Abstract
The global spread of multi-drug resistant P. falciparum, P. vivax, and P. malariae strains and absence of long-term effective vaccine makes chemotherapy the mainstay of malaria control strategies in endemic settings. The Mossman’s assay and the Organization for Economic Co-operation and Development (OECD), 2001 guideline 423, were used to determine the cytotoxicity and acute oral toxicity of a novel hybrid drug, artesunate-3-Chloro-4(4-chlorophenoxy) aniline (ATSA), in vitro and in vivo, respectively. A modified Desjardins method was used to screen for antiplasmodial activity using P. falciparum (3D7 and W2) strains in vitro. The Peter’s 4-day suppressive tests (4DTs) was used to evaluate the in vivo antimalaria activity using P. berghei ANKA strain, lumefantrine resistant (LuR), and piperaquine resistant (PQR) P. berghei lines. In silico prediction of absorption, distribution, metabolism, excretion, and toxicity (ADMET) profiles was assayed using PreADMET online prediction tool. The reference drug in all experiments was artesunate (ATS). Statistical significance between ATSA’s activities in treated and control mice was evaluated by one-way analysis of variance (ANOVA). Results show that inhibitory concentrations-50 (IC50) of ATSA is 11.47 ± 1.3 (3D7) and 1.45 ± 0.26 (W2) against 4.66 ± 0.93 (3D7) and 0.60 ± 0.15 (W2) ng/ml of ATS with a selective index of 2180.91(3D7) and a therapeutic index (TI) of > 71). No mortalities were observed in acute oral toxicity assays and mean weight differences for test and controls were statistically insignificant (P > 0.05). The in vivo activity of ATSA was above 40% with effective dosage-50 (ED50) of 4.211, 2.601, and 3.875 mg/kg body weight against P. berghei ANKA, LuR, and PQR lines, respectively. The difference between treated and control mice was statistically significant (P < 0.05). ATSA has high intestinal absorption (HIA) > 95% and has medium human ether-a-go-go related gene (hERG) K+ channel inhibition risks. Preclinical and clinical studies on ATSA are recommended to evaluate its value in developing novel drugs for future management of multi-drug resistant malaria parasites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malaria is still a global health burden (Joseph et al. 2019; Beteck et al. 2014). An estimated 241 M cases and 627,000 deaths were reported in 2020 with the highest disease burden occurring in the sub-Saharan Africa (Cravo 2022; Nghochuzie et al. 2020). The major parasite species responsible for global malaria incidences are P. vivax; the most wide spread (Angrisano and Robinson 2022) and P. falciparum (Hermansyah et al. 2017) the most virulent (Tachibana et al. 2022). Acquired immunity (Joseph et al. 2019) which develops after a few episodes of parasite infections is short-lived (Horata et al. 2017). Vaccine development to boost host immunity, remains elusive hence chemotherapy is the mainstay of malaria control efforts (Dhanawat et al. 2009). Hybrid therapy is a recent approach which involves linking two compounds with individual mechanisms of action into a single molecule (Muregi and Ishih 2010). The resultant hybrid drugs exhibit enhanced chemo-therapeutic profiles (Meunier 2008) such as reduced drug toxicity, increased therapeutic outcome, and improved dosage compliancy (Lombard et al. 2013; Nilsen et al. 2014). They also display high parasite selectivity (Sharma et al. 2014) due to synergistic output of hybridized molecules. Development of resistant parasites is also circumvented or delayed since individual molecules target the parasite using different modes of action (Muregi and Ishih 2010; Nilsen et al. 2014).
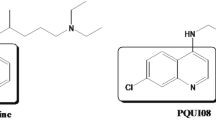
Various antimalarial drugs have been developed since the onset of hybridization. They include 4-aminoquinoline-pyrimidine that exhibited enhanced therapeutic outcome to both sensitive and resistant malaria parasites (Meunier 2008).
PA1103-SAR116242 showed improved antimalarial potency against CQ resistant and pyrimethamine resistant malaria strains; it acts by inhibiting hemozoin bio-crystallization (aminoquinoline moiety) and alkylating heme molecules (Meunier 2008). Trioxaquine comprising artesunate and 4,7-dichloroquinoline manifested superior antimalarial efficacy in treatment of cerebral malaria compared to precursors separately (Odhiambo et al. 2017). 4-Aminoquinolone-pyrimidine-derived hybrids also manifested higher efficacies in P. falciparum sensitive (D6) and resistant (W2) clones in vitro as well as in vivo in P. berghei parasites with wide safety margins compared to chloroquine (Manohar et al. 2012). Mefloquine-artesunate hybrid (MEFAS) derived from hybridization of mefloquine and artesunate gave improved potency compared to single molecules in vitro on P. falciparum W2 and 3D7 clones and in vivo on P. berghei NK65 strain (Varotti et al. 2008).
Malaria control is extremely hampered by existing multi-drug resistant Plasmodium falciparum, Plasmodium vivax, and Plasmodium malariae strains (Feng et al. 2020). Since the rapidly growing malaria parasites portray an exacerbated demand for lipids (Sifuna et al. 2019), type 2 fatty acid biosynthesis pathway offers an excellent target for antimalarial drugs. Inhibition of a vital P. falciparum enzyme; enoyl acyl carrier protein reductase (Pf. EACP) which catalyzes a NADH-dependent reduction of trans-2-enoyl-ACP to acyl-ACP, halts parasite survival (Sifuna et al. 2019). In this study, artesunate-3-chloro-4-(4-chlorophenoxy)aniline(ATSA) hybrid molecule was synthesized via covalent linkage of artesunate (ATS) and 3-chloro-4-(4-chlorophenoxy)aniline (ANI) under the concept of covalent biotherapy (Muregi and Ishih 2010). Toxicity assays of ATSA was determined by Mossman’s and the Organization for Economic Co-operation and Development (OECD) 423 protocols. Antimalarial activities were determined in vitro using P. falciparum (3D7) and (W2) and in mice using P. berghei ANKA and P. berghei lumefantrine resistant (LuR) and piperaquine resistant (PQR) parasite lines. The absorption, distribution, metabolism, excretion, and toxicity (ADMET) profiles were predicted in silico using the Pre-ADMET online tool. Artesunate (ATS) was used as a reference drug.
Experimental setup, methods, and conditions
Experimental site
This study was laboratory-based and all experiments were conducted at the malaria unit of the Centre for Biotechnology, Research and Development (CBRD), and the Centre for Traditional Medicine and Drug Research (CTMDR) both of Kenya Medical Research Institute (KEMRI) Headquarters, Mbagathi, Nairobi, Kenya.
Experimental animals
Randomly bred Swiss albino mice, 5 to 6 weeks old, same sex weighing 20 ± 2 g were maintained in an animal house experimental room in standard polypropylene (hard plastic) cages. The mice were placed in groups of three or five (separate male and female), clearly labeled with experimental details and fed on commercial rodent food and water ad libitum. Good Laboratory Practice and the KEMRI’s Animal Care and Use Committee (ACUC) standards and regulations were strictly adhered to hence minimizing animal suffering during all the assays. At the end of the experiments, both dead and moribund mice were euthanized using sodium pentobarbital (150 mg/kg), placed in biohazard disposable bags and autoclaved at 121 °C for 15 min to reduce environmental contamination during incineration.
Malaria parasites, Vero cells, and test drugs
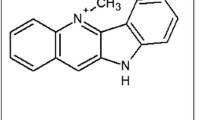
Cryopreserved P. falciparum, the chloroquine (CQ) sensitive 3D7 and CQ resistant, W2, P. berghei ANKA strain, P. berghei lumefantrine resistant (LuR), P. berghei piperaquine resistant (PQR), and Vero cell lines used in the assays were obtained from the KEMRI-CTMDR laboratory. To revive the cryopreserved P. berghei parasites, their suspensions were initially thawed, centrifuged to remove the cryopreservative and injected into three groups (P. berghei ANKA, LuR, and PQR) of two mice each using a needle of size 26G × 5/8″ through the intraperitoneal route. The parasites were passaged on a weekly basis into naive mice to resuscitate their virulence. These infected mice served as donors for setting the standard 4-day suppressive tests (4-DT) and curative tests after establishing a steady state parasitemia. Artesunate (ATS) was purchased from Sigma-Aldrich®, India. The hybrid drug (ATSA) was synthesized by covalently linking its precursors ATS and ANI through a sequential coupling solvent extraction process as summarized in Fig. 1. Briefly, 0.5 mmol of ATS was dissolved in dichloromethane (DCM) of volume v = 5 ml. 1-Ethyl-3-(3-dimethylaminopropyl) carbodiimide hydro-chloride (EDC) (1.5 eq), 1-hydroxy-benzotriazole (HOBt) (1.5 eq), and diisopropylethylamine (DIPEA) (3.0 eq) were then added and the whole mixture stirred at 0 °C in a round bottomed flask. To this mixture was added a solution of ANI (1.0 mmol) dissolved in 5 ml of DCM dropwise and the reaction stirred at room temperature overnight. The mixture was the quenched off with saturated NaHCO3, the organic phase separated and the aqueous phase back extracted with methylene chloride. Combined organic layers were dried using anhydrous magnesium sulfate (MgSO4), filtered and the solvent removed in vacuo.
Toxicity assays
Cytotoxicity assays
Vero E6 cell line was used to screen for the cytotoxicity of ATSA using the Mosmann, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetra-zolium bromide (MTT) cell viability assay. Prior to the assay, the trypan blue exclusion method was used to determine the cell density using an inverted microscope (A. Kruss Optronic, Germany) at × 400 magnification. Briefly, 100 µl of cell suspension at a density of 2 × 104 was seeded into 96-well flat-bottomed microtiter plates. The culture plates were then incubated at 37 °C with 5% CO2 for 24 h. Thereafter, 150 µl of the test drugs were added and a triplicate dilution was performed. The plates were again incubated for 24 h before 10 µl of 5 mg/ml MTT solution was added to each well to give a final concentration of 0.5 mg/ml. These plates were incubated for a further 4 h followed by addition of 100 µl dimethyl sulfoxide (DMSO) to dissolve formazan crystals. The absorbance was read at 562 nm/690 nm using a scanning multi-well spectrophotometer (Multi-scan EX Lab-systems). Data was entered in a MICROSOFT EXCEL software and inhibitory concentration that causes death of 50% cells (CC50) determined using Eq. 1 (Mosmann 1983).
The selective indices (SI) of the drugs were determined by Eq. 2:
Acute oral drug toxicity assays
Acute oral toxicity was conducted in accordance with the Organization of Economic Co-operation and Development (OECD 2001) guideline 423 Jonsson et al. 2013. Swiss female albino mice (three mice per group), 7 weeks old and weighing between 20 and 26 g were used. The mice were starved for 3 h, weighed and 200 µl of a single dose of 300 mg/kg body weight (bwt) of freshly prepared solutions of ATSA and ATS given by oral gavage using a stainless-steel feeding cannula. Negative control group received equal volume of distilled water. The mice were then observed continuously for the first 30 min post drug administration and then after 4 h and 24 h for any physical signs of drug intoxication: mortality, gross behavior, body conditions such as tremors, diarrhea, lethargy, salvation, and convulsions. The mice were continuously monitored at intervals of 4 days for 14 days with surviving mice weighed and the weight recorded. Therapeutic index (TI) of test drugs was then determined by Eq. 3:
where LD50 is lethal dose which cause death to 50% of the test animals while ED50 is the effective dose that suppresses 50% of the parasite (Muller and Milton 2012).
In vitro antiplasmodial screening assays
Human malaria parasites were cultured using the method of Trager and Jensen with slight modifications (Trager and Jensen 1976). P. falciparum cultures were maintained continuously at 37 °C followed by a 72 h susceptibility tests using radio-labelled [3H] hypoxanthine incorporation semi-automated microdilution assay technique in 96-well microtiter plates. Early-stage parasites, 3D7 and W2, were tested in duplicate. Briefly, 25 µl complete culture medium was added to all wells. Twenty-five microliters of either ATSA or TSA drugs was then added. A serial twofold dilution over a 64-fold concentration range was carried out using a motorized hand diluter. Two hundred microliters of parasitized RBCs at 0.4% parasitemia was then added to test wells. Into some control wells, 200 µl of non-parasitized RBCs was added. The plates were place in an air-tight gas chamber, gassed with 3% CO2, 5% O2, and 92% N2 and incubated for 72 h at 37 °C. Each specific well was then pulsed with 25 µl of culture medium containing 0.5 µCi of [3H] hypoxanthine and the plates incubated for 18 h. The contents of each well was harvested in glass fiber filters, washed several times and radioactivity measured in counts per minute using a liquid scintillator (Khan et al. 2017). The 50% inhibitory concentration (IC50) was obtained by nonlinear probit or regression of percentage growth inhibition for each drug.
In vivo assays
Parasite inoculation
Infected red blood cells (iRBCs) was collected into heparinized syringes using a needle whose size was 26G × 5/8 following cardiac puncture of the anesthetized donor mice with increasing parasitemia of between 10 and 15%. The parasitemia was adjusted downwards to approximately 1% using autoclaved phosphate saline with glucose (PSG) buffer. The buffer was initially constituted using 2.696 g disodium hydrogen phosphate, 5 g glucose, 0.156 g hydrated sodium dihydrogen phosphate, and 0.85 g sodium chloride all dissolved in 500 ml double-distilled water, sterilized by autoclaving and stored in the dark at 4 °C. During parasite injection, a mouse was restrained by holding tail ends with one hand while gently but firmly holding the loose skin at the neck and back using the same hand. The mouse was then held in an upright position and 200 µl parasite inoculum injected in the intraperitoneal (ip) cavity using the other hand.
Early infection tests
The standard 4-day chemo-suppressive tests (4DTs) were used to assess the percentage reduction in parasitemia in mice injected with P. berghei ANKA, LuR, and PQR iRBCs as described by Peters et al. (1975). Briefly, infected mice were distributed randomly into three test dose groups and a negative control group of five mice each. Drug solutions were freshly prepared just before administration by first solubilizing in dimethyl sulfoxide (DMSO) final concentration 1% followed by serial dilution with distilled water to required experimental concentrations. Two hundred microliters of each drug were administered orally to the mice at a time t = 3 h, 24 h, 48 h, and 72 h post infection using a stainless steel, 24-gauge feeding cannula (Harvard Apparatus; 25 mm in length, 1.25 mm ball diameter). Negative controls received distilled water. On day 4 (96 h) pi, thin blood smears from mice tail snips were prepared.
Thin smear staining and examination
Thin blood smears were fixed by immersing slides in absolute methanol for 30 s, air-drying, staining with 10% working Geimsa solution for 20 min, washing over running tap water and drying at the extreme edge of the hood (Omwoyo et al. 2014). A drop of immersion oil was placed on the smears and parasites examined using a microscope (OLYMPUS X3) at × 1000 magnification. Parasite load (percentage parasitemia; PP) from four random microscope fields was calculated using Eq. 4:
where TiRBC is the total number of infected RBCs while TRBC is the total number of RBCs. Percentage parasitemia suppression (PPS) (chemo-suppression) was determined using Eq. 5:
where A is the mean parasitemia in negative control group while B is the mean parasitemia in test groups.
Curative test
Experimental mice were injected ip with the P. berghei ANKA iRBCs and randomized into two test groups and a negative control of five mice each. Smears were made on D4 post-infection just before start of treatment to confirm infection and determine initial parasitemia. Drug solutions equivalent to ED50s of ATSA obtained in early infection test was administered on D4, D5, and D6. Smears were made on D7, D9, D11, and D13 to monitor the reduction in parasitemia. Percentage parasitemia was determined as previously described and average percentage suppression (APS) of parasitemia determined using Eq. 6:
where PD4 is the average % parasitemia before treatment, day 4, while PD7 is the average % parasitemia after treatment, day 7.
In silico prediction of ADMET profiles
ADMET profiles were predicted using Pre-ADMET online prediction tool. The 2D structures of ATSA and ATS were drawn using an online user interphase Chem-Doodle® drawing tool in Pre-ADMET server and directly submitted for calculation of absorption, distribution, metabolism, and toxicity parameters.
Data analysis
The in vitro data was expressed as mean ± SD while in vivo data was processed in Microsoft® Excel (Microsoft Corp.) data sheet and effective dose fifty (ED50) estimated graphically by linear regression using Statistica 2000 version 5.5. Statistical difference was determined using one-way analysis of variance (ANOVA) where a value of P < 0.05 was set as statistically significant.
Results
In vitro cytotoxicity and antiplasmodial activity
As shown in Fig. 2, the concentrations capable of causing visible alterations by 50% and thus inhibiting growth of cells (CC50) was 25.015 ± 2.325 µg/ml and 48.945 ± 0.035 µg/ml for ATSA and ATS, respectively. The IC50 for ATSA were 11.47 ± 1.3 ng/ml and 1.45 ± 0.11 ng/ml compared to 2.00 ± 0.93 ng/ml and 1.9 ± 0.15 ng/ml for ATSA using (3D7) and (W2), respectively. The selective index (SI50) was 2180.91 for ATSA and 42,475 for ATS using the sensitive 3D7 clone.
Acute in vivo toxicity
After 14 days, the mean weights of experimental mice in test and control groups ranged between 22.0 mg/kg body weight to 23.75 mg/kg as shown in Table 1. The mean weight difference between the test and control groups was statistically insignificant, P > 0.05. Based on these results, the LD50s for ATSA drug was estimated to be > 300 mg/kg bwt.
In vivo antimalarial activity assays
Early infection test
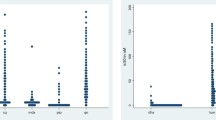
Percentage chemo-suppression of ATSA and ATS were determined in mice using the standard 4DTs against P. berghei ANKA, LuR, and PQR parasites. The results demonstrate dose-dependent relationships. In P. berghei ANKA, parasite chemo-suppression after a 3.0 mg/kg body weight was 41.47% for ATSA. ATSA suppressed LuR parasites by 63.30% and PQR parasites by 55.66% as shown in Fig. 3. The percentage activities of ATSA in P. berghei ANKA, LuR, and PQR compared to the controls were statistically significant P < 0.05. The effective dosages capable of decreasing the population of parasites by fifty percent (ED50s) were 4.211 mg/kg/day, 2.601 mg/kg/day, and 3.875 mg/kg/day for ATSA and 2.108 mg/kg/day, 1.883 mg/kg/day, and 0.961 mg/kg/day for ATS against P. berghei ANKA, LuR, and PQR parasites,respectively, as shown in Fig. 4.
Curative test
The average percentage chemo-suppression of ATSA in the curative test against P. berghei ANKA were determined on D7 in mice treated for 3 days (D4 to D6) with the drug’s ED50s value of 4.211 mg/kg/day obtained in the early infection test. The ATSA showed similar inhibitory potential compared to the untreated control and the percentage chemo-suppression of ATSA novel drug was statistically significant P < 0.05. Figure 5 indicates the average parasitemia between D4 and D13. The parasite load decreased gradually till D7. Beyond D7, growth of parasites began to increase.
In silico ADMET profiles
Absorption, distribution, metabolism, and toxicity profiles of ATSA with reference ATS were determined in silico, and the results are summarized in Table 2. Most ADMET parameters of the ATSA are similar as those of ATS which indicates the safety of the novel hybrid drug candidate.
Absorption profile
The human intestinal absorption (HIA), permeability to the human epithelial colorectal adenocarcinoma (Caco-2) cells, the Mandin-Darby canine kidney (MDCK) cells, P-glycoprotein (P-gp) inhibition, and skin permeability profiles demonstrate the absorption parameters. The novel drug ATSA shows a slightly higher HIA value, 96.831371% as compared to HIA value of 88.675981% for ATS. ATSA also exhibits a remarkably low permeability to MDCK cells (0.0695573* cm/s) as compared to 0.344241 cm/s for ATS but has high permeability to CaCO-2 cells (29.8626 cm/s) compared to 13.1902 cm/s for ATS.
ATSA inhibits P-gp and has a skin permeability of − 2.53826 cm/h while ATS is a non-inhibitor to P-gp with a skin permeability of − 3.77087 (cm/h), Table 2.
Distribution profile
Brain-blood barrier (BBB) penetration and percentage plasma protein binding (PPB) parameters display distribution patterns of ATSA and ATS. ATSA show a BBB value of 0.355308 compared to 0.0112762 for ATS. The PPB is 91.507% and 70.122% for ATSA and ATS respectively, Table 2
Metabolism profile
Metabolism was determined by screening whether ATSA in comparison with ATS was an inhibitor or a substrate to various members of cytochrome P450 gene (CYP) subfamilies: CYP 2C19 inhibition, CYP 2C9 inhibition, CYP 2D6 inhibition, CYP 3A4 inhibition, CYP 2D6 substrate, and CYP 3A4 substrate using Pre-ADMET predictor. It was found that ATSA is an inhibitor of CYP 2C19, CYP 2C9 and CYP 3A4 and non-substrate to CYP 2D6. ATSA also inhibits CYP 2D6 but it is a substrate for CYP 3A4, Table 2.
Toxicity profile
Toxicity was determined by screening for Ames mutagenicity, carcinogenicity in mouse or rat models and human ether-a-go-go related gene (hERG) potassium ion (K+) channel inhibition. ATSA shows non-mutagenicity to both TA100 and TA1535 strains similar to ATS. ATSA is carcinogenic to the rat model but not mouse model while ATS is carcinogenic to the mouse model alone. ATSA exhibit medium risks while ATS displays low risk of hERG K+ channel inhibition, Table 2.
Discussion
The world continues to lose effective antimalarial drugs due to the growing number of multi-drug resistant human malaria parasites. Since malaria continues to cause death mostly to children below the age of 5 years and pregnant women particularly in sub-Saharan Africa, alternative medications efficacious to both sensitive and resistant parasites are in constant need. This study thus evaluated the antimalarial activity, toxicity and in silico ADMET profiles of a novel molecule, artesunate-3-chloro-4(4-chlorophenoxy) aniline (ATSA) hybrid. Artesunate (ATS) was used as a standard drug. The in vitro cytotoxicity results revealed that the hybrid drug has a wide safety margin of 2180.91 compared to 42,475 for ATS using the sensitive 3D7 strain. No mortalities or significant weight differences occurred between the negative control mice and mice treated with ATSA at 300 mg/kg bwt. The LD50 for ATSA was estimated to be > 300 mg/kg with a therapeutic index (TI) > 71. The resultant safety margin was more than 30 times the effective dosage; 4.211 mg/kg/day required to reduce the parasite population by 50% (ED50).
ATSA exerted parasite chemo-suppression to both the sensitive and resistant P. falciparum and P. berghei parasites, P > 0.05. However, the antimalarial activity of ATSA was observed to be less than that of the popular clinically used trioxane drug artesunate. This might have been due to low solubility of the aniline component, which could in turn have affected the overall efficacy of the hybrid antimalarial candidate drug. It is also possible that ANI is a short acting drug and since artesunate is similarly a short acting antimalarial medicine, a decrease in the percentage parasite chemo-suppression for the hybrid was evident. However, the potency of this drug candidate may be enhanced through specific slight modifications of the linker as these have been shown to improve the chemotherapeutic outcome of hybridized drugs (Dambuza et al. 2015). ATSA targets the malaria parasites by two distinct mechanisms, ANI is critical in the FAS-II pathway in plasmodium apicoplasts (Sifuna et al. 2019). Artesunate on the other hand, promotes heme alkylation through its 1,2,3-trioxane entity which implies that development of resistance to this novel hybrid might be delayed or altogether circumvented (Coslédan et al. 2008).
Absorption of drugs into blood systems depends on apical-basolateral (A-B) permeability. Since the intestinal membrane acts as the first barrier to orally administered large and charged molecules (Gessner and Neundorf 2020), poor performance and low drug concentrations at target regions is attributed to limited solubility in aqueous media (Mehmood et al. 2020).
A drug penetrates membranes through passive diffusion, active transport and paracellular transport (Knöpfel et al. 2019) and various in silico tools are available to calculate percentage HIA as a sum of bioavailability and absorption. HIA is evaluated from the ratio of excretion or cumulative excretion in urine, bile and feces (Zhao et al. 2002) and permeability of a compound to either Caco-2 cells or MDCK cells. MDCK cells predict oral drug absorption with high accuracy. Caco-2 cells have multiple transport channels through the intestinal epithelia that mimics most transport pathways in gastrointestinal tracts. ATSA exhibited a high percentage HIA of 96.83% and a Caco-2 permeability of 29.86 cm/sec compared to 88.675981% and 13.1902 cm/s respectively for ATS. ATSA has remarkably low MDCK cell permeability of 0.0695573 cm/sec compared to the 0.344241 cm/s for ATS. This suggests that ATSA is highly bioavailable to suppress malaria infections.
Drug delivery into blood circulation through the skin has a wide range of advantages such as stomach bypass, higher patient compliancy, expeditious delivery of drugs with short half-life or narrow therapeutic index among others (Parhi and Mandru 2021). Skin permeability index analysis for a new drug is thus important as it indicates whether across-the-skin delivery is possible. It also indicates the possible extent of damage due to accidental contact with a drug (Silva et al. 2014). A negative value for skin permeability of − 2.44849 (cm/h) for ATSA and − 3.77087 (cm/h) of ATS suggest that ATSA cannot penetrate the skin and thus is equally safe as artesunate.
Distribution of a drug is determined by calculating the BBB penetration and percentage PPB profiles. BBB is a ratio of drug concentration in the brain to its concentration in blood (Cbrain/Cblood). Plasma protein binding of a drug influences its action and disposition as only unbound drug molecules are free to cross membranes by diffusion or active transport as well as for interaction with drug targets (Dohutia et al. 2017). From the results, ATSA has a considerably higher predicted BBB value of 0.355308 compared to 0.0112762 of ATS. It also has a higher PPB of 91.507% compared to 70.122% of ATS. A high BBB value may suggest that ATSA could find value in treatment of cerebral malaria. ATSA’s high PPB is likely to modify its pharmacokinetics hence its bioavailability and efficacy.
Drug metabolism is key to its eventual excretion from the body. In this study, the Pre-ADMET tool analyzed whether ATSA is a substrate or an inhibitor to the members of the CYP subfamily: CYP 2C19 inhibition, CYP 2C9 inhibition, CYP 2D6 inhibition, CYP 3A4 inhibition, CYP 2D6 substrate and CYP 3A4 substrate. Our results (Table 2) show ATSA as an inhibitor of CYP 2C19, CYP 2C9, and CYP 3A4 genes and a non-substrate to CYP 2D6 genes. It inhibits CYP 2D6 but it is a substrate for CYP 3A4. This displays an additional safety of ATSA to the human host cells.
Ames mutagenicity, carcinogenicity, and hERG K+ channel inhibition assays are used to determine toxicity profiles of drug candidates (Khan et al. 2017). Two strains of Salmonella typhimurium, TA100 and TA1535 (+ S9 activated with 10% liver homogenate and -S9 not activated) having mutations in genes responsible for histidine metabolism were used in predicting Ames test. The Ames test shows that ATSA is none mutagenic to the TA100 strain of bacteria. The hERG K+ channels are predominately expressed in cardiac muscles and blockade of these channels by drugs induces acquired long QT syndrome that may trigger arrhythmias (Tschirhart et al. 2019). ATSA exhibit medium risks to hERG K+ channel inhibition suggesting that it is safe.
Conclusion
Artesunate-3-chloro-4-(4-chlorophenoxy) aniline (ATSA) shows antimalarial chemosuppression activity against both the sensitive and the resistant human and mice malaria parasites with wide safety margins. This compound is thus a promising antimalarial drug candidate. To confirm the predicted ADMET parameters, in vivo studies are recommended. Pre-clinical and clinical studies should then follow to evaluate their value in the development of novel antimalarial drugs for future use in the management of multi-drug resistant malaria parasites.
Data availability
The datasets generated and/or analyzed during the current study are available from corresponding author on reasonable request.
References
Angrisano F, Robinson LJ (2022) Plasmodium vivax-how hidden reservoirs hinder global malaria elimination. Par Int 87:102526. https://doi.org/10.1016/j.parint.2021.102526
Beteck RM, Smit FJ, Haynes RK, N’Da DD (2014) Recent progress in the development of anti-malarial quinolones. Mal J 13(1):1–10
Coslédan F, Fraisse L, Pellet A, Guillouc F, Mordmullerd B, Kremsnerd GP, Morenf A, Mazierf D, Maffrand J, Meunier B (2008) Selection of a trioxaquine as an antimalarial drug candidate. PNAS 105(45):17579–17584
Cravo P (2022) On the contribution of the rodent model Plasmodium chabaudi for understanding the genetics of drug resistance in malaria. Par Int 91:102623. https://doi.org/10.1016/j.parint.2022.102623
Dambuza NS, Smith P, Evans A, Norman J, Taylor D, Andayi A, Egan T, Chibale K, Wiesner L (2015) Antiplasmodial activity, in vivo pharmacokinetics and anti-malarial efficacy evaluation of hydroxypyridinone hybrids in a mouse model. Mal J 14(1):1–8
Dhanawat M, Das N, Nagarwal RC, Shrivastava SK (2009) Antimalarial drug development: past to present scenario. Mini-Rev Med Chem 9(12):1447–1469
Dohutia C, Chetia D, Gogoi K, Bhattacharyya DR, Sarma K (2017) Molecular docking, synthesis and in vitro antimalarial evaluation of certain novel curcumin analogues. Braz J Pharm Sci 53(4):1–14
Feng LS, Xu Z, Chang L, Li C, Yan X, Gao C, Ding C, Zhao F, Shi F, Wu X (2020) hybrid molecules with potential in vitro antiplasmodial and in vivo antimalarial activity against drug-resistant Plasmodium falciparum. Med Res Rev 40(3):931–971
Gessner I, Neundorf I (2020) Nanoparticles modified with cell-penetrating peptides: conjugation mechanisms, physicochemical properties, and application in cancer diagnosis and therapy. Int J Mol Sci 21(7):1–21
Hermansyah B, Fitri LE, Sardjono TW, Endharti AT, Arifin S, Budiarti N, Candradikusuma D, Sulistyaningsih E, Berens-Riha N (2017) Clinical features of severe malaria: protective effect of mixed plasmodial malaria. Asian Pac J Trop Biomed 7(1):4–9
Horata N, Choowongkomon K, Ratanabunyong S, Tongshoob J, Khusmith S (2017) Acquisition of naturally acquired antibody response to Plasmodium falciparum erythrocyte membrane protein 1-dblα and differential regulation of igg subclasses in severe and uncomplicated malaria. Asian Pac J Trop Biomed 7(12):1055–1061. https://doi.org/10.1016/j.apjtb.2017.09.017
Jonsson M, Jestoi M, Nathanail AV, Kokkonen UM, Anttila M, Koivisto P, Karhunen P, Peltonen K (2013) Application of OECD Guideline 423 in assessing the acute oral toxicity of moniliformin. Food Chem Toxicol 53(2013):27–32
Joseph H, Eriksson E, Schofield L (2019) Early suppression of B cell immune responses by low doses of chloroquine and pyrimethamine: implications for studying immunity in malaria. Par Res 118(6):1987–1992
Khan FM, Bari MA, Islam MK, Islam MD, Kayser MS, Nahar N, Faruk MA, Rashid MA (2017) The natural anti-tubercular agents: in silico study of physicochemical, pharmacokinetic and toxicological properties. J App Pharm Sci 7(5):34–38
Knöpfel T, Himmerkus N, Günzel D, Bleich M, Hernando N, Wagner CA (2019) Paracellular transport of phosphate along the intestine. Am J Physi-Gastro Liver Physi 317(2):G233–G241
Lombard M, N’Da DD, Van Ba CT, Wein S, Norman J, Weisner L, Vial H (2013) Potent in vivo anti-malarial activity and representative snapshot pharmacokinetic evaluation of artemisinin-quinoline hybrids. Mal J 12(1):1–7
Manohar S, Rajesh CU, Khan SI, Tekwani BL, Rawat DS (2012) Novel 4-aminoquinoline-pyrimidine based hybrids with improved in vitro and in vivo antimalarial activity. ACS Med Chem Let 3(3):555–559
Mehmood Y, Khan IU, Shahzad Y, Khan RU, Igbal MS, Khan HA, Yousaf AM, Khalid SH, Asghar S, Asif M, Hussain T, Shah SU (2020) In vitro and in vivo evaluation of velpatasvir-loaded mesoporous silica scaffolds. A prospective carrier for drug bioavailability enhancement. Pharmaceutics 12(307):1–18
Meunier B (2008) Hybrid molecules with a dual mode of action: dream or reality. Acco Chemi Res 41(1):69–77
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immu Meth 65(80):55–63
Muller PY, Milton MN (2012) The determination and interpretation of the therapeutic index in drug development. Nat Re Drug Disc 11(10):751–761
Muregi FW, Ishih A (2010) Next-generation antimalarial drugs: hybrid molecules as a new strategy in drug design. Drug Dev Res 71(1):20–32
Nghochuzie NN, Olwal CO, Uduokang AJ, Amang-Etego LN, Amambua-Ngwa A (2020) Pausing the fight against malaria to combat the COVID-19 pandemic in Africa: is the future of malaria bleak? Fron Microbiol 11:1–5
Nilsen A, Miley GP, Forquer IP, Mather MW, Katneni K, Li Y, Pou S, Pershing AM, Stickles AM, Ryan E, Kelly JX, Doggett JS, White KL, Hinrichs DJ, Winter RW, Charman SA, Zakharov LN, Bathurst I, Burrows JN, Vaidya AB, Riscoe MK (2014) Discovery, synthesis, and optimization of antimalarial 4(1 H)-quinolone-3-diarylethers. J Med Chem 57(9):3818–3834
Odhiambo OC, Wamakima HN, Magoma GN, Kirira PG, Malala BJ, Kimani FT, Muregi FW (2017) Efficacy and safety evaluation of a novel trioxaquine in the management of cerebral malaria in a mouse model. Mal J 16(1):1–9
Omwoyo WN, Ogutu B, Oloo F, Swai H, Kalombo L, Melariri P, Mahanga GM, Gathirwa JW (2014) Preparation, characterization, and optimization of primaquine-loaded solid lipid nanoparticles. Int J Nanomed 9(1):3865–3874
Parhi R, Mandru A (2021) Enhancement of skin permeability with thermal ablation techniques: concept to commercial products. Drug Deliv Trans Res 11(3):817–841
Peters W, Portus JH, Robinson BL (1975) The chemotherapy of rodent malaria, XXII. Ann Trop Med Paras 69(2):155–171. https://doi.org/10.1080/00034983.1975.11686997
Sharma M, Chauhan K, Srivastava RK, Singh SV, Srivastava K, Saxena JK, Puri SK, Chauhan MS (2014) Design and synthesis of a new class of 4-aminoquinolinyl- and 9-anilinoacridinyl schiff base hydrazones as potent antimalarial agents. Chem Biol Drug Des 84(2):175–181
Sifuna MW, Wambui M, Nganga JK, Kariuki DW, Kimani FT, Muregi FW (2019) Antiplasmodial activity assay of 3-Chloro-4- (4-Chlorophenoxy ) aniline combinations with artesunate or chloroquine in vitro and in a mouse model. BioMed Res Int 2019:1–7
Silva NSR, Gonçalves LKS, Duarte JL, Silva JS, Santos CF, Braga FS, Silva RC, Costa JS, Hage-Melim LIS, Dos Santos CBR (2014) Computational analysis of physicochemical, pharmacokinetic and toxicological properties of deoxyhypusine synthase inhibitors with antimalarial activity. Comp Mol Biosci 04(04):47–57
Tachibana M, Takashima E, Morita M, Sattabongkot J, Ishino T, Culleton R, Torii M, Tsuboi T (2022) Plasmodium vivax transmission-blocking vaccines: progress, challenges and innovation. Par Int 87(2021):102525. https://doi.org/10.1016/j.parint.2021.102525
Trager W, Jensen BJ (1976) Human malaria parasites in continous culture. Reports 193(4254):673–75
Tschirhart JN, Li W, Guo J, Zhang S (2019) Blockade of the human ether a-go-go–related gene (hERG) potassium channel. Mol Pharm 95(4):386–397
Varotti FDP, Botelho ACC, Andrade AA, Paula RC, Fagundes EMS, Valverde A, Mayer LMU, Mendonca JS, Souza MVN, Boechat N, Krettli AU (2008) Synthesis, antimalarial activity, and intracellular targets of mefas, a new hybrid compound derived from mefloquine and artesunate. Antimic Agents Chem 52(11):3868–3874
Zhao YH, Le J, Abraham MH, Hersey A, Eddershaw PJ, Luscombe CN, Boutina D, Beck G, Brad S, Cooper I, Platts JA (2002) Evaluation of human intestinal absorption data and subsequent derivation of a quantitative structure-activity relationship (QSAR) with the Abraham descriptors. J Pharm Sci 91(2):605
Acknowledgements
The authors would like to acknowledge Stephen Kaniaru of KEMRI-CBRD for his guidance during in vitro work and Mr. Lucas Ogutu of KEMRI animal house for providing mice for in vivo assays.
Funding
This study was funded by research grants from AFRICA ai JAPAN PROJECT (Innovation Centre for Molecular Biology and Biochemistry) 2014 and National Commission for Science, Technology and Innovation (NACOSTI/RCD/ST&I 6th CALL MSc 055) awarded to Milka Wambui Waithera.
Author information
Authors and Affiliations
Contributions
Milka W. Waithera sourced for research funds and performed the experiments. Milka W. Waithera and Martin W. Sifuna analyzed data, drafted and revised the final manuscript. Daniel W. Kariuki, Johnson K. Kinyua, Francis T. Kimani, Joseph K. Nganga, and Masahiro Takei reviewed the final manuscript before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by KEMRI’s ACUC, KEMRI-ACU 01/10/2018.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Handling Editor: Una Ryan
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Waithera, M.W., Sifuna, M.W., Kariuki, D.W. et al. Antimalarial activity assay of artesunate-3-chloro-4(4-chlorophenoxy) aniline in vitro and in mice models. Parasitol Res 122, 979–988 (2023). https://doi.org/10.1007/s00436-023-07801-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-023-07801-x