Abstract
Background
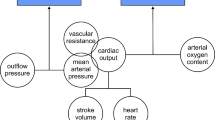
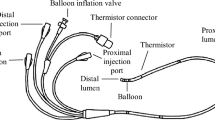
Preventing sudden changes in intraabdominal pressure (IAP) during surgical pneumoperitoneum may reduce adverse events. This study aimed to describe a valve system that stabilizes intraabdominal pressure, minimizing complications of erratic fluctuations in IAP.
Methods
Five male Sprague-Dowley rats were submitted to pneumoperitoneum, with the insufflator set sequentially at 5, 10, and 15 mmHg for each rat. Measures of IAP were taken initially without the valve and then using the same insufflator levels with the valve system regulated to three different pressures (5, 10, and 15 mmHg). The mean of the three highest registered pressures during a 15-min observation was used as the maximal pressure, and the mean of the three lowest registered pressures was used as the minimal pressure for each experimental setting.
Results
Without the valve system, the pressure level set by the insufflator correlated poorly with the actual IAP. When the valve system was used, the IAP pressure was limited by the valve settings regardless of the insufflator settings. Also, the variability of IAP was significantly higher when no valve was used than in all situations that had implementation of the system.
Conclusions
The valve system was very effective in stabilizing IAP, allowing a reproducible and reliable estimate of IAP and greatly reducing the variability resulting from the cycling mechanism of the insufflator. Due to the small dimensions of intracorporeal cavities in the newborn, this mechanism may help to improve safety when neonatal video-assisted surgery is performed.





Similar content being viewed by others
References
Bax NM (2005) Laparoscopic surgery in infants and children. Eur J Pediatr Surg 15:319–324
Fujimoto T, Segawa O, Lane GJ, Esaki S, Miyano T (1999) Laparoscopic surgery in newborn infants. Surg Endosc 13:773–777
Georgeson K (2003) Minimally invasive surgery in neonates. Semin Neonatol 8:243–248
Kuebler JF, Ure BM (2011) Minimally invasive surgery in the neonate. Semin Fetal Neonatal Med 16:151–156
Ure BM, Jesch NK, Gluer S (2002) What’s new in minimally invasive paediatric surgery? Eur J Pediatr Surg 12:361–365
Van Niekerk ML, Visser A, Venter DJ (2005) Laparoscopic antireflux surgery in infants and children. S Afr Med J 95:675–677
Waldschmidt J, Schier F (1991) Laparoscopic surgery in neonates and infants. Eur J Pediatr Surg 1:145–150
Rothenberg SS, Chang JH, Bealer JF (1998) Experience with minimally invasive surgery in infants. Am J Surg 176:654–658
Georgeson KE, Robertson DJ (2004) Minimally invasive surgery in the neonate: review of current evidence. Semin Perinatol 28:212–220
Gueugniaud PY, Abisseror M, Moussa M, Godard J, Foussat C, Petit P, Dodat H (1998) The hemodynamic effects of pneumoperitoneum during laparoscopic surgery in healthy infants: assessment by continuous esophageal aortic blood flow echo-Doppler. Anesth Analg 86:290–293
Guven S, Muci E, Unsal MA, Yulug E, Alver A, Duman MK, Mentese A (2010) The effects of carbon dioxide pneumoperitoneum on ovarian blood flow, oxidative stress markers, and morphology during laparoscopy: a rabbit model. Fertil Steril 93:1327–1332
Holland AJ, Ford WD (1998) The influence of laparoscopic surgery on perioperative heat loss in infants. Pediatr Surg Int 13:350–351
Iwanaka T, Arai M, Ito M, Kawashima H, Imaizumi S (2000) Laparoscopic surgery in neonates and infants weighing less than 5 kg. Pediatr Int 42:608–612
Iwanaka T, Uchida H, Kawashima H, Nishi A, Kudou S, Satake R (2004) Complications of laparoscopic surgery in neonates and small infants. J Pediatr Surg 39:1838–1841
Lindstrom P, Wadstrom J, Ollerstam A, Johnsson C, Persson AE (2003) Effects of increased intra-abdominal pressure and volume expansion on renal function in the rat. Nephrol Dial Transplant 18:2269–2277
Mulholland TL, Kropp BP, Wong C (2005) Laparoscopic renal surgery in infants 10 kg or less. J Endourol 19:397–400
Nishio S, Takeda H, Yokoyama M (1999) Changes in urinary output during laparoscopic adrenalectomy. BJU Int 83:944–947
Truchon R (2004) Anaesthetic considerations for laparoscopic surgery in neonates and infants: a practical review. Best Pract Res Clin Anaesthesiol 18:343–355
Unsal MA, Guven S, Imamoglu M, Aydin S, Alver A (2009) The effect of CO2 insufflation–desufflation attacks on tissue oxidative stress markers during laparoscopy: a rat model. Fertil Steril 92:363–368
Berguer R, Cornelius T, Dalton M (1997) The optimum pneumoperitoneum pressure for laparoscopic surgery in the rat model: a detailed cardiorespiratory study. Surg Endosc 11:915–918
Eleftheriadis E, Kotzampassi K, Papanotas K, Heliadis N, Sarris K (1996) Gut ischemia, oxidative stress, and bacterial translocation in elevated abdominal pressure in rats. World J Surg 20:11–16
Meier C, Contaldo C, Schramm R, Holstein JH, Hamacher J, Amon M, Wanner G, Trentz O, Menger MD (2007) A new model for the study of the abdominal compartment syndrome in rats. J Surg Res 139:209–216
Ure BM, Suempelmann R, Metzelder MM, Kuebler J (2007) Physiological responses to endoscopic surgery in children. Semin Pediatr Surg 16:217–223
Sumpelmann R, Schuerholz T, Marx G, Jesch NK, Osthaus WA, Ure BM (2006) Hemodynamic changes during acute elevation of intra-abdominal pressure in rabbits. Paediatr Anaesth 16:1262–1267
Bergstrom M, Swain P, Park PO (2007) Measurements of intraperitoneal pressure and the development of a feedback control valve for regulating pressure during flexible transgastric surgery (NOTES). Gastrointest Endosc 66:174–178
Festing MF, Altman DG (2002) Guidelines for the design and statistical analysis of experiments using laboratory animals. ILAR J 43:244–258
Chang DT, Kirsch AJ, Sawczuk IS (1994) Oliguria during laparoscopic surgery. J Endourol 8:349–352
Acknowledgments
The first author Brayner Dulfes Luis Marques Iorio is the recipient of a Brazilian governmental funding agency grant FAPESP 2010/01085-1.
Disclosures
Brayner Iorio, Rogerio F. de Barros, Márcio L. Miranda, António Gonçalves de Oliveira-Filho, and Joaquim M. Bustorff-Silva have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iorio, B., de Barros, R.F., Miranda, M.L. et al. Evaluation of a simple valve mechanism used to stabilize intraabdominal pressure during surgically induced pneumoperitoneum in small animals. Surg Endosc 26, 528–532 (2012). https://doi.org/10.1007/s00464-011-1913-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1913-9