BJOG 112(7):968–970
Hefni MA, Bhaumik J, El-Toukhy T, Kho P, Wong I, bdel-Razik T et al (2005) Safety and efficacy of using the LigaSure vessel sealing system for securing the pedicles in vaginal hysterectomy: randomised controlled trial. BJOG 112(3):329–333
Lee WJ, Chen TC, Lai IR, Wang W, Huang MT (2003) Randomized clinical trial of Ligasure versus conventional surgery for extended gastric cancer resection. Br J Surg 90(12):1493–1496
Thorbeck CV, Montes MF (2002) Haemorrhoidectomy: randomised controlled clinical trial of Ligasure compared with Milligan-Morgan operation. Eur J Surg 168(8–9):482–484
Buchweitz O, Matthias S, Muller-Steinhardt M, Malik E (2005) Laparoscopy in patients over 60 years old: a prospective, randomized evaluation of laparoscopic versus open adnexectomy. Am J Obstet Gynecol 193(4):1364–1368
Eltabbakh GH, Piver MS, Hempling RE, Recio FO, Paczos T (1999) Laparoscopic management of women with a family history of ovarian cancer. J Surg Oncol 72(1):9–13
Bessa SS (2008) Ligasure vs. conventional diathermy in excisional hemorrhoidectomy: a prospective, randomized study. Dis Colon Rectum 51(6):940–944
Campagnacci R, De Sanctis A, Baldarelli M, Di Emiddio M, Organetti L, Nisi M et al (2007) Hepatic resections by means of electrothermal bipolar vessel device (EBVS) LigaSure V: early experience. Surg Endosc 21(12):2280–2284
Castellvi J, Sueiras A, Espinosa J, Vallet J, Gil V, Pi F (2009) Ligasure versus diathermy hemorrhoidectomy under spinal anesthesia or pudendal block with ropivacaine: a randomized prospective clinical study with 1-year follow-up. Int J Colorectal Dis 24(9):1011–1018
Fareed M, El-Awady S, Abd-El monaem H, Aly A (2009) Randomized trial comparing LigaSure to closed Ferguson hemorrhoidectomy. Tech Coloproctol 13(3):243–246
Guerrieri M, Sanctis A, Baldarelli M, Nisi M, Rimini M, Coletta M et al (2008) Electrothermal bipolar energy-based device in laparoscopic right colectomy: our experience. Minerva Chir 63(6):455–460
Hubner M, Demartines N, Muller S, Dindo D, Clavien PA, Hahnloser D (2008) Prospective randomized study of monopolar scissors, bipolar vessel sealer and ultrasonic shears in laparoscopic colorectal surgery. Br J Surg 95(9):1098–1104
Milito G, Gargiani M, Cortese F (2002) Randomised trial comparing LigaSure haemorrhoidectomy with the diathermy dissection operation. Tech Coloproctol 6(3):171–175
Muzi MG, Milito G, Nigro C, Cadeddu F, Andreoli F, Amabile D et al (2007) Randomized clinical trial of LigaSure and conventional diathermy haemorrhoidectomy. Br J Surg 94(8):937–942
Sakr MF (2010) LigaSure versus Milligan-Morgan hemorrhoidectomy: a prospective randomized clinical trial. Tech Coloproctol 14(1):13–17
Wang JY, Lu CY, Tsai HL, Chen FM, Huang CJ, Huang YS et al (2006) Randomized controlled trial of LigaSure with submucosal dissection versus Ferguson hemorrhoidectomy for prolapsed hemorrhoids. World J Surg 30(3):462–466
Kennedy JS, Stranahan PL, Taylor KD, Chandler JG (1998) High-burst-strength, feedback-controlled bipolar vessel sealing. Surg Endosc 12(6):876–878
Lamberton GR, Hsi RS, Jin DH, Lindler TU, Jellison FC, Baldwin DD (2008) Prospective comparison of four laparoscopic vessel ligation devices. J Endourol 22(10):2307–2312
Landman J, Kerbl K, Rehman J, Andreoni C, Humphrey PA, Collyer W et al (2003) Evaluation of a vessel sealing system, bipolar electrosurgery, harmonic scalpel, titanium clips, endoscopic gastrointestinal anastomosis vascular staples and sutures for arterial and venous ligation in a porcine model. J Urol 169(2):697–700
Janssen PF, Brolmann HA, Kesteren PJ, Bongers MY, Thurkow AL, Heymans MW et al (2011) Peri-operative outcomes using LigaSure compared to conventional bipolar instruments in laparoscopic hysterectomy: a randomised controlled trial. BJOG 118(13):1568–1575
Saidi MH, Sadler RK, Vancaillie TG, Akright BD, Farhart SA, White AJ (1996) Diagnosis and management of serious urinary complications after major operative laparoscopy. Obstet Gynecol 87(2):272–276
Tamussino KF, Lang PF, Breinl E (1998) Ureteral complications with operative gynecologic laparoscopy. Am J Obstet Gynecol 178(5):967–970
Wu MP, Lin YS, Chou CY (2001) Major complications of operative gynecologic laparoscopy in southern Taiwan. J Am Assoc Gynecol Laparosc 8(1):61–67
Janssen PF, Brölmann HA, Huirne JA (2011) Recommendations to prevent urinary tract injuries during laparoscopic hysterectomy: a systematic Delphi procedure among experts. J Minim Invasive Gynecol 18(3):314–321
Bijen CBM, Vermeulen KM, Mourits MJE, de Bock GH (2009) Costs and effects of abdominal versus laparoscopic hysterectomy: systematic review of controlled trials. PLoS ONE 4(10):e7340
Sculpher M, Manca A, Abbott J, Fountain J, Mason S, Garry R (2004) Cost effectiveness analysis of laparoscopic hysterectomy compared with standard hysterectomy: results from a randomised trial. BMJ 328(7432):134
Disclosures
Dr. Janssen, Prof. Brölmann, Dr. van Kesteren, Dr. Bongers, Dr. Thurkow, Dr. Heymans, and Dr. Huirne have no conflicts of interest or financial ties to disclose.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Janssen, P.F., Brölmann, H.A.M., van Kesteren, P.J.M. et al. Perioperative outcomes using LigaSure™ compared to conventional bipolar instruments in laparoscopic salpingo-oophorectomy: a randomized controlled trial. Surg Endosc 26, 2884–2891 (2012). https://doi.org/10.1007/s00464-012-2274-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2274-8