Abstract
Background
The survival trends and prognostic factors of patients with extraosseous plasmacytoma (EOP) or extramedullary plasmacytoma (EMP) have not been reported in recent years. The objective of this study was to develop a novel nomogram and risk stratification system for predicting the overall survival (OS) of elderly patients with EOP based on the Surveillance, Epidemiology, and End Results (SEER) database.
Methods
The demographic characteristics of 900 patients aged 60 years and above, diagnosed with EOP between 2000 and 2019, were extracted from the SEER database. The patient population was randomly divided into a training cohort and an internal validation cohort in a ratio of 7:3. Univariate and multivariate Cox regression analyses were conducted to identify independent predictors of prognosis in elderly EOP patients, followed by developing a nomogram for prognostic assessment. The performance of the model was evaluated through receiver-operating characteristic (ROC) curves, C-index, calibration curves for calibration accuracy assessment, and decision curve analysis (DCA) to assess its clinical utility. All elderly EOP patients were stratified into three risk subgroups by cutoff value utilizing X-tile software based on their total OS scores for comparative analysis purposes. Kaplan–Meier (K–M) survival curve analysis was employed to validate any observed differences in OS among these three risk groups.
Results
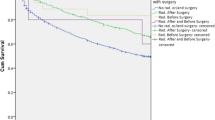
Six factors including age, year of diagnosis, marital status, primary site, surgery, and prior tumor history were identified to be independently predictive of the OS of elderly patients with EOP, and these predictors were included in the construction of the nomogram. The 1-, 3-, and 5-year area under the curves (AUCs) for OS were 0.717, 0.754, and 0.734 in the training cohort and 0.740, 0.730, and 0.765 in the validation cohort, respectively. The C-index values in the two cohorts were 0.695 and 0.690. The calibration curves and DCA exhibit commendable consistency and validity, respectively, thereby demonstrating their robust performance. The training set was stratified into low-, medium-, and high-risk subgroups based on the optimal cutoff points (167.8 and 264.8) identified. The K–M curve and cumulative risk curve exhibited statistically significant disparities in survival rates among the groups.
Conclusions
We developed a nomogram and risk classification system, which can serve as an intuitive and effective tool for clinicians to enhance the prediction of OS in elderly EOP patients, thereby facilitating the formulation of more rational and personalized treatment strategies.






Similar content being viewed by others
Data availability
The SEER database can be accessed at https://seer.cancer.gov/ without any restrictions on usage by non-academic users upon request.
References
Alfaar A et al (2022) Uveal melanoma and marital status: a relationship that affects survival. Int Ophthalmol 42(12):3857–3867
Barzenje DA et al (2018) Long-term outcome of patients with solitary plasmacytoma treated with radiotherapy: a population-based, single-center study with median follow-up of 13.7 years. Hematol Oncol 36(1):217–223
Buja A et al (2018) Marital status and stage of cancer at diagnosis: a systematic review. Eur J Cancer Care 27(1):e12755
Camp RL, Dolled-Filhart M, Rimm DL (2004) X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res off J Am Assoc Cancer Res 10(21):7252–7259
Chen Z et al (2018) Influence of marital status on small intestinal adenocarcinoma survival: an analysis of the surveillance, epidemiology, and end results (SEER) database. Cancer Manag Res 10:5667–5676
Copur MS, Manapuram S (2019) Multiple primary tumors over a lifetime. Oncology (williston Park) 33(7):629384
Dimopoulos MA, Kiamouris C, Moulopoulos LA (1999) Solitary plasmacytoma of bone and extramedullary plasmacytoma. Hematol Oncol Clin North Am 13(6):1249–1257
Dimopoulos MA et al (2000) Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood 96(6):2037–2044
Dores GM et al (2009) Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992–2004. Br J Haematol 144(1):86–94
El Ibrahimi S, Pinheiro PS (2017) The effect of marriage on stage at diagnosis and survival in women with cervical cancer. Psychooncology 26(5):704–710
Ellington TD et al (2021) Trends in solitary plasmacytoma, extramedullary plasmacytoma, and plasma cell myeloma incidence and myeloma mortality by racial-ethnic group, United States 2003–2016. Cancer Med 10(1):386–395
Finsinger P et al (2016) Clinical features and prognostic factors in solitary plasmacytoma. Br J Haematol 172(4):554–560
Gagelmann N et al (2019) Tandem autologous stem cell transplantation improves outcomes in newly diagnosed multiple myeloma with extramedullary disease and high-risk cytogenetics: a study from the chronic malignancies working party of the European society for blood and marrow transplantation. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant 25(11):2134–2142
Galieni P et al (2000) Clinical outcome of extramedullary plasmacytoma. Haematologica 85(1):47–51
Ghiassi-Nejad Z et al (2019) Overall survival trends and clinical characteristics of plasmacytoma in the united states: a national cancer database analysis. Clin Lymphoma Myeloma Leuk 19(5):310–319
Gore JL et al (2005) Marriage and mortality in bladder carcinoma. Cancer 104(6):1188–1194
Goyal G et al (2018) Treatment approaches and outcomes in plasmacytomas: analysis using a national dataset. Leukemia 32(6):1414–1420
Guo S-Q et al (2013) Prognostic factors associated with solitary plasmacytoma. Onco Targets Ther 6:1659–1666
Halamkova J et al (2021) Second primary malignancies in colorectal cancer patients. Sci Rep 11(1):2759
Han X et al (2008) Lymphoma survival patterns by WHO subtype in the United States, 1973–2003. Cancer Causes Control 19(8):841–858
Harwood AR, Knowling MA, Bergsagel DE (1981) Radiotherapy of extramedullary plasmacytoma of the head and neck. Clin Radiol 32(1):31–36
Holland J et al (1992) Plasmacytoma. Treatment results and conversion to myeloma. Cancer 69(6):1513–1517
Holler A et al (2022) Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts-a follow-up. Cancer Med 11(24):4743–4755
Jantunen E et al (2005) Autologous stem cell transplantation in patients with high-risk plasmacytoma. Eur J Haematol 74(5):402–406
Kilciksiz S et al (2008) Clinical and prognostic features of plasmacytomas: a multicenter study of Turkish oncology group-sarcoma working party. Am J Hematol 83(9):702–707
Knobel D et al (2006) Prognostic factors in solitary plasmacytoma of the bone: a multicenter rare cancer network study. BMC Cancer 6:118
Li X et al (2017) The influence of marital status on survival of gallbladder cancer patients: a population-based study. Sci Rep 7(1):5322
Li Y, Sun Z, Qu X (2022) Advances in the treatment of extramedullary disease in multiple myeloma. Transl Oncol 22:101465
Liu Y et al (2019) The impact of marriage on the overall survival of prostate cancer patients: a surveillance, epidemiology, and end results (SEER) analysis. Can Urol Assoc J = Journal De L’association Des Urologues Du Canada 13(5):E135–E139
Masshoff (1947) Isolated extramedullary plasmacytoma. Deutsche Medizinische Wochenschrift (1946) 72(33–34):489
Merrill RM, Johnson E (2017) Benefits of marriage on relative and conditional relative cancer survival differ between males and females in the USA. J Cancer Surviv Res Pract 11(5):578–589
Oka S, Ono K, Nohgawa M (2020) Successful retreatment with elotuzumab for multiple myeloma with extramedullary relapse while being treated with lenalidomide and dexamethasone. Pathol Oncol Res 26(3):1993–1995
Pencina MJ et al (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27(2):157–172
Pham A, Mahindra A (2019) Solitary plasmacytoma: a review of diagnosis and management. Curr Hematol Malig Rep 14(2):63–69
Pulte D, Gondos A, Brenner H (2008) Ongoing improvement in outcomes for patients diagnosed as having Non-Hodgkin lymphoma from the 1990s to the early 21st century. Arch Intern Med 168(5):469–476
Pulte D et al (2014) Recent improvement in survival of patients with multiple myeloma: variation by ethnicity. Leuk Lymphoma 55(5):1083–1089
Ramsingh G et al (2009) Prognostic factors influencing survival in solitary plasmacytoma. Br J Haematol 145(4):540–542
Reed V et al (2011) Solitary plasmacytomas: outcome and prognostic factors after definitive radiation therapy. Cancer 117(19):4468–4474
Sasaki R et al (2012) Multi-institutional analysis of solitary extramedullary plasmacytoma of the head and neck treated with curative radiotherapy. Int J Radiat Oncol Biol Phys 82(2):626–634
Shen X et al (2022) Survival trends and prognostic factors for patients with extramedullary plasmacytoma: a population-based study. Front Oncol 12:1052903
Soutar R et al (2004) Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol 124(6):717–726
Straetmans J, Stokroos R (2008) Extramedullary plasmacytomas in the head and neck region. Eur Arch Oto-Rhino-Laryngol off J Eur Fed Oto-Rhino-Laryngol Soc (EUFOS) Affiliated German Soc Oto-Rhino-Laryngol Head Neck Surg 265(11):1417–1423
Suh Y-G et al (2012) Radiotherapy for solitary plasmacytoma of bone and soft tissue: outcomes and prognostic factors. Ann Hematol 91(11):1785–1793
Swerdlow SH et al (2016) The 2016 revision of the world health organization classification of lymphoid neoplasms. Blood 127(20):2375–2390
Tang L, Pan Z, Zhang X (2022) The effect of marital status on the survival of patients with multiple myeloma. Hematology (amsterdam, Netherlands) 27(1):187–197
Thumallapally N et al (2017) Solitary plasmacytoma: population-based analysis of survival trends and effect of various treatment modalities in the USA. BMC Cancer 17(1):13
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Mak Int J Soc Med Decis Mak 26(6):565–574
Wang X et al (2018) Marital status and survival in patients with rectal cancer: an analysis of the surveillance, epidemiology and end results (SEER) database. Cancer Epidemiol 54:119–124
Wen G et al (2017) Management of extramedullary plasmacytoma: Role of radiotherapy and prognostic factor analysis in 55 patients. Chin J Cancer Res = Chung-Kuo Yen Cheng Yen Chiu 29(5):438–446
Yancik R, Ries LA (2000) Aging and cancer in America. Demographic and epidemiologic perspectives. Hematol Oncol Clin North Am 14(1):17–23
Zhou Y-J et al (2020) Marital status, an independent predictor for survival of gastric neuroendocrine neoplasm patients: a SEER database analysis. BMC Endocr Disord 20(1):111
Zhou D et al (2023) Marital status is an independent prognostic factor for cervical adenocarcinoma: a population-based study. Medicine 102(16):e33597
Zhu X et al (2021) Extramedullary plasmacytoma: long-term clinical outcomes in a single-center in china and literature review. Ear Nose Throat J 100(4):227–232
Acknowledgements
The authors deeply appreciate the invaluable contribution of the Surveillance, Epidemiology, and End Results database in furnishing us with a wealth of high-quality clinical data for our research.
Funding
The study was funded by a grant from the Shenzhen science and technology innovation commission, basic research (surface), JCYJ20220530144207017. The funding source did not contribute to idea generation, data gathering, interpretation, manuscript writing, or publication decision.
Author information
Authors and Affiliations
Contributions
YF and XZ: collected the data, while YiC and MT: analyzed and interpreted it. YiC: wrote the main manuscript text. YiC and YaC: designed the study. YaC and RW: critically reviewed the manuscript. All authors contributed to and approved the submitted version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The study has no conflicts of interest.
Patient consent statement
The acquisition of written patient consent was not considered essential for the purpose of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Y., Tang, M., Fu, Y. et al. A prognostic nomogram and risk classification system of elderly patients with extraosseous plasmacytoma: a SEER database analysis. J Cancer Res Clin Oncol 149, 17921–17931 (2023). https://doi.org/10.1007/s00432-023-05492-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05492-6