Abstract
Purpose
Leukemia-associated fusion genes are closely related to the occurrence, development, diagnosis, and treatment of leukemia. DNA microarrays and second-generation sequencing have discovered multiple B-ALL fusion genes. We identified a novel MEF2C::SS18L1 fusion gene in a child diagnosed with B-ALL. This study investigates the oncogenicity and prognosis of this fusion gene in B-ALL.
Methods
A child with B-ALL who has a MEF2C::SS18L1 fusion is reported as a newly discovered case. Compared the breakpoints, structural domains, clinical phenotypes, and differential expression genes of MEF2C::SS18L1 and MEF2D::SS18.Using “ONCOFUSE” software, the carcinogenicity of MEF2C::SS18L1 is predicted. Using whole transcriptome sequencing, we analyze the breakpoints and the secondary structure of the fusion protein. Further, we compared the structures, differentially expressed genes, and clinical phenotypes of MEF2D and MEF2C fusion genes by DESeq, GO functional enrichment, and flow cytometry immunophenotyping analysis.
Results
Whole transcriptome sequencing identified a MEF2C::SS18L1 fusion transcript in a 3-year-old child with B-ALL. The MADS box, MEF structural domain, HJURP_C structural domain, and TAD I structural domain of MEF2C, and the QPGY structural domain of SS18L1, make up the fusion protein. “Oncofuse” found a 0.99 Bayesian probability that the fusion gene drives cancer. The breakpoint positions, fusion protein secondary structures, differentially expressed genes, and clinical characteristics of this patient were identical to those with MEF2D::SS18 fusion gene.
Conclusion
We identified a novel MEF2C::SS18L1 fusion gene in childhood ALL, which shares similar structural and clinical characteristics with MEF2D::SS18. Further studies with more samples should be conducted in future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute lymphocytic leukemia (ALL), a common malignancy in children, often arises from interactions between exogenous (e.g., environmental exposure) or endogenous (e.g., genetic susceptibility) factors. Usually, genetic mutations may lead to transformation of lymphoid progenitor cells (Kuiper et al. 2007). According to the immunophenotype of tumor cells, ALL is divided into acute B-lymphocytic leukemia (B-cell precursor acute lymphoblastic leukemia, B-ALL) and acute T-lymphocytic leukemia (T-cell precursor acute lymphoblastic leukemia, T-ALL) (Arber et al. 2016).
About 75% of B-ALL patients exhibit abnormal chromosomal numbers or translocations (Mullighan 2012), which can generate fusion genes, including ETV6::RUNX1, TCF3::PBX1, BCR::ABL1, MLL-related fusion genes, etc. (Harrison and Foroni 2002; Onciu 2009). There are growing evidence suggesting that gene fusion is initial event in oncogenesis (Mitelman et al. 2007) and plays an important role in cases of aggressive cancer (Villanueva 2012). Early fusion interferes with the expression of hematopoietic-related genes and oncogenes, contributing to the development of B-ALL. In recent years, many new fusion genes have been detected in the development and relapse of B-ALL by DNA microarray and second-generation sequencing. These fusion genes are mainly involved in B-cell developmental processes such as cell cycle, apoptosis, proliferation, autophagy, and epigenetic regulation (Collins-Underwood and Mullighan 2010; Mullighan et al. 2007; Forero-Castro et al. 2016; Zakaria et al. 2017).
In our study, we describe a case with MEF2C::SS18L1, a novel fusion gene unprecedentedly detected in a 3-year-old boy diagnosed with B-ALL. We analyzed the oncogenicity of MEF2C::SS18L1 and its association with the prognosis of B-ALL. Our study sheds new light on the possible pathogenesis of B-ALL associated with MEF2C (myocyte enhancer factor 2C) fusion.
Materials and methods
Case
A 3-year-old child with primary B-ALL was included. Transcriptome analysis confirmed the presence of the MEF2C::SS18L1 fusion. Peripheral blood (PB) and bone marrow (BM) samples were collected from the patient for diagnosis and medical analysis. This study was approved by the Ethics Committee of the Children’s Hospital of Nanjing Medical University. The patient’s parents provided written informed consent to participate in this study.
Karyotyping and fluorescence in situ hybridization (FISH)
Conventional karyotyping was performed after short-term culture, and every 20 metaphase cells after G-binding were analyzed. Karyotypes were described according to the International System for Human Cytogenetic Nomenclature (ISCN 2016). FISH was carried out on every 500 interphase cells using the Vysis LSI JAK2 dual-color break-apart probe (Abbott Laboratories) according to the manufacturer’s recommendations.
Flow cytometry (FCM) immunophenotyping and fusion gene detection
Heparin-anticoagulated BM samples were used for the immunophenotyping. For each tube, at least 3 × 105 leucocytes were stained with the following monoclonal antibodies: CD34, CD117, CD10, CD19, CD20, CD79a, CD2, CD4, CD8, CD3, CD7, CD5, CD13, CD33, CD14, CD64, CD11b, HLA-DR, MPO, and CD45. Then, 2 × 104 target cells were obtained by the FACS Canto Plus flow cytometer (BD Biosciences). The immunophenotypes of abnormal juvenile cells were analyzed using the FACSDiva software (BD Biosciences). BM leucocytes were enriched using ACK lysis buffer, and total RNA was extracted with Trizol. Then 500 ng of RNA was transcripted into cDNA by random primers and Moloney Murine Leukemia Virus Reverse Transcriptase (Progema, Beijing). Based on qRT-PCR, a multi-fusion gene detection system, and the 43 Fusion Gene Screening Kit (Yuanqi Biopharmaceutical, Shanghai, China), was used to screen transcripts.
RNA sequencing (RNA-Seq) and fusion validation
Ribosomal RNA was removed from the total RNA by the Ribozero method and then subjected to cDNA synthesis. cDNA was used as a template to construct the library for sequencing. Whole messenger transcriptome sequencing was performed on the Illumina Hiseq X sequencing platform. Sequenced fragments were aligned with the UCSC hg19 reference genome by STAR software. FusionCatcher was used for gene fusion prediction. The downstream genes of the fusion gene were analyzed by variant effector prediction (VEP). The fusion gene was annotated in databases including Clinvar, dbSNP, 1000genome, genomeAD, ExAC, COSMIC, etc. RNA-Seq results were validated by RT-PCR, followed by Sanger sequencing.
Oncofuse to predict oncogenic potential
Oncofuse (http://www.unav.es/genetica/oncofuse.html) is employed to predict the oncogenic potential of fusion genes found by Next-Generation Sequencing in cancer cells. It is a post-processing step to validate in silico the predictions made by fusion detection software.The pipeline was executed by simply running a Java or Groovy script with some parameters on a standardized input file (all required packages were installed automatically via Groovy or Grape). The parameters are set based on features present in known oncogenic fusions. A complete list of features was shown in paper of Shugay et al. (Shugay et al. 2013). We provided IDs of fusion gene partners as well as locations of breakpoints (intron/exon ID and coordinate) within the major Refseq transcript of each gene.
Gene expression analysis
The quality of FastQ data for this patient was assessed by FastQC and controlled by Trim-Galore. Then the reads were mapped to the GRCh38 reference genome by Hisat2. The dataset GSE11504 was downloaded from the GEO, and gene expression data in children and adult bone marrows were collected. The dataset GSE11504 contained 25 cases of healthy children, adolescents and adults aged 2 months to 28 years. Since the gene expression in this dataset was detected by microarray, the batch effect was removed by the SVA package.
DEGs and enrichment analyses
The DEGs were calculated by the DESeq2 package according to | log2-fold-change |> 5 and adj. P-value < 1e-10. To pinpoint the DEGs induced by MEF2C::SS18L1 fusion, we constructed a protein–protein interaction network based on the STRING database, then filtered out the DEGs connected to MEF2C or SS18L1 for further analysis. The biological function of these DEGs was evaluated with GO analysis from the clusterProfiler package.
Results
Case presentation
This 3-year-old boy had suffered intermittent joint pain for about a month, which was self-relieving. Two weeks later, he was admitted to the hospital for persistent pain in the left hand joint. Blood testing showed a white blood cell count of 8.97 × 109/L, a hemoglobin level of 101 g/L, and a platelet count of 332 × 109/L. Morphologic examination of BM smears disclosed markedly active BM and lymphatic proliferation, with 93.0% of lymphocytes being primitive and juvenile (Fig. 1A). FCM revealed that about 81.0% of B lymphocytes in the BM were abnormally juvenile and positive for CD19, cCD79a, cCD22, and CD22 (Fig. 1B). The chromosomal karyotype was normal (Fig. 1C). FISH analysis showed negative results about MLL rearrangement, BCR/ABL fusion, ETV6/RUNX1 fusion, PDGFRB isolation, MYC disruption, and MEF2D disruption (Fig. 1D). Multiplex-nested RT-PCR, designed to amplify 43 fusion transcripts, was negative (Supplement Table 1). The copy number variation (CNV) assay did not detect large fragment deletions or duplications in IKZF1. MEF2C::SS18L1 fusion transcripts and PTPN11 mutation were detected by next-generation whole transcriptome sequencing. The child was diagnosed with B-ALL, initially stratified as low-risk, and treated with the CCCG-ALL2020 regimen with no significant adverse effects. MRD on day 19 was 12.41%, and the percentage of juvenile lymphocytes was 4.0%. Due to his poor response to the initial treatment, the risk was elevated to intermediate, according to CCCG ALL 2020. He was then given CAT chemotherapy, with MRD < 0.01% and the MEF2C::SS18L1 fusion gene turning negative on day 46, as well as a complete remission eventually achieved. The child is now on sequential chemotherapy.
Identification of MEF2C::SS18L1 fusion transcript by RNA-Seq
The primary BM sample was analyzed by RNA-Seq. We identified a novel MEF2C::SS18L1 fusion in B-ALL. RNA-Seq results indicated that the breakpoints were located in exon 6 of MEF2C on chromosome 5 and exon 5 of SS18L1 on chromosome 10 (Fig. 2A). The fusion protein consisted of a MADS box and a MEF domain, a HJURP_C structural domain, a TAD I structural domain in MEF2C, and the QPGY structural domain in SS18L1 (Fig. 2B).
MEF2C::SS18L1 fusion and comparison of its secondary structures with MEF2D::SS18 fusion protein. A RNA-Seq revealed breakpoints in exon 6 of MEF2C and exon 5 of SS18L1; B Schematic diagram of predicted secondary structure of MEF2C::SS18L1 fusion protein; C Comparison of MEF2C::SS18L1 and MEF2D::SS18 breakpoints
Predicted oncogenicity of MEF2C::SS18L1
We entered the breakpoint information of the MEF2C::SS18L1 fusion gene into "Oncofuse", and discovered that the fusion gene had a Bayesian probability of 0.99 of acting as an oncogenic driver (P < 0.05). The prediction results also demonstrate protein domains, respectively, retained in the 5’ fusion partner gene and the 3’ fusion partner gene (Table 1; Fig. 2B).
DEGs and GO annotations of MEF2C::SS18L1
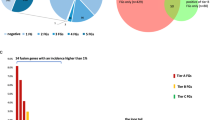
The DEGs between normal and B-ALL tissues were screened. We obtained 1782 up-regulated and 2429 down-regulated genes using the DESeq2 package, with thresholds of | log2-fold-change |> 5 and adj. P-value < 1e-10. The top 13 most significant DEGs (HOPX, NFATC2, HDAC9, RB1, SMARCE1, ATRX, ETS1, MYL3, TEAD4, CEBPA, TEAD2, KLF4, and SOX9) were shown on the volcano map (Fig. 3A). In order to obtain the DEGs induced by the MEF2C::SS18L1 fusion, we identified 81 DEGs associated with MEF2C or SS18L1 through the STRING database, including 32 down-regulated and 49 up-regulated, as shown in PPI maps (Fig. 3B-C). In GO enrichment analysis, these DEGs were associated with heart morphogenesis (GO:0003007), cell fate commitment (GO:0045165), Notch signaling pathway (GO:0007219), muscle tissue development (GO:0060537), muscle cell differentiation (GO:0042692), chromatin remodeling (GO:0006338), regulation of hemopoiesis (GO:1,903,706), and regulation of myeloid cell differentiation (GO:0045637) (Fig. 3D).
Discussion
In this study, we identified a novel MEF2C::SS18L1 fusion gene associated with childhood B-ALL. After 19 days of treatment, this three-year-old patient’s MRD was still 12.4%, and the percentage of juvenile lymphocytes was 4.0%. Response to early treatment (induction therapy) remains the most reliable independent factor for predicting the prognosis of childhood ALL, which is assessed internationally based on the prednisone sensitivity test (Conter et al. 2010). MRD is the strongest predictor for the long-term survival of ALL patients (Schultz et al. 2007). A retrospective analysis found that D19 MRD ≥ 1% during the early induction phase of chemotherapy was an independent risk factor for poor prognosis (Yu et al. 2020). The high MRD in the present case suggests that the new fusion gene may affect patients’ responses to treatments. Thus, we further analyzed the fusion gene with “Oncofuse”, finding that MEF2C::SS18L1 is a "driver" of ALL.
Currently, MEF2C::SS18 fusion has been reported in microsecretory adenocarcinoma (MSA), a novel subtype of salivary gland adenocarcinoma that tends to be less malignant or appears as an inert salivary gland tumor (Bishop et al. 2019). MSA has characteristic histologic and immunophenotypic features and most of MSA patients have MEF2C::SS18 fusion, which was identified as a typical marker in this disease. In a clinical study conducted by Justin A. Bishop et al., a total of 24 MSA cases were collected, and MEF2C::SS18 fusion was confirmed in 21 of them. The tumors exhibited consistent histologic features including: (1) microcystic ducts, (2) flattened intercalated duct-like cells, (3) monochromatic oval hyperpigmented nuclei, (4) abundant basophilic luminal secretions, (5) fibromuscular-like stroma, and (6) subtle infiltration of the periphery. These tumors were uniformly positive for S100 (24 of 24) and p63 (24 of 24) (Bishop et al. 2021). SS18 (SS18 subunit of BAF chromatin remodeling complex) is a gene with similar structure of SS18L1 (SS18L1 subunit of BAF chromatin remodeling complex). An analysis of SS18 and SS18L1 sequences has revealed that both proteins contain an SS18 N-terminal (SNH) domain and a QPGY domain (Kato et al. 2002). Therefore, it is reasonable to infer that there is similarity between MEF2C::SS18 and MEF2C::SS18L1. Although there is not any reports of MEF2C::SS18L1 in hematologic tumors at present, the presence of recurrent MEF2C::SS18 fusions in MSA suggests the importance and specificity of this fusion in pathogenesis of malignant tumor. Notably, all of these 24 MSA cases exhibited S100 and P63 positivity, which has also been reported to be associated with the development and prognosis of hematologic neoplasms. In a retrospective cohort study, a team of researchers evaluated the levels of inflammatory markers such as S100 protein in 128 children with pre-B ALL. They concluded that S100 could be used as a biomarker to assess ALL prognosis (Brix et al. 2023). Meanwhile, P63, as a member of the P53 family, shows different expression and function in different types and stages of leukemia (Xie and Xie 2013; Pruneri et al. 2005). However, whether S100 and P63 positivity are equally present in children with MEF2C::SS18L1 positive ALL requires further validation.
What role does the MEF2C::SS18L1 play in ALL? Growing evidence suggests that MEF2C is essential for the normal hematopoietic system, particularly the production of immature and mature lymph-like cells (Schüler et al. 2008). Integrated MEF2C and ectopic MEF2C expression are found in 20% of patients with acute myeloid leukemia (AML) (Schwieger et al. 2009). In a study based on gene expression data from 117 patients with incipient T-ALL, a new subpopulation named pre-T-cell (ETP) ALL has been identified, featuring early T-cell developmental arrest and various chromosomal rearrangements leading to constitutive activation of MEF2C (Homminga et al. 2011). The above implies that ectopic expression of MEF2C is involved in the development of T-ALL and AML. Strikingly, no MEF2C aberrations in B-ALL have been documented in previous studies. MEF2C is abundantly expressed in both hematopoietic stem cells (HSC) and common myeloid progenitor cells (CMPs). MEF2C expression gradually decreases during the maturation of granulocyte-monocyte progenitors (GMPs) and megakaryocyte-erythroid progenitors. Compared with that in HSCs and CMPs, MEF2C expression is higher in common lymphoid precursors (CLPs), and decreases when the cells commit to the B-cell lineage. In contrast, MEF2C expression is virtually absent in T cells (Canté-Barrett et al. 2014). So, it is suggested that in normal development, MEF2C helps to drive differentiation into the CLP lineage or B-cell lineage. This lineage direction may be due to active transcription as MEF2C cooperates with p300/CBP to acetylate histones (Canté-Barrett et al. 2014).
A genomic study by Gu et al. identified fusions between MEF2D (myocyte enhancer factor 2D) and five genes (BCL9, CSF1R, DAZAP1, HNRNPUL1, and SS18) in 22 B-ALL cases (Gu et al. 2016). Among them, MEF2D::SS18 fusion has caught our eye. MEF2D and MEF2C belong to the MEF2 protein family, which consists of four members: MEF2A, B, C, and D. MEF2 family members have multiple splicing variants and share a conserved N-terminal MADS box and MEF structural domain (Black and Olson 1998). MADS box and MEF structural domain regulate the transcriptional activity of MEF2 by recruiting co-activators or co-repressor factors (Black and Olson 1998). As mentioned above, SS18 and SS18L1 sequences are similar and both of them has a QPGY domain (Kato et al. 2002). The QPGY domain is essential for transcriptional activation, while the SNH domain acts as an interaction interface for a plethora of proteins, several of which are involved in epigenetic gene regulation, including SWI/SNF proteins (Bruijn and Geurts van Kessel 2006). By comparing the breakpoints and structural domains of MEF2C::SS18L1 and MEF2D::SS18 fusion genes, we found that they retained the MADS box and MEF structural domain in MEF2 and the QPGY domain in SS18 (Fig. 2C). SS18 exerts its regulatory role through protein–protein interactions, but both fusion genes have lost their SNH domains; thus, we speculate that they might have lost the functions of SS18. Gu et al. found that all MEF2D fusion partners can augment MEF2D transcriptional activation (Gu et al. 2016). We notice a γ region in some MEF2C isoforms that functions to suppress the transcriptional activity of MEF2C and is spliced out in many tissues due to a unique 3’-splice acceptor site in MEF2C. The activity of the g domain is repressed by phosphorylation of serine 396 (S396), thus facilitating sumoylation at lysine 391 (K391) of MEF2C and the recruitment of unknown co-repressors to inhibit transcription (Kang et al. 2006). However, the MEF2C::SS18L1 fusion gene has lost the exon that encodes the γ region, so we infer that MEF2C::SS18L1 fusion might also enhance MEF2C expression.
It has been reported that MEF2D rearrangements can enhance its transcriptional activity and lymphoid transformation, thus contributing to the development of a high-risk leukemia (Gu et al. 2016; Yasuda et al. 2016). Fusion with MEF2D can significantly up-regulate HDAC9 and HDAC11, activate the MAPK pathway, inhibit the expression of B-cell differentiation-related genes, and hinder V(D)J rearrangement, thereby blocking B-cell differentiation and maturation (Zhang and Meng 2022). HDAC11 competes with P300 in binding to MEF2, and p300/CBP can affect lineage direction (Fig. 2B). The immunophenotype of MEF2D-rearranged ALL is characterized by weak or absent expression of CD10 and overexpression of CD38 antigens (26). However, low or absent expression of CD10 is a feature of MLL-rearranged ALL. Both the 5-year event-free survival (EFS) and overall survival (OS) rates are significantly lower in patients with MEF2D fusion than in other ALL patients, indicating that MEF2D fusion is significantly associated with ALL prognosis (Gu et al. 2016; Zhang and Meng 2022; Ohki et al. 2019). Although their response to steroids is sensitive, MEF2D fusion patients still show a significantly worse prognosis, with more than half experiencing relapse or dying within 1 year (Ohki et al. 2019).
Since these two fusion proteins have structurally similar domains, would MEF2C::SS18L1-positive B-ALL patients have similar clinical, pathological, or genetic features as MEF2D::SS18 positive patients? In our study, we found that this patient with MEF2C::SS18L1 fusion also showed: (1) high expression of HDAC9, (2) deletion of CD10 and (3) high expression of CD38. Coincidentally, this is consistent with the performance of MEF2D::SS18 fusion positive ALL. However, further in-depth studies are needed to determine whether these two fusion genes have the same pathogenic mechanism. In addition, whole transcriptome sequencing revealed a mutation in the PTPN11 gene in this patient. A mutational analysis of RNAseq data showed that this mutation was also found in MEF2D fusion-positive patients (Gu et al. 2016). The co-occurrence of PTPN11 mutation and fusion gene indicated similar molecular mechanism of MEF2D fusion with our present MEF2C gene fusion. However, further molecular experiments are still needed.
There are some limitations of the present study. First, we have searched public databases and have not found whole transcriptome sequencing data from the bone marrow of healthy subjcts. Therefore, in the present DEGs analysis, we used dataset GSE11504 as control set, which is microarray data contained 25 cases of healthy children, adolescents and adults aged 2 months to 28 years. This microarray contains 47,000 transcripts, representing 38,500 human genes. Expression information of this dataset can be widely used for the discovery of new regulatory pathways, exploration of disease mechanisms, and discovery of biomarkers (Vitari et al. 2011). We also used SVA package to remove the batch effect. Second, as MEF2C::SS18L1 fusion gene is a novel identified fusion gene in the present ALL case, limited clinical expression and clinical data could be obtained. Currently we have only one clinical sample, and MEF2C::SS18 fusion has only been reported in Microsecretory Adenocarcinoma without public expression data. We will continue to follow more ALL patients with MEF2C::SS18L1 fusion gene to perform more analyses on gene expression, as well as their clinical outcomes.
In summary, we identified a new MEF2C::SS18L1 fusion gene in a child with B-ALL that has similar structure and clinical features to MEF2D::SS18. Unlike those with MEF2D fusion, this patient showed high expression of the EST1 gene. This patient has achieved complete remission and is on sequential chemotherapy. We will continue to follow him to further observe his prognosis. We suggest that physicians should re-evaluate the risk once MEF2C fusions are present in B-ALL. Meanwhile, we should further explore the mechanism of this fusion gene and develop targeted drugs to improve the prognosis of ALL patients.
Availability of data and materials
The patient’s data are available upon reasonable request.
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127(20):2391–2405
Bishop JA, Weinreb I, Swanson D, Westra WH, Qureshi HS, Sciubba J et al (2019) Microsecretory adenocarcinoma: a novel salivary gland tumor characterized by a recurrent MEF2C-SS18 fusion. Am J Surg Pathol 43(8):1023–1032
Bishop JA, Sajed DP, Weinreb I, Dickson BC, Bilodeau EA, Agaimy A et al (2021) Microsecretory adenocarcinoma of salivary glands: an expanded series of 24 cases. Head Neck Pathol 15(4):1192–1201
Black BL, Olson EN (1998) Transcriptional control of muscle development by myocyte enhancer factor-2 (MEF2) proteins. Annu Rev Cell Dev Biol 14:167–196
Brix N, Kessel C, Foell D, Hasle H, Albertsen BK, Bruun NH et al (2023) Phagocyte-related S100 proteins and cytokines in acute lymphoblastic leukemia and their prognostic value. Leuk Lymphoma 64(5):981–989
de Bruijn DR, Geurts van Kessel A (2006) Common origin of the human synovial sarcoma associated SS18 and SS18L1 gene loci. Cytogenet Genome Res 112(3–4):222–226
Canté-Barrett K, Pieters R, Meijerink JP (2014) Myocyte enhancer factor 2C in hematopoiesis and leukemia. Oncogene 33(4):403–410
Collins-Underwood JR, Mullighan CG (2010) Genomic profiling of high-risk acute lymphoblastic leukemia. Leukemia 24(10):1676–1685
Conter V, Bartram CR, Valsecchi MG, Schrauder A, Panzer-Grümayer R, Möricke A et al (2010) Molecular response to treatment redefines all prognostic factors in children and adolescents with B-cell precursor acute lymphoblastic leukemia: results in 3184 patients of the AIEOP-BFM ALL 2000 study. Blood 115(16):3206–3214
Forero-Castro M, Robledo C, Benito R, Abáigar M, África Martín A, Arefi M et al (2016) Genome-wide DNA copy number analysis of acute lymphoblastic leukemia identifies new genetic markers associated with clinical outcome. PLoS One 11(2)
Gu Z, Churchman M, Roberts K, Li Y, Liu Y, Harvey RC et al (2016) Genomic analyses identify recurrent MEF2D fusions in acute lymphoblastic leukaemia. Nat Commun 7:13331
Harrison CJ, Foroni L (2002) Cytogenetics and molecular genetics of acute lymphoblastic leukemia. Rev Clin Exp Hematol 6(2):91–113; discussion 200–2
Homminga I, Pieters R, Langerak AW, de Rooi JJ, Stubbs A, Verstegen M et al (2011) Integrated transcript and genome analyses reveal NKX2-1 and MEF2C as potential oncogenes in T cell acute lymphoblastic leukemia. Cancer Cell 19(4):484–497
Kang J, Gocke CB, Yu H (2006) Phosphorylation-facilitated sumoylation of MEF2C negatively regulates its transcriptional activity. BMC Biochem 7:5
Kato H, Tjernberg A, Zhang W, Krutchinsky AN, An W, Takeuchi T et al (2002) SYT associates with human SNF/SWI complexes and the C-terminal region of its fusion partner SSX1 targets histones. J Biol Chem 277(7):5498–5505
Kuiper RP, Schoenmakers EF, van Reijmersdal SV, Hehir-Kwa JY, van Kessel AG, van Leeuwen FN et al (2007) High-resolution genomic profiling of childhood ALL reveals novel recurrent genetic lesions affecting pathways involved in lymphocyte differentiation and cell cycle progression. Leukemia 21(6):1258–1266
Mitelman F, Johansson B, Mertens F (2007) The impact of translocations and gene fusions on cancer causation. Nat Rev Cancer 7(4):233–245
Mullighan CG (2012) Molecular genetics of B-precursor acute lymphoblastic leukemia. J Clin Invest 122(10):3407–3415
Mullighan CG, Goorha S, Radtke I, Miller CB, Coustan-Smith E, Dalton JD et al (2007) Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature 446(7137):758–764
Ohki K, Kiyokawa N, Saito Y, Hirabayashi S, Nakabayashi K, Ichikawa H et al (2019) Clinical and molecular characteristics of MEF2D fusion-positive B-cell precursor acute lymphoblastic leukemia in childhood, including a novel translocation resulting in MEF2D-HNRNPH1 gene fusion. Haematologica 104(1):128–137
Onciu M (2009) Acute lymphoblastic leukemia. Hematol Oncol Clin North Am 23(4):655–674
Pruneri G, Fabris S, Dell’Orto P, Biasi MO, Valentini S, Del Curto B et al (2005) The transactivating isoforms of p63 are overexpressed in high-grade follicular lymphomas independent of the occurrence of p63 gene amplification. J Pathol 206(3):337–345
Schüler A, Schwieger M, Engelmann A, Weber K, Horn S, Müller U et al (2008) The MADS transcription factor Mef2c is a pivotal modulator of myeloid cell fate. Blood 111(9):4532–4541
Schultz KR, Pullen DJ, Sather HN, Shuster JJ, Devidas M, Borowitz MJ et al (2007) Risk- and response-based classification of childhood B-precursor acute lymphoblastic leukemia: a combined analysis of prognostic markers from the Pediatric Oncology Group (POG) and Children’s Cancer Group (CCG). Blood 109(3):926–935
Schwieger M, Schüler A, Forster M, Engelmann A, Arnold MA, Delwel R et al (2009) Homing and invasiveness of MLL/ENL leukemic cells is regulated by MEF2C. Blood 114(12):2476–2488
Shugay M, Ortiz de Mendíbil I, Vizmanos JL, Novo FJ (2013) Oncofuse: a computational framework for the prediction of the oncogenic potential of gene fusions. Bioinformatics. 29(20):2539–2546
Villanueva MT (2012) Genetics: gene fusion power. Nat Rev Clin Oncol 9(4):188
Vitari AC, Leong KG, Newton K, Yee C, O’Rourke K, Liu J et al (2011) COP1 is a tumour suppressor that causes degradation of ETS transcription factors. Nature 474(7351):403–406
Xie MX, Xie YH (2013) Advances of studies on members of P53 family, interaction and relation with leukemia -review. Zhongguo Shi Yan Xue Ye Xue Za Zhi 21(5):1331–1335
Yasuda T, Tsuzuki S, Kawazu M, Hayakawa F, Kojima S, Ueno T et al (2016) Recurrent DUX4 fusions in B cell acute lymphoblastic leukemia of adolescents and young adults. Nat Genet 48(5):569–574
Yu J, Yi T, Lin G, Wen J, Chen L, Chen J et al (2020) Prognostic significance and risk factors of minimal residual disease ≥1% on 19th day of induction chemotherapy in children with acute lymphoblastic leukemia. Nan Fang Yi Ke Da Xue Xue Bao 40(2):255–261
Zakaria Z, Othman N, Ismail A, Kamaluddin NR, Esa E, Abdul Rahman EJ et al (2017) Whole-exome sequencing of ETV6/RUNX1 in four childhood acute lymphoblastic leukaemia cases. Asian Pac J Cancer Prev 18(4):1169–1175
Zhang H, Meng G (2022) A typical bedside-to-bench investigation of leukemogenic driver MEF2D fusion reveals new targeted therapy in B-cell acute lymphoblastic leukemia. Blood Sci 4(3):161–163
Acknowledgements
We thank the patient in this study.
Funding
This study was supported by the National Natural Science Foundation of China (81903383), the Natural Science Foundation of Jiangsu Province (BK20211009), Scientific Research Projects of Jiangsu Health Commission (ZDB2020018), a China Postdoctoral Science Foundation-funded project (2021M701764), the Special Fund for Health Science and Technology Development in Nanjing (JQX19008), the Nanjing Medical Science and Technology Development Project (YKK21149), and the Young Talent Support Project of the Children’s Hospital of Nanjing Medical University (TJGC2020016, TJGC2020007, TJGC2020014).
Author information
Authors and Affiliations
Contributions
CC and XY conceived the study. CC and WJ participated in method development and validation. WJ performed a bioinformatics analysis. CC, KM, and WJ carried out the data analysis. WP was involved in the management of the patient and provided clinical data. XY and FY reviewed and modified the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethics approval and consent to participate
Our study was approved by the IEC Institutional Review Board of the Children’s Hospital of Nanjing Medical University on August 7, 2020 (approval number: 202008043-1). The patient’s parents provided written informed consent to participate in this study. Patient data will not be shared with outside parties.
Consent for publication
All the authors agreed to the publication of the manuscript in its present form. Patient consent was managed according to local approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, C., Wang, J., Kang, M. et al. Identification of a novel MEF2C::SS18L1 fusion in childhood acute B-lymphoblastic leukemia. J Cancer Res Clin Oncol 150, 314 (2024). https://doi.org/10.1007/s00432-024-05846-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05846-8