Abstract
Background
Complex procedures for managing congenital abnormalities are reported to be feasible. However, neonatal videosurgery involves very specific physiologic constraints. This study evaluated the safety and complication rate of videosurgery during the first month of life and sought to determine both the risk factors of perioperative complications and the most recent trends in practice.
Methods
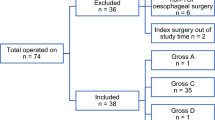
From 1993 to 2005, 218 neonates (mean age, 16 days; weight, 3,386 g) from seven European university hospitals were enrolled in a retrospective study. The surgical indications for laparoscopy (n = 204) and thoracoscopy (n = 14) were congenital abnormalities or exploratory procedures.
Results
Of the 16 surgical incidents that occurred (7.5%), mainly before 2001, 11 were minor (parietal hematoma, eventration). Three neonates had repeat surgery for incomplete treatment of pyloric stenosis. In two cases, the incidents were more threatening (duodenal wound, diaphragmatic artery injury), but without further consequences. No mortality is reported. The 26 anesthetic incidents (12%) that occurred during insufflation included desaturation (<80% despite 100% oxygen ventilation) (n = 8), transient hypotension requiring vascular expansion (n = 7), hypercapnia (>45 mmHg) (n = 5), hypothermia (<34.9°C) (n = 4), and metabolic acidosis (n = 2). The insufflation had to be stopped in 7% of the cases (transiently in 9 cases, definitively in 6 cases). The significant risk factors for an incident (p < 0.05) were young age of the patient, low body temperature, thoracic insufflation, high pressure and flow of insufflation, and length of surgery.
Conclusion
Despite advances in miniaturizing of instruments and growth in surgeons’ experience, the morbidity of neonatal videosurgery is not negligible. A profile of the patient at risk for an insufflation-related incident emerged from this study and may help in the selection of neonates who will benefit most from these techniques in conditions of maximal safety.


Similar content being viewed by others
References
Bax NM, Ure BM, van der Zee DC, van Tuijl I (2001) Laparoscopic duodenoduodenostomy for duodenal atresia. Surg Endosc 15: 217
Rothenberg SS (2002) Laparoscopic duodenoduodenostomy for duodenal obstruction in infants and children. J Pediatr Surg 37: 1088–1089
Rothenberg SS (2002) Thoracoscopic repair of tracheoesophageal fistula in newborns. J Pediatr Surg 37: 869–872
van der Zee DC, Bax NM (1995) Laparoscopic repair of acute volvulus in a neonate with malrotation. Surg Endosc 9: 1123–1124
Bax KM, van Der Zee DC (2002) Feasibility of thoracoscopic repair of esophageal atresia with distal fistula. J Pediatr Surg 37: 192–196
Gertner M, Farmer DL (2004) Laparoscopic cholecystecomy in a 16-day-old infant with chronic cholelithiasis. J Pediatr Surg 39: E17–E19
Gluer S, Scharf A, Ure BM (2002) Thoracoscopic resection of extralobar sequestration in a neonate. J Pediatr Surg 37: 1629–1631
Wurst H, Schulte-Steinberg H, Finsterer U (1993) Pulmonary CO2 elimination in laparoscopic cholecystectomy: a clinical study. Anaesthesist 42: 427–434
Bozkurt P, Kaya G, Yeker Y, Tunali Y, Altintas F (1999) The cardiorespiratory effects of laparoscopic procedures in infants. Anaesthesia 54: 831–834
Coppola L, Avogaro F, Vendramin ML, Belloli GP (1985) Anesthesiologic management of surgery in the 1st month of life: review of the literature and clinical contribution. Pediatr Med Chir 7: 503–511
Romero T, Covell J, Friedman WF (1972) A comparison of pressure–volume relations of the fetal, newborn, and adult heart. Am J Physiol 222: 1285–1290
Fujimoto T, Segawa O, Lane GJ, Esaki S, Miyano T (1999) Laparoscopic surgery in newborn infants. Surg Endosc 13: 773–777
Iwanaka T, Arai M, Ito M, Kawashima H, Imaizumi S (2000) Laparoscopic surgery in neonates and infants weighing less than 5 kg. Pediatr Int 42: 608–612
Truchon R (2004) Anaesthetic considerations for laparoscopic surgery in neonates and infants: a practical review. Best Pract Res Clin Anaesthesiol 18: 343–355
Kalfa N, Allal H, Raux O, Lopez M, Forgues D, Guibal MP, Picaud JC, Galifer RB (2005) Tolerance of laparoscopy and thoracoscopy in neonates. Pediatrics 116: e785–791
Rangel SJ, Henry MC, Brindle M, Moss RL (2003) Small evidence for small incisions: pediatric laparoscopy and the need for more rigorous evaluation of novel surgical therapies. J Pediatr Surg 38: 1429–1433
Esposito C, Ascione G, Garipoli V, De Bernardo G, Esposito G (1997) Complications of pediatric laparoscopic surgery. Surg Endosc 11: 655–657
Esposito C, Lima M, Mattioli G, Mastroianni L, Centonze A, Monguzzi GL, Montinaro L, Riccipetitoni G, Garzi A, Savanelli A, Damiano R, Messina M, Settimi A, Amici G, Jasonni V, Palmer LS (2003) Complications of pediatric urological laparoscopy: mistakes and risks. J Urol 169: 1490–1492
Peters CA (1996) Complications in pediatric urological laparoscopy: results of a survey. J Urol 155: 1070–1073
Bannister CF, Brosius KK, Wulkan M (2003) The effect of insufflation pressure on pulmonary mechanics in infants during laparoscopic surgical procedures. Paediatr Anaesth 13: 785–789
Gueugniaud PY, Abisseror M, Moussa M, Godard J, Foussat C, Petit P, Dodat H (1998) The hemodynamic effects of pneumoperitoneum during laparoscopic surgery in healthy infants: assessment by continuous esophageal aortic blood flow echo-Doppler. Anesth Analg 86: 290–293
Manner T, Aantaa R, Alanen M (1998) Lung compliance during laparoscopic surgery in paediatric patients. Paediatr Anaesth 8: 25–29
McHoney M, Corizia L, Eaton S, Kiely EM, Drake DP, Tan HL, Spitz L, Pierro A (2003) Carbon dioxide elimination during laparoscopy in children is age dependent. J Pediatr Surg 38: 105–110
Hazebroek EJ, Haitsma JJ, Lachmann B, Steyerberg EW, de Bruin RW, Bouvy ND, Bonjer HJ (2002) Impact of carbon dioxide and helium insufflation on cardiorespiratory function during prolonged pneumoperitoneum in an experimental rat model. Surg Endosc 16: 1073–1078
Sefr R, Puszkailer K, Jagos F (2003) Randomized trial of different intraabdominal pressures and acid–base balance alterations during laparoscopic cholecystectomy. Surg Endosc 17: 947–950
Wulkan ML, Vasudevan SA (2001) Is end-tidal CO2 an accurate measure of arterial CO2 during laparoscopic procedures in children and neonates with cyanotic congenital heart disease? J Pediatr Surg 36: 1234–1236
Hazebroek EJ, Schreve MA, Visser P, De Bruin RW, Marquet RL, Bonjer HJ (2002) Impact of temperature and humidity of carbon dioxide pneumoperitoneum on body temperature and peritoneal morphology. J Laparoendosc Adv Surg Tech A 12: 355–364
Moore SS, Green CR, Wang FL, Pandit SK, Hurd WW (1997) The role of irrigation in the development of hypothermia during laparoscopic surgery. Am J Obstet Gynecol 176: 598–602
Ott DE (1991) Laparoscopic hypothermia. J Laparoendosc Surg 1: 127–131
Gray RI, Ott DE, Henderson AC, Cochran SA, Roth EA (1999) Severe local hypothermia from laparoscopic gas evaporative jet cooling: a mechanism to explain clinical observations. JSLS 3: 171–177
Georgeson KE, Robertson DJ (2004) Minimally invasive surgery in the neonate: review of current evidence. Semin Perinatol 28: 212–220
Acknowledgment
We thank Dr. I. Valioulis at the Department of Pediatric Surgery, Aghios Loukas Hospital, Panorama Thessaloniki, Greece, and Professor Michel Robert at the Service de Chirurgie Viscérale Pédiatrique, Hôpital Clocheville, CHU Tours, France, for their participation in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalfa, N., Allal, H., Raux, O. et al. Multicentric assessment of the safety of neonatal videosurgery. Surg Endosc 21, 303–308 (2007). https://doi.org/10.1007/s00464-006-0044-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-006-0044-1