Abstract
Purpose
Breast cancer (BC) is currently the leading cause of death in women worldwide. Studies have confirmed that pregnancy is an independent factor affecting the survival of BC patients. BC found during pregnancy, lactation, or shortly after delivery is what we used to think of as pregnancy-associated breast cancer (PABC). The current expert definition of this concept is not uniform; however, there is growing evidence that postpartum breast cancer (PPBC) differs from other types of BC in terms of both biological features and prognosis, with a slightly different focus on diagnosis and treatment. With the increase of female reproductive age population and changes in fertility policies in China, patients with PPBC are receiving increasing attention. Here, we systematically analyzed the clinicopathological characteristics and chemotherapeutic response of patients with PPBC. We retrospectively analyzed the clinicopathological data, molecular subtypes, chemotherapy regimens, and pathological complete remission (pCR) rates of 1343 patients with non-metastatic BC at Harbin Medical University Cancer Hospital from January 1, 2012 to May 31, 2023. The categorical data were compared by chi-square test and Fisher exact test using logistic regression model. Predictor variables with P < 0.05 in the univariate analysis were included in the multivariate regression analysis to investigate the relationship between different age groups and pCR.
Results
A total of 714 patients were eligible for analysis in this study, and 667 patients had a history of pregnancy, 40 (5.6%) of whom were PPBC patients. When diagnosed with BC, patients with PPBC were younger, more likely to undergo breast-conserving surgery (BCS), and more likely to achieve pCR (P < 0.05). In molecular typing, human epidermal growth factor receptor 2 (HER-2)-positive and triple-negative breast cancer (TNBC) were more frequent. In the entire cohort, HER-2 expression and delivery status were independent predictors of pCR rates in BC patients after neoadjuvant chemotherapy (NAC).
Conclusion
Our findings suggest that postpartum status is an independent predictor of pCR attainment in BC patients. PPBC is more sensitive to chemotherapy than other patients.We need to pay more attention to this group and achieve individualized treatment, which will help us treat BC better and provide new targets and blueprints for our clinical therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the incidence of malignancies has been on the rise, and China has the highest annual incidence and mortality rate of malignancies in the world (Bray et al. 2018). After 1975, survival disparities among BC patients increased (Fan et al. 2014). By the end of 2020, the International Health Association reported that as many as 2.3 million people were diagnosed with BC, 126,000 more than in 2019. BC is increasing every year in China and has become the most common malignant disease in women (Johnson et al. 2013). In 2022, BC was listed as the fifth leading cause of cancer death in Chinese women. For BC, we advocate a three-stage approach of early detection, diagnosis, and treatment as much as possible. Currently, the treatment of BC tends to be diversified, and each treatment should be standardized and complete (Harbeck and Gnant 2017). Experts are also actively searching for treatments for BC.
Pregnancy is the growth and development of the embryo and fetus in the mother. The fertilization of a mature egg is the beginning of pregnancy, and the expulsion of the fetus and its appendages is the termination. Pregnancy is a very complex and highly coordinated physiological process (Gudnadottir et al. 2023). In recent years, the world economic landscape has gradually changed, and the pace of life has accelerated; modern people are under increasing employment and economic pressure, and raising the next generation requires more and more time and energy. As a result, childbirth is no longer the primary goal of today's young people (Jolly et al. 2000). According to the China Population Development Research Center, China’s one-child fertilitys rate declines from 0.7 to 0.5 between 2019 and 2022. In response to the aging population and declining fertility rate, China implemented a two-child policy on January 1, 2016, and a three-child policy on May 31, 2021, leading to a yearly increase in the age at which women become pregnant. According to the National Health Department and the Family Planning Commission, approximately 54 million women give birth at age 35 or older, which is extremely dangerous for women (Shan et al. 2018; Huang et al. 2023).
Older women are having children more frequently. In 2022, the average childbearing age in China was 29.1 years, well over 21.4 years in 1970, and experts believe that pregnancy is strongly associated with cancer incidence (Callihan et al. 2013). The relationship between BC and pregnancy is well known. BC is the most common pregnancy-related cancer in the world (Calsteren et al. 2010). BC is diagnosed during pregnancy in 0.2% of all BC cases, and the incidence has increased from 1 in 2000 in 1964 to 1 in 1000 (Czaplicki 2012). Pregnancy has a dual effect on BC, stopping the cancer’s progression and promoting metastasis (Proussaloglou et al. 2023).
Pregnancy is a function that is naturally endowed to humans. Most studies have shown that pregnancy has a strong protective effect on both humans and animals by slowing the development of BC, with each additional child resulting in a 5% reduction in the incidence of BC. Experts have found that menstruating women have a significantly lower risk of developing BC than women who have never given birth, because fetal cells in the mother’s tissues may help fight BC. Fetal cells may also provide the mother with immune surveillance for cancer cells, keeping the mother's immune system more alert. Meier found that the earlier a woman's pregnancy is, the more protective mechanisms are evident. The protective effect of the first pregnancy after age 30 was much later, and essentially no protective effect occurred in women who delivered at age 35 (Meier-Abt and Bentires-Alj 2014). Ploquin found that breast cancer in pregnancy (BCP) had the same survival outcome as women who did not deliver if patients were treated appropriately (Fortner et al. 2019; Ploquin et al. 2018). Sun stratified patients by age, and he found that pregnancy had little impact on the survival prognosis of BC patients, which was primarily driven by tumor biology (Sun and Lee 2020). However, some experts have different opinions. Schedin believes all patients with transitional delivery have a 10–30% increased risk of BC for at least ten years after delivery, the older the first pregnancy (Schedin 2006). Muñoz found that the protective effect of pregnancy depends on the woman's age at the time of her first pregnancy, which is of most significant benefit to young mothers. BC diagnosed 5–10 years after delivery had a higher risk of metastasis, and the crossover effect eliminated this risk over time (Muñoz-Montaño et al. 2021). When an adult woman gives birth, the significant change is postpartum breast degeneration, a process of breast degeneration in which the epithelial and lactational state of the breast degenerates and returns to its pre-pregnancy state after a period of tissue remodeling (Lyons et al. 2009). About 80–90% of normal breast epithelial tissue is removed through programmed death (Walker et al. 1989). Tumor cells can grow and progress in this wound-healing environment, a vitai risk window for BC development (Lund et al. 1996). In addition, breast degeneration is primarily characterized by increased collagen deposition, increased immune cell infiltration, increased cytokine influx, and increased bioactive fragmentation of protein hydrolysis targets. This microenvironmental change also drives its tumorigenesis (Clarkson et al. 2004; Stein et al. 2004). It is thus clear that pregnancy is a double-edged sword and cannot be considered a single risk or protective factor.
PPBC is a global health threat that affects approximately 150,000 to 350,000 young mothers each year, who face a higher risk of cancer and death and a much higher risk of dying. There is no clear definition of PPBC, and BC is generally considered to be diagnosed within five years of delivery (Callihan et al. 2013; Harvell et al. 2013). Previous studies on PPBC were mostly from Western countries, with only a few from Asia. Azim conducted a meta-analysis of 30 studies and found that BCP and PPBC patients had a worse prognosis than other BC patients (Azim et al. 2012). Rodriguez compared 797 PPBC cases with 4177 non-PPBC control cases. PPBC exhibited more advanced disease, larger tumors, and a higher percentage of hormone receptor (HR) negative tumors (Rodriguez et al. 2008). The risk of death in PPBC is also higher when controlling for age, race, and HR. Various theories have been proposed regarding why PPBC patients have a low survival rate. Tretli found a significant increase in estrogen levels during or shortly after pregnancy, and estrogen isa carcinogen in BC (Tretli et al. 1988). Asselin found that mammary stem cells during pregnancy respond strongly to steroid signals and that their temporary increase may be responsible for the more aggressive nature of PPBC (Asselin-Labat et al. 2010). And the combined effects of immunosuppression and increased angiogenesis will also play a role during pregnancy.
PPBC as a distinct BC subtype remains highly controversial, probably due to the lack of reliable biomarkers to diagnose PPBC, and further studies on the tumor biology of PPBC are needed to find better therapeutic interventions to prevent disease recurrence and progression in this population. Therefore, by analyzing the clinicopathological characteristics of PPBC patients and the pCR rate after NAC compared to other BC patients, we can find out whether pregnancy affects the response of NAC patients so that we can improve the understanding of the “postpartum effect” and choose a better treatment option.
Material and methods
Study sample
We conducted a retrospective cohort study that collected patients treated at Harbin Medical University Cancer Hospital from January 1, 2012, to May 31, 2023, who underwent physical examination, imaging (ultrasound, x-ray), and hollow needle biopsy of breast masses confirmed as BC, after communicating with the patients and their families and agreeing to NAC. Beforetreatment, the patients and their families were explained individual clinical and pathological information for clinical studies. The patient signed an informed consent regarding the medical history data and secondary use of the biospecimen. Patients underwent chemotherapy according to standard guidelines with a complete cycle of chemotherapy; surgical treatment was performed after completion of NAC, with mastectomy or breast-conserving surgery (BCS) depending on the patient's condition and wishes, and all patients underwent sentinel lymph node biopsy (SLNB) and axillary lymph node dissection (ALND) if lymph nodes had metastasized.
Inclusion and exclusion criteria
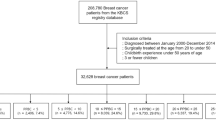
A total of 1343 patients were obtained for analysis, and detailed inclusion criteria included (1) female patients; (2) pathologically confirmed BC prior to chemotherapy; (3) all patients received NAC and completed treatment; (4) complete clinical and pathological data; (5) T1-T3 tumors as defined by the AJCC TNM staging system; and (6) patients underwent pathological IHC testing at the beginning and end of NAC. Exclusion criteria included (1) patients with incomplete data, (2) patients with multiple tumors, (3) patients with insufficient age at diagnosis and life status, (4) patients with occult BC, (5) male patients, and (6) patients with interrupted treatment or treatment at other hospitals. Finally, 714 patients who met this index were selected for analysis. This flow chart is shown in Fig. 1. The baseline characteristics of this cohort in this study are shown in Table 1.
This research complies with the World Medical Association Declaration of Helsinki 1964 and subsequently amended versions. All of the patients signed an informed consent form before the treatment.
Clinical and pathological variables
Study variables included patient age, delivery history, surgical procedure, menopausal status, body mass index (BMI) value, lymphatic infiltration status, ER status, PR status, HER-2 status, KI67 expression, P53 expression, T-stage, N-stage, clinical stage, molecular subtype, chemotherapeutic drug type, pathological type, histological grade, and pCR status. Patient information and treatment details were recorded from the time of diagnosis. Patients were divided into three groups according to delivery: as follows: Nulliparous, PPBC, and Parous > 5 years. Patients with PPBC were diagnosed with BC within 5 years of pregnancy. Age was divided into two groups using 40 years as a cut-off. Surgical procedures were divided into mastectomy and BCS. Natural menopause was defined as patients with over 12 months of future menstruation or over 60 years of age. BMI values were stratified according to international health standards: thin, BMI < 18.5; normal, 18.5 ≤ BMI < 24; overweight, 24 ≤ BMI < 30, and obese BMI ≥ 30. IHC was used to detect the HR status of patients, and positive ER and PR expression was defined as 1% nuclear staining of tumor cells. HER-2 was positive when IHC stained 3 + and negative when IHC stained 0 or 1 + HER-2. When IHC stained 2 + , its status was detected by fluorescence in situ hybridization (FISH), and HER-2 was considered negative when Fish was negative. Otherwise, it is a positive one. KI67 refers to an anti-germin monoclonal antibody, a proliferating cell nuclear antigen associated with the tumor cell cycle, interpreted as the percentage of tumor cell nuclei between 400 and 500 cells. KI67 positive nuclear ≥ 15% was defined as high expression, < 15% as low expression. Clinical and imaging staging was performed in all patients. T-stage staging was determined by palpation and ancillary examinations. N-stage was defined as abnormal axillary lymph nodes or lymph nodes detected by ultrasound. Metastatic disease was assessed by imaging. We classify cancer molecular subtypes into four types: HR(+)/HER-2(+), HR(+)/HER-2(−), HR(−)/HER-2(+), and TNBC. Pathologists observe tumor sections and analyze pathological types, like IDC, ILC, etc. According to the pathological assessment after NAC of the Chinese Society of Clinical Oncology, the Miller & Payne system is currently used to evaluate primary lesions. This system mainly compares pre- and post-treatment surgical specimens.
To assess the abundance of residual infiltrating tumor cells after NAC, specific interpretation criteria are divided into the following five levels: Grade 1 (G1): no change in infiltrating cancer cells or only a single cancer cell is changed, and there is no decrease in the number of tumor cells; Grade 2 (G2): mild decrease in infiltrating cancer cells, but the total number is still high, and the decrease does not exceed 30%; Grade 3 (G3): decrease in infiltrating cancer cells by 30–90%; Grade 4 (G4): decrease in infiltrating cancer cells by more than 90% and only small clusters or a few scattered single cancer cells remain; Grade 5 (G5): no infiltrating cancer cells at the original tumor bed site, but ductal carcinoma in situ (DCIS) may be present. G5 is used here as the study endpoint for this cohort.
Pathological detection and immunohistochemistry
IHC is a globally accepted method for detecting ER and PR in BC. Pathologists or pathology assistants cut tumor and benign breast tissue samples. They were placed in the same container during the initial evaluation, thus ensuring that typical breast structures were used as subsequent controls. All study results were reviewed and confirmed by both pathologists. Pathological sections were 4 μm thick and specimens were embedded in paraffin and incubated with primary antibody, secondary antibody, and streptavidin in sequence.
Statistical analysis
The data presented in this paper were analyzed using SPSS software version 26.0 (IBM Corporation, New York, USA) and the data presented in this paper were stratified by pregnancy status. Categorical data were expressed as counts and percentages and continued to be compared and analyzed using chi-square tests and univariate logistic regression analysis for correlation of clinical case parameters with pCR rates within each subgroup. Statistically significant variables for univariate analysis were included in multivariate analysis. To determine which variables were independent predictors of pCR, P < 0.05 was considered statistically significant. The nomogram was established based on clinicopathologic factors of BC patients. In addition, we analyzed the overall performance of the nomogram by plotting the receiver operating characteristic (ROC) curves and then calculating the AUC of the ROC curves with the aim of analyzing the overall performance of the nomogram, with the AUC exceeding 0.7 considered that the nomogram provided a reasonable estimation, and the above statistical analyses were performed by R4.1.0 software, including the car, rms, pROC, and rmda package.
Results
Characteristics of study sample
From January 1, 2012, to May 31, 2023, 1343 patients diagnosed with BC were studied at Harbin Medical University Cancer Hospital, 629 patients were excluded (472 patients without complete information, 93 patients discontinued or transferred, 13 patients diagnosed with occult BC, 1 male patient, 50 stage IV BC), and a total of 714 were included in the study. A total of 667 BC patients had a history of pregnancy, 40 patients with PPBC, 627 BC patients with Parous > 5 years, and 40 unproductive patients. The clinicopathological characteristics and treatment are shown in Table 1. The age distribution of the patients who delivered is shown in Fig. 2. The age range was 21–71, with a median age of 48. More women gave birth at the age of 24 years. Different gestational status was strongly associated with age at diagnosis, menopausal status, and surgical procedure (P < 0.05). In this cohort, PPBC patients were younger than other types of patients. 33 patients (82.5%) were diagnosed with BC before the age of 40 years, so most patients were in premenopausal status, and menstrual status was strongly correlated with age. The probability of positive HER-2 expression was higher in PPBC patients (45%) than in controls, and 11 patients (27.5%) presented with TNBC, but it was not statistically significant. Among all known molecular subtypes of BC, TNBC had the worst prognosis. Most clinicopathological features did not differ significantly between groups regarding parity (P > 0.05). In the entire cohort, younger patients were more likely to undergo BCS, but the overall breast-conservation rate was not high, at 4.8%. This may be related to the prevailing treatment setting and patient mindset. 90.2% of patients received anthracycline chemotherapy, the majority were IDC (69.3%), and the most common molecular subtype was HR(+)/HER-2(–) (44.3%).
Relationship between clinical factors and pCR in the maternal group
Among patients who delivered, 111 (16.6%) achieved pCR and 556 (83.4%) did not. The univariate analysis determined the factors affecting the pCR rate after NAC. Age, T stage, N stage, ER expression, PR expression, HER-2 expression, KI67 expression, histological grade, molecular subtype, clinical stage, type of pathology, and time of delivery were all strongly associated with pCR rate (P < 0.05) (Table 2). However, there was no significant correlation between chemotherapy regimen, surgical mode, menopausal status, BMI, P53 expression, lymphatic infiltration, and pCR (P > 0.05). Patients with younger age, lower T- and N-stage, ER-negative, PR-negative, HER2-positive, high KI67 expression, and lower BC histological grade were more likely to achieve pCR.
Factors that were statistically significant in the univariate analysis were entered into the multifactorial analysis (both of which were excluded due to differences in histological grading and type of pathology that could affect the results). Logistic regression analysis showed that patients with PPBC were more likely to achieve PCR compared with those who had been in labor for more than 5 years (OR = 2.526, CI 95% 1.026–6.219, P = 0.040). HER-2 positive patients were more likely to achieve pCR than negative ones (OR = 1.804, CI 95% 1.130–2.879, P = 0.013). These two factors were statistically significant. Delivery status and HER-2 expression were strongly associated with the performance of PCR in BC patients (P < 0.05) and were independent predictors of achieving postoperative PCR (Table 3).
Predictive analysis of patients obtaining pCR or NpCR
We used the ROC to predict the probability of obtaining pCR in BC patients (Figs. 3, 4). The results revealed that the probability of obtaining pCR was 56.0% for KI67 > 15 patients and 60.5% for HER- 2-positive patients (Table 4), with statistically significant differences (P < 0.05). In addition, this study also found that when clinical T or N staging was high, and ER or PR expression was positive, patients were less likely to achieve pCR, with probabilities of 56.4%, 57.9%, 64.5%, and 63.6%, respectively, with statistically significant differences (P < 0.05) (Table 5). BC patients were less likely to achieve pCR when women had been in labor for more than 5 years, but the difference was not statistically significant (P > 0.05).
Construction of nomogram-based prediction of pCR in patients with BC after receiving NAC
A nomogram based on clinicopathologic characteristics of BC patients was designed to predict the probability of reaching pCR when BC patients are NAC. Clinical T and N staging had the greatest impact on pCR, and pregnancy status also had a large impact, with PPBC patients more likely to reach pCR (Fig. 5). To assess the predictive ability of the a nomogram graph-based prediction model to achieve pCR in BC patients, we used the ROC curve. the AUC was 0.753 (95% CI: 0.604–0.808), indicating that the prediction model had good judgment (Fig. 6).
Correlation between clinical factors and pCR in the PPBC and Parous > 5 group
The present study analyzed the pCR rates for clinicopathological features in the different delivery groups (Table 6). In most cases, patients with PPBC were more likely to achieve pCR than those who had been in labor for more than 5 years, and this relationship was significant. We further analyzed the interaction between time to delivery and clinicopathological features of BC by general linear model (Table 7). patients with PPBC were associated with age, lymphatic infiltration, ER expression, PR expression, HER-2 expression, KI67 expression, p53 expression, and clinical stage, and RR values were calculated between subgroups (P < 0.001) (Fig. 7). patients with PPBC were more likely to reach pCR, a phenomenon that was only insignificant when BC patients were older.
Image description of RR values in PPBC patients (in the order of Table 8)
Describe the patient's pCR according to the RECIST standard
Clinical efficacy was evaluated according to the efficacy evaluation criteria of the solid tumor criteria (RECIST) version 1.1 (Table 8). Partial remission (PR) and complete remission (CR) were defined as good clinical response; progressive disease (PD) and stable lesions (SD) were defined as poor clinical response (Fig. 8). PR rates were highest in both groups, 50.0% and 66.9%, respectively. The overall outcome of chemotherapy was good, with only 11 patients progressing without improvement after treatment with NAC. Patients with PPBC were twice as likely to achieve CR (35.5% vs. 15.5%), and the difference was statistically significant (P < 0.05).
Effect of a history of abortion and lactation on pCR in BC patients
In the present study, we continued to analyze the effect of other reproductive histories on the pCR of BC patients (Table 9). A total of 437 patients experienced spontaneous or induced abortions. We found that abortion did not affect the response to chemotherapy in BC patients (P > 0.05). Only 55 of this group did not breastfeed their infants, and patients were categorized according to the duration of breastfeeding. When BC patients were breastfed for 13–24 months, patients were more likely to achieve pCR, and this correlation was significant (P < 0.05). In addition, the sensitivity to chemotherapy was similar in singleton and multiplex patients (P > 0.05).
Discussion
A total of 714 female patients with BC were selected for this study, of whom approximately 5.6% were patients with PPBC, similar to the epidemiological findings in China. This retrospective study analyzed the response of BC patients to NAC. We found that delivery status was an independent predictor of pCR rates after NAC in BC patients, that PPBC patients were younger at the time of BC diagnosis, that most patients were in an unmenopausal state, had a more significant proportion of the TNBC phenotype, and were more sensitive to chemotherapy than other groups (37.5% vs. 15.3%, P < 0.001), these data confirm the importance of the time of the start of the last delivery as a biomarker of NAC outcome in BC patients. When dealing with patients with PPBC, we should strongly recommend chemotherapy to patients and also need to study PPBC as a high-risk subset. By evaluating these factors, physicians can change the treatment decisions of BC patients and achieve appropriate individualized treatment.
Globally, cancer is a growing pregnancy complication, mainly due to the increasing age of women at childbirth (Eastwood-Wilshere et al. 2019). Cancer in women of maternal age remains a major global problem, which is more pronounced in lower socioeconomic countries. Westerners and Asians are different in lifestyle, genetic makeup, and tumor biology, which means that the findings of Western experts may not be apply to Asian populations (Bhoo-Pathy et al. 2013). Thyroid cancer, melanoma, lymphoma, cervical cancer, and BC are the most common PABCs, with only BC and melanoma increasing in recent years, especially PPBC (Johansson et al. 2011).
PPBC remains an under-recognized high-risk BC group, and the age of BC diagnosis is now gradually becoming younger, with a large proportion of patients diagnosed with BC under 45 years of age being PPBC, probably because younger BC patients are more likely to accept becoming mothers after cancer treatment (Colleoni et al. 2002). Goddard found that women had a high risk of having a BC diagnosis within 10 years of delivery and that this effect persisted until 30 years later (Goddard et al. 2019). One study found that PPBC patients had a higher axillary lymph node metastasis rate, and most patients presented with ER-negative, PR-negative, HER-2-positive, or TNBC tumors (Bonnier et al. 1997). This may also be because HR positive patients need endocrine therapy and have a reduced chance of getting pregnant after taking tamoxifen (Petrek et al. 2006). Guinee found that the shorter the interval between pregnancy and diagnosis of BC, the three times more likely to have metastasis and death than other types (Guinee et al. 1994). Some experts believe that the poor prognosis of PPBC patients is due to the young age of the patient and is not related to the presence or absence of pregnancy. Elena believes that this one-size-fits-all approach is incorrect, as pregnancy induces molecular and anatomical changes in the breast that can create a tumor-promoting environment. Experts recommend that the pregnancy history of BC patients must be asked for and fully documented at the time of consultation, and that we need to consider pregnancy as an independent prognostic factor affecting BC. We need to consider pregnancy as an independent poor prognostic factor affecting the survival of patients with BC (Johansson et al. 2011). Some studies have found that pregnancy after diagnosis and treatment of BC is not associated with survival. Therefore it is necessary to investigate PPBC as a risk subset for BC regardless of ER and PR status (Shagisultanova et al. 2022; Matthews and Hamilton 2009; Macias and Hinck 2012).
PPBC is an aggressive subtype characterized by a unique genetic profile, and PPBC affects women far beyond their last pregnancy. There are many potential mechanisms for the poor survival of PPBC patients, most notably the degenerative process of the mammary gland after delivery. Martinson found that changes in the mammary gland after weaning in mice increased tumor growth, invasion, and metastasis persisted for a long time. These changes persisted for a long time (Martinson et al. 2015). The first stage is reversible and occurs 1 to 2 days after weaning, when the lobes of the mammary glands are highly hyperplastic and hypertrophic, the follicular epithelium is arranged in single rows and filled with milk, the fibrous tissue around the milk ducts almost disappears and is replaced by capillaries, the follicles and milk ducts are generally dilated, the epithelial cells of the mammary glands undergo programmed death and regeneration, and redistribution of glands and fat can be observed (Clarkson et al. 2004). The second stage is irreversible and occurs within two weeks after weaning when the extracellular matrix remodeling system allows other cells to continue to die. The mammary gland structure undergoes rapid degenerative changes that are so rapid and extensive that the mammary gland recovers to a volume smaller than its pre-pregnancy level, differentiating the tissue into fat cells (O’Brien et al. 2010; Jindal et al. 2014). The activation of proteases marks this phase, and apoptosis continues throughout the degenerative process (Green and Lund 2005). During weaning-induced cell collapse, occult tumor cells are activated to the mammary stroma and then enter the blood system to spread and establish micrometastases in distant organs (Maller et al. 2013). Macrophages also appear to play a role in breast degeneration, and Condeelis found that macrophages promote tumor cell motility after receiving the recruitment of fibrillar collagen (Condeelis and Pollard 2006). Lyons found abundant fibrillar collagen, high cyclooxygenase-2 expression, and an aggressive phenotype in degenerating mammary glands. NSAIDs can reduce fibrillar collagen production, tumor growth and metastasis of tumor cells to distant sites, by inhibiting high cyclooxygenase-2 (Lyons et al. 2011). In addition to this, the activity of matrix metalloprotease-2 (MMP2) increased during mammary degeneration and human mammary epithelial cells, although constitutively inactive on intact laminin-5, acquired a motile phenotype on MMP2 cleaved laminin-5, contributing to the progression of PPBC (Giannelli et al. 1999). Tamburini found that PD-L1 and PD-1 are highly expressed in degenerated mammary glands, and PD-L1 and its receptor PD-1 can inhibit T-cell responses through the activation of pro-apoptotic signals. The promotion of tumor growth triggered by mammary gland degeneration is reversed after applying anti-PD-L1 therapy (Tamburini et al. 2019; Borges et al. 2020). SEMA7A is a glycosphatidylinositol membrane-anchored protein that promotes the attachment and spreading of multiple cell types. Black found that SEMA7A plays an essential role in degenerating mammary glands and that SEMA7A promotes PPBC progression by regulating tumor-associated COX-2 expression and fibroblast-mediated collagen deposition in the tumor microenvironment (Black et al. 2016). If SEMA7A is knocked down, COX-2 and collagen deposition are also reduced, suggesting that SEMA7A and COX-2 could be new targets for PPBC treatment. Thus, breast degeneration is the most crucial predictor of PPBC. Some experts found that PPBC also has a distinct pattern of visceral metastasis, where circulating tumor cells released after breast degeneration have an additional metastatic advantage that is not reflected in the brain, lung, or bone but is particularly evident in the liver, where metastasis is absent, probably due to a functional link between the breast and the liver (Black et al. 2016; Tarullo Sarah et al. 2020). Goddard found that rodents doubled their liver volume and increased anabolism during post-gestational lactation (Goddard et al. 2017).
It has also been shown that most PPBC is in an intermediate to advanced stage due to a delay in diagnosis (Ishida et al. 1992). Moreira believes that these patients are too young and that the difficulty in diagnosis is due to the different breast tissue itself (Moreira et al. 2010). Pregnancy and breastfeeding can lead to increased in breast volume with palpable masses, and the increased firmness and density can pose a significant challenge on physical examination and imaging (Taylor et al. 2011; Ruiz et al. 2017). During pregnancy, the patient carries a fetus with its own physical needs and risk factors, and the pregnant woman herself can feel anxious and desperate (Ferrari et al. 2018). After the pregnancy, the patient faces the stress of changing identity and must balance caring for the newborn with managing her health and receiving cancer care (Proussaloglou et al. 2023; Loibl et al. 2015). This trade-off can cause women to neglect their health. Lack of common sense by women and physicians is also thought to play an important role in delaying diagnosis. Conditions such as lactational adenomas, malformations, fibroadenomas, and cellulitis often occur during pregnancy and lactation, and these lesions can also influence the imaging physician's judgment (Baker et al. 2001; Presazzi et al. 2015; Lee and Bae 2020). Therefore, when dealing with PPBC patients, patients and doctors should take it seriously.
However, some experts have suggested otherwise, and Amant found that patients diagnosed with BC during pregnancy do not have an increased risk of metastasis and death. Patients with PABC have similar OS to non-pregnant patients (Amant et al. 2013). Litton also found higher OS rates when PPBC patients received appropriate local and systemic therapy (77% vs. 71%), and the authors primarily emphasized the importance of chemotherapy (Litton et al. 2013). In addition, proper exercise strengthens muscles, reduces inflammation and, lowers the risk of disease. The World Health Organization recommends 150 min of moderate-intensity physical activity per week for pregnant and postpartum women to help further heal and improve women's mental health (Bull et al. 2020; Neil-Sztramko et al. 2014). Recent studies have also identified potential targets for treating PPBC, including pathways related to lymphangiogenesis and immunomodulation, offering hope for treating these patients (Lefrère et al. 2021).
In this study, we continued to analyze the effect of breastfeeding and miscarriage on pCR in BC patients. Miscarriage does not affect the sensitivity of chemotherapy in BC patients. In 1980, experts concluded that there was a close association between miscarriage and BC, with undifferentiated mammary cells and fully differentiated cells in menstruating women, and that women who experienced miscarriage were likely to be partially differentiated and more susceptible to carcinogens (Braüner et al. 2013). The American College of Obstetricians and Gynecologists study found that abortion does not increase the risk of having BC. We have found a significant increase in the effectiveness of chemotherapy when BC patients are adequately breastfed. Very few women with BC have breastfed, in large part due to the mother's fear of transmitting cancer cells to her baby through her breast milk; there is no evidence of such transmission, but the average duration of breastfeeding is much shorter than for women without BC due to the psychological stress of having cancer (Breast cancer and breastfeeding 2002). One study found that breastfeeding has a significant protective effect on TNBC with BRCA1 mutation and that breastfeeding significantly reduces the risk of recurrence in BC patients, especially in postmenopausal women (Palmer et al. 2014). Therefore, experts suggest that the duration of breastfeeding should be extended appropriately. In addition, some studies have found that the duration of breastfeeding is shorter in countries with high average socioeconomic status, which is likely to be the reason for the increased incidence of BC in postmenopausal women in developed countries (Victora Cesar et al. 2016). Bernstein found that the endocrinology of a woman's second pregnancy differs from that of her first and that an increase in the number of pregnancies increases the risk of metastasis (Bernstein et al. 1986). In contrast, Woods suggested that an increase in the number of pregnancies reduces the menstrual cycle and maintains the organism in a low estrogenic state, acting as a breast conserving woman like pregnancy and exclusive breastfeeding (Woods et al. 1980).
Our study still has many limitations. First, this is a single-center study with inevitable selection bias, which may not fully represent the entire Chinese population, and subtle differences may not be detected due to the limited number of cases.
Secondly, there is no survival analysis in this study. The prognosis of patients is still the most critical endpoint of the study. In the subsequent study, we need continuous postoperative follow-up. Nevertheless, this study is also a rare study of the NAC response to pregnancy in BC patients in Asian countries. It allows us to better focus on this category of patients and make treatment choices, but we also need further research to confirm our findings and explore the biological background behind it.
Conclusion
In conclusion, different pregnancy statuses were independent predictors of achieving pCR after BC patients received NAC, and PPBC patients were likelier to achieve pCR than other patients. In previous studies, PPBC was often classified as PABC, hiding its biological characteristics. As a specific group, doctors need to analyze the biological factors of PPBC in more detail, and governments should develop additional policies to help patients achieve precise individualized treatment.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Availability of data and materials
The data and materials for this study are authentic and available. All the data can be found in the digital integrated management system of Harbin Medical University Cancer Hospital. Publicly archived datasets analysed or generated during the study may be provided by the corresponding author upon reasonable request.
Abbreviations
- ALND:
-
Axillary lymph node dissection
- BC:
-
Breast cancer
- BCS:
-
Breast conserving surgery
- BCP:
-
Breast cancer in pregnancy
- BMI:
-
Body mass index
- DCIS:
-
Ductal carcinoma in situ
- ER:
-
Estrogen receptor
- HER-2:
-
Human epidermal growth factor receptor-2
- HR:
-
Hormone receptor
- IDC:
-
Invasive ductal carcinoma
- IHC:
-
Immunohistochemical
- ILC:
-
Invasive lobular carcinoma
- MMP-2:
-
Matrix metalloprotease-2
- NAC:
-
Neoadjuvant chemotherapy
- PABC:
-
Pregnancy associated breast cancer
- PR:
-
Progesterone receptor
- pCR:
-
Pathologic complete response
- PPBC:
-
Postpartum breast cancer
- PSM:
-
Propensity score matching
- RECIST:
-
Response Evaluation Criteria In Solid Tumors
- ROC:
-
Receiver operating characteristic
- SLNB:
-
Sentinel lymph node biopsy
- TNBC:
-
Triple negative breast cancer
References
Amant F, von Minckwitz G, Han SN et al (2013) Prognosis of women with primary breast cancer diagnosed during pregnancy: results from an international collaborative study. J Clin Oncol 31(20):2532–2539. https://doi.org/10.1200/JCO.2012.45.6335
Asselin-Labat M-L, Vaillant F, Sheridan JM et al (2010) Control of mammary stem cell function by steroid hormone signalling. Nature 465(7299):798–802. https://doi.org/10.1038/nature09027
Azim HA, Santoro L, Russell-Edu W et al (2012) Prognosis of pregnancy-associated breast cancer: a meta-analysis of 30 studies. Cancer Treat Rev 38(7):834–842. https://doi.org/10.1016/j.ctrv.2012.06.004
Baker TP, Lenert JT, Parker J et al (2001) Lactating adenoma: a diagnosis of exclusion. Breast J 7(5):354–357. https://doi.org/10.1046/j.1524-4741.2001.20075.x
Bernstein L, Depue RH, Ross RK et al (1986) Higher maternal levels of free estradiol in first compared to second pregnancy: early gestational differences. J Natl Cancer Inst 76(6):1035–1039
Bhoo-Pathy N, Yip C-H, Hartman M et al (2013) Breast cancer research in Asia: adopt or adapt Western knowledge? Eur J Cancer 49(3):703–709. https://doi.org/10.1016/j.ejca.2012.09.014
Black SA, Nelson AC, Gurule NJ et al (2016) Semaphorin 7a exerts pleiotropic effects to promote breast tumor progression. Oncogene 35(39):5170–5178. https://doi.org/10.1038/onc.2016.49
Bonnier P, Romain S, Dilhuydy JM et al (1997) Influence of pregnancy on the outcome of breast cancer: a case-control study. Societe Francaise de Senologie et de Pathologie Mammaire Study Group. Int J Cancer 72(5):720–727. https://doi.org/10.1002/(sici)1097-0215(19970904)72:5%3c720::aid-ijc3%3e3.0.co;2-u
Borges VF, Lyons TR, Germain D et al (2020) Postpartum involution and cancer: an opportunity for targeted breast cancer prevention and treatments? Cancer Res 80(9):1790–1798. https://doi.org/10.1158/0008-5472.CAN-19-3448
Braüner CM, Overvad K, Tjønneland A et al (2013) Induced abortion and breast cancer among parous women: a Danish cohort study. Acta Obstet Gynecol Scand 92(6):700–705. https://doi.org/10.1111/aogs.12107
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Breast cancer and breastfeeding (2002) collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96,973 women without the disease. Lancet 360(9328):187–195. https://doi.org/10.1016/S0140-6736(02)09454-0
Bull FC, Al-Ansari SS, Biddle S et al (2020) World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 54(24):1451–1462. https://doi.org/10.1136/bjsports-2020-102955
Callihan EB, Gao D, Jindal S et al (2013) Postpartum diagnosis demonstrates a high risk for metastasis and merits an expanded definition of pregnancy-associated breast cancer. Breast Cancer Res Treat 138(2):549–559. https://doi.org/10.1007/s10549-013-2437-x
Clarkson RWE, Wayland MT, Lee J et al (2004) Gene expression profiling of mammary gland development reveals putative roles for death receptors and immune mediators in post-lactational regression. Breast Cancer Res 6(2):R92–R109. https://doi.org/10.1186/bcr754
Colleoni M, Rotmensz N, Robertson C et al (2002) Very young women (<35 years) with operable breast cancer: features of disease at presentation. Ann Oncol 13(2):273–279. https://doi.org/10.1093/annonc/mdf039
Condeelis J, Pollard JW (2006) Macrophages: obligate partners for tumor cell migration, invasion, and metastasis. Cell 124(2):263–266. https://doi.org/10.1016/j.cell.2006.01.007
Czaplicki KL (2012) Two lives intertwined: pregnancy-associated breast cancer. Clin J Oncol Nurs 16(5):E183–E189. https://doi.org/10.1188/12.CJON.E183-E189
Eastwood-Wilshere N, Turner J, Oliveira N et al (2019) Cancer in pregnancy. Asia-Pacific J Clin Oncol. 15(6):296–308. https://doi.org/10.1111/ajco.13235
Fan L, Strasser-Weippl K, Li JJ et al (2014) Breast cancer in China. Lancet Oncol 15(7):e279–e289. https://doi.org/10.1016/s1470-2045(13)70567-9
Ferrari F, Faccio F, Peccatori F et al (2018) Psychological issues and construction of the mother-child relationship in women with cancer during pregnancy: a perspective on current and future directions. BMC Psychol 6(1):10. https://doi.org/10.1186/s40359-018-0224-5
Fortner RT, Sisti J, Chai B et al (2019) Parity, breastfeeding, and breast cancer risk by hormone receptor status and molecular phenotype: results from the Nurses’ Health Studies. Breast Cancer Res 21(1):40. https://doi.org/10.1186/s13058-019-1119-y
Giannelli G, Pozzi A, Stetler-Stevenson WG et al (1999) Expression of matrix metalloprotease-2-cleaved laminin-5 in breast remodeling stimulated by sex steroids. Am J Pathol 154(4):1193–1201. https://doi.org/10.1016/S0002-9440(10)65371-0
Goddard ET, Hill RC, Nemkov T et al (2017) The rodent liver undergoes weaning-induced involution and supports breast cancer metastasis. Cancer Discov 7(2):177–187. https://doi.org/10.1158/2159-8290.CD-16-0822
Goddard ET, Bassale S, Schedin T et al (2019) Association between postpartum breast cancer diagnosis and metastasis and the clinical features underlying risk. JAMA Netw Open 2(1):e186997. https://doi.org/10.1001/jamanetworkopen.2018.6997
Green KA, Lund LR (2005) ECM degrading proteases and tissue remodelling in the mammary gland. BioEssays 27(9):894–903. https://doi.org/10.1002/bies.20281
Gudnadottir U, Du J, Hugerth LW et al (2023) Pre-pregnancy complications—associated factors and wellbeing in early pregnancy: a Swedish cohort study. BMC Pregnancy Childbirth 23(1):153. https://doi.org/10.1186/s12884-023-05479-8
Guinee VF, Olsson H, Möller T et al (1994) Effect of pregnancy on prognosis for young women with breast cancer. Lancet 343(8913):1587–1589. https://doi.org/10.1016/s0140-6736(94)93054-6
Harbeck N, Gnant M (2017) Breast cancer. Lancet 389(10074):1134–1150. https://doi.org/10.1016/s0140-6736(16)31891-8
Harvell DME, Kim J, O’Brien J et al (2013) Genomic signatures of pregnancy-associated breast cancer epithelia and stroma and their regulation by estrogens and progesterone. Hormones Cancer 4(3):140–153. https://doi.org/10.1007/s12672-013-0136-z
Huang C, Jiang Q, Su W et al (2023) Age-specific effects on adverse pregnancy outcomes vary by maternal characteristics: a population-based retrospective study in Xiamen, China. BMC Public Health 23(1):326. https://doi.org/10.1186/s12889-023-15235-4
Ishida T, Yokoe T, Kasumi F et al (1992) Clinicopathologic characteristics and prognosis of breast cancer patients associated with pregnancy and lactation: analysis of case-control study in Japan. Jpn J Cancer Res 83(11):1143–1149. https://doi.org/10.1111/j.1349-7006.1992.tb02737.x
Jindal S, Gao D, Bell P et al (2014) Postpartum breast involution reveals regression of secretory lobules mediated by tissue-remodeling. Breast Cancer Res 16(2):R31. https://doi.org/10.1186/bcr3633
Johansson ALV, Andersson TM-L, Hsieh C-C et al (2011) Increased mortality in women with breast cancer detected during pregnancy and different periods postpartum. Cancer Epidemiol Biomarkers Prevent 20(9):1865–1872. https://doi.org/10.1158/1055-9965.EPI-11-0515
Johnson RH, Chien FL, Bleyer A (2013) Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. J Am Med Assoc 309(8):800–805. https://doi.org/10.1001/jama.2013.776
Jolly M, Sebire N, Harris J et al (2000) The risks associated with pregnancy in women aged 35 years or older. Hum Reprod 15(11):2433–2437. https://doi.org/10.1093/humrep/15.11.2433
Lee SE, Bae YK (2020) Breast lesions during pregnancy and lactation: a pictorial essay. Ultrasonography 39(3):298–310. https://doi.org/10.14366/usg.19070
Lefrère H, Lenaerts L, Borges VF et al (2021) Postpartum breast cancer: mechanisms underlying its worse prognosis, treatment implications, and fertility preservation. Int J Gynecol Cancer 31(3):412–422. https://doi.org/10.1136/ijgc-2020-002072
Litton JK, Warneke CL, Hahn KM et al (2013) Case control study of women treated with chemotherapy for breast cancer during pregnancy as compared with nonpregnant patients with breast cancer. Oncologist 18(4):369–376. https://doi.org/10.1634/theoncologist.2012-0340
Loibl S, Schmidt A, Gentilini O et al (2015) Breast cancer diagnosed during pregnancy: adapting recent advances in breast cancer care for pregnant patients. JAMA Oncol 1(8):1145–1153. https://doi.org/10.1001/jamaoncol.2015.2413
Lund LR, Rømer J, Thomasset N et al (1996) Two distinct phases of apoptosis in mammary gland involution: proteinase-independent and -dependent pathways. Development 122(1):181–193. https://doi.org/10.1242/dev.122.1.181
Lyons TR, Schedin PJ, Borges VF (2009) Pregnancy and breast cancer: when they collide. J Mammary Gland Biol Neoplasia 14(2):87–98. https://doi.org/10.1007/s10911-009-9119-7
Lyons TR, O’Brien J, Borges VF et al (2011) Postpartum mammary gland involution drives progression of ductal carcinoma in situ through collagen and COX-2. Nat Med 17(9):1109–1115. https://doi.org/10.1038/nm.2416
Macias H, Hinck L (2012) Mammary gland development. Wiley Interdisciplinary Rev-Dev Biol 1(4):533–557. https://doi.org/10.1002/wdev.35
Maller O, Hansen KC, Lyons TR et al (2013) Collagen architecture in pregnancy-induced protection from breast cancer. J Cell Sci 126(Pt 18):4108–4110. https://doi.org/10.1242/jcs.121590
Martinson HA, Jindal S, Durand-Rougely C et al (2015) Wound healing-like immune program facilitates postpartum mammary gland involution and tumor progression. Int J Cancer 136(8):1803–1813. https://doi.org/10.1002/ijc.29181
Matthews TJ, Hamilton BE (2009) Delayed childbearing: more women are having their first child later in life. NCHS Data Brief 21:1–8
Meier-Abt F, Bentires-Alj M (2014) How pregnancy at early age protects against breast cancer. Trend Mol Med 20(3):143–153. https://doi.org/10.1016/j.molmed.2013.11.002
Moreira WB, Brandão EC, Soares AN et al (2010) Prognosis for patients diagnosed with pregnancy-associated breast cancer: a paired case-control study. Sao Paulo Med J 128(3):119–124
Muñoz-Montaño WR, Cabrera-Galeana P, De la Garza-Ramos C et al (2021) Prognosis of breast cancer diagnosed during pregnancy and early postpartum according to immunohistochemical subtype a matched case-control study. Breast Cancer Res Treat 188(2):489–500. https://doi.org/10.1007/s10549-021-06225-4
Neil-Sztramko SE, Kirkham AA, Hung SH et al (2014) Aerobic capacity and upper limb strength are reduced in women diagnosed with breast cancer: a systematic review. J Physiother 60(4):189–200. https://doi.org/10.1016/j.jphys.2014.09.005
O’Brien J, Lyons T, Monks J et al (2010) Alternatively activated macrophages and collagen remodeling characterize the postpartum involuting mammary gland across species. Am J Pathol 176(3):1241–1255. https://doi.org/10.2353/ajpath.2010.090735
Palmer JR, Emma V, Troester MA et al (2014) Parity, lactation, and breast cancer subtypes in African American women: results from the AMBER Consortium. J Natl Cancer Inst. https://doi.org/10.1093/jnci/dju237
Petrek JA, Naughton MJ, Case LD et al (2006) Incidence, time course, and determinants of menstrual bleeding after breast cancer treatment: a prospective study. J Clin Oncol 24(7):1045–1051. https://doi.org/10.1200/JCO.2005.03.3969
Ploquin A, Pistilli B, Tresch E et al (2018) 5-year overall survival after early breast cancer diagnosed during pregnancy: a retrospective case-control multicentre French study. Eur J Cancer 95:30–37. https://doi.org/10.1016/j.ejca.2018.02.030
Presazzi A, Di Giulio G, Calliada F (2015) Breast hamartoma: ultrasound, elastosonographic, and mammographic features. Mini pictorial essay. J Ultrasound 18(4):373–377. https://doi.org/10.1007/s40477-015-0175-0
Proussaloglou EM, Blanco LZ, Siziopikou KP (2023) Updates in the pathology of Pregnancy Associated Breast Cancer (PABC). Pathol Res Pract 244:154413. https://doi.org/10.1016/j.prp.2023.154413
Rodriguez AO, Chew H, Cress R et al (2008) Evidence of poorer survival in pregnancy-associated breast cancer. Obst Gynecol. 112(1):71–78. https://doi.org/10.1097/AOG.0b013e31817c4ebc
Ruiz R, Herrero C, Strasser-Weippl K et al (2017) Epidemiology and pathophysiology of pregnancy-associated breast cancer: a review. Breast 35:136–141. https://doi.org/10.1016/j.breast.2017.07.008
Schedin P (2006) Pregnancy-associated breast cancer and metastasis. Nat Rev Cancer 6(4):281–291. https://doi.org/10.1038/nrc1839
Shagisultanova E, Gao D, Callihan E et al (2022) Overall survival is the lowest among young women with postpartum breast cancer. Eur J Cancer 168:119–127. https://doi.org/10.1016/j.ejca.2022.03.014
Shan D, Qiu P-Y, Wu Y-X et al (2018) Pregnancy outcomes in women of advanced maternal age: a retrospective cohort study from China. Sci Reports 8(1):12239. https://doi.org/10.1038/s41598-018-29889-3
Stein T, Morris JS, Davies CR et al (2004) Involution of the mouse mammary gland is associated with an immune cascade and an acute-phase response, involving LBP, CD14 and STAT3. Breast Cancer Res 6(2):R75–R91. https://doi.org/10.1186/bcr753
Sun J, Lee MC (2020) Clinical presentation, diagnosis and prognosis of pregnancy-associated breast cancer. Adv Exp Med Biol 1252:87–93. https://doi.org/10.1007/978-3-030-41596-9_11
Tamburini BAJ, Elder AM, Finlon JM et al (2019) PD-1 blockade during post-partum involution reactivates the anti-tumor response and reduces lymphatic vessel density. Front Immunol 10:1313. https://doi.org/10.3389/fimmu.2019.01313
Tarullo Sarah E, Hill Ryan C, Hansen Kirk C et al (2020) Postpartum breast cancer progression is driven by semaphorin 7a-mediated invasion and survival. Oncogene 39(13):2772–2785. https://doi.org/10.1038/s41388-020-1192-9
Taylor D, Lazberger J, Ives A et al (2011) Reducing delay in the diagnosis of pregnancy-associated breast cancer: how imaging can help us. J Med Imaging Radiat Oncol 55(1):33–42. https://doi.org/10.1111/j.1754-9485.2010.02227.x
Tretli S, Kvalheim G, Thoresen S et al (1988) Survival of breast cancer patients diagnosed during pregnancy or lactation. Br J Cancer 58(3):382–384. https://doi.org/10.1038/bjc.1988.224
Van Calsteren K, Heyns L, De Smet F et al (2010) Cancer during pregnancy an: analysis of 215 patients emphasizing the obstetrical and the neonatal outcomes. J Clin Oncol 28(4):683–689. https://doi.org/10.1200/JCO.2009.23.2801
Victora Cesar G, Bahl R, Barros AJD et al (2016) Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 387(10017):475–490. https://doi.org/10.1016/S0140-6736(15)01024-7
Walker NI, Bennett RE, Kerr JF (1989) Cell death by apoptosis during involution of the lactating breast in mice and rats. Am J Anat 185(1):19–32. https://doi.org/10.1002/aja.1001850104
Woods KL, Smith SR, Morrison JM (1980) Parity and breast cancer: evidence of a dual effect. BMJ 281(6237):419–421. https://doi.org/10.1136/bmj.281.6237.419
Funding
This work was supported by grants from the Natural Science Foundation of China (Grant Number: 81872145).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. HD, SJ and MX designed research; DL, HD, YB, PY and YW performed research; MX administered the research; FL, HD, YW and XC analyzed the data; HD, SJ, DL and YB wrote the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The study was approved by Harbin Medical University and written informed consent was obtained from all study participants before treatment, and the authors confirmed that all the study was conducted in accordance with the contents of the revised 2013 revised Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Containing any form of personal data (including any personal details, images or videos) has been obtained the consent of the parents or legal guardian of the person or the child. Statements of all case reports have been approved for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dou, H., Jia, S., Ba, Y. et al. Clinical characteristics and pathologic complete response (pCR) rate after neoadjuvant chemotherapy in postpartum women with breast cancer. J Cancer Res Clin Oncol 149, 14185–14204 (2023). https://doi.org/10.1007/s00432-023-05194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-05194-z