Abstract
Purpose
The application of platinum-based chemotherapeutic agents is the traditional treatment paradigm for advanced and metastatic urothelial carcinoma, which has changed with the advent of immune checkpoint inhibitors (ICIs). This study aims to evaluate the efficacy of ICI therapy versus chemotherapy in the treatment of advanced and metastatic urothelial carcinoma.
Methods
A systematic literature search of Web of Science, Embase, PubMed, and Cochrane Central Register of Controlled Trials was performed by two independent investigators. The primary endpoint was overall survival (OS), progression-free survival (PFS), objective response rate (ORR), and adverse events (AEs).
Results
The patients treated with ICI monotherapy had no significant difference in OS than those treated with chemotherapy monotherapy (HR: 0.965, 95% CI 0.865–1.076, p = 0.518). However, the patients treated with ICI monotherapy had a higher ORR and lower incidence of high-grade (≥ grade 3) AEs than those treated with chemotherapy monotherapy (OR: 0.568, 95% CI 0.479–0.675, p < 0.001; OR: 0.614, 95% CI 0.446–0.845, p = 0.003). The patients treated with ICI in combination with chemotherapy had significantly better OS and PFS than those treated with chemotherapy alone (HR: 0.862, 95% CI 0.776–0.957, p = 0.006; HR: 0.788, 95% CI 0.707–0.879, p < 0.001). However, there was no significant difference in ORR or the incidence of grade 3 or higher AEs (OR: 0.951, 95% CI 0.582–1.554, p = 0.841; OR: 0.942, 95% CI 0.836–1.062, p = 0.328).
Conclusion
ICI monotherapy did not show statistically significant difference in OS but demonstrated higher ORR and lower incidence of high-grade (≥ grade 3) AEs. And a statistically significant OS and PFS benefit was found in patients treated with first-line ICI in combination with chemotherapy compared to chemotherapy alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urothelial carcinoma (UC) is one of the more common types of urological tumors, primarily arising from the bladder, as well as the urethra, ureter, and renal pelvis. The number of new diagnoses and deaths from bladder cancer alone reaches approximately 573,000 and 213,000 cases worldwide each year (Sung et al. 2021). The prognosis of advanced UC is extremely poor, with a 5-year survival rate of less than 5% for stage IV patients with metastases (Witjes et al. 2021). In recent years, with intensive research on immune checkpoint inhibitors (ICIs), such as antibodies to programmed cell death protein-1 inhibitor (PD-1) and its ligand programmed death ligand 1 (PD-L1), significant progress has been made in the treatment of tumors, including metastatic urothelial carcinoma (mUC) (Mollica et al. 2020). In addition, treatment guidelines published by organizations such as the European Association of Urology (EAU), the European Society for Medical Oncology (ESMO), and the National Comprehensive Cancer Network (NCCN) have recognized the important role of ICI in the second-line treatment of advanced urothelial cancer, maintenance therapy after first-line platinum-based chemotherapy, and in patients who are not suitable for platinum-based chemotherapy (Witjes et al. 2021; Powles et al. 2022; Flaig et al. 2022). However, due to the limited sample size of the included studies, there is no clear conclusion on whether replacing platinum-based chemotherapeutic agents with ICI is effective in improving patient prognosis. Therefore, we performed a meta-analysis of all relevant clinical trials comparing the efficacy and safety of these two treatment regimens, using ICI alone or ICI in combination with chemotherapy as the experimental group and standard platinum-based chemotherapy regimens as the control group.
Materials and methods
Search strategies
To obtain eligible studies, multiple databases were searched for articles published until May 1, 2023. The databases searched included Web of Science, Embase, PubMed, and Cochrane Central Register of Controlled Trials. The following keywords were used for all the studies related to ICIs: immune checkpoint inhibitors, ICI, Atezolizumab, Avelumab, Durvalumab, Pembrolizumab, Nivolumab, Tislelizumab, Toripalimab, Urothelial carcinoma, bladder cancer, bladder tumor, bladder neoplasm.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) the subjects included in the study should be patients with advanced or mUC, prospective phase III or IV clinical trials involving UC patients; (2) the intervention for the experimental group should be an first-line ICI alone or first-line ICI in combination with chemotherapy and for the control group, a platinum-based chemotherapeutic agent; (3) the format of the study should be a randomized controlled trial with at least one of the following indicators: overall survival (OS), progression-free survival (PFS), adverse events (AEs), or objective response rate (ORR).
The exclusion criteria were as follows: (1) duplicate publications; (2) reviews, conference papers, or preprints; and (3) studies that only dealt with the pharmacological effects of ICI without clinical trial data.
Data extraction and grouping
Shihao Li and Hong Xiong extracted the data from the identified publications independently. The following information was extracted from each publication: name of the first author, publication year, type of ICIs, number of cases in the experimental group, number of cases in the control group, survival outcome, and follow-up time. To further compare the differences between the treatment regimens, we grouped the patients according to the following rules: the observation index of Group A was the efficacy of ICI monotherapy versus chemotherapy monotherapy, and the efficacy of ICI in combination with chemotherapy versus chemotherapy alone was observed in Group B.
Quality assessment
The Quality Assessment of Diagnostic Accuracy Studies Newcastle‒Ottawa Score (NOS) quality assessment system (Stang 2010) was used to determine the quality of the enrolled studies. Enrolled studies were scored based on case definition, representation of cases, selection restrictions, definition of controls, comparability of cases and controls, determination of exposure, identical determination methods for cases and controls, and nonresponse rates. Studies with a score ≥ 6 were considered high quality.
Statistical analysis
The results were visualized using STATA 17SE software and Review Manager 5.3 software. The heterogeneity test was performed by I-squared (I2) statistics. The data were analyzed using a fixed-effects model by default and a random-effects model if I2 > 50%. We judged that there was significant heterogeneity among the included studies when the p was < 0.05; otherwise, there was no significant heterogeneity. The potential publication bias was estimated using Begg’s funnel plot. We judged that there was no publication bias if p > 0.05 for Begg’s test.
Results
Results of the literature search
The initial search of the above databases retrieved a total of 3,98,799 articles, and after a hierarchical screening process, a total of 3 studies were finally included (Galsky et al. 2020; Powles et al. 2020, 2021). A flow chart of screening eligible articles for the meta-analysis is shown in Fig. 1.
Characteristics of the enrolled studies
The three included studies were published between 2019 and 2023 and involved three different ICIs, including atezolizumab, durvalumab, and pembrolizumab. The characteristics of the included studies are listed in Table 1. The NOS quality evaluation scale assessed the quality of the included studies. The methodological quality of the included literature was high (Fig. 2).
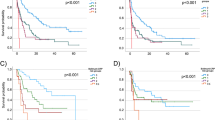
Overall survival
In Group A, the OS data were from 3 randomized controlled trials (RCTs) with a total of 2068 randomized patients, without any selection for PD-L1 status (unselected) (Galsky et al. 2020; Powles et al. 2020, 2021). The results of the meta-analysis showed that ICI monotherapy had no better OS than platinum-based chemotherapy (HR: 0.965, 95% CI 0.865–1.076, p = 0.518; Fig. 3a).
In Group B, the OS data used to compare patients were from 3 RCTs with a total of 2240 randomized patients, without any selection for PD-L1 status (unselected) (Galsky et al. 2020; Powles et al. 2020, 2021). The results of the meta-analysis showed that ICI in combination with chemotherapy had a better OS than platinum-based chemotherapy (HR: 0.862, 95% CI 0.776–0.957, p = 0.006; Fig. 3b).
Progression-free survival
In Group B, the PFS data used for comparison were from 2 RCTs with a total of 1554 randomized patients (Galsky et al. 2020; Powles et al. 2021). The results of the meta-analysis showed that ICI in combination with chemotherapy had a better PFS than platinum-based chemotherapy (HR: 0.788, 95% CI 0.707–0.879, p < 0.001; Fig. 3c).
Objective response rate
In Group A, the data for ORR comparison were available from 3 RCTs, for a total of 2105 patients (Galsky et al. 2020; Powles et al. 2020, 2021). The results of the meta-analysis showed that ICI monotherapy had a higher ORR than platinum-based chemotherapy (OR: 0.568, 95% CI 0.479–0.675, p < 0.001; Fig. 4a).
In Group B, the ORR data used for comparison were from 2 RCTs with a total of 1389 patients (Powles et al. 2020, 2021). The results of the meta-analysis showed that there was no significant difference between the ICI in combination with chemotherapy groups and the platinum-based chemotherapy monotherapy groups (OR: 0.951 95% CI 0.582–1.554, p = 0.841; Fig. 4b).
Adverse events
In Group A, the data for comparison of AEs were available from 3 RCTs, for a total of 2259 any-grade AEs (Galsky et al. 2020; Powles et al. 2020, 2021). The results of the meta-analysis showed that the ICI monotherapy had a lower incidence of high-grade (≥ grade 3) AEs than the platinum-based chemotherapy (OR: 0.614, 95% CI 0.446–0.845, p = 0.003; Fig. 4c).
In Group B, the AEs data used for comparison were from 3 RCTs with a total of 2797 any-grade adverse events (Galsky et al. 2020; Powles et al. 2020, 2021). The results of the meta-analysis showed that there was no significant difference between the ICI in combination with chemotherapy groups and the platinum-based chemotherapy monotherapy groups (OR: 0.942, 95% CI 0.836–1.062, p = 0.328; Fig. 4d).
Publication bias
The potential publication bias was estimated using Begg’s funnel plot. As shown in Fig. 5a, the Begg’s funnel plot showed symmetry, p = 1.000, so we judged that there was no publication bias.
Sensitivity analysis
Sensitivity analysis was used to assess the robustness of the meta-analysis. The leave-one-out test showed that no single study influenced the results, indicating that the results of the meta-analysis were stable and reliable (Fig. 5b).
Discussion
The immune checkpoint (IC) represents the inhibitory receptor whose main physiological function is to ensure peripheral immune tolerance by controlling the function of effector cells (Sivori et al. 2021). PD-1, one of the immune checkpoint receptors, is mainly expressed in T cells, monocytes, and natural killer (NK) cells, and its main ligand PD-L1 is mainly found on the surface of dendritic cells and macrophages, while this ligand can also be found on the surface of tumor cells (Hasegawa et al. 2020). The expression of this tumor-directed receptor on tumor-responsive effector cells and their ligands on tumor cells leads to a major mechanism of evasion of antitumor immunity. In contrast, ICIs work precisely by blocking the PD-1/PD-L1 pathway to enhance antitumor T-cell responsiveness and promote immune control of cancer cells. In fact, the first precedent for the use of immunotherapy for cancer treatment dates back to the late nineteenth century, when William B. Coley injected an inoperable cancer patient with streptococcal organisms in 1891, hoping that the bacterial infection would have the side effect of shrinking the malignant tumor (McCarthy 2006), and these bacterial products were collectively known as Coley’s Toxins. Calmette–Guérin (BCG) has been shown to have the ability to induce inflammation and has been used for over 30 years for the treatment and secondary prevention of non-muscle invasive bladder cancer (Redelman-Sidi et al. 2014).
Since the approval of ipilimumab (human IgG1 k anti-CTLA-4 monoclonal antibody) by the US Food and Drug Administration (FDA) in 2011, six additional ICIs have been approved for cancer treatment. These include the PD-1 inhibitors nivolumab, pembrolizumab, and cemiplimab and the PD-L1 inhibitors atezolizumab, avelumab, and durvalumab. Nivolumab is the first human IgG4 monoclonal antibody against PD-1 and was initially approved for the treatment of progressive, advanced, unresectable, metastatic melanoma, with results showing significant improvement in patient OS (Hodi et al. 2010). As clinical studies progressed, nivolumab was shown to be useful in the treatment of small cell lung cancer, non-small cell lung cancer, and other malignancies, all resulting in patients with clinical benefit (Wu et al. 2019; Ready et al. 2019) and prolonged disease-free survival in patients with mUC (Bajorin et al. 2021). Pembrolizumab is another PD-1 inhibitor that was approved for clinical trials in 2014. In a recent clinical trial (KEYNOTE-361), pembrolizumab did not appear to show satisfactory efficacy in the treatment of advanced UC, and overall patient survival was not significantly improved (Powles et al. 2021).
Avelumab is a PD-L1 blocking antibody approved for use in clinical trials in 2015. Avelumab demonstrated antitumor activity in the treatment of patients with platinum-resistant mUC, and a manageable safety profile was reported in all patients treated with avelumab. These data provided the rationale for the therapeutic use of avelumab in mUC, and on this basis, accelerated approval was granted by the FDA (Patel et al. 2018). In February 2016, the FDA granted the designation of the anti-PD-L1 monoclonal antibody durvalumab as a second-line or subsequent monotherapy for patients with locally advanced or metastatic urothelial malignancies, with accelerated approval. Based on data from late-stage phase I/II clinical trials, durvalumab demonstrated promising clinical activity and an encouraging and manageable safety profile in patients with locally advanced, metastatic UC (Powles et al. 2017). In May of 2016, atezolizumab was also approved for the treatment of locally advanced or metastatic urothelial malignancies and was the first PD-1/PD-L1 inhibitor approved in cisplatin chemotherapy for advanced or metastatic bladder cancer, which was later approved as a first-line agent (Rosenberg et al. 2016). In addition to these FDA-approved antibodies against PD-1, the National Medical Product Administration (NMPA) approved tislelizumab for marketing in 2019 for patients with relapsed or refractory classical Hodgkin’s lymphoma (r/r cHL) after at least second-line chemotherapy (Lee and Keam 2020). Tislelizumab has been shown in clinical trials to extend overall survival in patients with advanced uroepithelial cancer with a manageable safety profile (Ye et al. 2021). It was approved in 2020 for the treatment of patients with high PD-L1 expression after platinum-based chemotherapy (Administration NMPA 2021). In this study, we focused on the differences in the efficacy and prognosis of ICI versus chemotherapy in the treatment of advanced and mUC to ensure maximum patient benefit in clinical treatment. In summary, the application of ICI to the clinical treatment of malignancies of urothelial origin should be effective.
The most common AEs during ICI treatment are primarily cutaneous, intestinal, endocrine, pulmonary, and musculoskeletal damage. Approximately 23–33% of patients treated with ipilimumab monotherapy, 8–19% of patients treated with anti-PD-1 antibodies, and 44% of patients treated with the combination of ipilimumab and nivolumab experienced varying degrees of diarrhea (Spain et al. 2016). The incidence of grade 3 and 4 AEs reached 9% in patients treated with the combination (Spain et al. 2016). Compared with AEs from chemotherapy, immune-related adverse reactions (irAEs) associated with immunotherapy are usually longer in onset and longer in duration, and effective management depends on early identification and timely intervention of immunosuppressive and/or immunomodulatory strategies (Puzanov et al. 2017). In general, biomarkers from affected organs or the tumor microenvironment require tissue biopsy, which helps to predict biological behavior, especially for highly heterogeneous tumor tissues (Shioga et al. 2020). In addition, histopathology and immunohistochemistry are well-established clinical routines. It has been noted that monotherapy with ICI in patients with high PD-L1 expression may not improve prognosis (Guo et al. 2021). However, the study by Rizzo et al. noted that ICIs were associated with higher OS in PD-L1-positive patients (HR: 0.86, 95% CI 0.78–0.96); conversely, no differences were observed in PD-L1-negative patients (HR: 1.03, 95% CI 0.89–1.19) (Rizzo et al. 2022). Moreover, gut microbiota is also an important biomarker. The study by Hopkins et al. noted that the use of antibiotics in patients with UC treated with ICI resulted in decreased survival in cancer patients, whereas in patients receiving chemotherapy, no association between antibiotics and decreased survival was observed, suggesting that antibiotics may reduce the effectiveness of ICI therapy (Hopkins et al. 2020a). Proton pump inhibitors (PPIs) were negatively associated with patients with advanced UC treated with ICIs, independent of chemotherapy (Hopkins et al. 2020b). From some similar types of studies, it appears that antibiotics and PPIs may affect the efficacy of ICI by influencing the intestinal microecological balance, thus affecting the survival of patients with advanced UC (Gopalakrishnan et al. 2018; Maier et al. 2018).
Of course, there are still some limitations of our meta-analysis. The first is the study on baseline and prognosis, where it was noted that the patient population aged 80 years and older had better tolerability of ICI (Nebhan et al. 2021). Although patients in this age group represent a large proportion of those diagnosed with UC, there may be an underrepresentation in clinical trials. Then there is the question of whether the combination regimen of ICI and platinum-based chemotherapeutic agents can increase the clinical benefit for patients. Although we searched the literature in several databases, we did not find more studies of this type in existence, and we still need more data from studies of the same type for further analysis. From the data derived from the Begg’s funnel plot, there was no potential publication bias in the included literature regarding the combination regimen of ICI and platinum-based chemotherapeutic agents; thus, our study is credible.
Conclusion
ICI monotherapy did not show statistically significant difference in OS but demonstrated higher ORR and lower incidence of high-grade (≥ grade 3) AEs. And a statistically significant OS and PFS benefit was found in patients treated with first-line ICI in combination with chemotherapy compared to chemotherapy alone. In a word, ICIs are effective in providing clinical benefit to patients with advanced and metastatic UC compared to platinum-based chemotherapy monotherapy.
Ddata availability
The data analyzed in this study are available from the corresponding author on reasonable request.
References
Administration NMPA. January 18, 2021 Drug approval document pending receipt information release [EB/OL]. https://www.nmpa.gov.cn/zwfw/sdxx/sdxxyp/yppjfb/20210118091934189.html. 18 Jan 2021/1 May 2023.
Bajorin DF, Witjes JA, Gschwend JE et al (2021) Adjuvant nivolumab versus placebo in muscle-invasive urothelial carcinoma. N Engl J Med 384(22):2102–2114
Flaig TW, Spiess PE, Abern M et al (2022) NCCN Guidelines® insights: bladder cancer, version 2.2022. J Natl Compr Canc Netw 20(8):866–878
Galsky MD, Arija JÁA, Bamias A et al (2020) Atezolizumab with or without chemotherapy in metastatic urothelial cancer (IMvigor130): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 395(10236):1547–1557
Gopalakrishnan V, Spencer CN, Nezi L et al (2018) Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science 359(6371):97–103
Guo L, Wang X, Wang S et al (2021) Efficacy of immune-checkpoint inhibitors in PD-L1 selected or unselected patients vs. control group in patients with advanced or metastatic urothelial carcinoma. Oncoimmunology 10(1):1887551
Hasegawa M, Hasegawa G, Ikeda Y et al (2020) Emergence of undifferentiated urothelial carcinoma after pembrolizumab treatment for patient with invasive urothelial bladder cancer: a case report. SAGE Open Med Case Rep 8:2050313x20932694
Hodi FS, O’Day SJ, McDermott DF et al (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723
Hopkins AM, Kichenadasse G, Karapetis CS et al (2020a) Concomitant antibiotic use and survival in urothelial carcinoma treated with atezolizumab. Eur Urol 78(4):540–543
Hopkins AM, Kichenadasse G, Karapetis CS et al (2020b) Concomitant proton pump inhibitor use and survival in urothelial carcinoma treated with atezolizumab. Clin Cancer Res 26(20):5487–5493
Lee A, Keam SJ (2020) Tislelizumab: first approval. Drugs 80(6):617–624
Maier L, Pruteanu M, Kuhn M et al (2018) Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555(7698):623–628
McCarthy EF (2006) The toxins of William B. Coley and the treatment of bone and soft-tissue sarcomas. Iowa Orthop J 26:154–158
Mollica V, Rizzo A, Montironi R et al (2020) Current strategies and novel therapeutic approaches for metastatic urothelial carcinoma. Cancers (basel) 12(6):1449
Nebhan CA, Cortellini A, Ma W et al (2021) Clinical outcomes and toxic effects of single-agent immune checkpoint inhibitors among patients aged 80 years or older with cancer: a multicenter international cohort study. JAMA Oncol 7(12):1856–1861
Patel MR, Ellerton J, Infante JR et al (2018) Avelumab in metastatic urothelial carcinoma after platinum failure (JAVELIN Solid Tumor): pooled results from two expansion cohorts of an open-label, phase 1 trial. Lancet Oncol 19(1):51–64
Powles T, O’Donnell PH, Massard C et al (2017) Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol 3(9):e172411
Powles T, van der Heijden MS, Castellano D et al (2020) Durvalumab alone and durvalumab plus tremelimumab versus chemotherapy in previously untreated patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 21(12):1574–1588
Powles T, Csőszi T, Özgüroğlu M et al (2021) Pembrolizumab alone or combined with chemotherapy versus chemotherapy as first-line therapy for advanced urothelial carcinoma (KEYNOTE-361): a randomised, open-label, phase 3 trial. Lancet Oncol 22(7):931–945
Powles T, Bellmunt J, Comperat E et al (2022) Bladder cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol 33(3):244–258
Puzanov I, Diab A, Abdallah K et al (2017) Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) toxicity management working group. J Immunother Cancer 5(1):95
Ready N, Farago AF, de Braud F et al (2019) Third-line nivolumab monotherapy in recurrent SCLC: CheckMate 032. J Thorac Oncol 14(2):237–244
Redelman-Sidi G, Glickman MS, Bochner BH (2014) The mechanism of action of BCG therapy for bladder cancer–a current perspective. Nat Rev Urol 11(3):153–162
Rizzo A, Mollica V, Massari F (2022) Expression of programmed cell death ligand 1 as a predictive biomarker in metastatic urothelial carcinoma patients treated with first-line immune checkpoint inhibitors versus chemotherapy: a systematic review and meta-analysis. Eur Urol Focus 8(1):152–159
Rosenberg JE, Hoffman-Censits J, Powles T et al (2016) Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387(10031):1909–1920
Shioga T, Kondo R, Ogasawara S et al (2020) Usefulness of tumor tissue biopsy for predicting the biological behavior of hepatocellular carcinoma. Anticancer Res 40(7):4105–4113
Sivori S, Pende D, Quatrini L et al (2021) NK cells and ILCs in tumor immunotherapy. Mol Aspects Med 80:100870
Spain L, Diem S, Larkin J (2016) Management of toxicities of immune checkpoint inhibitors. Cancer Treat Rev 44:51–60
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Witjes JA, Bruins HM, Cathomas R et al (2021) European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur Urol 79(1):82–104
Wu YL, Lu S, Cheng Y et al (2019) Nivolumab versus docetaxel in a predominantly chinese patient population with previously treated advanced NSCLC: CheckMate 078 randomized phase III clinical trial. J Thorac Oncol 14(5):867–875
Ye D, Liu J, Zhou A et al (2021) Tislelizumab in Asian patients with previously treated locally advanced or metastatic urothelial carcinoma. Cancer Sci 112(1):305–313
Funding
This study was financially supported by Natural Science Foundation of Guangdong Province (2022A1515012195), Zhanjiang Science and Technology Plan Project (2020A01022, 2022A01017), Research Project of Traditional Chinese Medicine Bureau of Guangdong Province (20211221, 2022099), and Research Foundation for Advanced Talents of Affiliated Hospital of Guangdong Medical University (20401Z20190003).
Author information
Authors and Affiliations
Contributions
GZH took the whole responsibility of literature search, study design, and manuscript drafting. SHL and HX contributed to data extraction, concept formation, statistical revision, and major revision of the manuscript. YZ contributed to study design, concept formation, and major revision of the manuscript. HWL took the responsibility of collection of all information from the other authors, major revision of the manuscript, and full access to the data. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No potential conflicts of interest was disclosed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, G., Xiong, H., Li, S. et al. The efficacy of immune checkpoint inhibitors therapy versus chemotherapy in the treatment of advanced and metastatic urothelial carcinoma: a meta-analysis. J Cancer Res Clin Oncol 150, 5 (2024). https://doi.org/10.1007/s00432-023-05584-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-023-05584-3