Abstract
Background
Bleeding is a known and CO2 embolization a suggested risk factor for increased morbidity after laparoscopic liver resection. Devices for laparoscopic liver parenchymal transection must be evaluated for safety in this context.
Method
Twelve piglets underwent laparoscopic surgery during CO2 pneumoperitoneum, each animal receiving three 6 cm long transections into the liver parenchyma made with ultrasonic dissector, ultrasonic shears and vessel sealing system, respectively. Endpoints were bleeding, operation time and gas embolization. The transections and embolization events, evaluated with transesophageal echocardiography, were video recorded. Bleeding and embolization were also assessed on video tapes and operating time measured. Arterial blood gases were recorded on line.
Results
The ultrasonic dissector was least advantageous in terms of bleeding and operation time. Gas embolization was more frequent with the vessel sealing system than with the ultrasonic dissector and ultrasonic shears. During two episodes of gas embolization, pCO2 increased and pO2 and pH decreased.
Conclusions
Use of all three devices is feasible. Bleeding and operation time are greatest with the ultrasonic dissector. Gas embolization occurs during transection, though in most instances it is completely harmless. Laparoscopic liver surgery with these techniques used may pose a risk of gas embolization with clinical implications. Monitoring for such events is probably to be recommended.
Similar content being viewed by others
Laparoscopic liver surgery, originally used mainly for diagnostic procedures such as laparoscopically guided liver biopsies [1], has now expanded to include a wide variety of curative procedures. The first laparoscopic liver resection was reported in 1992 [2]. Currently, virtually all liver surgery can be performed laparoscopically, and such procedures are being performed at a growing number of institutions [3]. Laparoscopic techniques now can be used to perform liver resections for malignant tumors [4, 5] and donor hepatectomies [6, 7], among other procedures. Laparoscopic liver resections have the advantage of being minimally invasive, and further expansion of laparoscopic liver procedures is likely [8–10].
Two of the major risks posed by laparoscopic liver resection are bleeding and carbon dioxide (CO2) embolism. Parenchymal transection is a particularly critical moment in this context. To minimize peri- and postoperative morbidity, the transection technique should be safe and quick. This demand is accentuated in malignant liver surgery because of frequent comorbidity among the patients and during transplants from living relatives with laparoscopic donor hepatectomy. Intraoperative bleeding is recognized as negatively influencing morbidity [11] and recurrence of malignant disease [12, 13] after open procedures, and this is likely to occur also after laparoscopic liver resections.
Furthermore, laparoscopic procedures pose the additional risk of CO2 embolization to the pulmonary circulation, known to occur during pneumoperitoneum and dissection in the highly vasculated liver parenchyma [14]. This complication is poorly studied, and there is an ongoing discussion regarding its clinical relevance.
The traditional method of transecting liver parenchyma is digitoclasia, the “finger-fracture technique,” in which the parenchyma is broken up and divided between the fingers and the palpable parenchymal vascular structures are secured and severed. A refinement of this technique is the “clamp-crush technique,” in which a clamp is used to fracture and divide small sections of the parenchyma before securing and severing the supposedly spared vessels. In addition, vascular inflow to the liver is commonly occluded to reduce blood loss when the parenchyma is transected. However, occlusion can cause ischemic injury to the liver and increase the morbidity among the patients.
As improvements of parenchymal transection, new techniques and technology have evolved such as linear stapling cutters, water jet dissectors, ultrasonic dissectors, ultrasonic shears, vessel sealing systems, and others. These are now being applied to laparoscopic liver procedures. To date, however, the selection of a technique is based mostly on the surgeon’s preference rather than on objective data. The three devices in common use for laparoscopic liver transection are the ultrasonic dissector, the ultrasonic shears, and the vessel sealing system. These are considered safe and their use feasible [15–18].
Several animal studies have been performed, but with different end points, techniques, and study designs, making the results are difficult to interpret. The optimal method for transecting liver parenchyma, preferably one that does not necessitate vascular inflow control, has not been established, and a variety of techniques are in use. There still is room for improvement and evaluation.
This study aimed to compare the safety and efficacy of the ultrasonic dissector, the ultrasonic shears, and the vessel sealing system using the end points of bleeding, operation time, and CO2 embolization during a standardized laparoscopic liver transection and CO2 pneumoperitoneum in vivo with the pig liver.
Material and methods
The study protocol was approved by the Local Ethics Committee on Animal Experiments in Uppsala, Sweden.
Animal preparation
For this study, 12 piglets of Swedish country breed (mean weight, 31.2 ± 4.3 kg) were used. The animals were fasted overnight with free access to water before the experiment. Anesthesia was induced with an intramuscular (IM) injection of Zoletil forte veterinary (Tiletamin 50 mg/ml and zolazepam 50 mg/ml) 6 mg/kg, Rompun veterinary (xylazine 20 mg/ml) 2.2 mg/kg, and Atropin (atropine sulfate 0.5 mg/ml) 0.04 mg/kg. A peripheral ear vein was cannulated for further induction and maintenance of anesthesia and for fluid administration. Morphine 20 mg and ketamine 100 mg were given as a bolus IV injection. The anesthesia was maintained with a continuous IV infusion of ketamine 0.20 mg/kg/h, pancuronium bromide 0.24 mg/kg/h, and morphine 0.5 mg/kg/h.
A tracheotomy was performed, whereby the piglets were intubated (7-mm tube) and mechanically ventilated (Servo Ventilator 900C; Siemens Elema, Solna, Sweden) with a 70/30 mixture of N2O/O2 during the preparation. Volume-controlled ventilation was used. Minute ventilation was adjusted to maintain the partial pressure of arterial CO2 (pCO2) within the range 37 to 41 mmHg (5.0–5.6 kPa), and a peak end-expiratory pressure (PEEP) of 5 cm H2O was applied. The ventilation was not further adjusted during the study period. A pulmonary artery catheter (Swan-Ganz, CritiCath Ohmeda, Singapore, Singapore, 7.5 Fr) was inserted into the right external jugular vein for pressure monitoring, and an artery catheter (Boston Dickinson, Franklin, Lakes, NJ, USA, 18 G) was inserted via a branch of the right external carotid artery into the aortic arch for pressure monitoring and blood sampling. A central venous catheter (7 Fr) was inserted into the right external jugular vein, and an artery catheter (Boston Dickinson, 20 G) was inserted via a branch into the left iliac artery for insertions of the Paratrend sensor (Trendcare Monitoring System, TCM 17000; Diametrix Medical Inc., Roseville, Minnesota, USA).
The urinary bladder was incised, and a urinary catheter was inserted and secured. After the operation, the animals were killed with a potassium injection.
Operative technique
The operations were performed with the pigs in a supine position. All the operations were performed by one surgeon (U.J.) experienced in the handling of all three devices. A 10-mm trocar was introduced below the umbilicus, and a pneumoperitoneum of 12 mmHg was obtained with CO2 insufflation. The laparoscope was introduced, and two additional 10-mm trocars were placed under direct visualization on each side of the laparoscopic trocar.
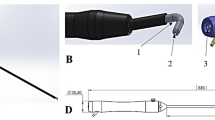
To facilitate the optimal operation site on the liver, a hand-assisted approach was used. The laparoscopic handport device, Omniport (Advanced Surgical Concepts, Bray, Ireland) was placed below the right costal arch. On each pig liver, three 6-cm transections were performed peripherally in the right lateral lobe, the right middle lobe, and the left middle lobe (Fig. 1). The transections were performed by alternating each device between the three lobes.
The parenchymal division was performed with three different devices: ultrasonic dissector (Cavitron Ultrasonic Surgical Aspirator, CUSA Excel, 10 mm; Valley Lab Inc., Boulder, CO, USA), ultrasonic shears (Autosonix, 5 mm; USSU, Norwalk, CT, USA), and vessel sealing system (LigaSure; 10 mm (Valley Lab Inc., Boulder, CO, USA). All three devices were adjusted to the settings recommended for liver operations by the manufacturer. No further resetting was performed during the operations.
The transection technique differed between the devices. During the transection with the ultrasonic shears and the vessel sealing system, one of the end blades was blindly inserted into the liver parenchyma before the blades were closed and energy was applied. In contrast, the ultrasonic dissector was used in a dissecting manner. That is, it was not blindly inserted into the liver parenchyma, and the dissecting area was visible when the liver cells were dissected. Spared vessels and ducts were secured and divided with diathermia EndoGrasp and EndoShears (Auto Suture, Tyco Health-Care, MA, USA). After the surgery, the operation field was observed 5 min for recurrent bleeding.
Measurements
Each operation was videotaped. Embolization in the right outflow tract of the heart was evaluated with transesophageal echocardiography (TEE) during the transections (Sonos 1000 Ultrasound system, Omniplane Probe; Hewlett Packard, Aliso Uiejo, California, USA). Bubbles visible with TEE were considered as gas embolization. The operations and the TEE image were video recorded simultaneously for later evaluation. The operation time was measured.
Experimental protocol
Nitrous oxide administration was discontinued after preparation of the animals, and they were ventilated with 30% O2 in air. After approximately 45 min, baseline values were obtained.
The lateral right, middle right, and middle left lobes were subjected to surgery. The transections were intended to be 6 cm long. All the operations started with the lateral right liver lobe, then moved to the right middle lobe, and finally to the left middle lobe, whereas the order in which the devices were used alternated. Thus, each device was used four times on each of the three different lobes.
The overall bleeding with each transection was estimated from the monitor and recorded in the following arbitrary units: no bleeding (grade 0), slight bleeding (grade 1), and profuse bleeding (grade 2). The most extensive CO2 embolism during each operation was estimated from the monitor and recorded in the following arbitrary units: no gas bubbling (grade 0), slight gas bubbling (grade 1), and extensive gas bubbling (grade 2). The amount of bleeding and the grade and duration of gas embolism were judged by two blinded observers. During the operations, the arterial blood gases were monitored online by a Paratrend sensor (Trendcare Monitoring System, TCM 17000; Diametrix Medical Inc., Roseville, Minneston, USA). After the liver had been harvested, the dissected area was calculated as the length, multiplied by the base, of the dissection.
Statistical analysis
To compare the three devices, Friedman’s analysis of variance (ANOVA) was performed, followed by multiple comparisons among the three different techniques based on ranks. All p values less than 0.05 were considered statistically significant.
Results
All the animals that underwent surgery survived the procedure, and no major complications occurred. Two small piglets were excluded. One experienced circulatory instability during the preparation with the catheters before surgery, making it impossible to obtain baseline values. For one piglet, we were not able to obtain the correct TEE image. The results from this animal were included in the study except for the embolization parameters. For the remaining nine animals, the experiments were completed as planned. The results are presented in Tables 1 and 2.
The use of all three devices was feasible, and no technical failures occurred. No difference was seen between the transected areas when the three devices were compared (p = 0.56).
The operation time was longer with the ultrasonic dissector than with the vessel sealing system (p = 0.001) and the ultrasonic shears (p = 0.0073), but did not differ between the vessel sealing system and the ultrasonic shears (p = 0.18). During the transection, bleeding was more extensive with the ultrasonic dissector than with the ultrasonic shears (p = 0.03), but there was no difference between the ultrasonic dissector and the vessel sealing system (p = 0.07), or between the ultrasonic shears and the vessel sealing system (p = 0.65; Table 1).
There was an overall statistically significant difference in the grades of embolization in the right heart between the devices (p = 0.05), but no difference was proved when the devices was compared in pairs. The total time for emboli relative to the total operation time was longer with the vessel sealing system than with the ultrasonic dissector (p = 0.0047), and longer with the vessel sealing system than with the ultrasonic shears (p = 0.0047). No difference was observed between the ultrasonic dissector and the ultrasonic shears (p = 1.0; Table 2).
Five episodes of grade 2 embolization were recorded: three with the vessel sealing system, one with the ultrasonic dissector, and one with the ultrasonic shears. When two of these events occurred, both of them during vessel sealing system transections, there was an immediate rise in pCO2 and decreases in pO2 and pH, as illustrated in Fig. 2. No recurrent bleeding was observed during the 5-min observation after the operations.
Discussion
Long operation time and excessive bleeding during laparoscopic liver surgery are associated with a higher rate of complications and shorter long-term survival. Carbon dioxide embolization to the cardiopulmonary circulation is considered a risk factor during laparoscopic surgery with CO2 pneumoperitoneum. This risk would theoretically be increased during surgical transection of the highly vasculated liver parenchyma. The risk of CO2 embolism at different CO2 pressures and with different transection devices has not been fully evaluated, and surgeons apparently select different strategies mainly according to personal preference. Moreover, the clinical relevance of emboli, which probably is affected by their size and number, is not clear. Enhanced monitoring of the patient is important for detecting and evaluating the effect of the emboli. We do not consider that the optimal pressure for pneumoperitoneum, optimal transection strategies, and optimal methods for monitoring cardiovascular variables have yet been found.
This study aimed to increase the safety of laparoscopic liver resections. We evaluated three devices for liver parenchymal transection using the end points of operation time, bleeding, and CO2 embolism in a porcine model. We monitored embolism by using TEE, which is considered a sensitive method for detecting CO2 emboli. To assess the clinical relevance of CO2 emboli, we also performed online monitoring of arterial blood gases.
The main finding in our study was that two of five extensive emboli events were associated with alteration in blood gases, which can indicate clinical relevance. Four different strategies have been developed to reduce hemorrhage during transection through the liver parenchyma: vascular occlusion of various types (e.g., the Pringle maneuver, in which vascular inflow is occluded by compression of the hepatoduodenal ligament), reduction of the pressure in the hepatic veins, direct prevention of bleeding when the vessels in the transection plane are severed, and finally, use of hemostatic agents. Occlusion of the vascular inflow clearly entails a risk of ischemic injury to the liver. Thus, the ideal liver transection technique should not necessitate vascular inflow occlusion. Refinement of the transection technique is therefore important.
Carbon dioxide embolization during laparoscopic liver parenchymal transection using a pneumoperitoneum is a matter of discussion. The clinical relevance of these events is still unclear, but they are considered a potential complication [19]. Embolic events have been reported in animal studies [14, 20]. During laparoscopic cholecystectomies in human patients, CO2 embolism has been reported, as detected through TEE monitoring, when the gallbladder is dissected from the liver [21]. In the cited study, slight cardiorespiratory instability was observed. However, arterial blood gases were not measured. In two patient series of laparoscopic liver resections, no clinically relevant gas embolization events were observed [9, 22].
Although no serious clinical events have, to our knowledge, been reported in the literature, surgeons consider embolization to be a risk. One factor is the pressure used to achieve pneumoperitoneum. Higher pressure could theoretically increase the risk. In the literature, three different pressure strategies are recognized. Kaneko et al. [10] reported the use of abdominal wall lifting to avoid embolism. In contrast, Buell et al. [23] reported the use of an 18- to 20-mmHg pneumoperitoneum in their series of laparoscopic liver resections. Most surgeons use the standard pressure of 12 to 14 mmHg. This pressure, considered sufficient for most laparoscopic procedures, was used in this current report. The influence of different pneumoperitoneum pressures on the risk of CO2 embolism was not examined in this study, and must be further evaluated in animal studies.
The implications of embolization for the cardiopulmonary circulation could depend on the size and number of emboli. To evaluate the emboli, we used TEE for detection, but we also used Paratrend to evaluate the impact on arterial blood gases. The Paratrend enables online monitoring of arterial blood gases, as well evaluation of rapid, transient, and persisting changes. A change in blood gases indicates aberration in the gas exchange in the lungs and could imply clinical relevance. Also, an embolic event could be rapid and thus overlooked if monitoring is performed only with TEE.
End-tidal carbon dioxide (EtCO2) also is commonly used to detect emboli. In an earlier experimental study, we found changes in arterial blood gases that lasted 4 h after an experimental embolization in a porcine model. In contrast, EtCO2 was back to preembolic values after less than 30 min [24]. Therefore, we consider monitoring with TEE and EtCO2 appropriate methods for detecting emboli, and we consider continuous monitoring of blood gases a superior means of identifying emboli of clinical relevance.
All three devices used in this study are in general clinical use for various procedures [4, 7, 25] and considered safe and effective [15–18]. We consider these three devices important to evaluate for other reasons. The ultrasonic dissector is commonly used also in centers that perform advanced liver surgery [26]. Use of the ultrasound activated scalpel, including the ultrasonic shears, was reported to entail a high risk of severe gas embolism with cardiac arrhythmias in a pig study [14].
The vessel sealing system is a relatively new and promising technique for parenchymal transection [18]. This new technique should perhaps be described in greater detail. A monopolar technique for heat necrosis in the parenchyma before resection was presented a few years ago [27]. InLine, a device for resection of the parenchyma after coagulative ablation, also has been developed. This device uses radiofrequency energy to achieve coagulative ablation in a plane. In this plane, the resection is performed as the surgeon sees fit, for instance, using diathermy, scalpel, or some other implement. The device is reported to reduce bleeding during transection, as compared with diathermy and suturing [28] or the ultrasonic dissector [29]. The vessel sealing system device used in this study is supposedly a bipolar refinement of this technique, combining heat necrosis of the parenchyma and the crush technique.
The operation time was longest with the ultrasonic dissector device. This can be explained by the fact that dissection of the vessels during the transection is more time consuming, requiring a supplementary diathermia grasp procedure to secure disrupted and bleeding vessels. Considering the small fragile vessels peripherally in the pig liver, the dissection is a challenge, and the result not as good as could be desired. The procedure can be refined by the use of a monopolar diathermia tip on the ultrasonic dissector. A time-consuming factor that might affect the other two devices is adhesion of carbonized liver parenchyma to the ultrasonic shears and vessel sealing system blades. However, we did not experience any such problems during the operations.
When using the vessel sealing system or the ultrasonic shears, the surgeon usually begins the transection by carefully but blindly inserting one end blade of these devices into the liver tissue. The ability of the devices to occlude vessels has been studied elsewhere, and they reportedly occlude vessels safely up to the size of 3.5 mm [30, 31]. Considering the peripheral location in the liver where the operations in this study were performed, no larger vessels could be anticipated. When larger resections are performed closer to the major vasculature in the liver, the risk of embolism is likely to be higher, and this must be evaluated in further animal studies.
When the end blade is inserted, disrupted vessels could cause bleeding unless they are properly occluded. In this study, the bleeding was significantly more extensive only for the ultrasonic dissector, as compared with the ultrasonic shears. Apparently no major bleeding was caused by the blind insertion of the ultrasonic shears or the vessel sealing system. One weakness of our study is that the blood loss was estimated, not measured. Our impression is that no major bleeding occurred that would be difficult to handle during the operations, and we saw no bleeding during the 5-min observation time after the operations. The possibility of a recurrent bleeding after the 5-min observation time must be considered, but was not evaluated in this study. The clinical relevance of the minor difference in bleeding between the devices is unclear.
In this study, a statistically significant difference was observed between the devices when we evaluated the time during which emboli were seen with TEE relative to the total transection time, and the ratio was least favorable for the vessel sealing system. Whether the total time with emboli has implications for the cardiopulmonary circulation is unclear. The size of the emboli could be more important. During two dissections with the vessel sealing system, in which grade 2 emboli were recorded on TEE, there was an influence on the arterial blood gases (Figure 2), with pO2 decreasing to approximately 8.6, pCO2 increasing to 8.6, and pH decreasing to 7.2. This finding implies that there could be differences between the different devices in the negative effects of emboli also during a peripheral transection in the liver.
In this study, embolization was more frequent and serious when the vessel sealing system was used. The reason for this is difficult to interpret and unknown to us. One plausible explanation could be the use of a 10-mm rather than a 5-mm vessel sealing system device.
In conclusion, our study supports the feasibility of using the three reported devices for laparoscopic liver parenchymal transection. The operation time was longer and bleeding was more of a problem with the ultrasonic dissector, but these disadvantages are probably of little clinical relevance. The study strengthens our apprehensions about the risk of gas embolism during laparoscopic liver resection. The number and severity of emboli were greatest when vessel sealing system was used. We recommend further studies of patients undergoing laparoscopic liver surgery with TEE supervision for early detection of emboli and blood gas monitoring online for evaluation of their severity. Postoperative morbidity after laparoscopic liver surgery using different transection strategies also should be evaluated further in clinical studies.
References
Lefor AT, Flowers JL (1994) Laparoscopic wedge biopsy of the liver. J Am Coll Surg 178: 307–308
Gagner MRM, Dubuc J (1992) Laparoscopic partial hepatectomy for liver tumor (abstract). Surg Endosc 6: 99
Rogula T, Gagner M (2004) Current status of the laparoscopic approach to liver resection. J Long Term Eff Med Implants 14: 23–31
Gigot JF, Glineur D, Santiago Azagra J, Goergen M, Ceuterick M, Morino M, Etienne J, Marescaux J, Mutter D, van Krunckelsven L, Descottes B, Valleix D, Lachachi F, Bertrand C, Mansvelt B, Hubens G, Saey JP, Schockmel R (2002) Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg 236: 90–97
O’Rourke N, Fielding G (2004) Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg 8: 213–216
Abouljoud M, Yoshida A, Dagher F, Moonka D, Brown K (2003) Living donor and split-liver transplantation: an overview. Transplant Proc 35: 2772–2774
Cherqui D, Soubrane O, Husson E, Barshasz E, Vignaux O, Ghimouz M, Branchereau S, Chardot C, Gauthier F, Fagniez PL, Houssin D (2002) Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 359: 392–396
Mala T, Edwin B, Gladhaug I, Fosse E, Soreide O, Bergan A, Mathisen O (2002) A comparative study of the short-term outcome following open and laparoscopic liver resection of colorectal metastases. Surg Endosc 16: 1059–1063
Farges O, Jagot P, Kirstetter P, Marty J, Belghiti J (2002) Prospective assessment of the safety and benefit of laparoscopic liver resections. J Hepatobiliary Pancreat Surg 9: 242–248
Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, Maeda T, Shiba T (2005) Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg 189: 190–194
Wei AC, Tung-Ping Poon R, Fan ST, Wong J (2003) Risk factors for perioperative morbidity and mortality after extended hepatectomy for hepatocellular carcinoma. Br J Surg 90: 33–41
Yamamoto J, Kosuge T, Takayama T, Shimada K, Yamasaki S, Ozaki H, Yamaguchi N, Mizuno S, Makuuchi M (1994) Perioperative blood transfusion promotes recurrence of hepatocellular carcinoma after hepatectomy. Surgery 115: 303–309
Stephenson KR, Steinberg SM, Hughes KS, Vetto JT, Sugarbaker PH, Chang AE (1988) Perioperative blood transfusions are associated with decreased time to recurrence and decreased survival after resection of colorectal liver metastases. Ann Surg 208: 679–687
Schmandra TC, Mierdl S, Bauer H, Gutt C, Hanisch E (2002) Transoesophageal echocardiography shows high risk of gas embolism during laparoscopic hepatic resection under carbon dioxide pneumoperitoneum. Br J Surg 89: 870–876
Strasberg SM, Drebin JA, Linehan D (2002) Use of a bipolar vessel-sealing device for parenchymal transection during liver surgery. J Gastrointest Surg 6: 569–574
Taniai N, Onda M, Tajiri T, Akimaru K, Yoshida H, Mamada Y (2002) Hepatic parenchymal resection using an ultrasonic surgical aspirator with electrosurgical coagulation. Hepatogastroenterology 49: 1649–1651
Schmidbauer S, Hallfeldt KK, Sitzmann G, Kantelhardt T, Trupka A (2002) Experience with ultrasound scissors and blades (UltraCision) in open and laparoscopic liver resection. Ann Surg 235: 27–30
Romano F, Franciosi C, Caprotti R, Uggeri F (2005) Hepatic surgery using the Ligasure vessel sealing system. World J Surg 29: 110–112
Takagi S (1998) Hepatic and portal vein blood flow during carbon dioxide pneumoperitoneum for laparoscopic hepatectomy. Surg Endosc 12: 427–431
Schmandra TC, Mierdl S, Hollander D, Hanisch E, Gutt C (2004) Risk of gas embolism in hand-assisted versus total laparoscopic hepatic resection. Surg Technol Int 12: 137–143
Derouin M, Couture P, Boudreault D, Girard D, Gravel D (1996) Detection of gas embolism by transesophageal echocardiography during laparoscopic cholecystectomy. Anesth Analg 82: 119–124
Cherqui D 2003 Laparoscopic liver resection. Br J Surg 90: 644–646
Buell JF, Thomas MJ, Doty TC, Gersin KS, Merchen TD, Gupta M, Rudich SM, Woodle ES (2004) An initial experience and evolution of laparoscopic hepatic resectional surgery. Surgery 136: 804–811
Jersenius U, Fors D, Rubertsson S, Arvidsson D (2006) The effects of experimental venous carbon dioxide embolization on hemodynamic and respiratory variables. Acta Anaesthesiol Scand 50(2): 156–162
Descottes B, Glineur D, Lachachi F, Valleix D, Paineau J, Hamy A, Morino M, Bismuth H, Castaing D, Savier E, Honore P, Detry O, Legrand M, Azagra JS, Goergen M, Ceuterick M, Marescaux J, Mutter D, de Hemptinne B, Troisi R, Weerts J, Dallemagne B, Jehaes C, Gelin M, Donckier V, Aerts R, Topal B, Bertrand C, Mansvelt B, Van Krunckelsven L, Herman D, Kint M, Totte E, Schockmel R, Gigot JF (2003) Laparoscopic liver resection of benign liver tumors. Surg Endosc 17: 23–30
Adam R, Pascal G, Azoulay D, Tanaka K, Castaing D, Bismuth H (2003) Liver resection for colorectal metastases: the third hepatectomy. Ann Surg 238: 871–883, discussion 883–874
Weber JC, Navarra G, Jiao LR, Nicholls JP, Jensen SL, Habib NA (2002) New technique for liver resection using heat coagulative necrosis. Ann Surg 236: 560–563
Haghighi KS, Steinke K, Hazratwala K, Kam PC, Daniel S, Morris DL (2005) Controlled study of in-line radiofrequency ablation (ILRFA) assisted transection of ovine liver. J Surg Res 123: 139–143
Haghighi KS, Wang F, King J, Daniel S, Morris DL (2005) In-line radiofrequency ablation to minimize blood loss in hepatic parenchymal transection. Am J Surg 190: 43–47
Spivak H, Richardson WS, Hunter JG (1998) The use of bipolar cautery, laparosonic coagulating shears, and vascular clips for hemostasis of small and medium-sized vessels. Surg Endosc 12: 183–185
Landman J, Kerbl K, Rehman J, Andreoni C, Humphrey PA, Collyer W, Olweny E, Sundaram C, Clayman RV (2003) Evaluation of a vessel sealing system, bipolar electrosurgery, harmonic scalpel, titanium clips, endoscopic gastrointestinal anastomosis vascular staples and sutures for arterial and venous ligation in a porcine model. J Urol 169: 697–700
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jersenius, U., Fors, D., Rubertsson, S. et al. Laparoscopic parenchymal division of the liver in a porcine model: comparison of the efficacy and safety of three different techniques. Surg Endosc 21, 315–320 (2007). https://doi.org/10.1007/s00464-006-0758-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0758-0