Abstract
In response to increasing complaints of head louse infestation in the area of Cambridge, UK, in the mid-1990s, a series of prevalence surveys in selected schools coupled with collection of lice were commissioned by the local health authority. Carers of infested children were provided with advice on treatment by school nurses. Lice collected during these surveys were tested in the laboratory for evidence of resistance to insecticides. These data were used by the health authority to make decisions about recommended insecticide use for control of head infestations. Surveys over 3 years 1995–1997 found increasing prevalence of lice and increasing resistance to pyrethroids and malathion insecticides across the city. In two selected linked schools, the school nurse initiated a series of workshops and demonstrations to encourage families to treat by wet combing with conditioner in line with government recommendations and local general practitioner advice. Surveys conducted before and after the combing initiative found that prevalence increased in one school and was effectively unchanged in the other. Data collected in 1996 and 1997 from two schools showed that some families were continuously infested across 2 years and would act as a reservoir of infestation for the rest of the community.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the past century, there have been numerous point prevalence surveys of head louse infestation from almost all parts of the world. The majority of these have been one-off investigations with little or no follow-up, and as such, do not provide more than just a snap-shot of what was happening in one relatively small community on one day. A few studies have followed up on the initial findings, either to check on the effectiveness of an intervention (Gholamnia Shirvani et al. 2011; Kavur et al. 2022; Moshki et al. 2017; Nor Faiza et al. 2019; Yingklang et al. 2018), the influence of demographic characteristics (Gholamnia Shirvani et al. 2011; Kavur et al. 2022; Moshki et al. 2017; Nor Faiza et al. 2019; Willems et al. 2005; Yingklang et al. 2018) or attempting to follow communities over a longer period, such as screening in consecutive years to look for influence of resistance (Downs et al. 1999, 2007). Generally, such studies have been conducted in schools, these being the perceived focal point of louse transmission as well as the convenient location for accessing children at the age when they are most likely to catch lice.
Some recent studies have focussed on educational targets for students to improve their self-care and behaviours in relation to head louse transmission using questionnaires and training aids (Gholamnia Shirvani et al. 2011; Kavur et al. 2022; Moshki et al. 2017; Nor Faiza et al. 2019; Yingklang et al. 2018). Each has shown improved knowledge and attitudes towards reduction of infestation after 2 weeks to 2 months, but only two studies reported a specific reduction of infestation outcome (Kavur et al. 2022; Yingklang et al. 2018). One group in Thailand found a 44% reduction in the intervention population compared with 65% increase in the controls, with incidence rates of 6.14 and 12.6% respectively over the study period (Yingklang et al. 2018). The other in Türkiye found a reduction of overall prevalence from 15.22 to 1.71% over an unspecified period (Kavur et al. 2022). Nobody has yet demonstrated whether these statistically significant short-term outcomes can have a long-term impact on the infestation rates in the societies involved. Recent studies have also highlighted social economic status (SES) as an important factor in determining both attitude and activity in relation to louse control (Gholamnia Shirvani et al. 2011; Kavur et al. 2022; Moshki et al. 2017; Nor Faiza et al. 2019; Willems et al. 2005; Yingklang et al. 2018), and noted that there are links between SES, educational status of parents, “clustering” (number of household members), and ability to manage infestation. However, beyond basic training, there has been no follow-up to aid households in louse management.
It has always been the case that within any school community, there are some children who are regularly infested, whether this is because their parents/guardians do not trouble to treat the infestation or whether they try and are not only unsuccessful but do not follow up and seek help when they find themselves unable to deal with the problem. Equally, there are always parents who regularly complain about “others” who don’t bother about treating head lice so that their children regularly become infested by them. The truth is probably somewhere in between but no data have been presented so far to show this either way.
In the UK, resistance of head lice to pyrethroid insecticides was first noted around 1993 following widespread use of products introduced approximately 2 years earlier (Burgess et al. 1995). By 1995, lack of efficacy was so common around the city of Cambridge that the local Consultant Community Paediatrician authorised a series of school surveys to determine the prevalence of head louse infestation and the sensitivity of any lice collected to the available insecticides. These surveys enabled us to monitor changes in infestation rates in these communities over 2–3 years and identify households where lice were a persistent problem.
Materials and methods
School screening
This study was initiated at a time when inspection of children for head lice by school nurses no longer took place. It was set up as a collaboration between the school health service for Cambridgeshire, UK, and the Medical Entomology Centre (MEC) to provide the designated medical officer for school health with information about the prevalence status of head louse infestation at the time and the susceptibility of those lice to available treatments. Letters were sent from MEC to the school nurses and head teachers of the 32 primary schools in Cambridge city and immediately adjoining villages inviting interest in taking part in the survey, with an initial aim to screen children in a first tranche of five schools representing the diversity of communities within the area. A secondary aim was to address the specific concerns of particular school communities about issues with head louse infestation.
Once schools had been selected, an appointment was made with the head teacher and school nurse for a team from MEC to visit and examine all children in the school on a single day. No notice was given to other staff or to parents/guardians to avoid deliberate absences or treatment of cases before the visit so that, if possible, all extant infestations could be identified. At that time, the designated medical officer for schools, in this case the Consultant Community Paediatrician, could authorise examinations under the provisions of the Education Act 1995, Part IX, Chapter II, Section 521 – “Examination of pupils for cleanliness” without consent of parents/guardians or referral to an ethics committee.
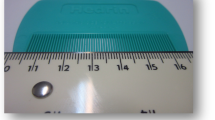
Screening was carried out using a plastic louse detection comb with teeth no more than 0.3 mm apart (Albyn of Stonehaven Ltd, Stonehaven, Scotland) on dry hair. The process varied from school to school but generally the examinations took place away from the classroom with the children being examined in a separate area from where their peers were waiting to be seen. Each child was combed systematically. The time spent combing each child depended upon how long, thick, and curly the hair was. In some cases, it was necessary to disentangle and brush hair before detection combing could be carried out, taking up to 5 min per individual, but for those with short straight hair, combing could be completed in less than 1 min. Any lice found were collected into 90 mm diameter glass Petri dishes lined with Whatman No. 1 filter paper. At the end of the school day, any child found to have lice was given a letter from the school nurse, which gave advice on treatment and an offer of assistance if required.
Testing for resistance
After visiting each school, any lice collected were returned to the laboratory and given a blood meal from the back of an investigator’s hand before any testing. Testing for sensitivity to insecticides used a modified version of the WHO method for determining susceptibility or resistance in lice (Burgess 2023; Burgess and Brown 1999).
Initial tests were conducted to identify the presence and distribution of permethrin resistance using 1.0% permethrin-treated filters. Alternative insecticide tests were performed using 5.0% malathion-impregnated papers (Burgess 2023; Burgess and Brown 1999).
Results
School screening
The first school survey in March and April 1995 included five schools, designated A–E in Table 1, from across the city of Cambridge. In total, 1379 children were screened. All schools visited were similar in size and all these communities thought they suffered a serious louse infestation problem. For example, one of the governors of School A told the headteacher that she would not be surprised if 50% of the children were infested. The actual number found was 11 out of a school attendance on the day of 316, a point prevalence of 3.48%. That year, the breakdown of infestation across classes and year groups was reported only to the individual schools themselves and their school nurses so that advice notes could be sent home. Total numbers, shown in Table 1, were forwarded to the Consultant Community Paediatrician.
Schools A and B in Table 1 were full Primary schools with children from 4 to 11 years of age (Year groups Nursery to Year 6). Schools C and E were Infant schools covering Nursery to Year 2 (ages 4–7), and School D was a Junior school that was fed by School C and covered Years 3–6 (ages 8–11).
Prevalence in all five schools was lower than was expected by the school staff, the school nurses, and the parents of children attending, with an overall indicative value of 6.74% across the city. Only children with live lice were included. The presence of eggshells (nits) alone was only evidence of past infestation, which in some cases had occurred several months before as judged by how far down the hair shaft they were placed, but in others they were close to the scalp indicating a recent successful treatment.
The screening observations, and the insecticide sensitivity test outcomes, resulted in a health authority policy change regarding recommended treatment from pyrethroid insecticides to malathion. To evaluate how effective that change had been, a second schools survey was set up approximately 1 year later. This series of visits in May and June 1996 examined children attending the same five schools shown in Table 1, plus four others (L-O) that were full Primary schools. This time the distribution of infestation across teaching groups was recorded. Table 2 shows data from schools A, B, E, and L–O, with findings from schools C and D for 1996 and a follow up in 1997 shown in Table 3.
Further screening in schools C and D was carried out in 1997 as part of an initiative by the school nurse to encourage parent/guardians to try to eliminate or manage infestations using the wet combing with conditioner approach encouraged by the Department of Health (DoH 1996). The first visit was to identify how many children had head lice in May 1997, after which the nurse held a series of information and training sessions for care givers, demonstrating wet combing and advocating it as the optimum approach for a sustainable whole school control (Ibarra et al. 2007). The second screening in June 1997 was to evaluate how effective the information and training had been for reducing the level of infestation in the two schools. Table 3 shows the numbers of lice found in each classroom group of students at each of the screening sessions. In school C the number of children found to have lice increased from 35 to 47 during the two weeks between visits and in school D there was a minimal reduction from 45 to 43 cases. Most children stated that their parent had neither checked nor wet combed their hair during the 2 weeks but, of those children found with lice at the first visit, 8 children from school C were louse free by the second visit but 18 were still infested and 19 children from school D had been cured but 18 had not. In school C there were 28 children who did not have lice at the first visit but were infested by the second visit and 24 in school D. One boy in school D had been treated the night before the second visit using a malathion lotion, which had been left in situ, and had failed to kill many of the lice. Some children who were infested at the first visit were absent for the second visit.
In these two schools, it was possible to trace infestations between them, because they were linked, and members of several families could be found in both. Thus, across three screening visits over 2 years, it was possible to identify households where infestation occurred regularly and perhaps continuously. Over 39 families with 58 children we found 105 instances of infestation, with 37 of the children infested on both screenings in 1997, indicating that any attempt to eliminate infestation through the wet combing initiative had little or no effect, if it had even been tried. Nine children were infested both in 1996 and 1997, and three children, all from different households, were infested at each of the three screening visits (Table 4).
Insecticide sensitivity
Lice collected during these visits were tested for insecticide sensitivity on the day they were collected. Some lice from all schools visited in 1995 remained susceptible to permethrin but others from the same schools were tolerant (Burgess 2023). Some exhibited minor tremors as a result of insecticide uptake but continued normal movements and took a blood meal if placed on the back of a hand. Probit analyses showed a general loss of sensitivity to permethrin, and a threefold relative resistance to malathion compared with susceptible laboratory reared lice, whereas carbaryl remained fully effective (Burgess 2023). By 1996, relative resistance to permethrin had increased 12-fold compared with susceptible lice, and for malathion was increased 10.5-fold (Burgess 2023).
In 1996, where enough insects were collected, the insecticide sensitivity of several groups of lice was tested by exposure to insecticide-based products rather than on insecticide treated test papers. It was found that 61.4% (89/145) of lice from School A; 50.5% (102/202) from School B; 63.2% (24/38) from School C; 80.8% (42/52) from School D; and 57.7% (15/26) from School N were resistant to pyrethroids. In addition, 75.0% (57/76) of lice from school D and 59.1% (39/66) from School N were resistant to malathion, but none of those tested from any school were resistant to carbaryl.
Discussion
This survey work conducted in and around the city of Cambridge found essentially similar point prevalence of head louse infestation in those school populations screened during both 1995 and 1996 (Table 1). However, between 1996 and 1997 the prevalence in Schools C and D approximately doubled (Table 3) and in School C the 1997 prevalence was nearly six times that in 1995. It also found that over the 1-year period from late spring 1995 to early summer 1996, levels of resistance to insecticides increased despite a change in recommended insecticide from permethrin to malathion (Burgess and Brown 1999).
The year 1995 was a turning point for head louse control in the UK. Insecticide resistance had a significant impact on general practice prescribing costs, as a result wet combing with conditioner was widely encouraged (DoH 1996), and became the standard recommendation by general practitioners in the health centre serving the population whose children attended Schools C and D. Consequently, it was appropriate for the school nurse working in those schools to attempt to encourage that approach to treatment during the spring of 1997. The results, shown in Table 3, demonstrate that either the programme of training and encouragement was inadequate, or else the parent carers of the children chose not to engage with it, such that there was no reduction in prevalence at all within the schools after the 2-week programme and an increase in School C of 34% in cases over that period.
Several households in the community had children attending both schools so infestation of one sibling in one school could be passed to another attending the other school, with a resulting onward risk for their classmates and friends. From Table 4, a trend can be seen in some households for lice to persist from 1 year to the next in individuals and to be passed back and forth between siblings. This continued infestation indicates that either the care givers made little or no attempt to eliminate the infestation from their children or else insecticide resistance or poor combing techniques made their efforts ineffective in a similar manner to the Belgian study that found 41% of the children identified with lice were still infested 2 weeks after being given advice on treatment and louse management (Willems et al. 2005). Some parents complained that other people were not treating, so their children were regularly reinfested, but it could be that most people who treated their children did not follow up to check whether the product used was effective. We have found similar situations of repeated and continuing infestations in other households participating in clinical intervention studies in which an additional factor of lice passing back and forth within extended and complex families occurred, where the contacts were outside the study area or chose not to be treated at the same time as their relatives.
Few studies have looked at infestation rates in the same population over time and fewer have considered the effects of resistance on the incidence or prevalence of lice. In Bristol, UK, Downs and colleagues (Downs et al. 2007) found infestation rates of 19.0%, 28.3%, and 16.7% in three schools screened in 1997, 1998, and 2000 respectively in an area where high levels of resistance to most insecticides had previously been detected (Downs et al. 1999). They speculated that the decrease in prevalence in 2000, which paralleled data from the Royal College of General Practitioners sentinel scheme (RCGP 2007), may have been the result of increased combing rather than a move from prescribed to over the counter purchased insecticides. That insecticide use had changed showed clearly in the weekly returns of the sentinel scheme (RCGP 2007), which recorded general practitioner consultations leading to a prescription. The incidence in 5–14-year-olds, the main group affected by head lice, showed 31 cases/100k population in 1994, 64 in 1995, peaked at 127 in 1996 and then declined to 77 in 1997, 37 in 1998, and just 10/100k in 1999. Rather than a true decline in incidence this reflected reduced prescribing by GPs following the DoH guidance (DoH 1996). Over the period, pharmaceutical industry sales figures showed no decline in purchasing of insecticides (Downs et al. 1999, 2007).
In Norway, where no resistance has been reported, despite its presence in nearby Denmark (Kristensen et al. 2006), prevalence was found to increase between October 2009 and May 2010 in 12 schools in the capital Oslo (Birkemoe et al. 2016). A combination of combing screening and questionnaires found a steady increase from 1.7% at the initial screening 3.2%, 3.4%, 5.8%, to 6.0% by the end of the study. However, it is not possible to say whether this was an accurate reflection of the infestation rate, since after the initial screening fewer than 40% of the students were included. The authors did identify that having a sibling with lice was the highest predictor of risk for infestation, followed by having had lice previously, similar to our findings shown in Table 4.
All the data collected from these successive examinations of European populations (Birkemoe et al. 2016; Downs et al. 1999, 2007; Kristensen et al. 2006; RCGP 2007) have shown prevalence of head lice increased over time in a manner that was primarily associated with presence or increase in insecticide resistance. This occurred irrespective of the type of intervention recommended by health professionals and even the specific targeted intervention programme we have described appeared to have no effect even in the short term, and it was only the presence of insecticide resistance that serendipitously allowed us to identify those households in this study where lice persisted as a reservoir for spread through the community. The two sets of data that did appear to show some later decline over time (Downs et al. 2007; RCGP 2007) probably only reflected a change of habit by caregivers from use of prescribed medications to those bought over the counter. Education programmes for hair care management and awareness of head lice, conducted in communities where ready access to advice and treatments are not normally available, have appeared to make a positive difference to prevalence, especially the most recent study in Türkiye that showed a reduction almost to zero by the fourth screening visit (Kavur et al. 2022). However, the report did not state over what interval this impact was achieved, and it remains to be seen whether such impacts are sustainable or whether prevalence would rapidly re-establish after the investigation ended, the question that currently follows on from the findings in some areas of significantly reduced prevalence of lice subsequent to the Covid-19 pandemic (Bonanno et al. 2022; Galassi et al. 2021; Launay et al. 2022; Mumcuoglu et al. 2022). Individual household case studies, such as that given by Adie (1997), show that in complex family structures elimination of infestation may be achieved by intensive and repeated interventions but that rapid reinfestation in these relationships may occur readily. Consequently, only repeat screening surveys carried out over more than just a few weeks can demonstrate those individuals and households who act as a reservoir of infestation and whether interventions are having any lasting effect on head louse prevalence in the community. This study is a revisitation of data that were originally collected for evaluating the development of insecticide resistance rather than measuring the long-term epidemiology of head lice in the schools in Cambridge. However, it is quite likely that some of the children found with lice in this study were treated effectively but were rapidly reinfested from their peers, something that we are currently finding in certain households as lice recover their numbers after the effects of Covid-19, with background indications that some of the current treatments are losing their effectiveness in a similar way to conventional insecticides in the mid-1990s.
Data availability
All non-confidential data are given in the manuscript.
References
Adie B (1997) Controversies in head lice treatment. In: Burrage H (ed) The North Thames Head Lice Symposium, pp 34–40
Birkemoe T, Lindstedt HH, Ottesen P, Soleng A, Næss Ø, Rukke BA (2016) Head lice predictors and infestation dynamics among primary school children in Norway. Fam Pract 33:23–29. https://doi.org/10.1093/fampra/cmv081
Bonanno M, Lee OS, Sayed C (2022) Decreases in scabies and lice cases among the pediatric and adult populations during COVID-19. Pediatr Dermatol 39:737–739. https://doi.org/10.1111/pde.15083
Burgess IF (2023) Head lice: an inexpensive bioassay for use as guidance for healthcare workers monitoring treatment failures for insecticide resistance (1994–1999). Parasitol Res 122:425–433. https://doi.org/10.1007/s00436-022-07737-8
Burgess IF, Brown CM (1999) Measuring insecticide resistance in human head lice Pediculus capitis (Anoplura: Pediculidae). In: Robinson WH, Rettich F, Rambo GW (eds) Proceedings of the 3rd International Conference on Urban Pests. Grafické závody, Prague, p 634
Burgess IF, Brown CM, Peock S, Kaufman J (1995) Head lice resistant to pyrethroid insecticides in Britain. Brit Med J 311:752. https://doi.org/10.1136/bmj.311.7007.752
DoH. (1996) The prevention and treatment of head lice. Department of Health, UK, London
Downs AMR, Stafford KA, Coles GC (1999) Head lice: prevalence in schoolchildren and insecticide resistance. Parasitol Today 15:1–4. https://doi.org/10.1016/s0169-4758(98)01361-1
Downs AMR, Ross AM, Fleming DM, Coles GC (2007) A downturn in the incidence of head lice infestation? Int J Dermatol 46:660–661. https://doi.org/10.1111/j.1365-4632.2007.01685.x
Galassi F, Ortega-Insaurralde I, Adjemian V, Gonzalez-Audino P, Picollo MI, Toloza AC (2021) Head lice were also affected by COVID-19: a decrease on pediculosis infestation during lockdown in Buenos Aires. Parasitol Res 120:443–450. https://doi.org/10.1007/s00436-020-07038-y
Gholamnia Shirvani Z, Amin Shokravi F, Ardestani MS (2011) Effect of designed health education program on knowledge, attitude, practice and the rate Pediculosis capitis in female primary school students in Chabahar city. (in Persian) Journal of Shahrekord University of Medical Sciences 13(3):25–35
Ibarra J, Fry F, Wickenden C, Olsen A, Vander Stichele RH, Lapeere H, Maryan J, Franks A, Smith JL (2007) Overcoming health inequalities by using the Bug Busting ‘whole-school approach’ to eradicate head lice. J Clin Nurs 16:1955–1965. https://doi.org/10.1111/j.1365-2702.2007.01795.x
Kavur H, Özkurt H, Büyükkatran F, Evyapan G, Kalkan S, Ҫelik Z, Kurcan E, Karataş DA, Alptekin D (2022) Effect of education and regular examination on the prevalence of head louse infestations in Adana. Türk Parazitoli Derg 46:327–333. https://doi.org/10.4274/tpd.galenos.2022.24006
Kristensen M, Knorr M, Rasmussen AM, Jespersen JB (2006) Survey of permethrin and malathion resistance in human head lice populations from Denmark. J Med Entomol 43:533–538. https://doi.org/10.1093/jmedent/43.3.533
Launay T, Bardoulat I, Lemaitre M, Blanchon T, Fardet L (2022) Effects of the COVID-19 pandemic on head lice and scabies infestation dynamics: a population-based study in France. Clin Exp Dermatol 47:867–872. https://doi.org/10.1111/ced.15054
Moshki M, Zamani-Alavijeh F, Mojadam M (2017) Efficacy of peer education for adopting preventive behaviors against head lice infestation in female elementary school students: a randomised controlled trial. PLoS ONE 12(1):e0169361. https://doi.org/10.1371/journal.pone.0169361
Mumcuoglu KY, Hoffman T, Schwartz E (2022) Head louse infestations before and during the COVID-19 epidemic in Israel. Acta Trop 232:106503. https://doi.org/10.1016/j.actatropica.2022.106503
Nor Faiza MT, Saliluddin SM, Lye MS, Rampal L, Ying LP (2019) Effectiveness of school-based health education intervention on knowledge, attitude and practices in pediculosis capitis. International Journal for Studies on Children, Women, Elderly and Disabled 7:23–32
RCGP (2007) Weekly Returns Service Annual Report. Royal College of General Practitioners, Birmingham Research Unit
Willems S, Lapeere H, Haedens N, Pasteels I, Naeyaert J-M, de Maeseneer J (2005) The importance of socio-economic status and individual characteristics on the prevalence of head lice in schoolchildren. Eur J Dermatol 15:387–392
Yingklang M, Sengthong C, Haonon O, Dangtakot R, Pinlaor P, Sota C, Pinlaor S (2018) Effect of a health education program on reduction of pediculosis in school girls at Amphoe Muang, Khon Kaen Province. Thailand. PLoS ONE 13(6):e0198599. https://doi.org/10.1371/journal.pone.0198599
Funding
This study was supported financially by a grant from the Department of Health paid through Cambridgeshire Health Authority.
Author information
Authors and Affiliations
Contributions
The author designed the study, performed the experiments, and wrote the manuscript. Unnamed colleagues who assisted in screening for lice are now either retired or inaccessible.
Corresponding author
Ethics declarations
Ethics approval
Not required because the Designated Medical Officer authorised examinations under the provisions of the Education Act 1995, Part IX, Chapter II, Section 521 – “Examination of pupils for cleanliness”.
Conflict of interest
The authors declare no competing interests.
Additional information
Section Editor: Boris Krasnov
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Burgess, I.F. Do some families act as a reservoir of head lice in the community? Surveys for prevalence and insecticide resistance suggest this is the case. Parasitol Res 122, 945–952 (2023). https://doi.org/10.1007/s00436-023-07795-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-023-07795-6