Abstract
Background
The ability of the Seprafilm adhesion barrier to prevent adhesion formation after abdominal and pelvic operations has been proved. With laparoscopy, a major technical roadblock with these sheets is their delivery into the peritoneal cavity. This study aimed to evaluate the incidence of postoperative complications and death after laparoscopic placement of Seprafilm slurry in patients who underwent laparoscopic colectomy.
Methods
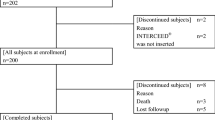
A total of 100 laparoscopic colectomies performed by a single surgeon were analyzed. For 50 patients, Seprafilm was delivered into the peritoneal cavity as a slurry. Group characteristics were evaluated in terms of age, sex, body mass index (BMI), and American Society of Anesthesiology (ASA) score. Complications within the first 30 days after surgery were reviewed. The relative risks with 95% confidence intervals were calculated to determine whether differences in the complication rates between the groups were statistically significant.
Results
Both groups were statistically similar in terms of age, sex, BMI, and ASA score. The differences between the control and experimental groups were examined for abdominal or pelvic abscess (4 vs. 2%), anastomotic leak (4% in both groups), subcutaneous abscess (2% in both groups), wound infection (8 vs. 0%), reoperative rate (8 vs. 6%), and readmission rate (6 vs. 8%). Although the mortality rate was slightly higher in group 2, all the deaths were unrelated to intraabdominal complications. The relative risks for complications were not statistically significant.
Conclusion
The initial data regarding Seprafilm slurry indicate no significant difference in complication rates between the control and experimental groups. This is the first study to evaluate the safety of Seprafilm slurry for patients undergoing laparoscopic colectomy.
Similar content being viewed by others
References
Menzies D, Ellis H (1990) Intestinal obstruction from adhesions: how big is the problem? Ann R Coll Surg Engl 72:60–63
Shinohara T, Kashiwagi H, Yanagisawa S, Yanaga K (2008) A simple and novel technique for the placement of anti adhesive membrane in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 18:188–191
Ray NF, Denton WG, Thamer M, Henderson SC, Perry S (1998) Abdominoadhesiolysis: inpatient care and expenditures in the United States in 1994. J Am Coll Surg 186:1–9
Lundorff P, Hahlin M, Kallfelt B, Thorburn J, Lindblom B (1991) Adhesion formation after laparoscopic surgery in tubal pregnancy: a randomized trial versus laparotomy. Fertil Steril 55:911–915
Szomstein S, Lo Menzo E, Simpfendorfer C, Zundel N, Rosenthal RJ (2006) Laparoscopic lysis of adhesions. World J Surg 30:535–540
Tittel A, Treutner KH, Titkova S, Öttinger A, Schumpelick V (2001) Comparison of adhesion reformation after laparoscopic and conventional adhesiolysis in an animal model. Langenbecks Arch Surg 386:141–145
Bailey IS, Rhodes M, O’Rourke N, Nathanson L, Fielding G (1998) Laparoscopic management of acute small bowel obstruction. Br J Surg 85:84–87
Onders RP, Mittendorf EA (2003) Utility of laparoscopy in chronic abdominal pain. Surgery 134:549–552
Borzellino G, Tasselli S, Zerman G et al (2004) Laparoscopic approach to postoperative adhesive obstruction. Surg Endosc 18:686–690
Gago L, Saed G, Chauhan S, Elhammady EF, Diamond MP (2003) Seprafilm (modified hyaluronic acid and carboxymethylcellulose) acts as a physical barrier. Fertil Steril 80:612–616
Beck D, Cohen Z, Fleshman J, Kaufman HS, Goor HV, Wolff BG (2003) A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum 46:1310–1319
Becker J, Dayton M, Fazio V, Beck DE, Stryker SJ, Wexner SD, Wolff BG, Roberts PL, Smith LE, Sweeney SA, Moore M (1996) Prevention of postoperative abdominal adhesions by a sodium hyaluronate-based bioresorbable membrane: a prospective, randomized double blind multicenter study. J Am Coll Surg 183:297–306
Chuang Y, Fan C, Cho F, Kan YY, Chang Y, Kang H (2008) A novel technique to apply a Seprafilm (hyaluronate-carboxymethylcellulose) barrier following laparoscopic surgeries. Fertil Steril 90:1959–1963
Ortiz M, Awad ZT (2009) An easy technique for laparoscopic placement of Seprafilm. Surg Laparoscopic Endosc Percutan Tech 19(5):e181–e183
Vrijland W, Tseng L, Eijkman H, Hop W, Jakimowicz J, Leguit P, Stassen L, Swank D, Haverlag R, Bonjer J, Jeekel H (2002) Fewer intraperitoneal adhesions with use of hyaluronic acid–carboxymethylcellulose membrane. Ann Surg 235:193–199
Greenawalt K, Colt M, Corazzini R, Krauth M, Holmdahl L (2010) A membrane slurry reduces postoperative adhesions in rat models of abdominal surgery. J Surg Res 1–6. doi:10.1016/j.jss.2010.02.009
Disclosures
Ziad T. Awad received a grant from Genzyme, Cambridge, MA, USA, after the project was completed. Adit Suresh and Brian G. Celso have no conflicts of interests or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suresh, A., Celso, B.G. & Awad, Z.T. Seprafilm slurry does not increase complication rates after laparoscopic colectomy. Surg Endosc 25, 2661–2665 (2011). https://doi.org/10.1007/s00464-011-1624-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-011-1624-2