Abstract
Background
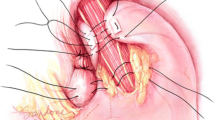
Although the first laparoscopic Nissen fundoplication was performed almost two decades ago, division of the short gastric vessels is still controversially discussed. The aim of this prospectively randomized trial was to evaluate the clinical and functional outcome following laparoscopic Nissen fundoplication with division versus saving of the short gastric vessels during short- and long-term follow-up.
Methods
Forty-one consecutive patients (30 men, 11 women) with gastroesophageal reflux disease were allocated to undergo Nissen fundoplication without division (group 1, n = 19) or with division (group 2, n = 22) of short gastric vessels. All patients were evaluated prior to and at 6 months as well as 5 years following fundoplication. Tests included endoscopy, barium swallow, 24-h pH monitoring, and esophageal manometry. Gastroesophageal reflux disease (GERD) symptoms were evaluated and a gastrointestinal quality-of-life index was calculated.
Results
Preoperative symptoms such as heartburn (84/86%), regurgitation (79/86%), pulmonary symptoms (47/45%), dysphagia (11/32%), chest pain (16/9%), and globus sensation (21/27%) were seen in groups 1 and 2, respectively. In group 1 regurgitation and mild dysphagia were seen in 7 and 26% of patients, respectively, at 5 years. In group 2 the rate of dysphagia decreased from 32 to 17% during short-term follow-up, but increased thereafter to 18%. Reflux esophagitis (preoperative rates: group 1, 74%; group 2, 59%) disappeared in all patients after fundoplication. Mean operative time (group 1, 109 min versus group 2, 125 min; p < 0.05) and mean blood loss (group 1, not measurable; group 2, 25 ml; p < 0.05) showed statistically significant differences. DeMeester score improved in group 1 from 26.6 to 2.2 and in group 2 from 24.7 to 2.5 at 5-year follow-up (p = 0.02). Lower esophageal sphincter (LES) resting pressure returned to normal values (group 1, 23.9 mmHg; group 2, 24.6 mmHg; p < 0.007) with regular relaxation. Quality-of-life index was high in both cohorts, without statistically significant differences between the two groups.
Conclusion
Routine division of the short gastric vessels during Nissen fundoplication in the followed patient group yields neither functional nor clinical advantages in short- or long-term follow-up.

Similar content being viewed by others
References
Donahue PE, Gm Larson, Stewardson RH, Bombeck CT (1977) Floppy Nissen fundoplication. Rev Surg 34:223–224
Bammer T, Hinder RA, Klaus A, Klingler PJ (2001) Five- to eight-year outcome of the first laparoscopic Nissen fundoplications. J Gastrointest Surg 5:42–48
DeMeester TR, Bonavina L, Albertucci M (1986) Nissen fundoplication for gastroesophageal reflux disease: evaluation of primary repair in 100 consecutive patients. Ann Surg 204:9–20
DeMeester TR, Stein HJ (1992) Minimizing the side effects of antireflux surgery. World J Surg 16:335–336
Klaus A, Raiser F, Swain JM, Hinder RA (2000) Manometric components of the lower esophageal double hump. Dig Dis 18:172–177
Laycovk WS, Trus TL, Hunter JG (1996) New technology for the division of short gastric vessels during laparoscopic Nissen fundoplication. Surg Endosc 10:71–73
Swanstrom LL, Pennings JL (1995) Laparoscopic control of short gastric vessels. J Am Coll Surg 181:347–351
Dallemagne B, Weerts JM, Jehaes C, Markiewiecz S (1993) Causes of failures of laparoscopic antireflux operation. Surg Endosc 10:305–310
Luostarinen ME, Isolauri JO (1999) Randomized trial to study the effect of fundic mobilization on long-term results of Nissen fundoplication. Br J Surg 86:614–618
Blomqvist A, Dalenbäck J, Hagedorn C, Lönroth H, Hyltander A, Lundell L (2000) Impact of complete gastric fundus mobilization on outcome after laparoscopic total fundoplication. J Gastrointest Surg 4:493–500
Watson DI, Pike GK, Baigrie RJ, Mathew G, Devitt PG, Britten-Jones R, Jamieson GG (1997) Prospective double-blind randomized trial of laparoscopic Nissen fundoplication with division and without division of short gastric vessels. Ann Surg 226:642–652
Yang H, Watson DI, Lally CJ, Devitt PG, Game PA, Jamieson GG (2008) Randomized trial of division versus nondivision of the short gastric vessels during laparoscopic Nissen fundoplication: 10-year outcomes. Ann Surg 247:38–42
O’Boyle CJ, Watson DI, Jamieson GG, Myers JC, Game PA, Devitt PG (2002) Division of short gastric vessels at laparoscopic Nissen fundoplication: a prospective double-blind randomized trial with 5-year follow-up. Ann Surg 235:165–170
Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, Goldsmith CA (2006) Randomized controlled trial of laparoscopic Nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: one-year follow-up. Surg Innov 13:238–249
Farah JF, Grande JC, Goldenberg A, Martinez JC, Lupinacci RA, Matone J (2007) Randomized trial of total fundoplication and fundal mobilization with or without division of short gastric vessels: a short-term clinical evaluation. Acta Cir Bras 22:422–429
Chrysos E, Tzortzinis A, Tsiaoussis J, Athanasakis H, Vasssilakis J, Xynos E (2001) Prospective randomized trial comparing Nissen to Nissen–Rossetti technique for laparoscopic fundoplication. Am J Surg 182:215–221
Monnier P, Savaary M (1984) Contribution of endoscopic assessment of esophageal reflux disease. Scand J Gastroenterol 19:26
Hinder RA, Filipi CJ, Wetscher G, Neary P, DeMeester TR, Perdikis G (1994) Laparoscopic Nissen fundoplication is an effective treatment for gastroesophageal reflux disease. Ann Surg 220:472–483
Wetscher GJ, Gadenstaetter M, Klingler PJ, Weiss H, Obrist P, Wykypiel H, Klaus A, Profanter C (2001) Efficacy of medical therapy and antireflux surgery to prevent Barrett’s metaplasia in patients with gastroesophageal reflux disease. Ann Surg 234:627–632
DeMeester TR, Wang CI, Wernly JA, Pellegrini CA, Little AG, Klementschitsch P, Bermudez G, Johnson LF, Skinner DB (1980) Technique, indications and clinical use of 24-hour esophageal pH monitoring. J Thorac Cardiovasc Surg 79:656–670
Pudel D, Westenhöfer J (1989) Fragebogen zum Essverhalten (FEV). Handanweisung. Göttingen, Hogrefe
Klaus A, Gadenstatter M, Mühlmann W, Kirchmayr W, Profanter C, Achem SR, Wetscher G (2003) Selection of patients with gastroesophageal reflux disease for antireflux surgery based on esophageal manometry. Dig Dis Sci 48:1719–1722
Salminen PT, Hiekkanen HI, Rantala AP, Ovasaka JT (2007) Comparison of long-term outcome of laparoscopic and conventional Nissen fundoplication: a prospective randomized study with an 11-year follow-up. Ann Surg 46:201–206
Amato G, Limongelli P, Pascariello A, Rossetti G, Del Genio G, Del Genio A, Iovino P (2008) Association between persistent symptoms and long-term qualitiy of life after laparoscopic total fundoplication. Am J Surg 196(4):582-586. doi:10.1016/j.amjsurg.2007.09.038
Wykypiel H, Gadenstaetter M, Klaus A, Klingler P, Wetscher GJ (2003) Nissen or partial posterior fundoplication; which antireflux procedure has a lower rate of side effects? Langenbecks Arch Surg 387:411–416
Donahue PE, Samelson S, Nyhus LM, Bombeck T (1985) The floppy Nissen fundoplication. Effective long term control of pathological reflux. Arch Surg 12:633–668
Rosetti M, Hell K (1977) Fundoplication for the treatment of gastroesophageal reflux in hiatal hernia. World J Surg 1:439–444
Wyman JB, Dent J, Heddle R, Dodds WJ, Toouli J, Downton J (1990) Control of belching by the lower oesophageal sphincter. Gut 31:639–646
Huntington TR, Danielson L (2001) Variation in fundic dimensions with respect to short gastric vessel division in laparoscopic fundoplication. Surg Endosc 15:76–79
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kösek, V., Wykypiel, H., Weiss, H. et al. Division of the short gastric vessels during laparoscopic Nissen fundoplication: clinical and functional outcome during long-term follow-up in a prospectively randomized trial. Surg Endosc 23, 2208–2213 (2009). https://doi.org/10.1007/s00464-008-0267-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-008-0267-4