Abstract
Background
The value of robotic assistance for intracorporeal suturing is not well defined. We compared robotic suturing with laparoscopic suturing on the FLS model with a large cohort of surgeons.
Methods
Attendees (n = 117) at the SAGES 2006 Learning Center robotic station placed intracorporeal sutures on the FLS box-trainer model using conventional laparoscopic instruments and the da Vinci® robot. Participant performance was recorded using a validated objective scoring system, and a questionnaire regarding demographics, task workload, and suturing modality preference was completed. Construct validity for both tasks was assessed by comparing the performance scores of subjects with various levels of experience. A validated questionnaire was used for workload measurement.
Results
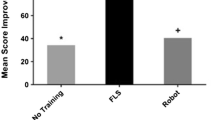
Of the participants, 84% had prior laparoscopic and 10% prior robotic suturing experience. Within the allotted time, 83% of participants completed the suturing task laparoscopically and 72% with the robot. Construct validity was demonstrated for both simulated tasks according to the participants’ advanced laparoscopic experience, laparoscopic suturing experience, and self-reported laparoscopic suturing ability (p < 0.001 for all) and according to prior robotic experience, robotic suturing experience, and self-reported robotic suturing ability (p < 0.001 for all), respectively. While participants achieved higher suturing scores with standard laparoscopy compared with the robot (84 ± 75 vs. 56 ± 63, respectively; p < 0.001), they found the laparoscopic task more physically demanding (NASA score 13 ± 5 vs. 10 ± 5, respectively; p < 0.001) and favored the robot as their method of choice for intracorporeal suturing (62 vs. 38%, respectively; p < 0.01).
Conclusions
Construct validity was demonstrated for robotic suturing on the FLS model. Suturing scores were higher using standard laparoscopy likely as a result of the participants’ greater experience with laparoscopic suturing versus robotic suturing. Robotic assistance decreases the physical demand of intracorporeal suturing compared with conventional laparoscopy and, in this study, was the preferred suturing method by most surgeons. Curricula for robotic suturing training need to be developed.



Similar content being viewed by others
References
Allen JW, Rivas H, Cocchione RN, Ferzli GS (2003) Intracorporeal suturing and knot tying broadens the clinical applicability of laparoscopy. JSLS 7:137–140
Kenngott HG, Muller-Stich BP, Reiter MA, Rassweiler J, Gutt CN (2008) Robotic suturing: technique and benefit in advanced laparoscopic surgery. Minim Invasive Ther Allied Technol 17:160–167
Stefanidis D, Korndorffer JR, Scott DJ (2005) Robotic laparoscopic fundoplication. Curr Treat Options Gastroenterol 8:71–83
Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR (2002) Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology 60:39–45 (discussion 45)
Mohr CJ, Nadzam GS, Alami RS, Sanchez BR, Curet MJ (2006) Totally robotic laparoscopic Roux-en-Y gastric bypass: results from 75 patients. Obes Surg 16:690–696
Sanchez BR, Mohr CJ, Morton JM, Safadi BY, Alami RS, Curet MJ (2005) Comparison of totally robotic laparoscopic Roux-en-Y gastric bypass and traditional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 1:549–554
Mohr CJ, Nadzam GS, Curet MJ (2005) Totally robotic Roux-en-Y gastric bypass. Arch Surg 140:779–786
Gutt CN, Oniu T, Mehrabi A, Kashfi A, Schemmer P, Buchler MW (2004) Robot-assisted abdominal surgery. Br J Surg 91:1390–1397
Rassweiler J, Safi KC, Subotic S, Teber D, Frede T (2005) Robotics and telesurgery—an update on their position in laparoscopic radical prostatectomy. Minim Invasive Ther Allied Technol 14:109–122
Korndorffer JR Jr, Dunne JB, Sierra R, Stefanidis D, Touchard CL, Scott DJ (2005) Simulator training for laparoscopic suturing using performance goals translates to the operating room. J Am Coll Surg 201:23–29
Hart SG, Staveland LE (1988) Development of NASA-TLX (task load index): results of empirical and theoretical research. In: Hancock PA, Meshkati N (eds) Human mental workload. Elsevier, Amsterdam, pp 139–183
Stefanidis D, Wang F, Korndorffer JR Jr, Dunne JB, Scott DJ (2010) Robotic assistance improves intracorporeal suturing performance and safety in the operating room while decreasing operator workload. Surg Endosc 24(2):377–382
Moorthy K, Munz Y, Dosis A, Hernandez J, Martin S, Bello F, Rockall T, Darzi A (2004) Dexterity enhancement with robotic surgery. Surg Endosc 18:790–795
Marecik SJ, Prasad LM, Park JJ, Jan A, Chaudhry V (2008) Evaluation of midlevel and upper-level residents performing their first robotic-sutured intestinal anastomosis. Am J Surg 195:333–337 (discussion 337–338)
Ruurda JP, Broeders IA, Pulles B, Kappelhof FM, van der Werken C (2004) Manual robot assisted endoscopic suturing: time-action analysis in an experimental model. Surg Endosc 18:1249–1252
Chang L, Satava RM, Pellegrini CA, Sinanan MN (2003) Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc 17:1744–1748
Acknowledgments
The authors thank Chris Bell, MD, Lee Ann Lau, MD, Marc Zerey, MD, Makram Gedeon, MD, Andrew Harrell, MD, and George Walker, RN, for their help with the conduct of this study and data acquisition. We also thank Anahita Mostafavi and Amanda Walters, BS, for their help with data entry and analysis.
Disclosures
Dimitrios Stefanidis, William W. Hope, and Daniel J. Scott have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Appendix: Robotic suturing questionnaire
Appendix: Robotic suturing questionnaire


Rights and permissions
About this article
Cite this article
Stefanidis, D., Hope, W.W. & Scott, D.J. Robotic suturing on the FLS model possesses construct validity, is less physically demanding, and is favored by more surgeons compared with laparoscopy. Surg Endosc 25, 2141–2146 (2011). https://doi.org/10.1007/s00464-010-1512-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-1512-1