Abstract
Purpose
Despite advanced technologies in breast cancer management, challenges remain in efficiently interpreting vast clinical data for patient-specific insights. We reviewed the literature on how large language models (LLMs) such as ChatGPT might offer solutions in this field.
Methods
We searched MEDLINE for relevant studies published before December 22, 2023. Keywords included: “large language models”, “LLM”, “GPT”, “ChatGPT”, “OpenAI”, and “breast”. The risk bias was evaluated using the QUADAS-2 tool.
Results
Six studies evaluating either ChatGPT-3.5 or GPT-4, met our inclusion criteria. They explored clinical notes analysis, guideline-based question-answering, and patient management recommendations. Accuracy varied between studies, ranging from 50 to 98%. Higher accuracy was seen in structured tasks like information retrieval. Half of the studies used real patient data, adding practical clinical value. Challenges included inconsistent accuracy, dependency on the way questions are posed (prompt-dependency), and in some cases, missing critical clinical information.
Conclusion
LLMs hold potential in breast cancer care, especially in textual information extraction and guideline-driven clinical question-answering. Yet, their inconsistent accuracy underscores the need for careful validation of these models, and the importance of ongoing supervision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Natural language processing (NLP) is increasingly used in healthcare, especially in oncology, for its ability to analyze free-text with diverse applications (Sorin et al. 2020a, b). Large language models (LLMs) like GPT, LLaMA, PaLM, and Falcon represent the pinnacle of this development, leveraging billions of parameters for highly accurate text processing (Sorin et al. 2020a, b; Bubeck et al. 2023). Despite this, the integration of such sophisticated NLP algorithms into practical healthcare settings, particularly in managing complex diseases like breast cancer, remains a technological, operational, and ethical challenge.
Breast cancer, the most common cancer among women, continues to pose significant challenges in terms of morbidity, mortality, and information overload (Kuhl et al. 2010; Siegel et al. 2019). While LLMs have shown promise in medical text analysis—with GPT-4 achieving a notable 87% success rate on the USMLE (Brin et al. 2023; Chaudhry et al. 2017) and extending its capabilities to image analysis (Sorin et al. 2023a, b, c)—their practical application in medicine and oncology in particular is still evolving.
We reviewed the literature on how large language models (LLMs) might offer solutions in breast cancer care.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher 2009). We searched the literature for applications of LLMs in breast cancer management using MEDLINE.
The search included studies published up to December 22nd 2023. Our search query was “(("large language models") OR (llm) OR (gpt) OR (chatgpt) OR (openAI)) AND (breast)”. The initial search identified 97 studies. To ensure thoroughness, we also examined the reference lists of the relevant studies. This, however, did not lead to additional relevant studies that met our inclusion criteria.
The criteria for inclusion were English language full-length publications that specifically evaluated the role of LLMs in breast cancer management. We excluded papers that addressed other general applications of LLMs in healthcare or oncology without a specific focus on breast cancer.
Three reviewers (VS, YA, and EKL) independently conducted the search, screened the titles, and reviewed the abstracts of the articles identified in the search. One discrepancy in the search results was discussed and resolved to achieve a consensus. Next, the reviewers assessed the full text of the relevant papers. In total, six publications met our inclusion criteria and were incorporated into this review. We summarized the results of the included studies, detailing the specific LLMs used, the utilized tasks, number of cases, along with publication details in a table format. Figure 1 provides a flowchart detailing the screening and inclusion procedure.
Quality was assessed by the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) criteria (Whiting 2011).
Results
All six studies included were published in 2023 (Table 1). All focused on either ChatGPT-3.5 or GPT-4 by OpenAI. Applications described include information extraction and question-answering. Three studies (50.0%) evaluated the performance of ChatGPT on actual patient data (Sorin et al. 2023a, b, c; Choi et al. 2023; Lukac et al. 2023), as opposed to two studies that used data from the internet (Rao et al. 2023; Haver et al. 2023). One study crafted fictitious patient profiles by the head investigator (Griewing et al. 2023).
Rao et al. and Haver et al. evaluated LLMs for breast imaging recommendations (Rao et al. 2023; Haver et al. 2023). Sorin et al., Lukac et al. and Griewing et al. evaluated LLMs as supportive decision-making tools in multidisciplinary tumor boards (Sorin et al. 2023a, b, c; Lukac et al. 2023; Griewing et al. 2023). Choi et al. used LLM for information extraction from ultrasound and pathology reports (Choi et al. 2023) (Fig. 2). Example cases for applications from studies are detailed in Table 2.
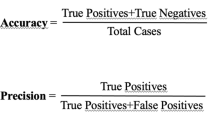
Accuracy of LLMs on different applications ranged from 50 to 98%. Best performance rates were achieved for information extraction and question-answering, with correct responses ranging from 88 to 98% (Choi et al. 2023; Rao et al. 2023) (Table 3). The lower performance was for clinical decision support in breast tumor boards, ranging between 50 and 70% (Sorin et al. 2023a, b, c; Lukac et al. 2023; Griewing et al. 2023). The range in performance on this task was wide between studies. However, the methods of the three studies also varied significantly (Sorin et al. 2023a, b, c; Lukac et al. 2023; Griewing et al. 2023). Sorin et al. and Lukac et al. used authentic patient data and compared ChatGPT-3.5 to the retrospective decisions in breast tumor board (Sorin et al. 2023a, b, c; Lukac et al. 2023). In both studies, the authors used reviewers that scored ChatGPT-3.5 responses (Sorin et al. 2023a, b, c; Lukac et al. 2023). (Griewing et al. 2023) crafted 20 fictitious patient files that were then discussed by a multidisciplinary tumor board. Their assessment was based on binary evaluation of various treatment approaches, including surgery, endocrine, chemotherapy, and radiation therapy. Griewing et al. were the only study providing insights into LLM performance on genetic testing for breast cancer treatment (Griewing et al. 2023). All three studies analyzed concordance between the tumor board and the LLM on different treatment options (Sorin et al. 2023a, b, c; Lukac et al. 2023; Griewing et al. 2023).
All studies discussed the limitations of LLMs in the contexts in which the algorithms were evaluated (Table 4). In all studies some of the information the models generated was false. When used as a support tool for tumor board, in some instances, the models overlooked relevant clinical details (Sorin et al. 2023a, b, c; Lukac et al. 2023; Griewing et al. 2023). Sorin et al. noticed absolute lack of referral to imaging (Sorin et al. 2023a, b, c), while Rao et al. who evaluated appropriateness of imaging noticed imaging overutilization (Rao et al. 2023). Some of the studies also discussed whether the nature of the prompt affects the outputs (Choi et al. 2023; Haver et al. 2023), and the difficulty to verify the reliability of the answers (Lukac et al. 2023; Rao et al. 2023; Haver et al. 2023).
According to the QUADAS-2 tool, all papers but one scored as high risk of bias for index test interpretation. For the paper by Lukac et al. the risk was unclear, refraining from a clear statement whether the evaluators were blinded to the reference standard. The study by Griewing et al. was the only one identified to have a low risk of bias across all categories (Griewing et al. 2023). The objective assessment of the risk of bias is reported in Supplementary Table 1.
Discussion
We reviewed the literature on LLMs applications related to breast cancer management and care. Applications described included information extraction from clinical texts, question-answering for patients and physicians, manuscript drafting and clinical management recommendations.
A disparity in performance was seen. The models showed proficiency in information extraction and responding to structured questions, with accuracy rates between 88 and 98%. However, their effectiveness diminished down to 50–70% in making clinical decisions, underscoring a gap in their application. In breast cancer care, attention to detail is crucial. LLMs excel at processing medical information quickly. However, currently, they may be less adept at navigating complex treatment decisions. Breast cancer cases vary greatly, each case distinguished by a unique molecular profile, clinical staging, and patient-specific requirements. It is vital for LLMs to adapt to the individual patient. While these models can assist physicians in routine tasks, they require further development for personalized treatment planning.
Interestingly, half of the studies included real patients’ data as opposed to publicly available data or fictitious data. For the overall published literature on LLMs in healthcare, there are more publications evaluating performance on public data. This includes performance on board examinations and question-answering based on guidelines (Sallam 2023). These analyses may introduce contamination of data, since LLMs were trained on vast data from the internet. For commercial models such as ChatGPT, the type of training data is not disclosed. Furthermore, these applications do not necessarily reflect on the performance of these models in real-world clinical settings.
While some claim that LLMs may eventually replace healthcare personnel, currently, there are major limitations and ethical concerns that strongly suggest otherwise (Lee et al. 2023). Using such models to augment physicians’ performance is more practical, albeit also constrained by ethical issues (Shah et al. 2023). LLMs enable automating different tasks that traditionally required human effort. The ability to analyze, extract and generate meaningful textual information could potentially decrease some physicians’ workload and human errors.
Reliance on LLMs and potential integration in medicine should be made with caution. The limitations discussed in the studies further underscore this note. These models can generate false information (termed “hallucination”) which can be seamlessly and confidently integrated into real information (Sorin et al. 2020a, b). They can also perpetuate disparities in healthcare (Sorin et al. 2021; Kotek et al. 2023). The inherent inability to trace the exact decision-making process of these algorithms is a major challenge for trust and clinical integration (Sorin et al. 2023a, b, c). LLMs can also be vulnerable to cyber-attacks (Sorin et al. 2023a, b, c).
Furthermore, this study highlights the absence of uniform assessment methods for LLMs in healthcare, underlining the need of establishing methodological standards for evaluating LLMs. The goal is to enhance the comparability and quality of research. The establishment of such standards is critical for the safe and effective integration of LLMs into healthcare, especially for complex conditions like breast cancer, where personalized patient care is essential.
This review has several limitations. First, due to the heterogeneity of tasks evaluated in the studies, we could not perform a meta-analysis. Second, all included studies assessed ChatGPT-3.5, and only one study evaluated GPT-4. There were no publications identified on other available LLMs. Finally, generative AI is currently a rapidly expanding topic. Thus, there may be manuscripts and applications published after our review was performed. LLMs are continually being refined, and so is their performance.
To conclude, LLMs hold potential for breast cancer management, especially in text analysis and guideline-driven question-answering. Yet, their inconsistent accuracy warrants cautious use, following thorough validation and ongoing supervision.
Data availability
Reviewed studies and their results can be located at PubMed database: https://pubmed.ncbi.nlm.nih.gov/
References
Brin D, Sorin V, Konen E, Nadkarni G, Glicksberg BS, Klang E (2023) How large language models perform on the united states medical licensing examination: a systematic review. medRxiv 23:543
Bubeck S, Chandrasekaran V, Eldan R, et al. (2023) Sparks of artificial general intelligence: Early experiments with gpt-4. arXiv preprint arXiv:2303.12712
Chaudhry HJ, Katsufrakis PJ, Tallia AF (2020) The USMLE step 1 decision. JAMA 323(20):2017
Choi HS, Song JY, Shin KH, Chang JH, Jang B-S (2023) Developing prompts from large language model for extracting clinical information from pathology and ultrasound reports in breast cancer. Radiat Oncol J 41(3):209–216
Decker H, Trang K, Ramirez J et al (2023) Large language Model−based Chatbot vs Surgeon-generated informed consent documentation for common procedures. JAMA Netw Open 6(10):e2336997
Griewing S, Gremke N, Wagner U, Lingenfelder M, Kuhn S, Boekhoff J (2023) Challenging ChatGPT 3.5 in senology-an assessment of concordance with breast cancer tumor board decision making. J Pers Med 13(10):1502. https://doi.org/10.3390/jpm13101502
Haver HL, Ambinder EB, Bahl M, Oluyemi ET, Jeudy J, Yi PH (2023) Appropriateness of breast cancer prevention and screening recommendations provided by ChatGPT. Radiology. https://doi.org/10.1148/radiol.230424
Jiang LY, Liu XC, Nejatian NP et al (2023) Health system-scale language models are all-purpose prediction engines. Nature 619(7969):357–362
Kotek H, Dockum R, Sun DQ (2023) Gender bias and stereotypes in Large Language Models. arXiv preprint arXiv:2308.14921
Kuhl C, Weigel S, Schrading S et al (2010) Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J Clin Oncol 28(9):1450–1457
Lee P, Drazen JM, Kohane IS, Leong T-Y, Bubeck S, Petro J (2023) Benefits, limits, and risks of GPT-4 as an AI Chatbot for medicine. N Engl J Med 388(13):1233–1239
Lukac S, Dayan D, Fink V et al (2023) Evaluating ChatGPT as an adjunct for the multidisciplinary tumor board decision-making in primary breast cancer cases. Arch Gynecol Obstet 308(6):1831–1844
Moher D (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(4):264
Rao A, Kim J, Kamineni M et al (2023) Evaluating GPT as an adjunct for radiologic decision making: GPT-4 versus GPT-3.5 in a breast imaging pilot. J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2023.05.003
Sallam M (2023) ChatGPT utility in healthcare education, research, and practice: systematic review on the promising perspectives and valid concerns. Healthcare 11(6):887
Shah NH, Entwistle D, Pfeffer MA (2023) Creation and adoption of large language models in medicine. JAMA 330(9):866
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34
Sorin V, Klang E (2021) Artificial intelligence and health care disparities in radiology. Radiology 301(3):E443–E443
Sorin V, Klang E (2023) Large language models and the emergence phenomena. Eur J Radiol Open 10:100494
Sorin V, Barash Y, Konen E, Klang E (2020a) Deep-learning natural language processing for oncological applications. Lancet Oncol 21(12):1553–1556
Sorin V, Barash Y, Konen E, Klang E (2020b) Deep learning for natural language processing in radiology—fundamentals and a systematic review. J Am Coll Radiol 17(5):639–648
Sorin V, Klang E, Sklair-Levy M et al (2023) Large language model (ChatGPT) as a support tool for breast tumor board. npj Breast Cancer. https://doi.org/10.1038/s41523-023-00557-8
Sorin V, Barash Y, Konen E, Klang E (2023a) Large language models for oncological applications. J Cancer Res Clin Oncol 149(11):9505–9508
Sorin V, Soffer S, Glicksberg BS, Barash Y, Konen E, Klang E (2023b) Adversarial attacks in radiology—a systematic review. Eur J Radiol 167:111085
Sorin V, Glicksberg BS, Barash Y, Konen E, Nadkarni G, Klang E (2023) Diagnostic accuracy of GPT multimodal analysis on USMLE questions including text and visuals. MedRxiv 10(2029):23297733
Temsah M-H, Altamimi I, Jamal A, Alhasan K, Al-Eyadhy A (2023) ChatGPT surpasses 1000 publications on PubMed: envisioning the road ahead. Cureus. https://doi.org/10.7759/cureus.44769
Whiting PF (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155(8):529
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Vera Sorin, Eyal Klang and Yaara Artsi. The first draft of the manuscript was written by Vera Sorin and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This is an observational study. No ethical approval was required.
Human participants and/or animals
This is a systematic review. No human and/or animals participated in this study.
Informed consent
This is a systematic review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sorin, V., Glicksberg, B.S., Artsi, Y. et al. Utilizing large language models in breast cancer management: systematic review. J Cancer Res Clin Oncol 150, 140 (2024). https://doi.org/10.1007/s00432-024-05678-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05678-6