Abstract
Purpose
This research aimed to clarify the metastatic patterns of subcarinal, right and left recurrent laryngeal nerve lymph nodes in thoracic esophageal squamous cell carcinoma and to investigate appropriate strategies for lymph node dissection.
Methods
Patients with thoracic esophageal squamous cell carcinoma receiving esophagectomy from December 2020 to April 2024 were retrospectively analyzed. Risk factors for subcarinal, right and left recurrent laryngeal nerve lymph nodes metastasis were determined by chi-square test and multivariate logistic regression analysis. We visualized the metastasis rates of these specific lymph nodes based on the different clinicopathological characteristics. Correlation between subcarinal, right and left recurrent laryngeal lymph nodes metastasis and postoperative complications were also analyzed.
Results
A total of 503 thoracic esophageal squamous carcinoma patients who underwent esophagectomy were enrolled. The metastasis rates of subcarinal, right and left recurrent laryngeal nerve lymph nodes were 10.3%, 10.3%, and 10.9%, respectively. The lymphovascular invasion status and tumor location were the significant predictors for subcarinal and right recurrent laryngeal nerve lymph nodes metastasis, respectively (P < 0.001 and P = 0.013). For left recurrent laryngeal nerve lymph node metastasis, younger age (P = 0.020) and presence of lymphovascular invasion (P = 0.009) were significant risk factors. Additionally, pulmonary infection is the most frequent postoperative complication in patients with dissection of subcarinal, right and left recurrent laryngeal lymph nodes. There was no significant difference in the incidence of anastomotic leakage (P = 0.872), pulmonary infection (P = 0.139), chylothorax (P = 0.702), and hoarseness (P = 0.179) between the subcarinal lymph node dissection cohort and the reservation cohort. The incidence of hoarseness significantly increased in both right (P = 0.042) and left (P = 0.010) recurrent laryngeal nerve lymph nodes dissection cohorts compared by the reservation cohorts, with incidence rates of 5.9% and 6.7%, respectively.
Conclusions
The metastasis rates of subcarinal, right and left recurrent laryngeal nerve lymph nodes in thoracic esophageal squamous cell carcinoma were all over 10%. The dissection of subcarinal lymph nodes does not increase postoperative complications risk, while recurrent laryngeal nerve lymph nodes dissection significantly increases the incidence of hoarseness. Thus, lymph node dissection of subcarinal lymph nodes should be conducted routinely, while recurrent laryngeal nerve lymph nodes dissection may be selectively performed in specific patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal carcinoma has high morbidity and mortality, with over 500,000 new cases and nearly 450,000 cancer-related deaths worldwide(Bray et al. 2024). At present, esophagectomy with lymph node dissection is still the main therapeutic method for esophageal carcinoma patients without systemic metastases, but the postoperative survival prognosis is still poor(Darling 2009; Lundberg et al. 2022), which is related to its high recurrence and metastasis rate. The lymph node metastasis is a crucial manner for the spread of esophageal carcinoma and a major contributor to the recurrence of tumor after surgery. The evaluation of lymph node metastasis status is also essential for prognostic prediction and postoperative treatment strategy selection in esophageal carcinoma patients. Thus, it is crucial to explore the lymph node metastatic pattern of tumor in order to investigate appropriate strategies for lymph node dissection in esophageal carcinoma.
Esophageal squamous cell carcinoma is the most prevalent pathological type(Huang and Yu 2018), which can be further classified into cervical, thoracic, and abdominal esophageal carcinoma based on the location of tumor with thoracic one being the main type. Unfortunately, the pattern and risk factors of lymph node metastasis in thoracic esophageal squamous cell carcinoma have not been fully elucidated. The subcarinal, right and left recurrent laryngeal nerve lymph nodes are common sites for lymph node metastasis in esophageal carcinoma. As regional lymph nodes of the esophagus, the dissection of subcarinal lymph nodes is often considered necessary(Ma et al. 2013; Shang et al. 2020). However, it was reported that in cases of early stage and upper thoracic esophageal carcinoma, subcarinal lymph node resection may not be required(Li et al. 2010). Recurrent laryngeal nerve lymph node resection is usually considered a routine procedure for lymph node dissection in thoracic esophageal carcinoma. Hong et al(Hong et al. 2022) reported the significance of bilateral dissection of recurrent laryngeal nerve lymph nodes for accurate nodal staging and reducing regional lymph node metastasis in early-stage esophageal squamous cell carcinoma. Zhang et al(Zhang et al. 2022) also revealed that the incidence of recurrent laryngeal nerve lymph nodes metastasis is not rare in esophageal squamous cell carcinoma, and recurrent laryngeal nerve lymph node dissection is considered to be beneficial for the improvement of long-term survival. However, it is noteworthy that the literature also highlighted the possibility of a rise in postoperative complications following bilateral recurrent laryngeal nerve lymph node dissection, and the authors believed that certain subgroup patients may benefit better from unilateral dissection. So far, there has been no consensus on the optimal strategy for subcarinal and recurrent laryngeal nerve lymph nodes dissection for thoracic esophageal squamous cell carcinoma. Therefore, exploring the patterns and risk factors of these specific lymph nodes metastasis is particularly crucial.
This study examined patients with thoracic esophageal squamous cell carcinoma who underwent esophagectomy with lymph node dissection, retrospectively. We analyzed the incidence rate and risk factors of subcarinal, right and left recurrent laryngeal nerve lymph nodes metastasis and assessed the postoperative complications rate in dissection of these lymph nodes, and further visualized the results. This research aimed to provide a basis for adequate lymph node dissection strategies for thoracic esophageal squamous cell carcinoma.
Patients and methods
Patient population
The medical records of 503 patients receiving radical surgery for thoracic esophageal squamous cell carcinoma between December 2020 and April 2024 in the First Affiliated Hospital of Xiamen University were retrospectively collected. We excluded patients receiving neoadjuvant therapy or combining with other malignancies.
All patients in our study underwent preoperative clinical staging using chest, neck and abdominal enhanced CT, cranial enhanced MRI, whole-body bone single-photon emission computed tomography, endoscopic ultrasonography, and pathological biopsy. The positron emission tomography/computed tomography is an optional but not mandatory examination. Additionally, the diagnosis of postoperative hoarseness was based on clinical manifestations and laryngoscopy examination. Before resumption of diet, usually on the 7th to 14th day after surgery, if the patient still presented with hoarseness, we performed routine laryngoscopy to determine the presence of vocal cord paralysis.
Surgical procedures and pathological assessment
All included thoracic esophageal squamous cell carcinoma patients received esophagectomy via McKeown, Ivor-Lewis or Sweet surgical procedures with standard two-field lymphadenectomy. The pathological stage of esophageal squamous cell carcinoma was based on the eighth edition of American Joint Committee on Cancer tumor-node-metastasis staging criteria(Rice et al. 2016, 2017).
Statistical analysis
Statistical analyses were performed with SPSS 25.0 statistical software (SPSS Inc, Chicago, IL, USA). Continuous data were presented as means ± standard deviation. The chi-square test or Fisher exact probability test was conducted to compare categorical variables. Multivariate logistic regression analysis was applied to identify risk factors for subcarinal, right and left recurrent laryngeal nerve lymph nodes metastasis in thoracic esophageal squamous cell carcinoma. All tests were two-sided, and a P value less than 0.05 was considered to be statistically significant.
Results
Baseline characteristics of thoracic esophageal squamous cell carcinoma patients
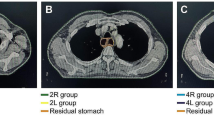
As shown in Table 1, a total of 503 thoracic esophageal squamous carcinoma patients who underwent esophagectomy were enrolled in our research, including 384 men and 119 women, with a median age of 62.4 years at the time of surgery (range: 41-83 years). Among all the patients, there were 468, 340, and 284 patients undergoing resection of subcarinal, right and left recurrent laryngeal nerve lymph nodes, respectively. The total numbers of subcarinal, right and left recurrent laryngeal nerve lymph nodes removed were 1861, 899, and 690, respectively. On average, each patient was resected with 3.98 subcarinal lymph nodes (range: 1–21), 2.64 right recurrent laryngeal nerve lymph nodes (range: 1–18), and 2.43 left recurrent laryngeal nerve lymph nodes (range: 1–13), respectively. As shown in Fig. 1, there were 48 (10.3%), 35 (10.3%), and 31 (10.9%) patients had metastatic subcarinal, right and left recurrent laryngeal nerve lymph nodes, respectively.
Correlation between subcarinal, right and left recurrent laryngeal lymph nodes metastasis and clinicopathological characteristics
As shown in Table 2, subcarinal lymph node metastasis was correlated with worse tumor differentiation (P = 0.025), higher pathological T stage (P = 0.003), presence of lymphovascular invasion (P < 0.001), and presence of nerve invasion (P = 0.001). In addition, tumor size was a potential important risk factor in subcarinal lymph node metastasis, although the difference was not statistically significant (P = 0.058). We also found that the incidence of subcarinal lymph node metastasis in the middle and lower thoracic esophageal squamous cell carcinoma was higher than that in the upper thoracic segment despite the difference was not statistically significant.
Right recurrent laryngeal nerve lymph node metastasis was related to the tumor location of upper and middle thoracic segment (P = 0.013), larger tumor size (P = 0.034), worse tumor differentiation (P = 0.026), higher pathological T stage (P = 0.048), and presence of lymphovascular invasion (P = 0.027). In addition, left recurrent laryngeal nerve lymph node metastasis was associated with younger age (P = 0.029) and presence of lymphovascular invasion (P = 0.012). However, there was no significant correlation between left recurrent laryngeal nerve lymph node metastasis and tumor location (P = 0.450), tumor size (P = 0.444), tumor differentiation (P = 0.483), pathological T stage (P = 0.589), and nerve invasion (P = 0.303). As shown in Fig. 2, we further analyzed and visualized the subcarinal, right and left recurrent laryngeal nerve, periesophageal and perigastric lymph nodes metastasis rates based on different tumor locations, tumor sizes, tumor differentiation statuses, pathological T stages, and lymphovascular invasion statuses.
Metastasis rates of right and left recurrent laryngeal nerve, subcarinal, periesophageal, and perigastric lymph nodes in thoracic esophageal squamous cell carcinoma based on different tumor locations (A-C), tumor sizes (D-E), tumor differentiations (F-H), pathological T stages (J-K), and lymphovascular invasion status (L-M)
Independent risk factors for subcarinal, right and left recurrent laryngeal lymph nodes metastasis
As shown in Table 3, the multivariate logistic regression analysis revealed that presence of lymphovascular invasion was the potential significant predictors for subcarinal lymph node metastasis (P < 0.001). The tumor location was an independent predictor for right recurrent laryngeal nerve lymph node metastasis (P = 0.013). For left recurrent laryngeal nerve lymph node metastasis, younger age (P = 0.020) and presence of lymphovascular invasion (P = 0.009) were significant risk factors in thoracic esophageal squamous cell carcinoma.
Correlation between subcarinal, right and left recurrent laryngeal lymph nodes metastasis and postoperative complications
As shown in Table 4, pulmonary infection is the most common postoperative complication in patients with dissection of subcarinal, right and left recurrent laryngeal lymph nodes. There was no significant difference in the incidence of anastomotic leakage (P = 0.872), pulmonary infection (P = 0.139), chylothorax (P = 0.702), and hoarseness (P = 0.179) between the subcarinal lymph node dissection cohort and the reservation cohort. In addition, the incidence of hoarseness significantly increased in both the right (P = 0.042) and left (P = 0.010) recurrent laryngeal nerve lymph nodes dissection cohorts compared by the reservation cohorts, with incidence rates of 5.9% and 6.7%, respectively.
Disscusion
The lymph node metastasis status is crucial for survival prediction and providing guidance for postoperative adjuvant therapy strategies in esophageal carcinoma patients(Feng et al. 2022; Wu et al. 2022). The abundant lymphatic drainage and anatomical location of the esophagus lead to the widespread distribution of lymph node metastasis in esophageal carcinoma from the neck to the abdomen. Among them, the subcarinal, right and left recurrent laryngeal nerve lymph nodes are important sites for lymph node metastasis, and dissection of these lymph nodes may potentially raise the risk of pulmonary infection(Ozaki et al. 2022; Xu et al. 2022), hoarseness(Koyanagi et al. 2015; Sato et al. 2016), chylothorax(Yang et al. 2020), and other postoperative complications. Therefore, exploring the lymph node metastasis pattern of esophageal carcinoma is necessary, which helps to carry out appropriate lymph node dissection procedure.
There is a high incidence of subcarinal, right and left recurrent laryngeal nerve lymph nodes metastasis in thoracic esophageal squamous cell carcinoma patients, with incidence rates of 10.4-17.5%(Li et al. 2010; Shang et al. 2020)、15.5-20.4%(Liu et al. 2019; Yuan and Mao 2023)、13.6-15.1%(Liu et al. 2019; Tachimori 2017), respectively. In our research, we found that the metastasis rates in these three stations of lymph nodes are 10.3%, 10.3%, and 10.9%, respectively, which is consistent with previous literature reports. The differences in lymph node metastasis rates reported in various literatures may be due to differences in baseline clinicopathological characteristics among the included population. For instance, the proportion of cases with higher pathological T stage in Shang et al’s study(Shang et al. 2020) was higher than that in our research. Therefore, further exploration of the correlation between the incidence of specific lymph node metastasis and the clinicopathological characteristics of thoracic esophageal squamous cell carcinoma patients can help identify potential risk factors affecting lymph node metastasis. Through the chi-square test and multivariate logistic regression analysis, we found that lymphovascular invasion is an independent predictor for subcarinal lymph node metastasis, while tumor location is an independent risk factor for right recurrent laryngeal nerve lymph node metastasis. This result suggested that the invasiveness of tumor, rather than tumor location, has a more significant effect on subcarinal lymph node metastasis, while for right recurrent laryngeal nerve lymph node metastasis, it may be the opposite. Shang et al(Shang et al. 2020) also found that the incidence rate of subcarinal lymph node metastasis in esophageal squamous cell carcinoma is not correlated with tumor location, but significantly correlated with depth of invasion and length of tumor. Li et al(Li et al. 2020) reported that right recurrent laryngeal nerve lymph node metastasis is related with tumor depth and tumor location. In our study, the incidence of right recurrent laryngeal nerve lymph node metastasis in upper and middle thoracic esophageal squamous cell carcinoma was as high as 13.0%, much higher than the rate of 2.3% in lower thoracic tumor. This suggests that patients with upper and middle thoracic esophageal squamous cell carcinoma need a more thorough dissection of the right recurrent laryngeal nerve lymph nodes. In addition, we found that age and lymphovascular invasion are independent risk factors for left recurrent laryngeal nerve lymph node metastasis. Sehitogullari et al(Sehitogullari et al. 2011) also found that local lymph node metastasis is more common in young esophageal carcinoma patients. However, Zhang et al(Zhang et al. 2018) believed that age is not an important risk factor for lymph node metastasis in thoracic esophageal squamous cell carcinoma. It was unclear whether our findings are due to differences in lymphatic drainage between young patients and older patients, or biases caused by insufficient sample size, which require further research to verify. Anyway, this suggests that for young tumor patients, the dissection of left recurrent laryngeal nerve lymph nodes may need to be more thorough.
Dissection of the subcarinal, right, and left recurrent laryngeal nerve lymph nodes will unavoidably result in tissue damage and lengthen the duration of the surgical procedure. However, it is debatable if this causes a significant rise in postoperative complications in cases of esophageal carcinoma. Xu et al(Xu et al. 2022) revealed that the incidence of postoperative pulmonary infection and anastomotic leakage in esophageal carcinoma patients undergoing subcarinal lymph node dissection is significantly higher than that in reservation group patients. Whereas, Shang et al(Shang et al. 2020) reported that subcarinal lymph node dissection does not increase the risk of postoperative pulmonary infection, anastomotic leakage, and chylothorax. Our study also found that there was no significant difference in the incidence of anastomotic leakage, pulmonary infection, chylothorax, and hoarseness between the subcarinal lymph node dissection group and the reservation group. We believed that careful surgical techniques and adequate perioperative treatment strategies can effectively prevent postoperative complications. However, it was worth noting that the incidence of postoperative hoarseness significantly increases in the right and left recurrent laryngeal nerve lymph node dissection groups compared to the reservation groups in our study. Currently, many novel tools and surgical techniques have been proposed for intraoperative protection of the recurrent laryngeal nerves. Studies have shown that intraoperative neural monitor is an effective tool for reducing the incidence of recurrent laryngeal nerve paralysis and hoarseness in esophagectomy(Lee et al. 2024; Wang et al. 2021). The hollow-out method, as a novel and safe technique for dissection of recurrent laryngeal nerve lymph nodes, has been reported to significantly reduce the incidence of hoarseness after esophagectomy(Chen et al. 2020). Oshikiri et al(Oshikiri and Goto et al., 2021) found that Robot-assisted minimally invasive esophagectomy can effectively reduce the incidence of left recurrent laryngeal nerve paralysis compared to conventional minimally invasive esophagectomy. The use of energy devices such as ultrasonic knives and electric hooks may cause thermal damage to the nerve(Owaki et al. 2002). Therefore, attention should be paid to sufficient distance from the recurrent laryngeal nerve and appropriate activation time when using these devices. In our research, protective measures for the recurrent laryngeal nerve included careful use of energy devices to avoid thermal damage, the use of hollow-out method and robot-assisted operating systems for dissection of the recurrent laryngeal nerve lymph nodes. Nonetheless, Dissection of recurrent laryngeal nerve lymph nodes potentially increases the occurrence of intraoperative recurrent laryngeal nerve injury, resulting in a postoperative hoarseness rate of over 20%(Duan et al. 2021; Park et al. 2016). Oshikiri et al(Oshikiri and Takiguchi et al., 2021) further reported that there is a strong correlation between recurrent laryngeal nerve paralysis and pneumonia, and preventing recurrent laryngeal nerve paralysis may reduce the incidence of pneumonia, although we did not find that dissection of the recurrent laryngeal nerve lymph nodes increases the incidence of postoperative pulmonary infection in our research. At present, there are no principles for which regions of the lymph nodes have to be dissected in guidelines. There is still controversy over whether to perform dissection for the recurrent laryngeal nerve lymph nodes. Several researches revealed that the extent of lymph node resection is not related to the prognosis of patients undergoing esophagectomy(Koen et al. 2014; Shridhar et al. 2013). Bilateral recurrent laryngeal nerve lymph nodes dissection has been reported to significantly increase postoperative complications, and specific subgroups of patients may only require unilateral lymph nodes dissection(Zhang et al. 2022). However, Chao et al(Chao et al. 2020) pointed out that an extended lymphadenectomy is safe and beneficial, and bilateral recurrent laryngeal nerve lymph nodes dissection can reduce local recurrence of tumor. Therefore, extra caution should be taken to prevent nerve damage during recurrent laryngeal nerve lymph nodes dissection, and personalized decision-making regarding dissection of these lymph nodes during esophagectomy may be feasible for tumor with mild primary lesions in the lower thoracic segment, particularly for the right recurrent laryngeal nerve lymph nodes.
Our study systematically reviewed and visualized the metastatic patterns of subcarinal, right and left recurrent laryngeal nerve lymph nodes in thoracic esophageal squamous cell carcinoma. However, our research also had some limitations. Firstly, the bias caused by retrospective research was inevitable. Secondly, the sample size for some groups such as cases with well differentiated and pathological T4 stage tumor was insufficient. Thirdly, some cases in our cohort did not undergo subcarinal or recurrent laryngeal nerve lymph nodes dissection, resulting in the inability to assess the lymph node metastasis status of these patients. Finally, this study did not conduct a survival prognostic analysis.
Conclusions
The metastasis rates of subcarinal, right and left recurrent laryngeal nerve lymph nodes in thoracic esophageal squamous cell carcinoma are all over 10%. The presence of lymphovascular invasion and location of tumor in the middle thoracic segment are independent risk factors for subcarinal and right recurrent laryngeal nerve lymph nodes metastasis, respectively, while age and lymphovascular invasion are independent predictors for left recurrent laryngeal nerve lymph node metastasis. The dissection of subcarinal lymph nodes does not increase postoperative complications risk, while recurrent laryngeal nerve lymph nodes dissection significantly increases the incidence of hoarseness. Therefore, lymph node dissection of subcarinal lymph nodes should be performed routinely, while recurrent laryngeal nerve lymph nodes dissection may be selectively performed.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A (2024) Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 74(3):229–263. https://doi.org/10.3322/caac.21834
Chao YK, Chiu CH, Liu YH (2020) Safety and oncological efficacy of bilateral recurrent laryngeal nerve lymph-node dissection after neoadjuvant chemoradiotherapy in esophageal squamous cell carcinoma: a propensity-matched analysis. Esophagus 17(1):33–40. https://doi.org/10.1007/s10388-019-00688-7
Chen WS, Zhu LH, Li WJ, Tu PJ, Huang JY, You PL, Pan XJ (2020) Novel technique for lymphadenectomy along left recurrent laryngeal nerve during thoracoscopic esophagectomy. World J Gastroenterol 26(12):1340–1351. https://doi.org/10.3748/wjg.v26.i12.1340
Darling G (2009) The role of lymphadenectomy in esophageal cancer. J Surg Oncol 99(4):189–193. https://doi.org/10.1002/jso.21209
Duan X, Yue J, Chen C, Gong L, Ma Z, Shang X, Yu Z, Jiang H (2021) Lymph node dissection around left recurrent laryngeal nerve: robot-assisted vs. video-assisted McKeown esophagectomy for esophageal squamous cell carcinoma. Surg Endosc 35(11):6108–6116. https://doi.org/10.1007/s00464-020-08105-2
Feng SK, Liu XB, Xing WQ, Liu Y, Chen PN, Jiang D, Sun HB (2022) Adjuvant chemotherapy for node-positive esophageal squamous cell Carcinoma improves survival. Ann Thorac Surg 114(4):1205–1213. https://doi.org/10.1016/j.athoracsur.2021.08.068
Hong TH, Kim HK, Lee G, Shin S, Cho JH, Choi YS, Zo JI, Shim YM (2022) Role of recurrent laryngeal nerve lymph node dissection in surgery of early-stage esophageal squamous cell carcinoma. Ann Surg Oncol 29(1):627–639. https://doi.org/10.1245/s10434-021-10757-w
Huang FL, Yu SJ (2018) Esophageal cancer: risk factors, genetic association, and treatment. Asian J Surg 41(3):210–215. https://doi.org/10.1016/j.asjsur.2016.10.005
Koen TA, Shapiro J, Looman CW, van Hagen P, Steyerberg EW, van der Gaast A, van Berge HM, Wijnhoven BP, van Lanschot JJ, Hulshof MC, van Laarhoven HW, Nieuwenhuijzen GA, Hospers GA, Bonenkamp JJ, Cuesta MA, Blaisse RJ, Busch OR, Ten KF, Creemers GJ, Punt CJ, Plukker JT, Verheul HM, van Dekken H, van der Sangen MJ, Rozema T, Biermann K, Beukema JC, Piet AH, van Rij CM, Reinders JG, Tilanus HW (2014) Lymph node retrieval during esophagectomy with and without neoadjuvant chemoradiotherapy: prognostic and therapeutic impact on survival. Ann Surg 260(5):786–792. https://doi.org/10.1097/SLA.0000000000000965
Koyanagi K, Igaki H, Iwabu J, Ochiai H, Tachimori Y (2015) Recurrent laryngeal nerve paralysis after Esophagectomy: respiratory complications and role of nerve Reconstruction. Tohoku J Exp Med 237(1):1–8. https://doi.org/10.1620/tjem.237.1
Lee S, Fujiwara Y, Gyobu K, Tamura T, Toyokawa T, Miki Y, Yoshii M, Kasashiima H, Fukuoka T, Shibutani M, Osugi H, Maeda K (2024) Evaluation of intraoperative neural monitoring during thoracoscopic surgery for Esophageal Cancer. Anticancer Res 44(1):157–166. https://doi.org/10.21873/anticanres.16798
Li YF, Hu Y, Lin P, Zheng B, Luo KJ, Yang H, Yang HX, Wang JY, Rong TH, Fu JH (2010) [Significance of subcarinal lymph node selective dissection in thoracic esophageal carcinoma]. Zhonghua Yi Xue Za Zhi 90(37):2636–2639
Li ZX, Li XD, Liu XB, Xing WQ, Sun HB, Wang ZF, Zhang RX, Li Y (2020) Clinical evaluation of right recurrent laryngeal nerve nodes in thoracic esophageal squamous cell carcinoma. J Thorac Dis 12(7):3622–3630. https://doi.org/10.21037/jtd-20-774
Liu Y, Zou ZQ, Xiao J, Zhang M, Yuan L, Zhao XG (2019) A nomogram prediction model for recurrent laryngeal nerve lymph node metastasis in thoracic oesophageal squamous cell carcinoma. J Thorac Dis 11(7):2868–2877. https://doi.org/10.21037/jtd.2019.06.46
Lundberg E, Lagergren P, Mattsson F, Lagergren J (2022) Life Expectancy in survivors of Esophageal Cancer compared with the background Population. Ann Surg Oncol 29(5):2805–2811. https://doi.org/10.1245/s10434-022-11416-4
Ma H, Li Y, Ding Z, Liu X, Xu J, Qin J (2013) The clinical significance of subcarinal lymph node dissection in the radical resection of oesophageal cancer. Interact Cardiovasc Thorac Surg 16(6):839–843. https://doi.org/10.1093/icvts/ivt070
Oshikiri T, Goto H, Horikawa M, Urakawa N, Hasegawa H, Kanaji S, Yamashita K, Matsuda T, Nakamura T, Kakeji Y (2021a) Incidence of recurrent laryngeal nerve Palsy in Robot-assisted Versus Conventional minimally invasive McKeown Esophagectomy in Prone position: a propensity score-matched study. Ann Surg Oncol 28(12):7249–7257. https://doi.org/10.1245/s10434-021-10123-w
Oshikiri T, Takiguchi G, Hasegawa H, Yamamoto M, Kanaji S, Yamashita K, Matsuda T, Nakamura T, Suzuki S, Kakeji Y (2021b) Postoperative recurrent laryngeal nerve palsy is associated with pneumonia in minimally invasive esophagectomy for esophageal cancer. Surg Endosc 35(2):837–844. https://doi.org/10.1007/s00464-020-07455-1
Owaki T, Nakano S, Arimura K, Aikou T (2002) The ultrasonic coagulating and cutting system injures nerve function. Endoscopy 34(7):575–579. https://doi.org/10.1055/s-2002-33221
Ozaki A, Mine S, Yoshino K, Fujiwara D, Nasu M, Hashiguchi T, Hashimoto T, Kajiyama Y, Tsurumaru M, Arakawa A (2022) Outcomes of esophagectomy for patients with esophageal squamous cell carcinoma accompanied by recurrent laryngeal nerve palsy at diagnosis. Esophagus 19(2):233–239. https://doi.org/10.1007/s10388-021-00890-6
Park SY, Kim DJ, Yu WS, Jung HS (2016) Robot-assisted thoracoscopic esophagectomy with extensive mediastinal lymphadenectomy: experience with 114 consecutive patients with intrathoracic esophageal cancer. Dis Esophagus 29(4):326–332. https://doi.org/10.1111/dote.12335
Rice TW, Ishwaran H, Hofstetter WL, Kelsen DP, Apperson-Hansen C, Blackstone EH (2016) Recommendations for pathologic staging (pTNM) of cancer of the esophagus and esophagogastric junction for the 8th edition AJCC/UICC staging manuals. Dis Esophagus 29(8):897–905. https://doi.org/10.1111/dote.12533
Rice TW, Ishwaran H, Ferguson MK, Blackstone EH, Goldstraw P (2017) Cancer of the Esophagus and Esophagogastric Junction: an Eighth Edition staging primer. J Thorac Oncol 12(1):36–42. https://doi.org/10.1016/j.jtho.2016.10.016
Sato Y, Kosugi S, Aizawa N, Ishikawa T, Kano Y, Ichikawa H, Hanyu T, Hirashima K, Bamba T, Wakai T (2016) Risk factors and clinical outcomes of recurrent laryngeal nerve paralysis after esophagectomy for thoracic esophageal carcinoma. World J Surg 40(1):129–136. https://doi.org/10.1007/s00268-015-3261-8
Sehitogullari A, Cikman O, Sayir F, Cobanoglu U, Demir C, Demir H (2011) Impact of lymph node metastases in esophageal carcinoma patients is independent of patient age. Asian Pac J Cancer Prev 12(3):599–603
Shang QX, Wang YC, Yang YS, Hu WP, Chen LQ (2020) Pattern of subcarinal lymph node metastasis and dissection strategy for thoracic esophageal cancer. J Thorac Dis 12(10):5667–5677. https://doi.org/10.21037/jtd-20-1776
Shridhar R, Hoffe SE, Almhanna K, Weber JM, Chuong MD, Karl RC, Meredith K (2013) Lymph node harvest in esophageal cancer after neoadjuvant chemoradiotherapy. Ann Surg Oncol 20(9):3038–3043. https://doi.org/10.1245/s10434-013-2988-4
Tachimori Y (2017) Pattern of lymph node metastases of squamous cell esophageal cancer based on the anatomical lymphatic drainage system: efficacy of lymph node dissection according to tumor location. J Thorac Dis 9(Suppl 8):S724–S730. https://doi.org/10.21037/jtd.2017.06.19
Wang X, Guo H, Hu Q, Ying Y, Chen B (2021) Efficacy of intraoperative recurrent laryngeal nerve monitoring during Thoracoscopic Esophagectomy for Esophageal Cancer: a systematic review and Meta-analysis. Front Surg 8:773579. https://doi.org/10.3389/fsurg.2021.773579
Wu LL, Zhong JD, Zhu JL, Kang L, Huang YY, Lin P, Long H, Zhang LJ, Ma QL, Qiu LH, Ma GW (2022) Postoperative survival effect of the number of examined lymph nodes on esophageal squamous cell carcinoma with pathological stage T1-3N0M0. BMC Cancer 22(1):118. https://doi.org/10.1186/s12885-022-09207-x
Xu B, Chen H, Zhang Q, Chen P, Liu Q, Chen M (2022) Value of subcarinal lymph node dissection in esophageal cancer surgery: a case-control study. Med (Baltim) 101(43):e31593. https://doi.org/10.1097/MD.0000000000031593
Yang YH, Park SY, Kim DJ (2020) Chyle Leakage after Esophageal Cancer surgery. Korean J Thorac Cardiovasc Surg 53(4):191–199. https://doi.org/10.5090/kjtcs.2020.53.4.191
Yuan LG, Mao YS (2023) [Characteristics of lymph node metastasis of right recurrent laryngeal nerve in thoracic esophageal squamous cell carcinoma]. Zhonghua Zhong Liu Za Zhi 45(6):508–513. https://doi.org/10.3760/cma.j.cn112152-20210820-00631
Zhang J, Liu Y, Che F, Luo Y, Huang W, Heng X, Li B (2018) Pattern of lymph node metastasis in thoracic esophageal squamous cell carcinoma with poor differentiation. Mol Clin Oncol 8(6):760–766. https://doi.org/10.3892/mco.2018.1606
Zhang S, Liu Q, Li B, Jia M, Cai X, Yang W, Liao S, Wu Z, Cheng C, Fu J (2022) Clinical significance and outcomes of bilateral and unilateral recurrent laryngeal nerve lymph node dissection in esophageal squamous cell carcinoma: a large-scale retrospective cohort study. Cancer Med 11(7):1617–1629. https://doi.org/10.1002/cam4.4399
Acknowledgements
This study was supported by Natural Science Foundation of Fujian Province (No. 2022J05301 and No.2021J05284), and Xiamen Municipal Bureau of Science and Technology (No. 3502Z20214ZD3011).
Funding
This study was supported by Natural Science Foundation of Fujian Province (No. 2022J05301 and No.2021J05284), and Xiamen Municipal Bureau of Science and Technology (No. 3502Z20214ZD3011).
Author information
Authors and Affiliations
Contributions
Guanzhi Ye: Data curation; Investigation; methodology; writing-original draft; writing-review and editing. Gaojian Pan: Data curation; methodology; validation; visualization. Xiaolei Zhu: Formal analysis; resources. Ning Li: Investigation. Hongming Liu: Visualization. Guojun Geng: Data curation; validation; project administration. Jie Jiang: Conceptualization; supervision.All authors have read and agreed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Xiamen University on 27 March 2024 (protocol number: XMYY-2024KYSB020).
Consent to participate
Due to the retrospective character of this analysis and the approval by the Ethics Committee of the First Affiliated Hospital of Xiamen University, informed consent was not required.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ye, G., Pan, G., Zhu, X. et al. Metastatic patterns of subcarinal, right and left recurrent laryngeal nerve lymph nodes in thoracic esophageal squamous cell carcinoma without neoadjuvant therapy. J Cancer Res Clin Oncol 150, 387 (2024). https://doi.org/10.1007/s00432-024-05911-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05911-2