Abstract
Purpose
Oral squamous cell carcinomas (OSCCs) adjacent to the mandible or with clinically suspected bone infiltration are surgically treated either with marginal or segmental resections. This retrospective study compared both resections regarding local recurrence and lymph node recurrence or secondary lymph node metastases.
Methods
All consecutive primary OSCC cases between January 2007 and December 2015 that underwent mandibular marginal or segmental resection were included. Rates of local and lymph node recurrences or secondary metastases and possible risk factors such as tumor localization according to Urken’s classification were recorded.
Results
In total, 180 patients with 85 marginal (group I) and 95 segmental (group II) mandibular resections were analyzed. The local recurrence rates were comparable between the groups (28.2% vs. 27.4%; p = 0.897). Lymph node recurrences or secondary metastases were higher in group I (9.4% (n = 8) vs. 6.2% (n = 6); p = 0.001). Tumor localization appears to affect the outcomes. Significantly fewer local and lymph node recurrences/metastases were found for Urken’s classification SB and S calculated by two-proportion z-test (p = 0.014 and 0.056, respectively). Local recurrences mostly emerged from soft tissues, which should be resected more radically than the bones.
Conclusion
While bone infiltration appears technically well controllable from an oncologic point of view, local recurrences and lymph node recurrences/metastases remain an issue. Regular clinical aftercare with imaging is crucial to detect recurrences.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Oral squamous cell carcinomas (OSCC) can infiltrate the mandible, and this likeliness for invasion is influenced among others by time (e.g., diagnosis delay), tumor biology, and adjacent localization measuring < 1 cm to the mandible (Pandey et al. 2007; Eichberger et al. 2022). Furthermore, tumorous bone involvement can range from limited cortical erosion to cancellous bone involvement with secondary pathologic fractures. However, the extent of resection and its influence on local recurrence and long-term survival are still being discussed, which results in heterogeneous concepts. These include mandible preservation and periosteal frozen section analysis of OSCC cases that lack cortical erosion in preoperative staging imaging. Marginal mandibular resection is contraindicated in OSCC cases with a radiologically confirmed invasion of the cancellous bone only (Wolff et al. 2012; Abler et al. 2005; Muscatello et al. 2010; Gou et al. 2018). Consequently, most authors agree that a segmental resection is recommended in the case of invasion of the mandibular cancellous bone to achieve a complete, free-margin resection.
Interestingly, the tumor invasion of the mandible appears to have minor prognostic value on the long-term survival of patients with OSCC (Mücke et al. 2011), and the extent of (radical) bone resection (marginal or segmental resection) failed to reveal a significant influence on local recurrence and long-term survival rates (Muñoz Guerra et al. 2003; Gou et al. 2018). However, a positive statistical correlation was reported for intraosseous tumor size and local recurrence rate (Guerra et al. 2003).
Despite these interpretations, local recurrence appears to more likely depend on soft tissue tumorous findings in cases of simultaneous soft tissue and mandibular involvement. Therefore, only segmental resection was recommended in selected cases (O’Brien et al. 2003). This supports the opinion that marginal resection can be as effective as segmental resections in terms of local recurrences (Wolff et al. 2004; Patel et al. 2008; Rao et al. 2012; Brown et al. 2002). However, as the extent of osseous resection has come to a general agreement as stated in the German S3 guideline (Wolff et al. 2012), the role of mucosal recurrences in T4 OSCCs with previous mandibular infiltration was also evaluated critically by Moratin et al. (Moratin et al. 2020). The authors revealed that the localization of tumorous bone invasions is a decisive variable when making decisions for the extent of mandibular resection and recommended that segmental resection is mandatory in anterior tumor localization.
Therefore, this study aimed to evaluate the prognostic value of both mandibular resection types and determine the risk of local recurrence depending on the type of resection and tumor localization. Further, we intended to analyze the correlation between the resection extent and risk of lymph node recurrence or secondary lymph node metastasis given their significant prognostic values (Safi et al. 2018).
Materials and methods
Ethical statement
All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. This retrospective study was approved by the Institutional Ethics Committee of the Technical University of Munich, Klinikum rechts der Isar (Approval no. 254/22 S-NP).
Patient population and treatment algorithm
All consecutive primary OSCC cases between January 2007 and December 2015 that underwent mandibular marginal or segmental resection at our department were included in this study. Patients who had recurrent tumors, positive history of radio-/radiochemotherapy in the head and neck area, or previous operations were excluded.
All patients underwent primary surgical treatment after preoperative staging. Based on clinical observation and computed tomography (CT), morphological signs of cortical erosion, or evident bone infiltration, resection procedures included marginal (group I) or segmental (group II) mandibulectomies. Marginal resection was performed if the tumor was attached to the bone surface or in the case of limited cortical erosion. Segmental resection was performed in the case of extensive tumor infiltration with cancellous bone involvement.
Investigated parameters
Data collection included sex, age, TNM classification, type of neck dissection, reconstruction method, preoperative CT and postoperative pathological findings, surgical duration (min), length of hospital stay (days), and local recurrence rate. According to the guidelines and preoperative decision of the tumor board, neck dissection was conducted in level I–III ipsilateral of the tumor location. In case of intraoperatively detected positive lymph nodes an extended neck dissection was performed in levels IV and V ipsilateral and levels I–III contralateral. In cases with tumors crossing the centerline, neck dissection levels I–III were conducted on both sides. Tumor localizations were categorized corresponding to Urken’s classification describing defects. TNM staging was based on the seventh and eighth editions of the UICC TNM staging system and on postoperative pathological findings. T4a tumors involved both medullary mandibular and soft tissue extension.
Additionally, subgroups were defined as follows:
-
(A)
With regard to radiological bone involvement based on preoperative CT staging imaging: r0, tumor without bone contact; r1, tumor attached to the bone; r2, tumor erosion/infiltration of the bone.
-
(B)
With regard to histologically confirmed bone involvement: h0, no infiltration of the bone; h1, tumor erosion/infiltration of the bone.
-
(C)
With regard to radiological lymph node status based on preoperative CT staging imaging: rlk0, unobtrusive lymph nodes; rlk1, suspicious lymph nodes; rlk2, metastatic lymph nodes.
-
(D)
With regard to histologically confirmed lymph node involvement: plk0, negative lymph node involvement; plk1, positive lymph node involvement.
Statistical analysis
To calculate the differences between groups I and II with regard to the local recurrence rate, two-proportion z-tests were used. For datasets following a normal distribution, such as time of postoperative local recurrence, surgical duration, and length of hospital stay, unpaired t tests were used. The correlation between preexisting risk factors and outcome variables was assessed by logistic regression analysis. The statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 25 (IBM Corp., Armonk, NY, USA), and p values < 0.05 were considered statistically significant. Lymph node recurrences and secondary lymph node metastasis were summarized to calculate possible clinically relevant differences caused by an expected low statistical power. G-Power (version 3.1.9.4) was used for power calculation for the analysis of lymph node recurrences/secondary lymph node metastasis.
Results
Study population
A total of 180 patients (48 female [27%], 132 male [73%]) with primary OSCC who underwent marginal (group I, n = 85) or segmental (group II, n = 95) mandibular resection were included in this study. The median age of the patients was 61 (27–82) years; 75.2% of the patients were smokers, 7.1% had type II diabetes, and 61% indicated alcohol abuse. As regards the American Society of Anesthesiologists status, 13.5% were in class I, 67.4% in class II, 19.1% in class III, and 0% in class IV.
The patients were reconstructed according to the reconstructive standard after oncological resection. Here, group I was reconstructed with different microvascular grafts and group II either with alloplastic titanium plate plus microvascular flap or with a microvascular bone flap. Bony mandibular reconstruction with a microvascular bone graft (fibula or iliac crest) was performed freehand, partially adjusted with a resection guide (KLS ReconGuide), or CAD/CAM planed (Weitz et al. 2023).
Specifications of groups I and II with regard to the tumor localization (Urken’s classification), TNM classification, grading, resection status, and adjuvant therapy regimen are presented in Table 1. Logistic regression analysis of T-classification and resection type (marginal vs. segmental) showed statistical significance (regression coefficient, 1.104; p < 0.001).
The distribution of patients with marginal and segmental resection with regard to the results of preoperative CT and postoperative pathological findings are shown in Table 2.
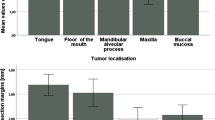
Surgical duration and hospitalization
The total median operation time of all patients was 573 (282–960) min. The median operation time of group II was significantly higher than that of group I [616.5 (321–960) and 533 (282–735) min, respectively; p < 0.001]. Moreover, group II had a significantly longer hospital stay [19 (7–81) and 15 (7–100) days, respectively; p = 0.025] (Figs. 1 and 2).
Local recurrence rate
The local recurrence rates for groups I and II in total and subgroups with regard to preoperative CT and postoperative pathological findings are presented in Table 3. In total, the local recurrence rate in group I was similar to that of group II (28.2% and 27.4%; p = 0.897). Of 52 recurrent cases, 44 showed tumor recurrence arising from soft tissues, whereas only six cases showed bone recurrence alongside soft tissue involvement. Groups I and II comprised three recurrences with bone and soft tissue involvement each. Soft tissue recurrences were detected in 12 cases in group I and in 32 cases in group II. Group II had a higher local recurrence rate than group I (26.7% vs. 22.2%, p = 0.733) in subgroup r1 (radiological tumor attachment to the bone). In the same subgroup r1, patients without histologically confirmed pathological bone involvement presented similar tendencies of the local recurrence rate (37.5% vs. 20%, p = 0.301), such as patients with histologically positive lymph nodes (33.3% versus 23.1%, p = 0.745).
Radiological bone involvement: r0, tumor without bone contact; r1, tumor attached to the bone; r2, tumor erosion/infiltration of the bone. Histological bone involvement: h0, no infiltration of the bone; p1, tumor erosion/infiltration of the bone; plk1, positive lymph nodes.
For the calculation of differences between the two cohorts with regard to the local recurrence rate and lymph node recurrence rate, two-proportion z-tests were used. *p values < 0.05 were considered statistically significant.
Patients in the same subgroup with histologically confirmed tumor erosion/infiltration of the bone (h1) showed a higher local recurrence rate following marginal resections (33.3% versus 25%; p = 0.733). Contrarily, cases without bone contact in preoperative CT scans (subgroup r0), cancers with radiological diagnosis (subgroup r2), and those with histologically confirmed tumor erosion/bone infiltration (subgroup h1) had a higher local recurrence rate if they underwent marginal resection (29.2% versus 16.7%, p = 1.000; 40% versus 25%, p = 0.321; 27.3% versus 25%, p = 0.892). In contrast, patients in group II without any histologically confirmed bone infiltration (subgroup p0) showed a higher local recurrence rate (53.3% versus 31.5%; p = 0.119). The mean postoperative local recurrence time was 22.1 ± 21.3 months in group I and 20.1 ± 24.5 in group II (p = 0.766) and occurred 24 times in group I and 26 times in group II.
Lymph node recurrence/secondary lymph node metastasis
The calculated statistical power with an expected effect size of 0.1 only reached a very low level of power (0.16; G-Power Version 3.1.9.4). Therefore, in the analysis, no difference was found between lymph node recurrence and secondary lymph node metastasis. In total, the rates of lymph node recurrence and secondary lymph node metastasis in group I were significantly higher than those in group II (9.4% [n = 8] and 6.2% [n = 6], respectively; p = 0.001). All six patients in group II and seven out of eight patients in group I received adjuvant radio(chemo)therapy. Four of six patients in group II and three of eight patients in group I had lymph node recurrences, and the other half of the patients had secondary lymph node metastases. In the r0, r1, and h0 subgroups, group I had a higher lymph node recurrence rate/secondary lymph node metastasis rate than group II (8.3% and 0%, p = 0.464; 8.3% and 6.3%, p = 0.166; 9.3% and 12.5%, p < 0.001, respectively). However, subgroups r2 and p1 showed significantly higher rates of lymph node recurrence/secondary lymph node metastasis in group II (10% versus 9.2%, p = 0.024; 13.6% versus 6.5%, p < 0.001, respectively).
CT detection of pathological lymph nodes
Preoperative detection of pathological lymph nodes by CT scans showed a sensitivity of 99.2% and a specificity of 100% (Table 4).
For datasets following a normal distribution such as time of postoperative local recurrence and lymph node recurrence, unpaired t tests were used. *p values < 0.05 were considered statistically significant. CT, computed tomography.
Predictive factors for local and lymph node recurrence rate or secondary lymph node metastasis rate
Logistic regression was performed to analyze factors potentially predictive of the local recurrence rate, including the resection type, positive/negative lymph nodes, adjuvant therapy, or tumor location. A significant association was found between local recurrences and effectiveness of adjuvant radiotherapy and adjuvant radiochemotherapy (regression coefficient, 0.599, p = 0.042; Table 5). Furthermore, tumor location corresponding to Urken’s classification in total and tumor location corresponding to groups S and SB showed a significant correlation with the local recurrence rate (regression coefficients, − 0.738, − 1.099, and − 2.303; p = 0.004, 0.002, and 0.002, respectively). None of the patients in the BSB group suffered from local recurrence. Clinically relevant influencing factors such as resection type, positive/negative lymph nodes, or tumor size according to T-classification did not show any statistical significance in the logistic regression (Table 5). Logistic regression was also performed to detect the correlation between the rates of lymph node recurrence or secondary lymph node metastasis and the clinically relevant influencing factors mentioned above. Significances were detected between the rates of lymph node recurrence or secondary lymph node metastasis and tumor location analog to Urken’s classifications B, S, and SB (regression coefficients, − 1.997, − 3.807, and − 2.351; p < 0.001, 0.001, and 0.001, respectively). None of the patients in the BSB group suffered lymph node recurrence. Tumor location in total and other clinically relevant influencing factors did not show statistical significance in the logistic regression (Table 5).
The rates of local and lymph node recurrence/secondary lymph node metastasis according to tumor location are presented in Table 6. According to Urken’s classification, the SB group had a significantly lower local recurrence rate than the B group or in all patients (p = 0.004 and 0.014, respectively). Furthermore, the B group presented a higher local recurrence rate than the S group and all patients (p = 0.062 and 0.813, respectively). The RB group had a slightly higher and the S group a slightly lower local recurrence rate than other groups.
Group S showed fewer lymph node recurrences/metastases than the overall cohort and the B group (p = 0.055 and 0.056, respectively) and significantly fewer lymph node recurrences/metastases than the RB group (p = 0.008). The SB group had slightly lower and the RB and B groups slightly higher lymph node recurrence/secondary lymph node metastasis rates than other groups (Table 6).
Discussion
The tumor size and expected biomechanical stability of the remaining mandible determine the extent of the resection—marginal (I) versus segmental (II). According to our results there was a significant correlation between tumor size (T-classification) and resection type (marginal vs. segmental). Our data showed that segmental resections not only required significantly longer operation time but also led to a longer hospital stay (p < 0.001 and 0.025, respectively). Furthermore, segmental resections also bear a significant loss in the quality of life of patients (Dholam et al. 2019; Rogers et al. 2004). Still, with regard to recurrences, few compromises in the case of mandibular infiltrations are possible (Gou et al. 2018; Li et al. 2017).
Local recurrences
The local recurrence rates of both resection types (I versus II) were similar and comparable with the findings of other studies (Mücke et al. 2011; Wolff et al. 2004; Stoop et al. 2020). Cases with histological confirmation of preoperative radiological tumor proximity to the mandible (r1) were associated with a higher local recurrence rate, which was not statistically significant but remains clinically relevant. However, our results indicated that cortical erosion due to tumor progression had better outcomes than cancellous bone involvement (Li et al. 2017). Further, in cases with limited tumor involvement, marginal resections were reported to be safe with respect to recurrences (Muscatello et al. 2010; Gou et al. 2018; Guerra et al. 2003) in the underlying cortical bone, which serves as a possible protective barrier (Mücke et al. 2011; Li et al. 2017; Ash et al. 2000). In case of cancellous tumor infiltration, segmental resections were recommended regarding the survival rate (Gou et al. 2018). No higher local recurrence rates were detected in cases without histological tumor invasion (h0). If radiologically depicted tumor appears close to the mandible, periosteal fresh-frozen sections may be the answer to deciding whether a segmental resection must be performed (Wolff et al. 2012). This was also emphasized by Brown and Lewis, who summarized in their review that marginal resections can reach a safe resection margin; however, in 15.5% of the patients, bone invasion was noted although not primarily suspected. According to their conclusion, the extent of resection should be based on clinical observation and at least two imaging techniques (Brown et al. 2001). As the assessment of CT scans is impaired by metal artefacts, magnetic resonance imaging is an optimal additional imaging technique alongside CT because it can provide additional important information regarding the extent of cancellous bone involvement (Wolff et al. 2012). Furthermore, PET-CT represents a useful supplement for diagnosing bone invasion besides the imaging modalities mentioned above (Lin et al. 2021). Thus, over- or undertreatment due to imprecise preoperative radiological findings can be increasingly avoided. This aspect can be improved in our workflow, as our retrospective analysis shows; however, only three fresh-frozen sections were taken and two of them were positive for OSCC infiltration. Therefore, a consequent segmental resection, instead of a consecutive marginal resection, should have been decided in these cases.
The local recurrence rate was higher in group I, especially in cases with radiologically diagnosed and histologically confirmed tumor invasion. Even without statistical significance it was clinically plausible (p = 0.733). This finding is supported by the results of other authors (Mücke et al. 2011; Rogers et al. 2004; Ash et al. 2000). Interestingly, the local recurrence rate in cases without postoperative histological osseous tumor invasion was greater and close to statistical significance in group II (p = 0.072). These, partly contradicting, findings led us back to the fact that most local recurrences in our patients were found in the soft tissues. Segmental resections were mostly planned preoperatively in cases with at least cT2 tumor stage (cortical erosion) or cT4 (bone infiltration), which also have a great extent of soft tissues. Despite the risk of recurrences in higher T-stages, this was not detected to have a statistically significant influence in other investigations (Patel et al. 2008; Stoop et al. 2020). According to our results, the greatest risk of local recurrence was not due to the bone but to soft tissue recurrence. As the evaluation of free bony resection margins appears technically well controllable from an oncologic point of view with the use of intraoperative cytological assessment (Nieberler et al. 2020), local recurrences of soft tissues and lymph node recurrences/metastases remain an issue. Thus, tumor resections should be conducted less invasively in the bone (segmental resections should only be considered in case of medullar bone infiltration) and more radically in soft tissues. Although recurrences mostly emerged from the soft tissue in our study, the potential likelihood of insufficient resection because of CAD/CAM surgery with fewer options to react easily should be further investigated. But none of these studies found a significant correlation between resection method and overall survival rate (Lin et al. 2014; Ma et al. 2022; Camuzard et al. 2017). In our opinion we would rather resect more bone than necessary, because we will achieve a good reconstruction anyway in CAD/CAM cases. In fact, the described risk factors like presence of advanced tumor stage, positive/close surgical margins, or nodal, vascular, or perineural invasion have a greater impact on survival rate than the type of bony tumor resection and reconstruction (Lin et al. 2014; Ma et al. 2022; Camuzard et al. 2017).
Lymph node recurrences or secondary lymph node metastases
Our results showed that segmental resections resulted in higher rates of lymph node recurrences or secondary lymph node metastases in cases with radiologically diagnosed and histologically confirmed bone infiltration (p = 0.024 and p < 0.001, respectively). As extended tumors with higher T-classification have a greater risk of distant or lymph node metastases, this patient population must be closely monitored after surgery. For safe detection of lymph nodes, alongside physical examination, which can be difficult in irradiated necks, objective three-dimensional imaging appears necessary. The calculated specificity of 100% exceeds even the results from ultrasonography (Ash et al. 2000) and supports our suggestion. The significantly higher rates of lymph node recurrences or metastases even in subgroups r0, r1, and h0 can lead to the assumption that occult lymph node metastasis is possibly more likely to occur in large tumors with close bone proximity but without infiltration. Therefore, close cervical monitoring is necessary (Pentenero et al. 2005; Vassiliou et al. 2020). Nevertheless, the emergence of occult lymph node metastasis appears to be not only dependent on tumor size, but also on multiple, genetic, and tumor biological factors (Méndez et al. 2011; Myo et al. 2005).
Predictive factors for recurrences
In the logistic regression, the calculated statistically significant risk factors turned out to be (a) adjuvant therapy and (b) tumor localization for local recurrences. Concerning lymph node recurrences or metastases, none of the calculated risk factors reached statistical significance. Further, the lower rates of tumor infiltration localization of SB and S according to Urken’s classification (Brown et al. 2016) reached statistical significance in further analyses for local and lymph node recurrences or metastases. Moratin et al. already reported that localization might influence local and lymph node recurrences/metastases. Unlike our findings, which indicate the body and ramus (B and RB) to be an area of risk, Moratin et al. found the anterior mandible (S) to have an increased risk of local recurrence (Moratin et al. 2020). In our study, tumors with greater extension from the symphysis to the body of the jaw (SB) showed significantly fewer local recurrences and tendencies for fewer lymph node recurrences or metastases. This might be due to the greater extent of tumor/soft tissue resection. Furthermore, the anterior region (S and SB) provides better access and overview for tumor resection than the posterior region (B and RB).
Limitations
The retrospective design of this study has known weaknesses. Even in our head and neck cancer department, the mandible is affected in only a small fraction of patients with tumors. This makes large numbers hardly achievable in a prospective study in a reasonable time frame. Moreover, the eight-year study period might lead to the assumption that any changes to the team of surgeons can influence surgical outcomes. This argument can be weakened by the consistent teaching mentality of our experienced surgeons toward residents, which leads to reliable and quick results (Zhu et al. 2021; Han et al. 2022). Furthermore, tumor surgeries are always led by a senior consultant.
The site of mandibular tumor infiltration and consequently the resection site appear to influence the postoperative quality of life. Resections including the symphysis are reported to achieve a lower postoperative quality of life (Warshavsky et al. 2019), which include tumor resection localizations of class S according to Urken’s classification. By contrast, B and R tumors appear to be associated with better quality of life (Warshavsky et al. 2019); however, our data revealed that the local recurrence rate is significantly higher (Table 6). This must be considered in the long-term evaluation of the quality of life with respect to recurring operations, which can lower the overall quality of life.
According to O’Brien et al., recurrences mostly emerged from soft tissues, especially in cases of incomplete resection with positive resection margins (O’Brien et al. 2003). In our cases, histological resection margins were mostly classified as R0 postoperatively; however, 13 cases were graded R1 and two R2, emphasizing the value of 3D soft tissue imaging and clinical examination after surgery in cases of mandibular tumor invasion.
Conclusions
Lymph node recurrence and secondary lymph node metastasis rates were significantly higher in the group of marginal resections. No significant differences in local recurrences could be detected between marginal and segmental resection types, but initial tumor location had an impact on local and lymph node recurrence rates. Urken’s classification SB and S showed significantly fewer local and lymph node recurrences/metastases. As the occult metastasis rate remains high and recurrences predominantly emerge from soft tissues and rarely from the bones, close clinical examination and 3D imaging of soft tissues form an important combination to detect recurrences in this vulnerable patient population. Furthermore, we recommend a less invasive tumor ablation in the bone and a more radical resection in soft tissues.
Data availability
The data presented in this study are available on request from the corresponding author.
References
Abler A, Roser M, Weingart D (2005) On the indications for and morbidity of segmental resection of the mandible for squamous cell carcinoma in the lower oral cavity. Mund Kiefer Gesichtschir 9(3):137–142. https://doi.org/10.1007/s10006-005-0607-7
Ash CS, Nason RW, Abdoh AA, Cohen MA (2000) Prognostic implications of mandibular invasion in oral cancer. Head & neck 22(8):794–798. https://doi.org/10.1002/1097-0347(200012)22:8<794::aid-hed8>3.0.co;2-w
Brown JS, Lewis-Jones H (2001) Evidence for imaging the mandible in the management of oral squamous cell carcinoma: a review. Br J Oral Maxillofac Surg 39(6):411–418. https://doi.org/10.1054/bjom.2001.0717
Brown JS, Kalavrezos N, D’Souza J, Lowe D, Magennis P, Woolgar JA (2002) Factors that influence the method of mandibular resection in the management of oral squamous cell carcinoma. Br J Oral Maxillofac Surg 40(4):275–284. https://doi.org/10.1016/s0266-4356(02)00116-x
Brown JS, Barry C, Ho M, Shaw R (2016) A new classification for mandibular defects after oncological resection. Lancet Oncol 17(1):e23-30. https://doi.org/10.1016/S1470-2045(15)00310-1
Camuzard O, Dassonville O, Ettaiche M, Chamorey E, Poissonnet G, Berguiga R, Leysalle A, Benezery K, Peyrade F, Saada E, Hechema R, Sudaka A, Haudebourg J, Demard F, Santini J, Bozec A (2017) Primary radical ablative surgery and fibula free-flap reconstruction for T4 oral cavity squamous cell carcinoma with mandibular invasion: oncologic and functional results and their predictive factors. Eur Arch Otorhinolaryngol 274(1):441–449. https://doi.org/10.1007/s00405-016-4219-7
Dholam KP, Sadashiva KM, Gurav S (2019) Study of Quality of Life in Patients with Soft Tissue Reconstruction Following Mandibulectomy. Journal of Maxillofacial and Oral Surgery 18(2):266–272. https://doi.org/10.1007/s12663-018-1122-3
Eichberger J, Weber F, Spanier G et al (2022) Loss of MMP-27 Predicts Mandibular Bone Invasion in Oral Squamous Cell Carcinoma. Cancers 14(16):4044. https://doi.org/10.3390/cancers14164044
Guerra MF, Campo FJ, Gías LN, Pérez JS (2003) Rim versus sagittal mandibulectomy for the treatment of squamous cell carcinoma: two types of mandibular preservation. Head Neck 25(12):982–989. https://doi.org/10.1002/hed.10316
Han SH, Kim YC, Kwon TK, Lee DY (2022) Cumulative sum analysis of the learning curve of free flap reconstruction in head and neck cancer patients. Clin Exp Otorhinolaryngol 15(2):177–182. https://doi.org/10.2153/ceo.2021.01053
Li C, Lin J, Men Y, Yang W, Mi F, Li L (2017) Does medullary versus cortical invasion of the mandible affect prognosis in patients with oral squamous cell carcinoma? J Oral Maxillofac Surg 75(2):403–415. https://doi.org/10.1016/j.joms.2016.08.005
Lin CH, Kang CJ, Tsao CK, Wallace CG, Lee LY, Lin CY, Wang HM, Ng SH, Yen TC, Liao CT (2014) Priority of fibular reconstruction in patients with oral cavity cancer undergoing segmental mandibulectomy. PLoS ONE 9(4):e94315. https://doi.org/10.1371/journal.pone.0094315
Lin NC, Su IH, Hsu JT, Tsai KY, Chen MYC (2021) FDG-PET predicts bone invasion and prognosis in patients with oral squamous cell carcinoma. Sci Rep 11(1):15153. https://doi.org/10.1038/s41598-021-94567-w
Ma H, Shujaat S, Bila M, Nanhekhan L, Vranckx J, Politis C, Jacobs R (2022) Survival analysis of segmental mandibulectomy with immediate vascularized fibula flap reconstruction in stage IV oral squamous cell carcinoma patients. J Stomatol Oral Maxillofac Surg 123(1):44–50. https://doi.org/10.1016/j.jormas.2020.12.003
Méndez E, Lohavanichbutr P, Fan W et al (2011) Can a metastatic gene expression profile outperform tumor size as a predictor of occult lymph node metastasis in oral cancer patients? Clin Cancer Res 17(8):2466–2473. https://doi.org/10.1158/1078-0432.CCR-10-0175
Moratin J, Horn D, Metzger K et al (2020) Squamous cell carcinoma of the mandible - Patterns of metastasis and disease recurrence in dependence of localization and therapy. Journal of Cranio-Maxillo-Facial Surgery : Official Publication of the European Association for Cranio-Maxillo-Facial Surgery 48(12):1158–1163. https://doi.org/10.1016/j.jcms.2020.10.006
Mücke T, Hölzle F, Wagenpfeil S, Wolff KD, Kesting M (2011) The role of tumor invasion into the mandible of oral squamous cell carcinoma. J Cancer Res Clin Oncol 137(1):165–171. https://doi.org/10.1007/s00432-010-0870-3
Muñoz Guerra MF, Naval Gías L, Campo FR, Pérez JS (2003) Marginal and segmental mandibulectomy in patients with oral cancer: a statistical analysis of 106 cases. J Oral Maxillofac Surg 61(11):1289–1296. https://doi.org/10.1016/s0278-2391(03)00730-4
Muscatello L, Lenzi R, Pellini R, Giudice M, Spriano G (2010) Marginal mandibulectomy in oral cancer surgery: a 13-year experience. Eur Arch Oto-Rhino-Laryngol 267(5):759–764. https://doi.org/10.1007/s00405-009-1045-1
Myo K, Uzawa N, Miyamoto R, Sonoda I, Yuki Y, Amagasa T (2005) Cyclin D1 gene numerical aberration is a predictive marker for occult cervical lymph node metastasis in TNM Stage I and II squamous cell carcinoma of the oral cavity. Cancer 104(12):2709–2716. https://doi.org/10.1002/cncr.21491
O’Brien CJ, Adams JR, McNeil EB et al (2003) Influence of bone invasion and extent of mandibular resection on local control of cancers of the oral cavity and oropharynx. Int J Oral Maxillofac Surg 32(5):492–497
Pandey M, Rao LP, Das SR, Mathews A, Chacko EM, Naik BR (2007) Patterns of mandibular invasion in oral squamous cell carcinoma of the mandibular region. World J Surg Oncol 5(1):12. https://doi.org/10.1186/1477-7819-5-12
Patel RS, Dirven R, Clark JR, Swinson BD, Gao K, O’Brien CJ (2008) The prognostic impact of extent of bone invasion and extent of bone resection in oral carcinoma. Laryngoscope 118(5):780–785. https://doi.org/10.1097/MLG.0b013e31816422bb
Pentenero M, Gandolfo S, Carrozzo M (2005) Importance of tumor thickness and depth of invasion in nodal involvement and prognosis of oral squamous cell carcinoma: a review of the literature. Head Neck 27(12):1080–1091. https://doi.org/10.1002/hed.20275
Rao LP, Shukla M, Sharma V, Pandey M (2012) Mandibular conservation in oral cancer. Surg Oncol 21(2):109–118. https://doi.org/10.1016/j.suronc.2011.06.003
Rogers SN, Devine J, Lowe D, Shokar P, Brown JS, Vaugman ED (2004) Longitudinal health-related quality of life after mandibular resection for oral cancer: a comparison between rim and segment. Head Neck 26(1):54–62. https://doi.org/10.1002/hed.10351
Safi AF, Kauke M, Grandoch A, Nickenig HJ, Zöller J, Kreppel M (2018) The importance of lymph node ratio for patients with mandibular infiltration of oral squamous cell carcinoma. J Cranio-Maxillo-Fac Surg 46(6):1007–1012. https://doi.org/10.1016/j.jcms.2018.03.021
Spiesecke P, Neumann K, Wakonig K, Lerchbaumer MH (2022) Contrast-enhanced ultrasound (CEUS) in characterization of inconclusive cervical lymph nodes: a meta-analysis and systematic review. Sci Rep 12(1):7804. https://doi.org/10.1038/s41598-022-11542-9
Stoop CC, de Bree R, Rosenberg AJWP, van Gemert JTM, Forouzanfar T, Van Cann EM (2020) Locoregional recurrence rate and disease-specific survival following marginal vs segmental resection for oral squamous cell carcinoma with mandibular bone invasion. J Surg Oncol 122(4):646–652. https://doi.org/10.1002/jso.26054
Vassiliou LV, Acero J, Gulati A et al (2020) Management of the clinically N(0) neck in early-stage oral squamous cell carcinoma (OSCC). An EACMFS position paper. J Cranio-Maxillo-Facial Surg 48(8):711–718. https://doi.org/10.1016/j.jcms.2020.06.004
Warshavsky A, Fliss DM, Frenkel G et al (2019) Quality of life after mandibulectomy: the impact of the resected subsite. Int J Oral Maxillofacial Surg 48(10):1273–1278. https://doi.org/10.1016/j.ijom.2019.02.013
Weitz J, Grabenhorst A, Singer H, Niu M, Grill FD, Kamreh D, Claßen CAS, Wolff KD, Ritschl LM (2023) Mandibular reconstructions with free fibula flap using standardized partially adjustable cutting guides or CAD/CAM technique: a three- and two-dimensional comparison. Front Oncol 9(13):1167071. https://doi.org/10.3389/fonc.2023.1167071
Wolff D, Hassfeld S, Hofele C (2004) Influence of marginal and segmental mandibular resection on the survival rate in patients with squamous cell carcinoma of the inferior parts of the oral cavity. J Cranio-Maxillo-Fac Surg 32(5):318–323. https://doi.org/10.1016/j.jcms.2004.05.005
Wolff KD, Follmann M, Nast A (2012) The diagnosis and treatment of oral cavity cancer. Deutsches Arzteblatt International 109(48):829–835. https://doi.org/10.3238/arztebl.2012.0829
Zhu W-y, Choi WS, Wong MCM, Pu JJ, Yang W-f, Su Y-x (2021) The learning curve of computer-assisted free flap jaw reconstruction surgery using 3d-printed patient-specific plates: a cumulative sum analysis. Front Oncol 11:737769. https://doi.org/10.3389/fonc.2021.737769
Acknowledgements
We would particularly like to thank Dr. Sonja Grill, PhD, MSc, for her statistical consultations and Enago for language corrections.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding.
Author information
Authors and Affiliations
Contributions
LMR: study concept, literature, writing of manuscript; MN: data acquisition, data analysis and interpretation, writing of manuscript, literature research, and acquisition of ethical approval; VS: data acquisition and interpretation; CC: data interpretation and literature research; HS: radiographic investigation and interpretation and literature research; AMF: operation planning and manuscript editing; K-DW: study concept, manuscript editing, and leading surgeon; FDG: study concept, data analysis, writing of manuscript, acquisition of ethical approval, and literature research.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no financial or nonfinancial competing interests.
Ethical approval
All clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. This retrospective study was approved by the Institutional Ethics Committee of the Technical University of Munich, Klinikum rechts der Isar (Approval no. 254/22 S-NP).
Consent to participate and to publish
Patient consent was not applicable and waived due to the retrospective nature of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ritschl, L.M., Niu, M., Sackerer, V. et al. Effect of segmental versus marginal mandibular resection on local and lymph node recurrences in oral squamous cell carcinoma: is tumorous bone infiltration or location and resulting soft tissue recurrences a long-term problem?. J Cancer Res Clin Oncol 149, 11093–11103 (2023). https://doi.org/10.1007/s00432-023-04963-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04963-0