Abstract
Introduction
Adjuvant treatment with immune checkpoint inhibitors, such as PD1-antibodies (ICI) ± CTLA4-antibodies (cICI) or targeted therapy with BRAF/MEK inhibitors (TT), has shown a significant improvement in disease-free survival (DFS) for high-risk melanoma patients. However, due to specific side effects, the choice of treatment is often influenced by the risk of toxicity. Therefore, the role of physicians in treatment decisions of patients is crucial. This study investigated for the first time in a multicenter setting the attitudes and preferences of dermatooncologists in Germany and Switzerland regarding adjuvant treatment with (c)ICI and TT.
Methods
In the GERMELATOX-A study, 108 physicians (median age: 32 yrs, 67.6% female) from 11 skin cancer centers were surveyed to rate typical side effect scenarios of (c)ICI and TT treatments and then compared to patients’ ratings evaluated in a previous analysis from the same centers. The scenarios described mild-to-moderate or severe toxicity and included melanoma relapse leading to death. The physicians were asked about the level of side effects they would tolerate in exchange for a reduction in melanoma relapse and an increase in survival at 5 years.
Results
The preferences of physicians and patients revealed significant differences regarding adjuvant melanoma treatment with (c)ICI and TT (p < 0.05). Compared to patients, physicians tend to value a melanoma relapse less severe, according to a visual analog scale. They were also less threatened by all scenarios of side effects during adjuvant treatment with (c)ICI or TT, compared to patients. Physicians required lower risk reductions for disease-free survival (DFS) and overall survival (OS) for both ICI and TT and their drug-related side effects to accept these treatments. In case of severe side effects, physicians required similar 5-year DFS rates for ICI and TT (60–65%), while patients needed a 15% improvement of 5-year DFS for ICI compared to TT (80%/65%). For survival, physicians expected an OS improvement of + 10% for all three treatment modalities, whereas patients required a higher increase: + 18–22% for ICI and + 15% for TT.
Conclusion
Our study highlights the importance of understanding the patient’s perspective and a potential difference to the doctor’s view when making decisions about adjuvant melanoma treatment with (c)ICI and TT, especially as these treatments are increasingly being implemented in earlier stages.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the years, significant advancements have been made in the treatment of melanoma, particularly with the introduction of targeted therapies and immunotherapies for patients with advanced melanoma (Garutti et al 2022). These treatments have been successful in the metastatic setting and have now progressed to the adjuvant setting, where they can benefit high-risk patients. High-risk melanoma is defined as a deep invasive primary tumor with or without ulceration (AJCC (8th edition) stage IIB and IIC) or with regional nodal disease (AJCC stage III). The 10-year melanoma-specific survival rates range from 84% for AJCC stage II down to 69% for AJCC stage III (Gershenwald et al 2017). While patients with thinner melanomas can be cured by surgery alone, increasing tumor thickness is associated with the risk of relapse and metastatic disease. Therefore, the healthcare provider and the patient must decide when to use adjuvant therapy, whether to treat in the adjuvant setting or wait until recurrence, and whether the benefits of adjuvant therapy outweigh the risks.
Adjuvant therapies such as immune checkpoint blockade or targeted therapy have been approved and are now considered standard of care not only for high-risk patients but also for intermediate-risk patients in AJCC stage IIB. These therapies have shown improvements in disease-free survival (DFS) and distant metastasis survival (DMFS), which can serve as a surrogate parameter for overall survival (Kobeissi and Tarhini 2022; Long et al. 2022). Adjuvant therapy is considered potentially curative and can prevent relapse and the poor outcomes seen in metastatic disease. In stage IV, adjuvant treatment with PD1-antibodies (ICI) ± CTLA4-antibodies (cICI), has also been demonstrated to be very effective and is, therefore, increasingly used in daily routine (Livingstone et al. 2022).
The toxicity of targeted therapy, dabrafenib and trametinib, is characterized by symptoms such as fever, gastrointestinal symptoms, joint pain, a decrease in the left ventricular function, and eye disorders (Lazaroff and Bolotin 2023) that can also impair quality of life (Scarpato et al. 2022; Lai-Kwon et al. 2023) In contrast, immune checkpoint inhibitors (c(ICI)) can induce autoimmune toxicity in nearly every organ system and a small subset of patients with a fatal course (Wang et al 2018). Despite the frequency of side effects, in the majority of patients, health-related quality of life (HrQoL) is not or only temporarily impaired (Bottomley et al. 2021; Khattak et al. 2022; Pedersen et al 2023; Lai-Kwon et al. 2023). However, in case of severe side effects, HRQoL may be persistently impaired, which can eventually lead to treatment stop (Pedersen et al. 2023; Wang et al. 2018).
In contrast to TT, (c)ICI has the potential for severe side effects that may be chronic and may be fatal or accompanied by a deterioration for quality of life (Wang et al. 2018; Schulz et al. 2022). Therefore, it is important to discuss the risks and benefits of therapy with the patient considering the benefits and risks of the treatment. Especially in adjuvant treatment, physicians need to discuss the individual risk–benefit ratio with eligible patients thoroughly. The physician’s beliefs may influence this decision-making process, so it is important to be aware of any differences between patients’ and physicians’ attitudes toward toxicity. Currently, there is limited knowledge about the differences between melanoma patients and their physicians concerning their preferences toward the toxicity of adjuvant melanoma treatment (Krammer et al. 2014; Weiss et al. 2020). However, it is known that patients and physicians may rate the benefit–risk ratios differently in other tumor entities (Zhang et al. 2023).
We conducted a study to evaluate the attitudes of dermatooncologists towards toxicity during adjuvant treatment and compared the results with a patient cohort we previously evaluated in these melanoma centers (Kähler et al. 2023). We aimed to identify any differences between melanoma patients and their treating physicians regarding the risk–benefit of adjuvant treatment in melanoma. There is limited data available about physician preferences for benefit versus toxicity in these treatments in the adjuvant setting. This study is the first to investigate, in a multicenter approach, how dermatooncologists value different spectrums of toxicity of adjuvant immunotherapy and targeted therapy in direct comparison to their patients.
Methods
Physicians, patients and study centers
This is a cross-sectional, observational, non-interventional questionnaire study that involved ten German and one Swiss skin cancer center with high expertise in treating melanoma. The study included dermatologists and dermatology residents who were familiar with the treatment of melanoma and worked in a German/Swiss melanoma center where melanoma patients are diagnosed, resected, and treated with systemic therapy by dermatooncologists.
The group of physicians was compared with previously evaluated patients with low-risk melanoma, defined as T1a, at least 8 weeks after initial diagnosis, no sentinel node biopsy or significant co-morbidities (Kähler et al. 2023). The rationale for low-risk melanoma patients was to choose a patient cohort with the experience of melanoma diagnosis, but not in the situation of having to decide for or against adjuvant treatment, to avoid ethical conflicts potentially induced by this study that may influence a patient’s decision.
We collected information on various sociodemographic factors, including age, gender, marital status, employment status, and working hours. We also asked about previous experience with cancer and co-morbidities. Additionally, we evaluated professional data such as the frequency of contact with melanoma patients, frequency of prescription of adjuvant treatment, duration of being a dermato-oncologist, percentage of subjects treated with mild side effects, and percentage of subjects treated with severe toxicity.
Treatment trade-off
A survey tool that met the objective of our study was not available, so we created a new questionnaire. The questionnaire’s treatment scenarios were based on the literature and the expertise of two clinical dermato-oncologists. Pre-testing of the questionnaire for comprehensibility was done by three independent physicians and four volunteering patients provided feedback was used to revise it.
To elicit preferences, we used a paper-based treatment-trade-off task. Participants were asked to imagine having melanoma with a 30% chance of 5-year DFS and a 50% chance of 5-year OS. We described three treatments (TT, ICI, or cICI treatment), including the nature and probability of side effects, and asked participants to choose their preferred treatment. Additionally, we evaluated preferences for the recurrence of melanoma after adjuvant treatment, resulting in 12 different scenarios (an example is provided in the supplementary).
Scenario 1 = TT without side effects.
Scenario 2 = TT with mild to moderate side effects.
Scenario 3 = TT with severe side effects.
Scenario 4 = ICI without side effects.
Scenario 5 = ICI with mild to moderate side effects.
Scenario 6 = ICI with mild to moderate side effects and abnormal blood values.
Scenario 7 = ICI with severe side effects.
Scenario 8 = cICI without side effects.
Scenario 9 = cICI with mild to moderate side effects.
Scenario 10 = cICI with mild to moderate side effects and abnormal blood values.
Scenario 11 = cICI with severe side effects.
Scenario 12 = Recurrence of melanoma after adjuvant treatment (only rated for acceptability).
In contrast to previous uses of treatment-trade-off, participants were not presented a series of different DFS and OS rates for each scenario (1). Instead, the participants were requested to specify the minimum number of prevented recurrences or deaths necessary for them to opt for the treatment instead of not receiving any treatment. In other words, they were asked to state the required chances of DFS and OS that would make them choose the treatment over the alternative of no treatment. The statement to be completed, for example, “I would choose the treatment described in scenario 1 if it would prevent a relapse in at least ___ of these 70 patients.”
Participants were additionally asked to rate the acceptability of each scenario using visual analog scales (VAS) ranging from 0% = completely unbearable to 100% = completely bearable.
Thus, for each scenario, participants rated the minimally required increase in DFS and OS, respectively, as well as acceptability using the VAS.
Primary endpoint
The primary objective was to determine preferences for adjuvant treatment with severe side effects in terms of the minimum required benefit, as defined in the treatment trade-off task, which was an additional chance of 5-year DFS.
Secondary endpoints
To identify preferences for adjuvant treatments with mild to moderate and severe side effects during (c)ICI and TT, we needed to determine the minimum benefit required in terms of the additional chance of 5-year DFS and 5-year OS. This will be stated in the treatment trade-off task.
Additional assessments
We asked physicians to rate their preference for infusion or oral medication on a 5-point scale from “completely agree” to “do not agree at all”.
Self-applied medication: “It is okay for me to take the medicine on my own”.
Supervised medication: “It seems beneficial to me to have the drug administered under the supervision of a doctor”.
Rather visits than self-application: “I’m happy to put up with infusions and more frequent visits to the doctor, as long as I then don’t have to be responsible for taking the medicine myself”.
Acceptance of long doctor’s appointments: “I can accept that an appointment with infusion and medical examination can take several hours”.
Compliance with a strict intake schedule: “I can stick to a precise schedule for taking pills”.
Importance of treatment method (infusion vs. pill): “The way I get the medicine administered (infusion or pills) matters to me”.
In addition, participants rated their preference for dosage via infusion vs. pill on a horizontal VAS from − 100 (infusion) to + 100 (pills) and 0 indicating “undecided”.
The same data as previously for patients (Kähler et al 2023) were assessed in this second part of the study for physicians: preferences, socio-demographics, and self-experience with cancer.
Sample size calculation
The number of participants to be included was determined according to the primary endpoint of preferences for BRAF/MEKi treatment. To determine the percentage of participants who would choose BRAF/MEKi treatment at a 5-year-DFS of 65% or lower with a 95% confidence interval width of ± 10 percentage points, 104 analyzable data sets were needed (or less if the distribution of participants would differ from 50:50; calculated with PASS Sample Size 2008).
Statistical approach
For all variables, descriptive statistics were computed (frequencies, percentages, mean, median, and/or standard deviation (SD), as applicable).
Participants were excluded from the OS, DFS, or VAS analysis, respectively, if they misordered two or more pairs of scenarios (e.g. lower rank for mild-to-moderate side effects than for severe side effects in otherwise identical scenarios) as this was regarded as an indicator of insufficient understanding of the rating task.
OS, DFS, and VAS were analyzed as the arithmetic mean along with the 95% confidence interval. Differences between treatment scenarios were tested with paired samples t tests. Preferences for the different scenarios (PFS, OS, VAS) were tested for differences for statistically significant differences between treatment scenarios and between physicians and patients using paired samples t tests.
Significance levels equal to or below 0.05 were considered statistically significant; no adjustment for multiple testing was performed.
The association of treatment preferences (DFS, OS, VAS) with important characteristics (socio-demographic data, self-experience with cancer, psychological constructs) was assessed using bivariate tests (Pearson correlations or t-tests, depending on variable scaling).
Results
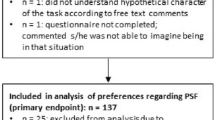
All 115 physicians who gave informed consent could be included in the analysis. From the analysis of the different scenario ratings, between 7 and 11 questionnaires had to be excluded, with n = 108 analyzable for the primary endpoint (Fig. 1). Out of 165 patients who have been analyzed in a previous part of the study (Kähler et al. 2023), 3 had to be excluded from analysis for different reasons. Regarding the analysis of the scenario ratings, between 11 and 25 patients had to be excluded, with n = 137 analyzable for the primary endpoint.
Study flowchart represented included, excluded, and analyzed physicians in comparison to previously analyzed patients (Kähler et al. 2023)
Characteristics of physicians
Dermatologists were between 25 and 60 years of age (mean 33.9 years, median 32.0, SD 7.7), 67% were female. Most were in a relationship or married and living with one person. Median working hours were 42 per week (Table 1).
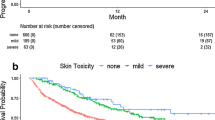
Physicians had a median of 40 patient contacts per month, according to Table 2. Their experience as a physician ranged from 0.1 to 35 years, with a median of 3.5. They reported that severe side effects were more common in patients during cICI (median 30%) than in TT or ICI (median 10%). The experience of physicians as clinical dermatologists or the frequency of consultations with melanoma patients did not correlate with scenario ratings, except for scenario 3 (severe side effects during TT), as shown in Table 3.
Patient characteristics
To describe the group of patients analyzed in our previous study, we present the socio-demographic characteristics of the full analysis set, which included 162 patients (Kähler et al. 2023). The patient cohort was predominantly German/Swiss (95%), with the remaining 5% having different nationalities. The group was almost equally divided between male (47%) and female (57%) subjects. The patients’ ages ranged from 24 to 93 years, with a median age of 60 years. The median time since melanoma diagnosis was 1 year (SD 5 years, range: 0–32 years). Most patients were married and living with one person, and the majority were either employed (with a median of 39 h/week) or retired.
Scenario rating concerning disease-free survival
In various scenarios, physicians required significantly fewer prevented relapses to accept the treatment and its side effects compared to patients (Tables 4, 5, 6).
In case of severe side effects, physicians required for TT a median reduction of 30 out of 70 relapses (mean 31.6, SD 17.8, range 1–70, 95% confidence interval 28.1–35). Physicians needed identical numbers of relapses prevented for TT (30) and (c)ICI (35) compared to patients who required 15 additional prevented relapses at 5 yrs for (c)ICI (50) compared to TT (35). In other words, physicians required similar 5-year DFS rates for ICI and TT (60–65%). Patients needed a 15% improvement of 5-year DFS for ICI compared to TT (80%/65.0%).
In case of no side effects, both physicians and patients requested a similar reduction in relapses. The ratings were 10/10 for TT, 10/10 for ICI, and 10/15 for cICI. However, when mild-to-moderate side effects were present, the situation changed. Physicians requested a significantly lower number of prevented relapses compared to patients. The ratings were 20/30 for TT, 15/20 for ICI, and 16/29 for cICI. Most of the scenarios were statistically different from each other, as shown in Table 6.
Scenario rating concerning overall survival
In case of no or mild-to-moderate side effects, physicians require a lower number of prevented deaths (5 and 10 for TT, 5 and 5 for ICI, 5 and 10 for cICI; median, Table 8) than patients (5 and 15 for TT, 5 and 15 for ICI, 10 and 20 for cICI; median, Kähler et al. 2023). Most physician ratings of scenarios were statistically different from each other (Table 7). Acceptance decreased with the severity of side effects. For TT with severe side effects, physicians and patients required a median of 15/25 avoided deaths and 20/30 avoided deaths for ICI or 20/35 deaths in case of cICI (p < 0.001), respectively.
For survival, in case of mild-to-moderate side effects, physicians expected an equal OS improvement (+ 5 to 10%) for all three treatment modalities, whereas patients required an increase of 15–22% for 5-year melanoma survival (ICI + 18 to 22% compared to TT + 15%; Kähler et al. 2023). In case of severe toxicity, physicians expected an equal OS improvement (+ 15 to 20%) for all three treatment modalities, whereas patients required an increase of 25–35% for 5-year melanoma survival ((c)ICI + 30 to 35% compared to TT + 25%).
The average ratings regarding OS were statistically different for most scenarios in both patients and physicians (table not shown).
Scenario rating by socioeconomic characteristics
There was a weak correlation (r < 0.3) between age and DFS ratings with older patients tending to require higher effectiveness to accept a treatment. In physicians, in contrast, gender, income, or co-morbidities did not show any association with DFS or OS rating.
Impact of self-experience of cancer on scenario rating
3.5% of physicians experienced cancer themselves (Table 8). Additionally, 67% of physicians had close persons affected by cancer. Our study showed that previous cancer experience did not correlate with PFS, OS, and scenario ratings in either group, except for a significant OS rating for scenarios 8 and 9 (cICI without side effects or only with mild-to-moderate side effects) in the patient cohort who had previous cancer experience.
The average ratings for PFS scenarios were similar for both patients with and without cancer experience. However, the average ratings for OS scenarios were also similar between the two groups, except for scenarios 8 and 9, which showed some differences (data not shown).
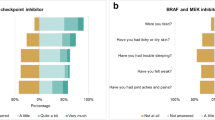
Dosage form preferences: infusion vs. oral medication
90% of physicians and 63% of patients (Kähler et al. 2023) agreed that it was acceptable to take their medicine on their own (Table 9). Physicians were more likely to agree with this statement than patients. Both patients and physicians rather disagreed to prefer supervised medication, and there was no significant difference between the two groups in this regard.
On average, patients and physicians disagreed that they would accept infusions and doctor visits, with physicians being more opposed to this idea. However, both groups were willing to accept appointments that take several hours, and most of them stated that they could stick to a precise intake schedule, with physicians being more confident in this regard.
Interestingly, more patients than physicians had a strong preference for a particular administration method (infusion or pills), and this difference was highly significant (Table 10).
According to the results of the horizontal VAS, most physicians and patients preferred pills over infusions, with a median score of 31 and 41.5 (Table 11) on a scale ranging from − 100 (infusion preferred) to + 100 (pills preferred). However, a significant number of participants chose “0,” indicating no preference. The mean score was 26.1, with a standard deviation of 61.6 and a range of − 100 to 100, based on a sample size of 161 patients. Patients generally did not see any benefits in supervised medication. On average, they disagreed with the idea of preferring infusions and doctor visits, and tended to prefer appointments that took several hours. Patients also stated that they could adhere to a precise intake schedule and that the method of administration (infusion or pills) was important to them.
Discussion
Our study revealed that patients and physicians have differing perspectives on toxicity during adjuvant therapy. The doctor´s view has been evaluated in dermatooncologists of 11 melanoma centers.
Association with physicians’ and patients’ characteristics
Noteworthy, the group of physicians is healthier, younger, more educated, wealthier, and less affected by previous cancer diagnoses compared to the patient cohort (Kähler et al. 2023).
In the physician cohort factors such as age, gender, professional experience, and intensity of contact with melanoma patients did not show any correlation with the ratings of scenarios related to melanoma treatment.
For patients, we know that their ability to communicate treatment side-effects, comorbidities, and their view on the treatment risk/benefit profile has been identified as a critical driver of clinical decisions in adjuvant AJCC stage III disease (Livingstone et al. 2021).
Older melanoma patients tended to require higher effectiveness to accept an adjuvant treatment, this was reflected in the DFS ratings (Kähler et al 2023). The effect sizes were small though. These results are similar to our previous GERMELATOX analysis that evaluated patient preferences for adjuvant interferon-alpha (Kähler et al. 2016). In contrast, Weilandt et al. showed in a discrete choice approach in melanoma patients that increasing age, toxicity, and impact on their daily routine were more relevant than efficacy (Weilandt et al. 2021). They also found that married patients and patients with a higher level of education have higher expectations of treatment efficacy (Weilandt et al. 2021). In our study, a pre-existing cancer diagnosis did not influence average scenario ratings regarding acceptability or DFS in patients (Kähler et al 2023). Average scenario ratings regarding OS also did not differ between patients with experience with cancer and those without, except for scenarios 8 and 9 (cICI without or only mild to moderate side effects) but, again, with small effect sizes only (Kähler et al. 2023).
Physicians should be aware of the difference in perspectives between the patient and themselves and guide the informed consent process accordingly. Atkinson et al. found that physicians favored adjuvant therapy for their patients in 35% of cases, favored observation in 35% of cases, and had no preference in 29% of cases. Although these preferences were not communicated to the patients, the patient´s choice regarding adjuvant therapy (treatment vs. observation only) showed a significant, albeit small, correlation with the physician’s preference (treatment vs. observation only/no preference) (Atkinson et al. 2023).
Difference between the perception of TT versus (c)ICI
In our study, physicians and patients had different perspectives on the side effects of TT and ICI. Physicians were less concerned by IO toxicity and potentially long-lasting side effects and generally had a less negative view of toxicity maybe due to their awareness of the benefits of successful side effect management. Patients, on the other hand, were more willing to accept severe side effects induced by TT compared to (c)ICI. Patients rated potentially lethal or not resolving side effects induced by (c)ICI worse. However, most of the scenarios were rated as completely unacceptable by less than 1% of the patients and 0% of the physicians, showing the immense willingness of German and Swiss patients to tolerate treatment-related side effects.
Interestingly, patients were more willing to accept TT-associated pyrexia if the drug efficacy and, therefore, their outcome benefit is known (Mansfield et al. 2021), physicians should focus on precise and adequate information in the informed consent process.
The more negative perception of severe side effects during adjuvant treatment with (c)ICI compared to TT has also been confirmed by the comparison of the acceptability of scenarios. This can be explained by the possibility of long-lasting toxicity with sequelae and as well potentially fatal course of autoimmune side effects. A trial with structured interviews of melanoma physicians and nurses identified severe immune-related treatment side-effects overall and recurrence-free survival as highly influential factors in their immunotherapy decision-making (Livingstone et al. 2020). Melanoma patients scored higher on HRQoL social well-being at pre-treatment of ICI, were more likely to endorse positive statements about adjuvant immunotherapy, and perceived that their physician preferred adjuvant therapy combined with lower decisional regret and higher satisfaction, even if they experienced toxicity or recurrence (Atkinson et al. 2023). This may have an impact on patient–physician discussions and patient reflection at the time of treatment choice. Decisional regret was also lower in patients in that trial who had undergone lymph node dissection consistent with the idea that more aggressive treatment may be associated with less decisional regret (Atkinson et al. 2023). Therefore, the aspect of decisional regret should be considered and communicated in informed consent processes.
The difference in the mode of administration between c(ICI) and TT might also be a reason for melanoma patients to rate TT superior to (c)ICI. Most patients and dermatologists in our trial stated it was acceptable for them to take the medicine on their own. For dermatologists, this was significantly more the case than for patients. The majority did not see benefits in supervised medication. Most patients and dermatologists stated they could stick to a precise intake schedule, which was even more pronounced in dermatologists. More patients than dermatologists stated having a strong preference for an administration method (infusion or pills), which was highly significant. Our patients preferred the autonomy of an oral medication whereas the melanoma cohort of Weilandt and co-workers showed in their analysis that patients favored infusions. This might be explained by the fact that in our patient cohort, the decision for melanoma treatment and treatment regimen was an entirely fictitious scenario. Therefore, our patients might value the autonomy of an oral medication higher, whereas patients facing the adjuvant treatment decision in a real scenario perhaps might somewhat be overwhelmed by the challenge of understanding the process and therefore prefer to delegate the treatment responsibility regarding medication intake to their physician. Stellato and co-workers showed in a Canadian cohort that physicians assigned the highest preference for orally administered treatments (corresponding to the dosing regimen for dabrafenib–trametinib), melanoma patients had a similar preference for orally administered treatments and infusions administered over 30 min every 3 weeks (corresponding to the dosing regimen for pembrolizumab) (Stellato et al. 2019).
Do current treatment options meet our expectations?
We observed that physicians tend to accept a less significant treatment benefit by adjuvant treatment as compared to patients. This might be because physicians are not personally involved in the treatment process. A study by Weiss et al. suggests that previous cancer experience could affect treatment outcome ratings. Patients and physicians who have had personal cancer experience tended to value life prolongation by melanoma treatment more positively than healthy controls or physicians without personal cancer experience (Weiss et al. 2020).
In our trial, physicians tended to rate melanoma relapse less negatively than patients (Kähler et al. 2023), which could be due to their more optimistic view of treatment options and outcomes.
For DFS patients’ expectations towards efficacy differed between the three treatment modalities only by a range of 6 percentage points, despite the distinct rate of grade 3–4 adverse events (ranging from 14.4 to 71.0%, Table 12, Kähler et al. 2023).
In general, the clinical trials conducted by Dummer et al. (2020), Larkin et al. (2023), Livingstone et al. (2022), and Schadendorf et al. (2022) have shown that the treatment efficacy is capable of meeting the expectations in terms of DFS found in our physician cohort. However, some follow-up data are still immature, and for cICI, only 4-year DFS data are available so far. Physicians and patients expected higher DFS rates for TT and ICI in case of severe side effects than shown for these treatment options in clinical studies (Kähler et al. 2023). In this situation, the efficacy would not be high enough for the patients. For OS (Table 13), the results are similar, but in case of severe side effects, the gap between expectations and the efficacy demonstrated in clinical trials so far seems to be smaller in case of using cICI. The gap between the expectations from risks and benefits of TT and ICI is more noticeable compared to cICI. This suggests that patients may not value the risk–benefit ratio as much as they do for cICI. However, it is important to note that cICI is only administered to specific patients in the adjuvant setting in AJCC stage IV.
In contrast, the expectations of the physician cohort for OS are concordant with the results from clinical trials for the available treatment options, as well as for severe toxicity.
Krammer et al. showed in their trial that attitudes towards toxicity and benefit vastly differed between healthy participants, physicians and melanoma patients. Whereas melanoma patients showed a high willingness to endure side effects despite very small survival gains (down to 1 extra week) or even only hope with no survival benefit, healthy controls were more critical, while physicians were the most therapy adverse (Krammer et al. 2014). Stellato et al. described that patients preferred an increased probability of remaining cancer-free over 21 months whereas physicians prioritized remaining alive over 36 months (Stellato et al. 2019).
Limitations of the study
Our study had some limitations. Firstly, the physician cohort we selected was mostly female and younger than a typical patient cohort; however, this corresponds with the typical composition of this group of persons. Secondly, we used a previously analyzed patient population with only low-risk melanoma as surrogates for those in later disease stages, due to ethical reasons. Thirdly, we did not analyze the perceptions of adjuvant melanoma treatment over time, so we may have missed possible changes in the individual course of the disease. However, evidence suggests that the tumor stage does not necessarily influence patients’ preferences (Atkinson et al. 2023). Fourthly, the usual melanoma patient cohort consists of more male than female patients, while in our study, more female patients were willing to participate. Finally, patient preferences were elicited based on hypothetical scenarios, which may not be completely comparable to real-life treatment decisions.
Overall, our study revealed a significant information and knowledge gap between physicians and patients, indicating different perspectives on treatment side effect perception. The most important goal should be to increase patients’ confidence in current treatment modalities and the competence of their physician. Physicians should be able to change their perspective to improve their understanding of possible reasons for patients declining adjuvant treatment.
References
Atkinson TM, Hay JL, Young Kim S, Schofield E, Postow MA, Momtaz PW et al (2023) Decision-making and health-related quality of life in patients with melanoma considering adjuvant immunotherapy. Oncologist 28(4):351–357. https://doi.org/10.1093/oncolo/oyac266. (PMID: 36745014; PMCID: PMC10078893)
Bottomley A, Coens C, Mierzynska J, Blank CU, Mandala M, Long GV et al (2021) Adjuvant pembrolizumab versus placebo in resected stage III melanoma (EORTC 1325-MG/KEYNOTE-054): health-related quality-of-life results from a double-blind, randomised, controlled, phase 3 trial. Lancet Oncol 22(5):655–664. https://doi.org/10.1016/S1470-2045(21)00081-4
Dummer R, Hauschild A, Santinami M, Atkinson V, Mandala M, Kirkwood JM et al (2020) Five-year analysis of adjuvant dabrafenib plus trametinib in stage III melanoma. N Engl J Med 383(12):1139–1148. https://doi.org/10.1056/NEJMoa2005493
Garutti M, Bergnach M, Polesel J, Palmero L, Pizzichetta MA, Puglisi F (2022) BRAF and MEK inhibitors and their toxicities: a meta-analysis. Cancers (basel). https://doi.org/10.3390/cancers15010141
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI et al (2017) Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 67(6):472–492. https://doi.org/10.3322/caac.21409
Kaehler KC, Blome C, Forschner A, Gutzmer R, Haalck T, Heinzerling L et al (2016) Preferences of German melanoma patients for interferon (IFN) alpha-2b toxicities (the DeCOG “GERMELATOX survey”) versus melanoma recurrence to quantify patients’ relative values for adjuvant therapy. Medicine (baltimore) 95(46):e5375. https://doi.org/10.1097/MD.0000000000005375
Kähler KC, Hüning S, Nashan D, Meiss F, Rafei-Shamsabadi DA, Rissmann H et al (2023) Preferences of German and Swiss melanoma patients for toxicities versus melanoma recurrence during adjuvant treatment (GERMELATOX-A-trial). J Cancer Res Clin Oncol 149(13):11705–11718. https://doi.org/10.1007/s00432-023-05027-z. (Epub 2023 Jul 5. PMID: 37405475; PMCID: PMC10465664)
Khattak MA, Luke JJ, Long GV, Ascierto PA, Rutkowski P, Schadendorf D et al (2022) Adjuvant pembrolizumab versus placebo in resected high-risk stage II melanoma: health-related quality of life from the randomized phase 3 KEYNOTE-716 study. Eur J Cancer 176:207–217. https://doi.org/10.1016/j.ejca.2022.08.004
Kobeissi I, Tarhini AA (2022) Systemic adjuvant therapy for high-risk cutaneous melanoma. Ther Adv Med Oncol 14:17588359221134088. https://doi.org/10.1177/17588359221134087
Krammer R, Heinzerling L (2014) Therapy preferences in melanoma treatment-willingness to pay and preference of quality versus length of life of patients, physicians and healthy controls. PLoS ONE 9(11):e111237. https://doi.org/10.1371/journal.pone.0111237. (PMID: 25369124; PMCID: PMC4219712)
Lai-Kwon J, Inderjeeth AJ, Lisy K, Sandhu S, Rutherford C, Jefford M (2023) Impact of immune checkpoint inhibitors and targeted therapy on health-related quality of life of people with stage III and IV melanoma: a mixed-methods systematic review. Eur J Cancer 184:83–105. https://doi.org/10.1016/j.ejca.2023.02.005. (Epub 2023 Feb 18. Erratum in: Eur J Cancer. 2023 Sep;190:112937. PMID: 36907021)
Larkin J, Del Vecchio M, Mandalá M, Gogas H, Arance Fernandez AM, Dalle S et al (2023) Adjuvant nivolumab versus ipilimumab in resected stage III/IV melanoma: 5-year efficacy and biomarker results from CheckMate 238. Clin Cancer Res 29(17):3352–3361. https://doi.org/10.1158/1078-0432.CCR-22-3145. (PMID: 37058595; PMCID: PMC10472092)
Lazaroff J, Bolotin D (2023) Targeted therapy and immunotherapy in melanoma. Dermatol Clin 41(1):65–77. https://doi.org/10.1016/j.det.2022.07.007
Livingstone A, Agarwal A, Stockler MR, Menzies AM, Howard K, Morton RL (2020) Preferences for immunotherapy in melanoma: a systematic review. Ann Surg Oncol 27(2):571–584. https://doi.org/10.1245/s10434-019-07963-y
Livingstone A, Dempsey K, Stockler MR, Howard K, Long GV, Carlino MSM et al (2021) Adjuvant immunotherapy recommendations for stage III melanoma: physician and nurse interviews. BMC Cancer 21(1):1014. https://doi.org/10.1186/s12885-021-08752-1.PMID:34507552;PMCID:PMC8434723
Livingstone E, Zimmer L, Hassel JC, Fluck M, Eigentler TK, Loquai C et al (2022) Adjuvant nivolumab plus ipilimumab or nivolumab alone versus placebo in patients with resected stage IV melanoma with no evidence of disease (IMMUNED): final results of a randomised, double-blind, phase 2 trial. Lancet 400(10358):1117–1129. https://doi.org/10.1016/S0140-6736(22)01654-3
Long GV, Luke JJ, Khattak MA, de la Cruz Merino L, Del Vecchio M, Rutkowski P et al (2022) Pembrolizumab versus placebo as adjuvant therapy in resected stage IIB or IIC melanoma (KEYNOTE-716): distant metastasis-free survival results of a multicentre, double-blind, randomised, phase 3 trial. Lancet Oncol 23(11):1378–1388. https://doi.org/10.1016/S1470-2045(22)00559-9
Mansfield C, Myers K, Klein K, Patel J, Nakasato A, Ling YL et al (2021) Risk tolerance in adjuvant and metastatic melanoma settings: a patient perspective study using the threshold technique. Future Oncol 17(17):2151–2167. https://doi.org/10.2217/fon-2020-1193
Pedersen S, Holmstroem RB, von Heymann A, Tolstrup LK, Madsen K, Petersen MA et al (2023) Quality of life and mental health in real-world patients with resected stage III/IV melanoma receiving adjuvant immunotherapy. Acta Oncol 62(1):62–69. https://doi.org/10.1080/0284186X.2023.2165449
Scarpato L, Festino L, Vanella V, Madonna G, Mastroianni M, Palla M, Ascierto PA (2022) Dermatologic adverse events associated with targeted therapies for melanoma. Expert Opin Drug Saf 21:385–395. https://doi.org/10.1080/14740338.2022.1986000. (Epub 2021 Nov 2 PMID: 34595993)
Schadendorf D, Hauschild A, Mandalà M, Kirkwood JM, Robert C, Grob J-J et al (2022) Adjuvant dabrafenib plus trametinib (D + T) versus placebo in patients with resected stage III BRAFV600-mutant melanoma: updated 5-year distant metastases-free survival (DMFS) analysis of COMBI-AD. J Clin Oncol 40(16 suppl):9563–9563. https://doi.org/10.1200/JCO.2022.40.16_suppl.9563
Schulz TU, Zierold S, Sachse MM, Pesch G, Tomsitz D, Schilbach K et al (2022) Persistent immune-related adverse events after cessation of checkpoint inhibitor therapy: prevalence and impact on patients’ health-related quality of life. Eur J Cancer 176:88–99. https://doi.org/10.1016/j.ejca.2022.08.029
Stellato D, Thabane M, Eichten C, Delea TE (2019) Preferences of Canadian patients and physicians for adjuvant treatments for melanoma. Curr Oncol 26(6):e755–e765. https://doi.org/10.3747/co.26.5085. (Epub 2019 Dec 1. PMID: 31896946; PMCID: PMC6927775)
Wang DY, Salem JE, Cohen JV, Chandra S, Menzer C, Ye F et al (2018) Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 4(12):1721–1728. https://doi.org/10.1001/jamaoncol.2018.3923
Weilandt J, Diehl K, Schaarschmidt ML, Kiecker F, Sasama B, Pronk M et al (2021) Patient preferences for treatment of advanced melanoma: impact of comorbidities. J Dtsch Dermatol Ges 19(1):58–70. https://doi.org/10.1111/ddg.14293
Weiss J, Kirchberger MC, Heinzerling L (2020) Therapy preferences in melanoma treatment- willingness to pay and preference of quality versus length of life of patients, physicians, healthy individuals and physicians with oncological disease. Cancer Med 9(17):6132–6140. https://doi.org/10.1002/cam4.3191
Zhang M, He X, Wu J, Xie F (2023) Differences between physician and patient preferences for cancer treatments: a systematic review. BMC Cancer 23(1):1126. https://doi.org/10.1186/s12885-023-11598-4
Funding
Open Access funding enabled and organized by Projekt DEAL. The work was supported by Novartis.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Katharina C. Kähler and Christine Blome. The first draft of the manuscript was written by Katharina C. Kähler and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
KCK serves as consultant to Philogen, BMS, MSD, Sanofi Aventis, Immunocore and received travel grants and speaker fees from Philogen, Pierre Fabre, BMS, MSD, Sun Pharma, Sanofi Aventis, Novartis, Medac and has received research support by Novartis. RG reports grants or contracts from Novartis, Sun Pharma, Amgen, Sanofi, Merck-Serono, Kyowa-Kirin, and Almirall-Hermal; payment or honoraria for lectures, presentation, manuscript writing or educational events from Roche Pharma, Bristol Myers Squibb, Novartis, Merck Sharp & Dohme, Almirall-Hermal, Amgen, and Merck-Serono; support for attending meetings and/or travel from Sun Pharma, Pierre Fabre, and Boehringer-Ingelheim; participation on a data safety monitoring board or advisory board for Roche Pharma, Bristol Myers Squibb, Novartis, Merck Sharp & Dohme, Almirall-Hermal, Amgen, Pierre Fabre, Merck-Serono, Sun Pharma, Merck-Serono, Sanofi, 4SC and Immunocore. YA received honoraria and travel grants from BMS, MSD, Novartis, Almirall Hermal, SUN, Sanofi, Pierre-Fabre. EL served as consultant and/or has received honoraria from Bristol-Myers Squibb, Merck Sharp & Dohme, Novartis, Pierre-Fabre, Sanofi, Sunpharma, Takeda and travel support from Bristol-Myers Squibb, Pierre- Fabre, Sunpharma and Novartis, outside the submitted work. GL received travel support from Sun Pharma, Pierre Fabre, research funding from Novartis. FM served as consultant and/or has received honoraria from Novartis, Bristol-Myers Squibb, Merck Sharp & Dohme, Pierre Fabre, Sanofi Genzyme, Sun Pharma and travel support from Novartis, Sun Pharma, Pierre Fabre and Merck Sharp & Dohme, outside the submitted work. DARS served as consultant and/or has received honoraria from BMS, MSD, Pierre Fabre, Sanofi Genzyme, Roche, Novartis, Sun Pharma. SWF has no conflicts. DN has no conflicts. CL served for advisory Boards and received speakers fees and travel reimbursement from BMS, MSD, Merck, Almirall Hermal, Sanofi, Immunocore, Sun Pharma, Biontech, Pierre Fabre, Merck, Novartis. JCH served for advisory boards and received speakers fees and travel reimbursement from Amgen, BMS, Delcath, GSK, Immunocore, MSD, Novartis, Onkowissen, Pierre Fabre, Sanofi, Sunpharma. MMS has received consulting fees from Novartis and Sanofi. LVM has served as advisor and/or received speaking fees and/or participated in clinical trials sponsored by Almirall, Amgen, Eli Lilly, Incyte, MSD, Novartis, Pierre Fabre, Roche, and Sanofi outside of the current work. LH Lucie Heinzerling declares speakers and advisory board honoraria from Bristol-Myers Squibb GmbH & Co. KGaA, Immunocore Ireland Ltd, Kyowa Kirin GmbH, MSD Sharp & Dohme GmbH, Novartis Pharma GmbHm Pieris Pharmaceuticals, Pierre Fabre Pharma GmbH, Sanofi-Aventis Deutschland GmbH, Stemline Therapeutics Switzerland GmbH, SUN Pharmaceutical Europe Industries BV, Therakos (UK) LTD. Patents: IL-12 plasmid DNA; VEGF-D for lymphangiogenesis; soluble prognostic marker for melanoma. Clinical studies within the institution: Agenus, AstraZeneca Inc., Bristol Myers Squibb, Huya Bioscience, IO Biotech, Merck Sharp & Dohme GmbH, Pfizer, Pierre Fabre, Regeneron, Replimune, Sanofi Aventis. MVH has received honoraria from Sanofi, Almirall, Biofrontera, Galderma, Novartis, BMS, MSD, Roche, Immunocore, Sun Pharmaceuticals, Pierre Fabre. CC has no conflicts. JR has no conflicts. CB has received speaker honoraria, research grants and/or awards from Amgen/Celgene, AstraZeneca, Bauerfeind, Hartmann, Helios Klinik Leisnig, Janssen-Cilag, Kreussler, Lilly, Mapi Group, medi, Pfizer, Stiefel Laboratories, The EuroQol Group, UCB, and Urgo.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Christian-Albrechts-University Kiel (2nd March 2020/D435/20).
Consent to participate
All patients have given written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An abstract containing parts of the submitted data has been accepted as poster at the ASCO Annual Meeting in 2022.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kähler, K.C., Gutzmer, R., Angela, Y. et al. Preferences of physicians for treatment-related toxicity vs. recurrence in melanoma (GERMELATOX-A): the doctors’ perspective. J Cancer Res Clin Oncol 150, 252 (2024). https://doi.org/10.1007/s00432-024-05713-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05713-6