Abstract
Background
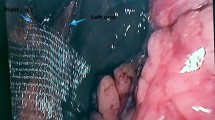
Laparoscopic repair of an intrathoracic stomach has been associated with a high recurrence rate. The use of biologic or synthetic mesh to reinforce the crural repair has been shown to reduce recurrence. This study aimed to assess a simplified technique for reinforcing the crural repair using absorbable Vicryl mesh secured with BioGlue during laparoscopic repair of an intrathoracic stomach.
Methods
The charts of all patients who underwent laparoscopic repair of an intrathoracic stomach from June 2006 to March 2009 using the described technique were retrospectively reviewed. Intrathoracic stomach was defined as more than 50% of the stomach herniated into the chest. Follow-up assessment was routinely performed 1 year or more after surgery and included endoscopy, video esophagram, Bravo 48-h pH monitoring, and a gastroesophageal reflux disease (GERD)–health-related quality-of-life (HRQL) questionnaire.
Results
A total of 35 patients (male:female = 10:25) with a mean age of 70 years (48–89 years) and a mean body mass index (BMI) of 30.4 kg/m2 (20.4–44.8 kg/m2) underwent repair using this technique. The median operating time was 144 min (101–311 min), and the median hospital stay was 2 days (1–21 days). There were three conversions (8.6%) and one intraoperative complication (2.9%). Three patients (8.6%) experienced postoperative complications. No mesh-related complications occurred. Follow-up assessment 1 year or more after surgery was available for 21 of the 25 eligible patients [median follow-up period, 14 months (11–34 months)]. There were two recurrences (9.5%), one of them asymptomatic. The median GERD-HRQL score was 5 (2–28). Nearly all the patients (91.3%) were satisfied with the operation, and 96% would have it again.
Conclusion
Vicryl mesh secured with BioGlue is a simple and easy method for reinforcing the crural closure during laparoscopic repair of an intrathoracic stomach. The recurrence rate at 1 year is low and comparable with that of other series using biologic mesh secured with sutures or tacks.

Similar content being viewed by others
References
Stylopoulos N, Gazelle GS, Rattner DW (2002) Paraesophageal hernias: operation or observation? Ann Surg 236:492–500; discussion 500–501
Ozdemir IA, Burke WA, Ikins PM (1973) Paraesophageal hernia: a life-threatening disease. Ann Thorac Surg 16:547–554
Edye MB, Canin-Endres J, Gattorno F, Salky BA (1998) Durability of laparoscopic repair of paraesophageal hernia. Ann Surg 228:528–535
Huntington TR (1997) Short-term outcome of laparoscopic paraesophageal hernia repair: a case series of 58 consecutive patients. Surg Endosc 11:894–898
Koger KE, Stone JM (1993) Laparoscopic reduction of acute gastric volvulus. Am Surg 59:325–328
Oddsdottir M, Franco AL, Laycock WS, Waring JP, Hunter JG (1995) Laparoscopic repair of paraesophageal hernia: new access, old technique. Surg Endosc 9:164–168
Perdikis G, Hinder RA, Filipi CJ, Walenz T, McBride PJ, Smith SL, Katada N, Klingler PJ (1997) Laparoscopic paraesophageal hernia repair. Arch Surg 132:586–589; discussion 590–581
Pitcher DE, Curet MJ, Martin DT, Vogt DM, Mason J, Zucker KA (1995) Successful laparoscopic repair of paraesophageal hernia. Arch Surg 130:590–596
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF et al (2000) Laparoscopic repair of large type III hiatal hernia: objective follow-up reveals high recurrence rate. J Am Coll Surg 190:553–560; discussion 560–551
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R, Frantzides CT (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20:367–379
Hazebroek EJ, Koak Y, Berry H, Leibman S, Smith GS (2009) Critical evaluation of a novel DualMesh repair for large hiatal hernias. Surg Endosc 23:193–196
Hazebroek EJ, Ng A, Yong DH, Berry H, Leibman S, Smith GS (2008) Evaluation of lightweight titanium-coated polypropylene mesh (TiMesh) for laparoscopic repair of large hiatal hernias. Surg Endosc 22:2428–2432
Granderath FA, Granderath UM, Pointner R (2008) Laparoscopic revisional fundoplication with circular hiatal mesh prosthesis: the long-term results. World J Surg 32:999–1007
Muller-Stich BP, Holzinger F, Kapp T, Klaiber C (2006) Laparoscopic hiatal hernia repair: long-term outcome with the focus on the influence of mesh reinforcement. Surg Endosc 20:380–384
Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, Jobe B, Polissar N, Mitsumori L, Nelson J et al (2006) Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg 244:481–490
Kemppainen E, Kiviluoto T (2000) Fatal cardiac tamponade after emergency tension-free repair of a large paraesophageal hernia. Surg Endosc 14:593
Muller-Stich BP, Linke G, Leemann B, Lange J, Zerz A (2006) Cardiac tamponade as a life-threatening complication in antireflux surgery. Am J Surg 191:139–141
Ayazi S, Lipham JC, Portale G, Peyre CG, Streets CG, Leers JM, Demeester SR, Banki F, Chan LS, Hagen JA et al (2009) Bravo catheter-free pH monitoring: normal values, concordance, optimal diagnostic thresholds, and accuracy. Clin Gastroenterol Hepatol 7:60–67
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Velanovich V, Vallance SR, Gusz JR, Tapia FV, Harkabus MA (1996) Quality-of-life scale for gastroesophageal reflux disease. J Am Coll Surg 183:217–224
Tatum RP, Shalhub S, Oelschlager BK, Pellegrini CA (2008) Complications of PTFE mesh at the diaphragmatic hiatus. J Gastrointest Surg 12:953–957
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG, Demeester TR, Swanstrom LL, Daniel Smith C, Filipi CJ (2008) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23:1219–1226
Diwan TS, Ujiki MB, Dunst CM, Swanstrom LL (2008) Biomesh placement in laparoscopic repair of paraesophageal hernias. Surg Innov 15:184–187
Jacobs M, Gomez E, Plasencia G, Lopez-Penalver C, Lujan H, Velarde D, Jessee T (2007) Use of surgisis mesh in laparoscopic repair of hiatal hernias. Surg Laparosc Endosc Percutan Tech 17:365–368
Johnson JM, Carmody BJ, Jamal MK, DeMaria EJ (2005) Onlay hiatal reinforcement utilizing human acellular dermal matrix: three case series. Surg Innov 12:239–241
Delany HM, Porreca F, Mitsudo S, Solanki B, Rudavsky A (1982) Splenic capping: an experimental study of a new technique for splenorrhaphy using woven polyglycolic acid mesh. Ann Surg 196:187–193
Delany HM, Rudavsky AZ, Lan S (1985) Preliminary clinical experience with the use of absorbable mesh splenorrhaphy. J Trauma 25:909–913
Maurer PK, McDonald JV (1985) Vicryl (polyglactin 910) mesh as a dural substitute. J Neurosurg 63:448–452
Mori N, Takano K, Miyake T, Nishio T, Muto S, Koshizuka K, Nakagomi H, Kubo M, Tada Y (1998) A comparison of prosthetic materials used to repair abdominal wall defects. Pediatr Surg Int 13:487–490
Marmon LM, Vinocur CD, Standiford SB, Wagner CW, Dunn JM, Weintraub WH (1985) Evaluation of absorbable polyglycolic acid mesh as a wound support. J Pediatr Surg 20:737–742
Alamanni F, Fumero A, Parolari A, Trabattoni P, Cannata A, Berti G, Biglioli P (2001) Sutureless double-patch-and-glue technique for repair of subacute left ventricular wall rupture after myocardial infarction. J Thorac Cardiovasc Surg 122:836–837
Herget GW, Kassa M, Riede UN, Lu Y, Brethner L, Hasse J (2001) Experimental use of an albumin-glutaraldehyde tissue adhesive for sealing pulmonary parenchyma and bronchial anastomoses. Eur J Cardiothorac Surg 19:4–9
Hewitt CW, Marra SW, Kann BR, Tran HS, Puc MM, Chrzanowski FA Jr, Tran JL, Lenz SD, Cilley JH Jr, Simonetti VA et al (2001) BioGlue surgical adhesive for thoracic aortic repair during coagulopathy: efficacy and histopathology. Ann Thorac Surg 71:1609–1612
Nadler RB, Loeb S, Rubenstein RA, Vardi IY (2006) Use of BioGlue in laparoscopic partial nephrectomy. Urology 68:416–418
Passage J, Tam R, Windsor M, O’Brien M (2005) Bioglue: a review of the use of this new surgical adhesive in thoracic surgery. ANZ J Surg 75:315–318
Raanani E, Latter DA, Errett LE, Bonneau DB, Leclerc Y, Salasidis GC (2001) Use of “BioGlue” in aortic surgical repair. Ann Thorac Surg 72:638–640
Tansley P, Al-Mulhim F, Lim E, Ladas G, Goldstraw P (2006) A prospective, randomized, controlled trial of the effectiveness of BioGlue in treating alveolar air leaks. J Thorac Cardiovasc Surg 132:105–112
Ellis FH Jr, Crozier RE, Shea JA (1986) Paraesophageal hiatus hernia. Arch Surg 121:416–420
Pearson FG, Cooper JD, Ilves R, Todd TR, Jamieson WR (1983) Massive hiatal hernia with incarceration: a report of 53 cases. Ann Thorac Surg 35:45–51
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zehetner, J., Lipham, J.C., Ayazi, S. et al. A simplified technique for intrathoracic stomach repair: laparoscopic fundoplication with Vicryl mesh and BioGlue crural reinforcement. Surg Endosc 24, 675–679 (2010). https://doi.org/10.1007/s00464-009-0662-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-009-0662-5