Abstract
Purpose
The decision-making process regarding cancer treatment is emotionally challenging for patients and families, harboring the risk of decision regret. We aimed to explore prevalence and determinants of decision regret following radiotherapy.
Methods
This cross-sectional observational study was conducted at a tertiary cancer center to assess decision regret following radiotherapy. The study employed the German version of the Ottawa Decision Regret Scale (DRS) which was validated in the study population. Decision regret was categorized as absent (0 points), mild (1–25 points), and strong (> 25 points). Various psychosocial outcome measures were collected using validated questionnaires to identify factors that may be associated with decision regret.
Results
Out of 320 eligible patients, 212 participated, with 207 completing the DRS. Median age at start of radiotherapy was 64 years [interquartile range (IQR), 56–72], genders were balanced (105 female, 102 male), and the most common cancer types were breast (n = 84; 41%), prostate (n = 57; 28%), and head-and-neck cancer (n = 19; 9%). Radiotherapy was applied with curative intention in 188 patients (91%). Median time between last radiotherapy fraction and questionnaire completion was 23 months (IQR, 1–38). DRS comprehensibility was rated as good or very good by 98% (196 of 201) of patients. Decision regret was reported by 43% (n = 90) as absent, 38% (n = 78) as mild, and 18% (n = 38) as strong. In the multiple regression analysis, poor Eastern Cooperative Oncology Group performance status, low social support, and dissatisfaction with care were independent risk factors for higher decision regret after radiotherapy.
Conclusions
The German version of the DRS could be used to assess decision regret in a diverse cohort of cancer patients undergoing radiotherapy. Decision regret was prevalent in a considerable proportion of patients. Further studies are necessary to validate these findings and obtain causal factors associated with decision regret after radiotherapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Decision regret is a multifaceted emotional response encompassing feelings of disappointment and remorse concerning the choices made during the treatment decision-making process (Landman 1987). It can be described as a feeling that opting for a different course of action would have resulted in a more favorable outcome in the current situation (Coricelli et al. 2007). This adverse emotional sensation can arise when uncertainty surrounding the optimal choice remains unresolved or when an undesirable outcome prompts the belief that an alternative decision might have been more beneficial (Joseph-Williams et al. 2011). This phenomenon is particularly pertinent in the field of oncology, where treatment decisions often carry profound implications for patients' lives (Connolly and Reb 2005). Prevalence and determinants of decision regret were studied in several cancer types, such as prostate cancer (Wallis et al. 2022), breast cancer (Martinez et al. 2015), lung cancer (Sullivan et al. 2023), and head-and-neck cancer (Nallani et al. 2022). The Ottawa Decision Regret Scale (DRS) was initially developed by Brehaut and colleagues and has demonstrated its validity and reliability as a measurement tool for decision regret (Brehaut et al. 2003).
Radiotherapy is a cornerstone in cancer treatment, and about 50% of all cancer patients in Europe undergo at least one course of radiotherapy during their disease (Lievens et al. 2020). While numerous studies have explored decision regret in various healthcare settings, its prevalence and determinants in the context of radiotherapy remain underexplored (de Groot et al. 2012; Nallani et al. 2022; Windon et al. 2019; Zoumpou et al. 2023). Decision regret for (1) not omitting radiotherapy after surgery (e.g., in older women with low-risk breast cancer (Kunkler et al. 2023)), (2) for not deciding to undergo primary surgery instead of radical radiotherapy [e.g., in men with localized prostate cancer (Hamdy et al. 2023)], (3) for not opting for a different radiotherapy fractionation schedule [e.g., short-course neoadjuvant radiotherapy instead of long-course neoadjuvant chemoradiation in patients with rectal cancer (Ciseł et al. 2019)] or (4) for a less aggressive radiotherapy regimen (e.g., omitting radiotherapy boost to the tumor bed or omitting coverage of the elective lymph nodes in women with breast cancer (Bartelink et al. 2015)) are only some examples that may occur in patients after radiotherapy. Understanding the factors contributing to decision regret after radiotherapy is crucial not only for enhancing patient satisfaction and well-being but also for refining the shared decision-making process between patients and healthcare providers.
Decision regret may be dependent on cultural differences (Hawley and Morris 2017; López et al. 2014; Shaw et al. 2015), providing a rationale to examine this issue separately for individual countries. However, there is a paucity of studies about decision regret after radiotherapy in cancer patients in Germany (Köksal et al. 2023, 2022). We therefore aimed at investigating the prevalence and determinants of decision regret in cancer patients who were treated with radiotherapy for their disease at a large tertiary German cancer center. Previous studies have found relationships between decision regret and various patient-reported outcomes, such as quality of life (Calderon et al. 2019), distress, depression, anxiety (Sheehan et al. 2007), perception of the decision-making process (Yamauchi et al. 2019), satisfaction with care (Berkowitz et al. 2021), social support (Wallis et al. 2022), and health literacy (Joyce et al. 2020), wherefore we also surveyed these patient-reported psychosocial outcome measures to find potential variables that are associated with decision regret. We also aimed to examine the reliability of the German version of the DRS in a broad group of cancer patients, in order to facilitate its usage in subsequent studies.
Materials and methods
Study design
This was a cross-sectional observational study performed at the Department of Radiation Oncology, Leipzig University Medical Center. Inclusion criteria for this study were (1) at least one course of radiotherapy for a malignant disease, (2) age of ≥ 18 years, (3) the ability to understand the German questionnaires, and (4) informed consent to participate in this study. Cancer patients who attended follow-up appointments after radiotherapy between July 10, 2023 and August 18, 2023 in the outpatient clinic of the Department of Radiation Oncology, Leipzig University Medical Center, were eligible for the study and were actively asked to participate in the study. Participating patients were able to either fill out the questionnaires during the waiting time for the medical consultation, or at home after the follow-up appointment. The study was approved in advance by the local ethics committee (reference number 077/23-ek) and was performed in accordance with the declaration of Helsinki. All patients provided written informed consent.
Questionnaires and variables
The German version of the 5-item Ottawa DRS (Brehaut et al. 2003), which has previously been validated concerning decision regret in patient caregivers [DRS-C (Haun et al. 2019)], was used in this study. A forward translation of the original DRS was also performed (A.M.T.) and results were compared with the existing German DRS-C. The German DRS-C and the independently translated DRS were almost identical, so that we decided to use the same wording as the German DRS-C in order to ensure comparability. The German version of the DRS is shown in the Supplementary Material. DRS scores range from 0 to 100, with 0 indicating no regret and 100 indicating a high degree of regret. Following the previous validation study of the Ottawa DRS, degree of decision regret was subdivided into absent (0 points), mild (1–25 points), and strong (> 25 points) decision regret (Brehaut et al. 2003). In addition, patients were asked to indicate the comprehensibility and explicitness of the DRS using 5 questions, each with a 5-point Likert scale (Supplementary Material). For reliability analysis, Cronbach's alpha was calculated to assess the internal consistency. In order to find determinants of decision regret, various patient-reported psychosocial outcome measures were collected. Quality of life was measured with the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 (Aaronson et al. 1993) questionnaire, and distress was assessed with the German version of the National Comprehensive Cancer Network (NCCN) distress thermometer ranging from 0 (no distress) to 10 (extreme distress) (Mehnert et al. 2006). Depression and anxiety were measured using the German versions of the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al. 2001) and Generalized Anxiety Disorder Screener (GAD-7) (Spitzer et al. 2006), respectively. Patients' experiences concerning participation in the decision-making process of radiation treatment were examined using the Shared Decision Making Questionnaire (SDM-Q-9) (Kriston et al. 2010), and patient satisfaction with care during radiotherapy was quantified with the Satisfaction with Comprehensive Cancer Care (SCCC) questionnaire (Esser et al. 2021). Here, patients were explicitly asked to answer these questionnaires according to their last radiotherapy course. Assessment of social support was performed with the SSUK-8 (Ullrich and Mehnert-Theuerkauf 2010), while health literacy was assessed with the HLS-EU-Q16 (Niedorys et al. 2020). Only paper questionnaires were used in the study. In addition, patient and treatment characteristics regarding the last course of radiotherapy were retrospectively extracted from the medical records. Tumor stage at the time of radiotherapy was indicated based on the current staging classification system at that time. Possible radiotherapy-related toxicities at the time of study participation were classified according to the Common Terminology Criteria for Adverse Events (CTCAE) v5.0.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics version 29 (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to display the study cohort. To investigate the univariate relationships between distress and covariates, Pearson correlations and one-way analysis of variance (ANOVA) tests were employed based on the scale of the respective covariate. If the one-way ANOVA yielded significant results, Tukey’s post hoc testing was applied. For exploring the multivariable connections between decision regret and covariates, a linear regression with decision regret as dependent variable was performed. In the regression analysis, listwise deletion of missing data was performed (i.e., complete-case analysis). Assumptions of a linear regression analysis (linearity, normality, homoscedasticity, absence of multi-collinearity, uncorrelatedness of residuals) were checked. Details of the model performance and the assumption test results are shown in the Supplementary Material. Considering the exploratory nature of our analyses, we did not perform adjustments for multiple testing. A p value of < 0.05 was considered statistically significant for all analyses.
Results
Study flow diagram
This cross-sectional study recruited a total of 212 patients out of 320 eligible patients (66% response rate) (Fig. 1). Of these 212 patients, 207 completed the DRS and were included in the final analysis. A comparison between patients who refused to participate in the study and patients who agreed to participate is shown in the Supplementary Table 1. While age, gender, and primary cancer were not significantly different between participants and non-participants, Eastern Cooperative Oncology Group (ECOG) performance status was significantly worse in non-participants (p < 0.001, χ2-test).
Characteristics of the study cohort
Patient and treatment characteristics are shown in Table 1. The median age of the participants was 64 years (IQR, 56–72), with a balanced distribution of gender (n = 105 female, n = 102 male). The most prevalent cancer types were breast cancer (n = 84; 41%), prostate cancer (n = 57; 28%), and head-and-neck cancer (n = 19; 9%). Curative radiotherapy (including radiotherapy for oligo-metastatic disease) was administered to 188 patients (91%), while the remaining 19 patients (9%) underwent palliative treatment. The median number of treatment fractions was 25 (IQR, 18–31). Concomitant chemotherapy, hormone deprivation therapy, and novel targeted therapies including immune checkpoint inhibitors were applied in 23 (11%), 70 (34%), and 4 patients (2%), respectively. The majority of patients (n = 171; 83%) had been treated as outpatients. The median interval between radiotherapy and questionnaire completion was 23 months (IQR, 1–38 months).
Test characteristics of the German version of the DRS
DRS comprehensibility was rated as good or very good by 98% (196 of 201) of patients (Table 2). The vast majority agreed with the statement “it is clear to which decision the questions refer” {mean [standard deviation (SD)] 1.70 [0.73]} on a 5-point Likert scale ranging from 1 to 5. Twenty-nine out of 200 patients (15%) stated that answering the DRS distressed them very or quite significantly.
Internal consistency of the German version of the DRS as measured by Cronbach’s α was 0.76 (95% CI, 0.70–0.81).
Prevalence and determinants of decision regret
The distribution of decision regret among cancer patients who had received radiotherapy for their disease is shown in Fig. 2. The mean and the median value of decision regret on the DRS, which ranges from 0 to 100 points, were 13.62 (SD, 18.73) and 5 points (IQR, 0–20), respectively. Decision regret was denied by 43% (n = 90), whereas 38% (n = 79) reported mild decision regret, and 18% (n = 38) strong decision regret.
Distribution of decision regret (n = 207). A Histogram showing both absolute and relative frequencies regarding the level of decision regret, as assessed using the German version of the Decision Regret Scale. B Pie chart showing the frequency of absent (0 points), mild (1–25 points), and strong (> 25 points) decision regret after radiotherapy
Decision regret inversely correlated with global quality of life (Pearson’s r = − 0.26, p < 0.001), patient involvement in the decision-making process (r = − 0.22, p < 0.01), satisfaction with care (r = − 0.36, p < 0.001), social support (r = − 0.33, p < 0.001), and health literacy (r = − 0.29, p < 0.001) (Table 3). There was a positive correlation of decision regret with distress (r = 0.17, p < 0.05), depression (r = 0.27, p < 0.001), and anxiety (r = 0.23, p < 0.01).
In the univariate analyses in which the associations of several categorical variables with decision regret were analyzed using one-way ANOVA tests, male gender (p < 0.05), poor ECOG performance status at the follow-up consultation (p < 0.001), primary cancer type (p < 0.001), and hospitalization during radiotherapy (p < 0.05) were associated with higher levels of decision regret (Table 4). In the post hoc Tukey’s test, patients with head-and-neck cancer were found to exhibit significantly higher levels of patient-reported decision regret compared to patients with breast or prostate cancer (both p < 0.05). Neither development of radiotherapy-induced high-grade (grade 3 or 4 according to CTCAE v5.0) toxicities (p = 0.125) nor tumor progression at the time of the time of study participation (p = 0.281) were associated with decision regret, although it should be pointed out that the number of patients with high-grade toxicities (n = 12) and with progressive disease (n = 8) were small. Among continuous variables, neither age (r = 0.05, p = 0.507) nor number of treatment fractions (r = 0.03, p = 0.707) were associated with decision regret. The time between end of radiotherapy and study participation did also not influence the extent of decision regret in our cohort (r = − 0.08, p = 0.246). In line with this, there was also no association with decision regret, if time between last day of course of radiotherapy and questionnaire completion was analyzed as an ordinal variable with 6-month and 12-month intervals (p = 0.443).
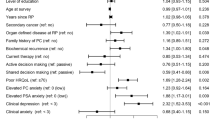
All parameters that were significantly associated with decision regret in the univariate analysis were simultaneously entered into a linear regression model with decision regret as dependent variable. The linear regression model significantly predicted decision regret (F(12,183) = 7.421, p < 0.001, adj. R2 = 0.283). A poorer ECOG performance status (β = 0.197; p < 0.01), lower social support (β = − 0.236; p < 0.001) and lower satisfaction with care (β = − 0.236; p < 0.001) remained independent risk factors for decision regret after radiotherapy (Table 5).
Discussion
In this single-center cross-sectional observational study performed at a large German tertiary cancer center, more than half of the investigated patients (56%) reported some form of decision regret, with 18% feeling strong decision regret after radiation treatment. Both comprehensibility and explicitness of the German version of the DRS were considered good by the participating patients, and the internal consistency as assessed with Cronbach’s α was acceptable. Higher ECOG performance status at the follow-up consultation, lower social support, and lower satisfaction with care were associated with decision regret in the multiple regression analysis.
There is a paucity of data regarding the prevalence of decision regret after radiotherapy in the German healthcare system (Köksal et al. 2023, 2022). Köksal et al. reported a strong decision regret prevalence of 13.9% after adjuvant radiotherapy in a cohort of 172 patients with breast cancer treated at a German tertiary cancer center (Köksal et al. 2023). This is well comparable to the prevalence of strong decision regret in the subgroup of breast cancer patients in our study (8 out of 84 patients [10%] with strong decision regret). In a further study, Köksal and colleagues examined the prevalence of decision regret in a group of 108 patients with head-and-neck cancer who were treated with surgery and adjuvant radiotherapy (Köksal et al. 2022). While 40.5% reported no decision regret, 30.1% indicated mild decision regret, and 29.4% even strong decision regret. Strong decision regret was reported by about half of head-and-neck cancer patients in our cross-sectional study (47%), but results should be interpreted very cautiously due to the low number of head-and-neck cancer patients in our study (n = 19). However, a further study also observed relatively high rates of decision regret in head-and-neck cancer patients, namely about one third of patients reporting strong decision regret at 3 and 6 months after cancer treatment (Nallani et al. 2022). The relatively high prevalence of decision regret observed in patients with head-and-neck cancer could be attributed, in part, to the fact that both definitive (chemo)radiation and surgery with risk-adapted adjuvant (chemo)radiation represent comparable treatment approaches for a significant subset of head-and-neck cancer subtypes (Henriques De Figueiredo et al. 2016; Nichols et al. 2022; Pakkanen et al. 2022; Palma et al. 2022), so that the decision-making process is stressful for the patients which increases the risk of subsequent decision regret. It has been shown that higher decisional conflict is a risk factor for later decision regret (Becerra Pérez et al. 2016), making decision support interventions such as patient-centered treatment decision aids a promising strategy to mitigate decisional conflict and subsequent regret (Bigelow et al. 2021; Stacey et al. 2017; Windon et al. 2021). In the observational study concerning decision regret in head-and-neck cancer patients from Nallani and colleagues, higher decision regret was associated with advanced disease stage at presentation, primary non-surgical treatment, and lower health literacy (Nallani et al. 2022). If further studies validate these relatively high rates of decision regret after radiotherapy in head-and-neck cancer patients, there is a need to develop multi-professional strategies to reduce decision regret in this vulnerable population.
Satisfaction with care was found to be inversely correlated with decision regret in our cohort. However, given the cross-sectional observational design of our study, it is not possible to unequivocally indicate a causal effect. While low satisfaction with radiotherapy could in theory causally contribute to higher rates of decision regret, it may also be conceivable that strong decision regret may result in higher post-hoc perceived dissatisfaction with care. A recent large multicenter study observed relatively high satisfaction with radiotherapy care in Germany (Fabian et al. 2023). Tumor entity, treatment center, and quality of life were independent determinants of patient satisfaction with radiotherapy care in this study. The fact that the treatment center itself was reported as a major determinant of patient satisfaction with radiotherapy care in the study of Fabian et al. highlights the importance of regular patient satisfaction assessment as part of the internal quality management. Indeed, regular assessments of patient satisfaction are required in the quality management guideline of the Federal Joint Committee (Gemeinsamer Bundesausschuss, G-BA) (Boywitt et al. 2022).
Lack of social support which was measured with the SSUK-8 was another variable that was associated with decision regret in the multiple regression analysis. In a recent population-based, prospective cohort study of 2072 patients with localized prostate cancer, social support at baseline was also found to be associated with decision regret after treatment (Wallis et al. 2022). Furthermore, a systematic review by Szproch and Maguire identified lack of social support with higher levels of decision regret after cancer treatment (Szproch and Maguire 2022). Recommending or referring patients to the psycho-oncology service as well as connecting patients with existing support groups may improve perceived social support (Korotkin et al. 2019; Sautier et al. 2014). Psychosocial care in which both the patient and his or her partner and family are addressed may also improve this outcome measure (Hartmann et al. 2010; Lorenz et al. 2019). However, especially cancer patients experiencing loneliness and social isolation remain a challenging population who suffer from low perceived social support, which is difficult to address even with psycho-oncologic interventions (Deckx et al. 2014; Hogan et al. 2002). Further prospective studies in which decision regret is assessed longitudinally are needed to further examine the relationship between social support and decision regret.
ECOG performance status at the time of questionnaire completion was found to be linked with decision regret in our study. There are various potential patient and treatment characteristics that can deteriorate patients’ ECOG performance status, e.g., higher age, presence of treatment-related adverse events, higher tumor stage, and tumor recurrence, etc. (Corrêa et al. 2012; Datta et al. 2019). As non-participants of the study exhibited a worse ECOG performance status than participants, the exact rate of decision regret may even be higher, although this remains speculative. Furthermore, it cannot be ruled out that patients at the end of their life tend to exhibit higher decision regret, as they might feel regret to have wasted their lifetime with cancer treatments that did not lead to long-term survival. Again, longitudinal analyses of decision regret including mixed-methods design and with linkage to progression-free survival are required to further elaborate on this issue and to explore reasons for decision regret after radiotherapy in more detail.
Patients who experience regret often retrospectively report being insufficiently informed (Hoffman et al. 2017; Morris et al. 2015), and patients' experiences concerning participation in the decision-making process were inversely correlated with decision regret at least in the univariate analysis of our cross-sectional study (r = − 0.22, p < 0.01). The relationship between the extent of patient participation in the decision-making process and the hazard of post-treatment decision regret is considered to be complex. While numerous studies indicate that patients actively participating in decision-making experience lower regret compared to those in passive roles (Wilding et al. 2020; Wollersheim et al. 2020), others reported opposite findings (Livaudais et al. 2013; Wagland et al. 2019). Chichua and colleagues suppose that decisional regret is linked not to the preferred or adopted role in the decision-making process, but to the discrepancy between them (Chichua et al. 2022). Both involuntary passive and active roles can result in increased regret (Mancini et al. 2012; Wagland et al. 2019). While active participation allows realistic expectations and preference expression, patients' health literacy must be considered (Joyce et al. 2020). In a study with 368 early breast cancer patients, too much perceived responsibility was associated with less baseline treatment knowledge and increased decision regret (Livaudais et al. 2013). Clinicians should therefore consider assessing patients' decisional capacity and preferences when offering recommendations and support (Chichua et al. 2022).
The participating patients found the comprehensibility of the German version of the DRS to be good, and the internal consistency, evaluated using Cronbach's α, was deemed acceptable. In comparison with the original DRS and the Japanese version of the DRS, internal consistency was a bit lower [Cronbach’s α of 0.76 in our study versus 0.81–0.92 in the original DRS (Brehaut et al. 2003) versus 0.85 in the Japanese version (Tanno et al. 2016)]. The German version of the DRS for caregivers (DRS-C), which was investigated in a cohort of caregivers of deceased people with cancer, also had a good internal consistency with a Cronbach’s α of 0.83 (Haun et al. 2019). Importantly, the comprehensibility of the DRS was indicated as good or very good by 98% in our cohort, supporting the usage of this questionnaire in subsequent studies.
Even though this cross-sectional study is the largest study examining the prevalence of decision regret after radiotherapy in Germany with a fairly good response rate, there are some limitations of the analysis. First, sampling error could have occurred, as the collected data originate from only a portion of the overall population who received radiotherapy in our institution. We attempted to partly address this issue by comparing the key demographic variables between participants and non-participants. Second, the missing longitudinal analysis of the degree of decision regret over time prevents an in-depth analysis about the duration of decision regret after radiotherapy. In a large longitudinal analysis about decision regret in patients with prostate cancer, the percentage of patients reporting regret increased over time in patients who were treated with radiotherapy, whereas it decreased in patients undergoing active surveillance (Hurwitz et al. 2017). Another study found relatively stable rates of decision regret over time in patients with localized breast cancer (Martinez et al. 2015). Third, given the single-center approach of our study, caution is warranted regarding the generalizability and transferability of our results to other centers in Germany. As patients with breast cancer (41%) and prostate cancer (28%) comprise the majority of patients treated with radiotherapy, our analyses regarding decision regret in patients with other cancer types are limited by the low patient number for those cancer types, so that multi-center studies with larger sample sizes are required. In this context, it has also to be mentioned that patients who had received radiotherapy with palliative intention were underrepresented in our cohort, so that transferability of our findings to this cohort is complicated. Last, recall bias may have occurred when patients were asked about their satisfaction with radiotherapy care as well as their involvement in the decision-making process, as median time between last day of radiotherapy and questionnaire completion was 23 months.
Conclusions
Almost a fifth of cancer patients in our cohort reported strong decision regret and more than half at least some form of decision regret regarding their last course of radiotherapy. Strong decision regret was associated with a poor performance status, low social support, and dissatisfaction with care. The German version of the DRS was found well understandable, supporting its usage in further studies. Additional research is needed to investigate risk factors for decision regret across various types of cancer.
Availability of data and material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Bartelink H, Maingon P, Poortmans P, Weltens C, Fourquet A et al (2015) Whole-breast irradiation with or without a boost for patients treated with breast-conserving surgery for early breast cancer: 20-year follow-up of a randomised phase 3 trial. Lancet Oncol 16:47–56
Becerra Pérez MM, Menear M, Brehaut JC, Légaré F (2016) Extent and predictors of decision regret about health care decisions: a systematic review. Med Decis Mak 36:777–790
Berkowitz R, Vu J, Brummett C, Waljee J, Englesbe M, Howard R (2021) The impact of complications and pain on patient satisfaction. Ann Surg 273:1127–1134
Bigelow EO, Windon MJ, Fakhry C, Kiess AP, Seiwert T, D’Souza G (2021) Development of a web-based, patient-centered decision aid for oropharyngeal cancer treatment. Oral Oncol 123:105618
Boywitt D, Klakow-Franck R, Heidecke C-D (2022) Qualität in der Gesundheitsversorgung sichern und weiterentwickeln: Maßnahmen und Perspektiven. Bundesgesundheitsblatt - Gesundheitsforschung - Gesundheitsschutz 65:270–276
Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L et al (2003) Validation of a decision regret scale. Med Decis Mak 23:281–292
Calderon C, Ferrando PJ, Lorenzo-Seva U, Higuera O, Ramon YCT et al (2019) Validity and reliability of the decision regret scale in cancer patients receiving adjuvant chemotherapy. J Pain Symptom Manag 57:828–834
Chichua M, Brivio E, Mazzoni D, Pravettoni G (2022) Shared decision-making and the lessons learned about decision regret in cancer patients. Support Care Cancer 30:4587–4590
Ciseł B, Pietrzak L, Michalski W, Wyrwicz L, Rutkowski A et al (2019) Long-course preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: long-term results of the randomized Polish II study. Ann Oncol 30:1298–1303
Connolly T, Reb J (2005) Regret in cancer-related decisions. Health Psychol 24:S29-34
Coricelli G, Dolan RJ, Sirigu A (2007) Brain, emotion and decision making: the paradigmatic example of regret. Trends Cogn Sci 11:258–265
Corrêa GT, Bandeira GA, Cavalcanti BG, Santos FB, Rodrigues Neto JF et al (2012) Analysis of ECOG performance status in head and neck squamous cell carcinoma patients: association with sociodemographical and clinical factors, and overall survival. Support Care Cancer 20:2679–2685
Datta SS, Ghosal N, Daruvala R, Chakraborty S, Shrimali RK et al (2019) How do clinicians rate patient’s performance status using the ECOG performance scale? A mixed-methods exploration of variability in decision-making in oncology. Ecancermedicalscience 13:913
de Groot J, Vernooij-Dassen M, Hoedemaekers C, Hoitsma A, Smeets W, van Leeuwen E (2012) Decision making by relatives about brain death organ donation: an integrative review. Transplantation 93:1196–1211
Deckx L, van den Akker M, Buntinx F (2014) Risk factors for loneliness in patients with cancer: a systematic literature review and meta-analysis. Eur J Oncol Nurs 18:466–477
Esser P, Sautier L, Sarkar S, Schilling G, Bokemeyer C et al (2021) Development and preliminary psychometric investigation of the German Satisfaction with Comprehensive Cancer Care (SCCC) Questionnaire. Health Qual Life Outcomes 19:147
Hamdy FC, Donovan JL, Lane JA, Metcalfe C, Davis M et al (2023) Fifteen-year outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med 388:1547–1558
Hartmann M, Bäzner E, Wild B, Eisler I, Herzog W (2010) Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: a meta-analysis. Psychother Psychosom 79:136–148
Haun MW, Schakowski A, Preibsch A, Friederich HC, Hartmann M (2019) Assessing decision regret in caregivers of deceased German people with cancer—a psychometric validation of the Decision Regret Scale for Caregivers. Health Expect 22:1089–1099
Hawley ST, Morris AM (2017) Cultural challenges to engaging patients in shared decision making. Patient Educ Couns 100:18–24
Henriques De Figueiredo B, Fortpied C, Menis J, Lefebvre JL, Barzan L et al (2016) Long-term update of the 24954 EORTC phase III trial on larynx preservation. Eur J Cancer 65:109–112
Hoffman RM, Lo M, Clark JA, Albertsen PC, Barry MJ et al (2017) Treatment decision regret among long-term survivors of localized prostate cancer: results from the prostate cancer outcomes study. J Clin Oncol 35:2306–2314
Hogan BE, Linden W, Najarian B (2002) Social support interventions: do they work? Clin Psychol Rev 22:383–442
Hurwitz LM, Cullen J, Kim DJ, Elsamanoudi S, Hudak J et al (2017) Longitudinal regret after treatment for low- and intermediate-risk prostate cancer. Cancer 123:4252–4258
Joseph-Williams N, Edwards A, Elwyn G (2011) The importance and complexity of regret in the measurement of “good” decisions: a systematic review and a content analysis of existing assessment instruments. Health Expect 14:59–83
Joyce DD, Heslop DL, Umoh JI, Brown SD, Robles JA et al (2020) Examining the association of health literacy and numeracy with prostate-related knowledge and prostate cancer treatment regret. Urol Oncol 38:682.e11–82.e19
Köksal M, Saur L, Scafa D, Sarria RG, Leitzen C et al (2022) Late toxicity-related symptoms and fraction dose affect decision regret among patients receiving adjuvant radiotherapy for head and neck cancer. Head Neck 44:1885–1895
Köksal M, Hoppe C, Schröder A-K, Scafa D, Koch D et al (2023) Decision regret in breast cancer patients after adjuvant radiotherapy. Breast 68:133–141
Korotkin BD, Hoerger M, Voorhees S, Allen CO, Robinson WR, Duberstein PR (2019) Social support in cancer: how do patients want us to help? J Psychosoc Oncol 37:699–712
Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M (2010) The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns 80:94–99
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613
Kunkler IH, Williams LJ, Jack WJL, Cameron DA, Dixon JM (2023) Breast-conserving surgery with or without irradiation in early breast cancer. N Engl J Med 388:585–594
Landman J (1987) Regret: a theoretical and conceptual analysis. J Theory Soc Behav 17:135–160
Lievens Y, Borras JM, Grau C (2020) Provision and use of radiotherapy in Europe. Mol Oncol 14:1461–1469
Livaudais JC, Franco R, Fei K, Bickell NA (2013) Breast cancer treatment decision-making: are we asking too much of patients? J Gen Intern Med 28:630–636
López ME, Kaplan CP, Nápoles AM, Hwang ES, Livaudais JC, Karliner LS (2014) Satisfaction with treatment decision-making and treatment regret among Latinas and non-Latina whites with DCIS. Patient Educ Couns 94:83–89
Lorenz I, Bodschwinna D, Hallensleben N, Döhner H, Niederwieser D et al (2019) INPART—a psycho-oncological intervention for partners of patients with haemato-oncological disease—study protocol. BMC Cancer 19:885
Mancini J, Genre D, Dalenc F, Ferrero JM, Kerbrat P et al (2012) Patients’ regrets after participating in a randomized controlled trials depended on their involvement in the decision making. J Clin Epidemiol 65:635–642
Martinez KA, Li Y, Resnicow K, Graff JJ, Hamilton AS, Hawley ST (2015) Decision regret following treatment for localized breast cancer: is regret stable over time? Med Decis Mak 35:446–457
Mehnert A, Müller D, Lehmann C, Koch U (2006) Die deutsche Version des NCCN Distress-Thermometers: Empirische Prüfung eines Screening-Instruments zur Erfassung psychosozialer Belastung bei Krebspatienten. Zeitschrift Für Psychiatr Psychol Und Psychother 54:213–223
Morris BB, Farnan L, Song L, Addington EL, Chen RC et al (2015) Treatment decisional regret among men with prostate cancer: racial differences and influential factors in the North Carolina Health Access and Prostate Cancer Treatment Project (HCaP-NC). Cancer 121:2029–2035
Nallani R, Smith JB, Penn JP, Bur AM, Kakarala K et al (2022) Decision regret 3 and 6 months after treatment for head and neck cancer: observational study of associations with clinicodemographics, anxiety, and quality of life. Head Neck 44:59–70
Nichols AC, Theurer J, Prisman E, Read N, Berthelet E et al (2022) Randomized trial of radiotherapy versus transoral robotic surgery for oropharyngeal squamous cell carcinoma: long-term results of the ORATOR trial. J Clin Oncol 40:866–875
Pakkanen P, Irjala H, Ilmarinen T, Halme E, Lindholm P et al (2022) Survival and larynx preservation in early glottic cancer: a randomized trial comparing laser surgery and radiation therapy. Int J Radiat Oncol Biol Phys 113:96–100
Palma DA, Prisman E, Berthelet E, Tran E, Hamilton S et al (2022) Assessment of toxic effects and survival in treatment deescalation with radiotherapy vs transoral surgery for HPV-associated oropharyngeal squamous cell carcinoma: the ORATOR2 phase 2 randomized clinical trial. JAMA Oncol 8:1–7
Sautier L, Mehnert A, Höcker A, Schilling G (2014) Participation in patient support groups among cancer survivors: do psychosocial and medical factors have an impact? Eur J Cancer Care (engl) 23:140–148
Shaw J, Zou X, Butow P (2015) Treatment decision making experiences of migrant cancer patients and their families in Australia. Patient Educ Couns 98:742–747
Sheehan J, Sherman KA, Lam T, Boyages J (2007) Association of information satisfaction, psychological distress and monitoring coping style with post-decision regret following breast reconstruction. Psychooncology 16:342–351
Spitzer RL, Kroenke K, Williams JB, Löwe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166:1092–1097
Sullivan DR, Wisnivesky JP, Nugent SM, Stone K, Farris MK et al (2023) Decision regret among patients with early-stage lung cancer undergoing radiation therapy or surgical resection. Clin Oncol (r Coll Radiol) 35:e352–e361
Szproch AK, Maguire R (2022) A systematic review of the factors associated with regret post-cancer treatment. J Psychosoc Oncol 40:1–25
Tanno K, Bito S, Isobe Y, Takagi Y (2016) Validation of a Japanese version of the decision regret scale. J Nurs Meas 24:E44-54
Ullrich A, Mehnert-Theuerkauf A (2010) Psychometrische Evaluation und Validierung einer 8-Item Kurzversion der Skalen zur Sozialen Unterstützung bei Krankheit (SSUK) bei Krebspatienten. Klinische Diagnostik Und Evaluation 3:359–381
Wagland R, Nayoan J, Matheson L, Rivas C, Brett J et al (2019) “Very difficult for an ordinary guy”: factors influencing the quality of treatment decision-making amongst men diagnosed with localised and locally advanced prostate cancer: findings from a UK-wide mixed methods study. Patient Educ Couns 102:797–803
Wallis CJD, Zhao Z, Huang L-C, Penson DF, Koyama T et al (2022) Association of treatment modality, functional outcomes, and baseline characteristics with treatment-related regret among men with localized prostate cancer. JAMA Oncol 8:50–59
Wilding S, Downing A, Selby P, Cross W, Wright P et al (2020) Decision regret in men living with and beyond nonmetastatic prostate cancer in the United Kingdom: a population-based patient-reported outcome study. Psychooncology 29:886–893
Windon MJ, D’Souza G, Faraji F, Troy T, Koch WM et al (2019) Priorities, concerns, and regret among patients with head and neck cancer. Cancer 125:1281–1289
Windon MJ, Le D, D’Souza G, Bigelow E, Pitman K et al (2021) Treatment decision-making among patients with oropharyngeal squamous cell cancer: a qualitative study. Oral Oncol 112:105044
Wollersheim BM, van Stam MA, Bosch R, Pos FJ, Tillier CN et al (2020) Unmet expectations in prostate cancer patients and their association with decision regret. J Cancer Surv 14:731–738
Yamauchi K, Nakao M, Nakashima M (2019) Correlates of regret with treatment decision-making among Japanese women with breast cancer: results of an internet-based cross-sectional survey. BMC Womens Health 19:86
Zoumpou T, Fleishman A, Jones DB, Wee CC (2023) Decision regret up to 6 years after sleeve gastrectomy. Surg Endosc 37:9381–9392
Fabian A, Rühle A, Domschikowski J, Trommer M, Wegen S et al (2023) Satisfaction with radiotherapy care among cancer patients treated in Germany-secondary analysis of a large multicenter study. Strahlenther Onkol
Niedorys B, Chrzan-Rodak A, Ślusarska B (2020) Health literacy—a review of research using the European Health Literacy Questionnaire (HLS-EU-Q16) in 2010–2018. Pielegniarstwo XXI wieku/nursing in the 21st century 19:29–41
Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL et al (2017) Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 4:Cd001431
Acknowledgements
The authors wish to thank the patients who kindly participated in this study. We thank Dr. Kathrin Forstner from the Department of Medical Psychology and Medical Sociology, University of Leipzig, for helping with the translation of the original DRS into the German version of the DRS. Alexander Rühle was supported by a Clinician Scientist Program of the Medical Faculty of the University of Leipzig.
Funding
Open Access funding enabled and organized by Projekt DEAL. Alexander Rühle was supported by a Clinician Scientist Program of the Medical Faculty of the University of Leipzig. Open Access Publication was supported by the Open Access Publishing Fund of Leipzig University.
Author information
Authors and Affiliations
Contributions
Conceptualization, AM-T, NHN, CS; methodology, AR, AH, AM-T, NHN, CS; software, AR, LW, AH; validation, AR, AH, formal analysis, AR, LW, AH; investigation, LW; resources, AM-T, NHN; data curation, AR, LW, AH; writing—original draft preparation, AR; writing—review and editing, LW, AH, AM-T, NHN, CS; visualization, AR, LW; supervision, AR, NHN, CS; project administration, AR, NHN, CS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no competing interests in relation to this study.
Ethical approval
The study was approved by the local institutional review board in advance (077/23-ek).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rühle, A., Wieland, L., Hinz, A. et al. Decision regret of cancer patients after radiotherapy: results from a cross-sectional observational study at a large tertiary cancer center in Germany. J Cancer Res Clin Oncol 150, 167 (2024). https://doi.org/10.1007/s00432-024-05638-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-05638-0