Abstract
Background
Hiatal mesh implantation in the operative treatment of gastroesophageal reflux disease has become an increasing therapy option. Besides clinical results little is known about histological changes in the esophageal wall.
Methods
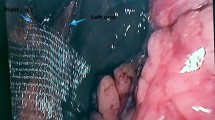
Two different meshes [polypropylene (PP), Prolene®; polypropylene–polyglecaprone 25 composite (PP–PG), Ultrapro®] were placed on the diaphragm circular the esophagus of 20 female rabbits. After three months a swallow with iodine water-soluble contrast medium for functional analysis was performed. After the animals were sacrificed, histopathological evaluation of the foreign-body reaction, the localization of the mesh relating to the esophageal wall was analyzed.
Results
Sixteen rabbits survived the complete observation period of three months. After three months distinctive mesh shrinkage was observed in all animals and meshes had lost up to 50% of their original size before implantation. We found a delayed passage of the fluid into the stomach in all operated animals. There was a significant increased diameter of the outer ring of granulomas in the PP group (76.5 ± 8.0) compared to the PP–PG group (64 ± 8.5; p = 0.002). However, we found a mesh migration into the esophageal wall in six out of seven animals (PP) and five out of nine animals (PP-PG), respectively.
Conclusion
Experimental data suggest that more knowledge is necessary to assess the optimal size, structure, and position of prosthetic materials for mesh hiatoplasty. The indication for mesh implantation in the hiatal region should be carried out very carefully.





Similar content being viewed by others
References
Laws HL, Clements RH, Swillie CM (1997) A randomized, prospective comparison of the Nissen fundoplication versus the Toupet fundoplication for gastroesophageal reflux disease. Ann Surg 225(6):647–653
Zugel N, Jung C, Bruer C, Sommer P, Breitschaft K (2002) A comparison of laparoscopic Toupet versus Nissen fundoplication in gastroesophageal reflux disease. Langenbecks Arch Surg 386(7):494–498
Hashemi M, Peters JH, DeMeester TR, Huprich JE, Quek M, Hagen JA, Crookes PF, Theisen J, DeMeester SR, Sillin LF, et al. (2000) Laparoscopic repair of large type III hiatal hernia: objective followup reveals high recurrence rate. J Am Coll Surg 190(5):553–560
Granderath FA, Schweiger UM, Kamolz T, Pasiut M, Haas CF, Pointner R (2002) Laparoscopic antireflux surgery with routine mesh-hiatoplasty in the treatment of gastroesophageal reflux disease. J Gastrointest Surg 6(3):347–353
Soper NJ, Dunnegan D (1999) Anatomic fundoplication failure after laparoscopic antireflux surgery. Ann Surg 229(5):669–676
Hunter JG, Smith CD, Branum GD, Waring JP, Trus TL, Cornwell M, Galloway K (1999) Laparoscopic fundoplication failures: patterns of failure and response to fundoplication revision. Ann Surg 230(4):595–604
Carlson MA, Frantzides CT (2001) Complications and results of primary minimally invasive antireflux procedures: a review of 10,735 reported cases. J Am Coll Surg 193(4):428–439
Kuster GG, Gilroy S (1993) Laparoscopic technique for repair of paraesophageal hiatal hernias. J Laparoendosc Surg 3(4):331–338
Johnson JM, Carbonell AM, Carmody BJ, Jamal MK, Maher JW, Kellum JM, DeMaria EJ (2006) Laparoscopic mesh hiatoplasty for paraesophageal hernias and fundoplications: a critical analysis of the available literature. Surg Endosc 20(3):362–366
Arendt T, Stuber E, Monig H, Folsch UR, Katsoulis S (2000) Dysphagia due to transmural migration of surgical material into the esophagus nine years after Nissen fundoplication. Gastrointest Endosc 51(5):607–610
Gajbhiye R, Quraishi AH, Mahajan P, Warhadpande M (2005) Dysphagia due to transmural migration of polypropylene mesh into esophagus. Indian J Gastroenterol 24(5):226–227
Desai KM, Diaz S, Dorward IG, Winslow ER, La Regina MC, Halpin V, Soper NJ (2006) Histologic results 1 year after bioprosthetic repair of paraesophageal hernia in a canine model. Surg Endosc 20(11):1693–1697
Treutner KH, Bertram P, Lerch MM, Klimaszewski M, Petrovic-Kallholm S, Sobesky J, Winkeltau G, Schumpelick V (1995) Prevention of postoperative adhesions by single intraperitoneal medication. J Surg Res 59(6):764–771
Muller SA, Treutner KH, Jorn H, Anurov M, Oettinger AP, Schumpelick V (2002) Phospholipids reduce adhesion formation in the rabbit uterine horn model. Fertil Steril 77(6):1269–1273
Zuhlke HV, Lorenz EM, Straub EM, Savvas V (1990) Pathophysiology and classification of adhesions. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir; 1009–16
Leach RE, Burns JW, Dawe EJ, Smith Barbour MD, Diamond MP (1998) Reduction of postsurgical adhesion formation in the rabbit uterine horn model with use of hyaluronate/carboxymethylcellulose gel. Fértil Steril 69(3):415–418
Rosch R, Junge K, Quester R, Klinge U, Klosterhalfen B, Schumpelick V (2003) Vypro II mesh in hernia repair: impact of polyglactin on long-term incorporation in rats. Eur Surg Res 35(5):445–450
Kamolz T, Granderath FA, Bammer T, Pasiut M, Pointner R. Dysphagia (2002) and quality of life after laparoscopic Nissen fundoplication in patients with and without prosthetic reinforcement of the hiatal crura. Surg Endosc 16(4):572–577
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2006) Impact of laparoscopic nissen fundoplication with prosthetic hiatal closure on esophageal body motility: Results of a prospective randomized trial. Arch Surg 141(7):625–632
Granderath FA, Carlson MA, Champion JK, Szold A, Basso N, Pointner R, Frantzides CT (2006) Prosthetic closure of the esophageal hiatus in large hiatal hernia repair and laparoscopic antireflux surgery. Surg Endosc 20(3):367–379
Granderath FA, Kamolz T, Schweiger UM, Pointner R (2004) Prosthetic material for crural closure in laparoscopic antireflux surgery. Surg Endosc 18(1):171–172
Keidar A, Szold A (2003) Laparoscopic repair of paraesophageal hernia with selective use of mesh. Surg Laparosc Endosc Percutan Tech 13(3):149–154
Frantzides CT, Madan AK, Carlson MA, Stavropoulos GP (2002) A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs. simple cruroplasty for large hiatal hernia. Arch Surg 137(6):649–652
Hui TT, Thoman DS, Spyrou M, Phillips EH (2001) Mesh crural repair of large paraesophageal hiatal hernias. Am Surg 67(12):1170–1174
Oelschlager BK, Barreca M, Chang L, Pellegrini CA (2003) The use of small intestine submucosa in the repair of paraesophageal hernias: initial observations of a new technique. Am J Surg 186(1):4–8
Klosterhalfen B, Klinge U, Hermanns B, Schumpelick V (2000) Pathology of traditional surgical nets for hernia repair after long- term implantation in humans. Chirurg 71(1):43–51
Schumpelick V, Klinge U, Welty G, Klosterhalfen B (1999) Meshes within the abdominal wall. Chirurg 70(8):876–887
Conze J, Klinge U, Schumpelick V (2005) Incisional hernia. Chirurg 76(9):897–909
Conze J, Kingsnorth AN, Flament JB, Simmermacher R, Arlt G, Langer C, Schippers E, Hartley M, Schumpelick V (2005) Randomized clinical trial comparing lightweight composite mesh with polyester or polypropylene mesh for incisional hernia repair. Br J Surg 92(12):1488–1493
Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V (2002) Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res 63(6):765–771
Klinge U, Klosterhalfen B, Ottinger AP, Junge K, Schumpelick V (2002) PVDF as a new polymer for the construction of surgical meshes. Biomaterials 23(16):3487–3493
Conze J, Junge K, Klinge U, Weiss C, Polivoda M, Oettinger AP, Schumpelick V (2005) Intraabdominal adhesion formation of polypropylene mesh. Influence of coverage of omentum and polyglactin. Surg Endosc 19(6):798–803
Conze J, Rosch R, Klinge U, Weiss C, Anurov M, Titkowa S, Oettinger A, Schumpelick V (2004) Polypropylene in the intra-abdominal position: influence of pore size and surface area. Hernia 8(4):365–372
Junge K, Rosch R, Krones CJ, Klinge U, Mertens PR, Lynen P, Schumpelick V, Klosterhalfen B (2005) Influence of polyglecaprone 25 (Monocryl) supplementation on the biocompatibility of a polypropylene mesh for hernia repair. Hernia 9(3):212–217
Hergueta-Delgado P, Marin-Moreno M, Morales-Conde S, Reina-Serrano S, Jurado-Castillo C, Pellicer-Bautista F, Herrerias-Gutierrez JM (2006) Transmural migration of a prosthetic mesh after surgery of a paraesophageal hiatal hernia. Gastrointest Endosc 64(1):120
Klinge U, Klosterhalfen B, Muller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165(7):665–673
Klinge U, Klosterhalfen B, Muller M, Ottinger AP, Schumpelick V (1998) Shrinking of polypropylene mesh in vivo: an experimental study in dogs. Eur J Surg 164(12):965–969
Klinge U, Klosterhalfen B, Conze J, Limberg W, Obolenski B, Ottinger AP, Schumpelick V (1998) Modified mesh for hernia repair that is adapted to the physiology of the abdominal wall. Eur J Surg 164(12):951–960
Klinge U, Klosterhalfen B, Birkenhauer V, Junge K, Conze J, Schumpelick V (2002) Impact of polymer pore size on the interface scar formation in a rat model. J Surg Res 103(2):208–214
Aly A, Munt J, Jamieson GG, Ludemann R, Devitt PG, Watson DI (2005) Laparoscopic repair of large hiatal hernias. Br J Surg 92(5):648–653
Andujar JJ, Papasavas PK, Birdas T, Robke J, Raftopoulos Y, Gagne DJ, Caushaj PF, Landreneau RJ, Keenan RJ (2004) Laparoscopic repair of large paraesophageal hernia is associated with a low incidence of recurrence and reoperation. Surg Endosc 18(3):444–447
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jansen, M., Otto, J., Lynen Jansen, P. et al. Mesh migration into the esophageal wall after mesh hiatoplasty: comparison of two alloplastic materials. Surg Endosc 21, 2298–2303 (2007). https://doi.org/10.1007/s00464-007-9514-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-007-9514-3