Abstract
Purpose
Neoantigens produced from mutations in tumors are important targets of T-cell-based immunotherapy and immune checkpoint blockade has been approved for treating multiple solid tumors. We investigated the potential benefit of adoptive neoantigen-reactive T (NRT) cells in combination with programmed cell death protein 1 inhibitor (anti-PD1) for treating lung cancer in a mouse model.
Methods
NRT cells were prepared by co-culturing T cells and neoantigen-RNA vaccine-induced dendritic cells. Then, adoptive NRT cells in combination with anti-PD1 were administered to tumor-bearing mice. Pre- and post-therapy cytokine secretion, antitumor efficacy, and tumor microenvironment (TME) changes were determined both in vitro and in vivo.
Results
We successfully generated NRT cells based on the 5 neoantigen epitopes identified in this study. NRT cells exhibited an enhanced cytotoxic phenotype in vitro and the combination therapy led to attenuated tumor growth. In addition, this combination strategy downregulated the expression of the inhibitory marker PD‐1 on tumor-infiltrating T cells and promoted the trafficking of tumor-specific T cells to the tumor sites.
Conclusion
The adoptive transfer of NRT cells in association with anti-PD1 therapy can exert an antitumor effect on lung cancer, and is a feasible, effective, and novel immunotherapy regimen for treating solid tumors.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Globally, lung cancer is the most common cancer, with China ranking first in the number of cancer-related deaths (Siegel et al. 2021; Zheng et al. 2022). Surgical interventions in the early stages and systemic treatments (such as chemotherapy, radiotherapy, targeted therapy, and immunotherapy) in advanced stages of lung cancer prolong the survival of patients. However, cancer statistics report the 5-year survival rate for all stages is 21% and only 6% for metastatic lung cancer (Siegel et al. 2021). However, targeted drugs and checkpoint inhibitors (ICIs) recently have drastically improved the prognosis of patients and become the foundation of first-line therapy for the specified types of metastatic non-small cell lung cancer (NSCLC). Unfortunately, patients with negative driving genes or low expression of programmed cell death protein 1 (PD1)/ programmed cell death ligand 1 (PD-L1) do not respond well to these treatments (Grant et al. 2021; Soria et al. 2018; Reck et al. 2016). Therefore, new therapies or combining different therapies are crucial for improving the survival and life quality of patients with NSCLC.
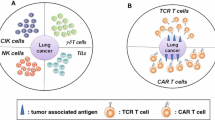
Cancer immunotherapy was ranked among the top ten scientific breakthroughs in 2013 by Science. Modern immunology offers three immunotherapeutic approaches based on T cells to treat cancer: ICIs, a method that is designed to “unleash” immunosuppressive T-cell responses; cancer vaccines, which have either prophylactic or therapeutic effect; and adoptive cell therapy (ACT), based on the transfusion of immunocompetent cells in the body to directly kill cancer cells or stimulate an immune response. ICIs have revolutionized cancer treatment and 25% of patients who received ICIs showed a positive response. ICIs are now FDA-recommend for the treatment of types of cancer (Thompson 2018). PD1 is primarily expressed in CD8 + T and CD4 + T cells; whereas its ligands, PD-L1/L2, are expressed in cancer cells, stromal cells, and some immune cells in the tumor microenvironment (TME). The activation of the PD1 signaling pathway inhibits T-cell proliferation and impairs effector cell cytotoxicity and cytokine secretion (Pardoll 2012), which is crucial for immune evasion. However, anti-PD1/PD-L1 antibodies can reinvigorate the stifled immune response, inducing a potent antitumor response (Bagchi et al. 2021). ACT, represented by chimeric antigen receptor T cells (CAR-T), tumor-infiltrating lymphocytes (TILs), and T-cell receptor-engineered T (TCR-T) therapy, has become the focus of research and clinical practice since Professor Rosenberg published promising results of TILs therapy in 2002 (Dudley et al. 2002). ACT is based on immune cells, which isolate tumorfighting immune cells from the tissue or circulating blood of the patient. After the screening, engineering modification, amplification, cell function identification, and quality inspection, the immune cells are infused back into the patients (Tran et al. 2014, 2016; Zacharakis et al. 2018; Morgan et al. 2006; Kochenderfer et al. 2010). ACT helps to “liberate” highly reactive T-cell subpopulations from the host TME and provides a good expansion environment that is not restrained by normal tolerance mechanisms to fulfill the clinical infusion cell numbers requirement. Currently, there are 47 and 34 clinical trials involving TILs and CAR-T ACT therapy for solid tumors and hematological malignancies, respectively.
The concept of neoantigen was first proposed by Professor Gross in 1943 who hypothesized that neoantigens can be a suitable target for cancer immunotherapy (Gross 1943; Ward et al. 2016). During the 1980s, Professor Boon and other researchers also demonstrated that somatic gene mutations were the source of neoantigens that can be recognized by T cells in tumors (Plaen et al. 1988; Wölfel et al. 1995). The malignant transformation of cells is due to the continuous accumulation of genomic DNA damage (Jiang et al. 2019). These mutations can cause tumors to express mutant proteins termed neoantigens, which are tumor-specific and not expressed in normal cells. The immune system has an inherent ability to distinguish self from non-self and neoantigens become an ideal target to be recognized by T cells, thereby stimulating antitumor immunity (Schumacher and Schreiber 2015; Castle et al. 2012). Previous studies have shown that the higher neoantigen mutation burden was positively associated with stronger T-cell response, more TILs infiltrating, and better prognosis of patients (Rooney et al. 2015; Howitt et al. 2015). RNA-sequencing (RNA-seq) data published by The Cancer Genome Atlas (TCGA) based on 18 solid tumors revealed that the gene expression signature of cytotoxic T cells was positively correlated with the number of neoantigens in each tumor. Furthermore, early clinical data also showed that neoantigen load had a predictive role in the responses to ICIs and ACT in patients with NSCLC (Friese et al. 2020; Goodman et al. 2017; Hellmann et al. 2018).
Early research based on neoantigens mainly focused on vaccines owing to their advantages of preventing “off-target” and immune tolerance. Furthermore, tumor-specific T-cell responses induced by neoantigen vaccines can also induce immune memory to prevent tumor recurrence (Li et al. 2017; Lauss et al. 2017). In 2017, Professor Sahin first reported the application of personalized mutation RNA vaccines in patients with melanoma. The results showed that the vaccine stimulated an immune response to a variety of specific neoantigens (Sahin et al. 2017). Zhenyu Ding reported that the personalized neoantigen pulsed dendritic cell vaccine achieved an objective effectiveness rate of 25% and a disease control rate of 75% in 12 patients with advanced lung cancer (Ding et al. 2021). In 2021, to the best of our knowledge, we provided the first report on the good efficacy of neoantigen-reactive T cells induced by RNA vaccine in a mouse model with lung cancer (Sun et al. 2021).
Despite the promising efficacy of neoantigen-reactive T (NRT)-ACT observed in animal experiments, it is associated with certain limitations such as infiltration, recognition, killing, and durable survival in the immunosuppressive TME of solid tumors similar to CAR-T and TILs-ACT treatments (Martinez and Moon 2019; Anderson et al. 2017; Krenciute et al. 2017; Zabel et al. 2019; Drent et al. 2019; Eyquem et al. 2017). Therefore, breaking through these bottlenecks by improving the ability of T cells and regulating the TME has become the prime focus of ACT research. Recent studies have shown that the PD1 or cytotoxic T lymphocyte-associated protein 4 (CTLA-4) pathways are the key regulators of T‐cell exhaustion, and ICIs can reactivate the antitumor T‐cell immunity in the suppressive TME (Pauken and Wherry 2015; Thommen and Schumacher 2018). In a recent study, the combination of neoantigen peptide vaccine with PD1 inhibitor (nivolumab) in advanced lung cancer showed synergistic effects, which stimulated a durable neoantigen-specific T-cell response, increased cytotoxic T-cell migration to the tumor, and promoted the spread of neoantigen epitopes (Ott et al. 2020). A phase 1 trial for anti-PD1-resistant metastatic lung cancer showed that TILs-ACT administered with nivolumab is generally safe and clinically active (Creelan et al. 2021). These findings indicate the efficacy of the synergistic action of ICIs and ACT in cancer immunotherapy. However, whether anti-PD1 functions in adoptive NRT cells of lung cancer remains to be ascertained.
To address the limitations of our previous research and the barriers of ACT in solid tumors, in the present study, we first optimized the neoantigen screening methods and then transferred NRT cells along with the PD‐1 inhibitor in the NSCLC mouse model. This study may provide a new strategy for improving the efficacy of ACT for solid tumors.
Materials and methods
Materials
The reagents and antibodies used in the present study are listed in Table S1.
Cell culture
Lewis cells and B16 cells, a murine NSCLC and melanoma cell line, were obtained from the American Type Culture Collection. The cells were cultured in the Roswell Park Memorial Institute (RPMI)-1640 medium, supplemented with 10% fetal bovine serum (FBS) and 1% penicillin and streptomycin at 37 °C in the presence of 5% CO2.
Mouse strains
The study was performed using 6–8‐week‐old sex-matched C57BL/6 mice purchased from Vital River Laboratory Animal Technology Co. Ltd. All mice were housed and bred under specific pathogen-free conditions at Shanghai East Hospital, Tongji University School of Medicine, and the protocol was approved by the Ethics Committee of Tongji University (TJBB03721106).
Tumor‐bearing mouse model
Conventional T cells were prepared by injecting 2 × 106 Lewis cells into the flank of the C57BL/6 mice, whereas ACT experiments were performed by injecting 0.5 × 106 Lewis cells into the mice. The tumor volume was measured every other day and calculated by the following formula: length × width2/2.
Generation of antigen-presenting cells (dendritic cells (DCs))
Bone marrow-derived DCs (BMDCs) were induced as described previously (Roney 2019). Briefly, the mice were euthanized by CO2 inhalation, their bone marrow cells were then flushed out from the femur, and resuspended and grown in the complete RPMI-1640 medium (55 μM 2-mercaptoethanol, 10 mM of HEPES, 10% heat-inactivated FBS, and 1% penicillin and streptomycin) containing 20 ng/mL granulocyte–macrophage colony-stimulating factor (GM-CSF) during the first three days and 10 ng/mL GM-CSF during the following seven days at 37 °C and 5% CO2. The complete medium was supplemented with 10 ng/mL interleukin (IL)-4 from the 6th day to the 10th day. On day 10, BMDCs, which were floating or lightly adherent in the culture, were harvested.
T-cell preparation
The T cells of tumor-bearing mice were isolated as described previously (Sun et al. 2021). Briefly, when the tumor could be palpated subcutaneously, a single-cell suspension was prepared from the spleen of the tumor-bearing mice. Then, T cells were isolated by negative selection using Miltenyi Pan T Cell Isolation Kit II. The purity of the T cells obtained by this method was more than 90%.
Cancer neoantigen prediction
As reported previously (Sun et al. 2021), whole-exome sequencing (WES) and RNA-seq of normal tissues and Lewis cells were performed first. Mutated genes that could express abnormal proteins were selected by comparing with UCSC Genome Brower and then normalized to reads per kilobase million units (Chen et al. 2019). Furthermore, candidate neoantigen epitopes were predicted using the MuPeXI pipeline and MuTect2 system (Bjerregaard et al. 2017; Kim et al. 2019).
Neoantigen long-peptide synthesis
A total of 10 candidate neoantigen peptides (length: 27 amino acids) were synthesized by solid-phase peptide synthesis and purified using reverse-phase high-performance liquid chromatography (GenScript, USA) with strict quality control (purity: > 98%). Each predicted neoantigen epitope was designed for one synthetic long-peptide (SLP) vaccine (Sangon Biotech (Shanghai) Co. Ltd).
Peptide pulsing and screening
The IFN-γ ELISpot-Plus kit was used to pulse and screen the SLP vaccine according to the manufacturer’s instructions. Briefly, 2 × 104 DCs were stimulated with 0.15 μg of the SLP vaccine for 24 h in a 96-well plate. Then, 2 × 105 T cells were co-cultured with peptide-simulated-DCs for another 24 h. The remaining steps are the same as the interferon γ (IFN-γ) enzyme-linked immunosorbent spot (ELIspot) assay reported previously (Sun et al. 2021).
Generation of in vitro-transcribed RNA (IVT- RNA)
The detailed methodology has been published elsewhere (Tran et al. 2014; Sun et al. 2021). Before preparing IVT-RNA, we first built tandem minigene (TMG) according to five neoantigen sequences and then inserted it into the pcDNA3.1 vector to construct a DNA template for IVT-RNA (Sangon Biotech (Shanghai) Co. Ltd). RNA purity and concentrations were assessed using the NanoDrop spectrophotometer. RNA was then aliquoted into micro tubes and stored at − 80 °C until further use.
Preparation of neoantigen-reactive T cells
DCs were transfected with IVT-RNA using Amaxa Mouse DC Nucleofector Kit to generate neo-DCs as published previously. A quantitative polymerase chain reaction (PCR) was performed to assess the transfection condition. A minigene-specific primer (forward: TTCAGCAGCTCAGCCACC; reverse: AGCAACAATGCCCACGAT) and a primer for β-actin (forward: GGTCCACACCCGCCACCAG; reverse: CACATGCCGGAGCCGTTGTC) were purchased from Life Technologies. PCR was performed using Advanced Master Mix and the 7500 Fast Real-Time PCR machine, and all calculated threshold cycles were 30 or less.
These neo-DCs were co-cultured with T cells in a ratio of 1:4 in a complete medium at 37 °C in the presence of 5% CO2 for 8 h. Then, 100 U/mL IL-2 was added to the medium for another 48 h. From day 3, 20 ng/mL IL-7, 6000 U/mL IL-2, and 30 ng/mL VivoMAb anti-mouse CD3ε were added to the complete medium. The neo-DCs were replenished for restimulation according to NRT cell growth. The medium was replaced starting at about three days and then every other day or as required post-stimulation. The NRT cells were harvested from day 10 to day 14 and were used for assays and adoptive therapy.
Flow cytometry
The anti‐mouse monoclonal antibodies used for cell surface staining were: CD45, CD3, CD4, CD8, CD279 (PD‐1), CD137, CD62L, and CD45RA. CD45, CD11b, and F4/80 were used for staining tumor‐associated macrophages (TAMs). CD11c and major histocompatibility complex II were used for staining of DCs. CD4 and forkhead box P3 (Foxp3) were used for staining regulatory T (Treg) cells. After harvesting from the cultured T cells, DCs, or tumor-cell suspensions, the cells were incubated with the anti-mouse CD16/32 antibody for 10 min at room temperature to block fragment crystallizable (FC) receptors and then stained with surface staining antibodies for 30 min in the dark. After washing twice, the cells were assayed using an Arial II‐Optics flow cytometer, and the data obtained were analyzed using the FlowJo_10.0 software. In some experiments, the Fixable Viability Stain dye was used to exclude dead cells before blocking FC receptors. Intracellular Foxp3 staining was performed using the anti-mouse Foxp3 staining set according to the manufacturer’s instructions.
To determine the intracellular IFN‐γ, granzyme B, and tumor necrosis factor-alpha (TNF-α) levels in T cells, 1 × 106 T cells were stimulated using the cell activation cocktail for 4 h. Surface staining was performed before cell fixation and permeabilization. Then, the cells were incubated with cytokine antibodies for 30 min in the dark. The cells were washed twice with the Perm/Wash™ buffer before acquisition on an Arial II-Optics flow cytometer. All the experiments were performed in triplicates.
Enzyme-linked immunosorbent assay (ELISA)
T cells were co-cultured with Lewis and B16 cells in different ratios such as 1:1, 5:1, and 10:1 (1 × 105 Lewis cells) in a capture antibody‐coated 96‐well plate overnight. Then, the supernatants were collected and stored at − 80 °C for further experiments. The concentrations of IFN‐γ and TNF‐α in these supernatants were determined using ELISA kits following the manufacturer’s instructions.
Antitumor effects in vivo
As described earlier, 0.5 × 106 Lewis cells were injected into the C57BL/6 mice for ACT experiments. When tumors reached a volume of 50 mm3, the mice were randomized into four groups to receive cyclophosphamide (CTX, 100 mg/kg) for lymphodepletion (Day 1). We established four groups according to the ACT regimen: (1) Conventional T cells (T group), (2) Conventional T cells plus anti-PD1 (T + anti-PD1 group), (3) NRT cells (NRT group), and (4) NRT cells plus anti-PD1 (NRT + anti-PD1 group). A total of 1 × 107 T cells were injected into the mice through the tail vein (Day 0), and rIL‐2 (180,000 units) was injected intraperitoneally for three days (Days 1–3). The anti‐PD1 antibody (10 mg/kg) or an equal volume of phosphate‐buffered saline (PBS) was injected intraperitoneally four times (Days 7, 10, 13, and 16). The tumor volume was measured every other day and calculated by the following formula: length × width2/2. The mice were sacrificed on Day 35.
Histopathological analysis
The mouse lungs and intestines were resected and fixed with 3.5% formaldehyde. Further, hematoxylin and eosin (H&E) staining was performed by Pathology Institute of Service Biotechnology Co. Ltd (Wuhan, China). For immunofluorescence (IF) analysis, the resected tumor tissues were perfused with 0.1 M PBS (pH 7.4), embedded into an optimal cutting temperature compound, and frozen for cryosections. Primary antibodies used for IF staining were anti-CD3 and anti-CD137. Cy3-conjugated Goat anti-Rabbit IgG and FITC-conjugated Goat anti-Rabbit IgG were used as secondary antibodies. DAPI was used for nucleus staining. The microscopic analysis of the H&E-stained samples and IF images were performed by DS-U3 and ECLIPSE C1 Ortho-Fluorescent Microscopy (Nikon, Japan).
Statistical analysis
Statistical analyses were performed by the paired Student’s t test using GraphPad Prism 8.0. All data are presented as the mean ± standard error of the mean from three independent assays. *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 were considered statistically significant.
Results
Identification and screening of tumor neoantigen
The complex genetic phenotype and biochemical characteristics of organisms are determined by sequencing the nucleotides on the multinucleotide chain (Heather and Chain 2016). In the field of cancer immunology, the DNA and RNA sequences associated with tumorigenesis, development, and antitumor immunity lay a foundation for ACT based on neoantigens. Somatic gene products should be transcribed, translated, processed, and presented to MHC molecules as a prerequisite for stimulating an immune response. Therefore, the identification and affinity of MHC allelic expression is a key step in the prediction of neoantigens (Vogelstein et al. 2013; Lawrence et al. 2013). As mentioned previously, NSCLC has a higher mutation burden and more TILs infiltration, which makes it an ideal candidate for the adoptive transfer of NRT cells (Lawrence et al. 2013). As shown in Fig. 1a, we first identified the genetic mutations that are capable of expressing abnormal proteins by WES and RNA-seq. After that, 10 candidate neoantigens were predicated as previously reported (Sun et al. 2021) (Table 1).
Identification and screening of tumor neoantigens. a The scheme of vaccine preparation; b Mouse bone marrow cells were induced for 10 days; red arrows indicate typical dendritic cells (DCs); c Flow cytometry analysis for the purity of DCs (CD11C + MHCII +); d Neoantigen-specific T-cell response after DCs were loaded with the synthesized long-peptide (SLP)-vaccine and co-cultured with T cells
To assess the immunogenicity of the predicted neoantigens, we synthesized long-peptide vaccines (SLP vaccine) based on the neoantigen sequence, isolated and cultured DCs and T cells. As shown in Fig. 1b, the morphology of DCs under a microscope is very typical. Similar to the results of a previous study (Helft et al. 2015), we found that the purity of induced DCs (CD11C + MHCII +) can reach 48.68% (Fig. 1c) through flow cytometry analysis, which confirmed that the mouse BMDCs were successfully established. Then, DCs were stimulated with 10 SLP vaccines and co-cultured with T cells, after which IFN-γ ELISpot assays were performed to determine the T-cell-specific antigen response. Our results showed that 5 of the predicted 10 neoepitopes presented a significant immune response (Fig. 1d), confirming that the candidate neoantigens can stimulate a specific T-cell response.
Preparation of neoantigen-reactive T Cells
On the basis of the 5 neoepitopes that stimulated specific T-cell response, we prepared tandem minigene (TMG) and IVT-RNA vaccine based on previously reported methods (Tran et al. 2014; Sun et al. 2021) (Table 1 and Fig. 2a). IVT-RNA was then transfected into DCs by electroporation to generate Neo-DCs. Lastly, T cells and neo-DCs were co-cultured to produce NRT cells (Fig. 2b). Transfection efficiency was assessed using quantitative PCR, which showed that IVT-RNA was significantly upregulated in neo-DCs compared with that in conventional DCs (Fig. 2c). As shown in Fig. 2e and f, the CD3 + CD137 + T-cell ratio greatly increased from 0.022% in the conventional T group to 8.28% in the NRT group. In addition, the cell clusters in the neo-DCs and T cells co-culturing group significantly increased, indicating an augmented T-cell activation (Fig. 2d). The higher CD3 + CD137 + T-cell ratio suggested more tumor-specific T cells in the total transfer of ACT products and antitumor activity (Seliktar-Ofir et al. 2017; Krishna et al. 2020).
Preparation of neoantigen-reactive T (NRT) cells. a Basic structure of the tandem minigene (TMG) construct. A minigene construct encoding the amino acid sequence flanked by 12 wild-type protein sequences. Multiple minigenes were fused to generate the TMG construct; b The scheme of NRT cell production; c The expression of IVT-RNA determined through quantitative polymerase chain reaction (PCR) after extraction of total RNA from Neo-DCs and conventional DCs (Con-DCs); d T cells and DCs/Neo-DCs were co-cultured for 72 h. Images of cell clusters (T: left; NRT: right) under a microscope are shown; e The expression of CD3 and CD137 determined by flow cytometry (n = 3, error bars represent SD); f Activated T-cell percentage (CD3 + CD137 + T) in NRT cell preparation
NRT cell effector function assessment in vitro
T cells play a major role in eradicating cancer cells via cytokine secretion and direct killing of malignant cells, whereas memory T cells provide long-term protective immunity against cancer cells (Restifo et al. 2012; Reina-Campos et al. 2021). IFN-γ is a proinflammatory cytokine released from cytotoxic T lymphocytes (CTLs) with a cytotoxic function that has an antineoplastic effect during the cell-mediated adaptive immune response (Farhood et al. 2019; Ho et al. 2015). Along with IFN-γ, Granzyme B, perforin, and TNF-α are also major functions of CTLs that play an important role in antitumor immunity. Perforin is a pore-punching toxin that damages the cell membrane of the tumor or virus-infected cells through which cytotoxins, such as IFN-γ, Granzyme B, and TNF-α, enter the cytosol and initiate apoptosis. TNF-α binding to surface receptors elicits a wide range of biological activities, including cytostasis and hemorrhagic necrosis of tumor cells and tumors (Cullen et al. 2010; Vredevoogd et al. 2019). To investigate the effector function of NRT cells, we attempted to evaluate them through flow cytometry and ELISA assay in the present study. As expected, NRT cells showed increased secretion of IFN-γ and TNF-α than conventional T cells; however, it did not affect the production of Granzyme B (Fig. 3a–c). Meanwhile, ELISA results also showed more secretion of IFN-γ and TNF-α in the NRT group (Fig. 3d). To confirm the immune specificity of NRT to other tumor cells, we co-cultured T/NRT cells with B16 cells. As shown in Figure S1a-b, there was no difference in IFN-γ and TNF-α secretion by T/NRT cells co-culturing with B16 cells. Taken together, these results confirmed that NRT cells have increased specific cytokine secretion capacity compared with conventional T cells. The increasing number of NRT cells in ACT product combined with the strengthened cell effector function indicated an enhancing antitumor activity.
Assessment of cytokine production and immune response in T cells and neoantigen-reactive T (NRT) cells. T cells were acquired after rapid expansion protocol (REP). Flow cytometry for the analysis of a interferon (IFN)-γ-producing cells; b TNF-α-producing cells; and c Granzyme B-producing cells; d T cells were co-cultured with Lewis cells overnight; supernatant was collected to determine the IFN-γ and TNF-α levels by ELISA
Antitumor Effect of NRT‐ACT in combination with a PD‐1 Inhibitor in vivo
Recent studies have shown that NSCLC has a high mutation rate and susceptibility toward PD1/PDL-1 inhibitors. We demonstrated that NRT-ACT exerts a strong antitumor effect in our previous study (Sun et al. 2021; Lawrence et al. 2013; Reck et al. 2016). To further investigate the antitumor effect of NRT-ACT combined with PD1 inhibitors, we designed the treatment experiments for NSCLC in the mouse model (Fig. 4a). As shown in Fig. 4b and c, the single NRT-ACT or PD1 inhibitor therapy was associated with a similar trend of preventing tumor growth, whereas the combination strategy significantly attenuated tumor growth.
Antitumor effect of neoantigen-reactive T-adoptive cell therapy (NRT‐ACT) in vivo. a Flow graph for the in vivo experiment. b and c Tumor growth curves and weight of tumor-bearing mice after ACT; the number of experimental mice (n) = 5. d and e The differential distribution of immune cells in tumor tissues after ACT (the analysis was started with 10,000 live cells in three replicates)
Next, we detected the distribution of the immune cell population in the tumor tissues by flow cytometry. More leukocytes (CD45 +) and T cells (CD3 + , CD4 + , and CD8 +) infiltrating into the tumor tissue were present in the NRT and anti-PD1 groups than in the conventional T-cell group (Figs. 4d–e, 5a). More TILs in the tumor site are positively correlated with stronger T-cell response and better patient prognosis (Rooney et al. 2015; Howitt et al. 2015). Moreover, an increased number of T cells in both the single NRT group and the NRT combination group indicated that the NRT cells could infiltrate into the tumor microenvironment (TME) or stimulate the endogenous immune response (Fig. 5a), thus enhancing antitumor effects. CD137 (4‐1BB), which is usually expressed on activated T cells, was used to identify and isolate tumor-specific T cells from TILs. Similarly, the clinical effects of ACT rely on the presence of tumor‐specific T lymphocytes (Seliktar-Ofir et al. 2017; Krishna et al. 2020; Wolfl et al. 2007). To determine the tumor‐specific T lymphocytes in the TME after NRT-ACT, we examined the CD3 + CD137 + T-cell populations by flow cytometry and performed the immunofluorescence analysis of the tumor tissue. As expected, NRT-ACT increased CD3 + CD137 + T-cell infiltration, and the combination with anti-PD1 also augmented the number of CD3 + CD137 + T cells (Fig. 5b-d). Our experiments showed that the NRT-ACT combination with anti-PD1 significantly increased TIL infiltration, especially the tumor-specific T cells, preventing tumor progression.
The differential distribution of immune cells in tumor tissues after adoptive cell therapy (ACT). a CD4 (red) and CD8 (green) levels in tumors; b CD3 and CD137 levels in tumors. Representative images of CD3 (red) and CD137 (green) immunostaining and DAPI nuclear staining (blue) of tumors after ACT, as indicated; scale bar = 50 mm; c CD137 levels in intra-tumoral T cells after ACT as determined by flow cytometry (Started the analysis from CD3 + T cells and performed three independent experiments); d Statistical chart of differences; e Differential levels of the inhibitory marker programmed cell death protein 1 in intra-tumoral T cells after ACT (Started the analysis from CD3 + T cells and performed three independent experiments); f Statistical chart of differences
Similar to the challenges faced by TIL-ACT in solid tumors, the durable survival and maintaining the killing ability of T cells in the immunosuppressive TME should be addressed. It is also known as T-cell exhaustion, which is defined by poor cytokine secretion and function, sustained expression of inhibitory receptors (such as PD1) that desensitizes TCR signaling, and a state distinct from that of functional effector or memory T cells (Blank et al. 2019; Baitsch et al. 2012). To explore the state of T cells after NRT-ACT, we detected the level of inhibitory marker PD‐1 in TILs (CD3 + PD1 + T cells). As shown in Fig. 5e-f, a significant decrease in the level from 47.23% in the NRT group to 32.90% in the NRT plus anti-PD1 group was observed. A certain degree of decrease was observed in the T plus anti-PD1 group than in the T-cell group. Meanwhile, our experiment also demonstrated similar PD1 expression on conventional and NRT cells (Figure S2a-b).These results suggest that anti-PD1 may revitalize exhausted T cells and enhance the response to cancer immunotherapy. Furthermore, the anti-PD1 plus NRT-ACT combination may induce endogenous immune cells and their differentiation into pleiotropic immune effectors or memory cells.
It has been reported that the transfusion of T cells with a long-lived and self-renewing memory phenotype in B16 melanoma tumors and B-cell malignancies exerts augmented and continuous antitumor effects (Chen et al. 2021; Klebanoff et al. 2011). We evaluated levels of CD45RA and CD62L in T cells in peripheral blood mononuclear cells after ACT in all four cohorts to characterize different immune biomarkers outside the TME. The two NRT cell groups had a higher percentage of peripheral effector memory CD3 + T(CD45RA−CD62L−) cells than the two T-cell groups (Figure S3a-c), suggesting that these adoptively infused memory T cells were persistent in the circulating blood. Moreover, the two anti-PD1 groups showed more effector T (CD45RA+CD62L−) cells than the single T and NRT groups, indicating the increased number of effector cells after ICI treatment (Figure S3c). The changes in the immune cell phenotype in the TME and peripheral blood and the enhanced cytotoxicity of T cells may be the mechanism for preventing tumor progression.
Current studies mainly focus on engineering T cells for the ACT; however, a heterogeneous population of tumor-associated fibroblasts, Treg cells, and TAMs infiltrated in the TME are supposed to increase drug resistance and promote tumor progression (Mantovani et al. 2017; Togashi et al. 2019; Martínez-Reyes and Chandel 2021; Mantovani et al. 2022). To determine the effect of ACT on the TME, Treg cells and TAMs were detected by flow cytometry. As shown in Figure S4a-d, no significant difference was observed in the TAM cell and Treg populations in the four cohorts, suggesting that immunosuppressive cells in the TME may not affect the antitumor efficacy of ACT and ICI therapy. Given the different CD45 + cell numbers shown in Fig. 4c, we speculate that other cell subsets such as DCs, neutrophils, or B cells in the TME may show varying degrees of increase in the NRT + anti-PD1 treatment group.
Finally, toxicity studies were performed to assess immune-related adverse events in the lung, intestine, liver, and kidney after treatment. Figure S5a–c shows no significant differences in alanine aminotransferase, aspartate aminotransferase, blood urea nitrogen, and creatinine among the four groups, suggesting low toxicity in the liver and renal function. Figure S3d also shows no significant morphological changes in the histopathological results of the lung and intestine.
Taken together, we confirm that the combination of NRT‐ACT and anti-PD1 can induce antitumor effects against lung cancer, and this novel immunotherapy strategy is safe and feasible.
Discussion
Immunotherapy based on TIL-ACT has been reported to trigger tumor regression in patients with metastatic melanoma and metastatic cholangiocarcinoma as reported by Rosenberg et al. (Dudley et al. 2002; Tran et al. 2014). Moreover, clinical studies on lung cancer treatment are also underway at present (NCT02621021, NCT04614103, and NCT03645928). Even in the most mature CAR-T therapy, about 7% of patients in initial clinical trials died while waiting for the production of CAR-T cells (with a median time from enrollment to infusion of 45 days in the ELIANA trial) (Amini et al. 2022; Maude et al. 2018). Waiting nearly 2 months to prepare T-cell products for patients with advanced malignancy who have limited survival time. Therefore, it is very important and urgent to reduce the time of T-cell preparation and bridging therapies. In this context, we designed the NRT experiment for simplifying the process and improving the efficacy of ACT in solid tumors. There are four main advantages of NRT cells whose production is induced by our neoantigen-RNA vaccine: ① NRT cells induced by the RNA vaccine are tumor-specific and do not attack normal tissues (Lang et al. 2022), ② Patients with advanced cancers cannot tolerate surgery that is required to obtain sufficient tumor tissues for isolating TILs because of the tumor location or deteriorating physical condition. However, obtaining gene sequencing data from only a very small number of tumor cells isolated from puncture, endoscopic specimens, or superficial metastatic lymph node samples is convenient, ③ Since the onset of the COVID-19 pandemic, several countries have stepped up their efforts on vaccine research and development. RNA vaccines based on neoantigens can be produced quickly by relying on mature and advanced vaccine preparation technologies, thus saving the waiting time of patients, ④Unlike DNA vaccines, RNA vaccines do not integrate into the host’s genome, thereby significantly reducing the latent risk of biogenetics. After a series of processes from gene sequencing to NRT preparation, our experiments showed that the proportion of CD3 + CD137 + T cells increased considerably and the secretion of IFN-γ and TNF-α was enhanced significantly, indicating the augmentation of NRT cells’ antitumor ability. Importantly, qualified NRT products can be manufactured within 3–4 weeks using this procedure, which considerably reduces the clinical waiting time.
CAR-T therapy has revolutionized the field of cancer therapeutics because of its inspiring efficacy against relapsed or refractory B-cell malignancies and has been approved by the FDA (Heymach et al. 2018). However, its success against solid tumors is questionable. Although our NRT cells can partly solve the problem of T-cell-specific recognition, similar to CAR-T therapy, the TIL-ACT treatment still faces other impediments such as infiltration, killing, and prolonged survival in the immunosuppressive TME (Martinez and Moon 2019; Anderson et al. 2017; Krenciute et al. 2017; Zabel et al. 2019; Drent et al. 2019; Eyquem et al. 2017). Furthermore, merely focusing on delivering the T cells to the tumor site and their subsequent performance is insufficient. Tumors also induce the secretion of immunosuppressive cytokines such as vascular endothelial growth factor (VEGF), interleukin-10 (IL-10), and transforming growth factor-β (TGF-β), which recruit regulatory T (Treg cells) and myeloid-derived suppressor cells (MDSCs) and then actively mediate tolerance. These immunosuppressive cytokines and the environment can hinder protective immunosurveillance and hamper effective antitumor immune responses because of tumor angiogenesis, immune escape, inhibiting the presentation of APC, and impairing the function of tumor-specific CD8 + T cells and CD4 + T helper cells, thus promoting tumor progression eventually (Mirzaei et al. 1850; Li et al. 2020). Previous studies have reported that non-myeloablative chemotherapy remarkably prolongs the in vivo persistence of transferred T cells after ACT. In addition, a significant increase in the concentration of CD8 + T cells as well as that of IL-7 and IL-15 in the peripheral blood samples of patients was detected. Both cytokines are involved in maintaining the homeostasis of T cells and promoting the expansion of transferred T cells (Dudley et al. 2002, 2008). Meanwhile, lymphodepletion can enhance the efficacy of TILs by eliminating MDSC and Treg cells in the TME. Therefore, in the present study, we used CTX in the non-myeloablative regime along with IL-2, which not only provided a suitable environment for the survival of NRT cells but also promoted the proliferation and survival of NRT cells in vivo. Our experiments confirmed that the use of NRT-ACT and the PD1 inhibitor for monotherapy yielded comparable results. In addition, radiotherapy has been reported to be an immunogenic tumor reduction strategy that can be used to kill tumor cells at the primary or metastatic site, upregulate the expression of neoantigens, or manipulate the TME (Schoenfeld et al. 2022; Lhuillier et al. 2021). Therefore, in our next study, we aim to stimulate endogenous antitumor immunity by radiation before NRT infusion to create a suitable environment for NRT cells.
To date, ICIs such as including PD1/PD-L1 inhibitors and CLTA-4 blockade are the most widely studied and clinically administered immunotherapies. PD1/PD-L1 inhibitors have recently become the cornerstone of first-line therapy for treating gene-negative patients of advanced NSCLC (Grant et al. 2021). Although the actual mechanism of action and the therapeutic potential of ICIs remain undefined, limited clinical data suggest that the frequency of somatic mutations or the production of tumor neoantigens within a tumor type is positively correlated with the clinical response to ICIs (Yarchoan et al. 2017). NSCLC exhibits a high mutation load and is susceptible to PD1/PDL-1 inhibitors, making it an ideal candidate for NRT-ACT combined with ICIs (Lawrence et al. 2013; Reck et al. 2016). Although ICIs have yielded encouraging results in both research and clinical trials and the presence of numerous TILs has become a positive prognostic marker in multiple solid tumors, the efficacy of a single PD‐1 agent against metastatic cancer is not satisfactory (Fridman et al. 2012). One reason for this failure of cancer elimination is the deterioration of T-cell function signified by decreased effector cytokine production, impaired cytotoxicity, and overexpression of inhibitory receptors (PD1 + T cells) along with the corresponding upregulation of PD-L1/PD-L2 in tumor cells (Zou et al. 2016). T-cell exhaustion was primarily identified from chronic viral infection and then a similar phenomenon was observed in the case of cancers in humans induced by exposure to persistent antigens and inflammatory signals in the TME. Previous studies have demonstrated that PD‐1/PD‐L1 inhibitors can reverse the exhaustion of CD8 + T cells and restimulate the helper activity of tumor-specific CD4 + T cells, and thus, restore antitumor T‐cell immunity (Pauken and Wherry 2015; Balança et al. 2021). Another report also reported that PD1 inhibitors mediated the reinvigoration/proliferation of circulating memory T cells and exhausted T cells at the tumor site (Balança et al. 2020). To enhance the killing function and survival ability as well as revitalize the exhausted state of NRT cells in the TME, we demonstrated that the combination of NRT‐ACT and the PD‐1 inhibitor can exert a strong antitumor effect, which was confirmed by the presence of more T cells and tumor-specific T cells (CD3 + CD137 + T) infiltrating the tumor tissue. Additionally, the expression of PD‐1 was downregulated after the therapy, suggesting that the PD‐1 inhibitor may reverse the exhausted state of T cells, although some studies have reported that distinct subsets of exhausted CD8 + T cells exhibited different potentials for recovery after inhibiting the PD1 pathway. For example, exhausted CD8 + T cells with intermediate expression of PD1 (PD1int) can be reinvigorated by anti-PD1,however, those with a high expression of PD1 (PD1hi) cannot (Blackburn et al. 2008). Furthermore, changes in the immune cell phenotype and their proportions in the peripheral blood and TME suggested that the combination regimen may induce endogenous immune cells and their differentiation into pleiotropic immune effector cells. Our innovative proposal is an inspiring strategy for NSCLC and has the potential to extend to ACT therapy for other solid tumors.
Similar to our previous study about NRT-ACT (Sun et al. 2021), the present study has certain limitations. Although our experiments confirmed the strengthened antitumor effect using the combined strategy and downregulation of the expression of the exhausted marker PD1, whether revitalization was caused by NRT or conventional T cells is unclear. Further studies are required to solve the problems of tumor-specific T cells homing and overcoming the immunosuppressive TME in solid tumors.
In conclusion, current immunotherapies are not effective in all patients but researchers are doing their best to develop novel treatments that benefit more people. However, monotherapy may not be effective for patients with advanced cancers. In the present study, we demonstrated that the combination of NRT‐ACT and anti-PD1 can elicit a strong antitumor response against lung cancer. Furthermore, this combination strategy may serve as a reference for ACT therapy against other solid tumors.
Availability of data and materials
The data presented in this study are available in the article or supplementary files.
Code availability
Not applicable.
References
Amini L, Silbert SK, Maude SL, Nastoupil LJ, Ramos CA, Brentjens RJ, Sauter CS, Shah NN, Abou-El-Enein M (2022) Preparing for CAR T cell therapy: patient selection, bridging therapies and lymphodepletion. Nat Rev Clin Oncol 19(5):342–355
Anderson KG, Stromnes IM, Greenberg PD (2017) Obstacles posed by the tumor microenvironment to T cell activity: a case for synergistic therapies. Cancer Cell 31(3):311–325
Bagchi S, Yuan R, Engleman EG (2021) Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Annu Rev Pathol 16:223–249
Baitsch L, Fuertes-Marraco SA, Legat A, Meyer C, Speiser DE (2012) The three main stumbling blocks for anticancer T cells. Trends Immunol 33(7):364–372
Balança CC, Scarlata CM, Michelas M, Devaud C, Sarradin V, Franchet C, Martinez Gomez C, Gomez-Roca C, Tosolini M, Heaugwane D et al (2020) Dual relief of T-lymphocyte proliferation and effector function underlies response to PD-1 blockade in epithelial malignancies. Cancer Immunol Res 8(7):869–882
Balança CC, Salvioni A, Scarlata CM, Michelas M, Martinez-Gomez C, Gomez-Roca C, Sarradin V, Tosolini M, Valle C, Pont F et al (2021) PD-1 blockade restores helper activity of tumor-infiltrating, exhausted PD-1hiCD39+ CD4 T cells. JCI Insight 6(2):e142513
Bjerregaard AM, Nielsen M, Hadrup SR, Szallasi Z, Eklund AC (2017) MuPeXI: prediction of neo-epitopes from tumor sequencing data. Cancer Immunol Immunother CII 66(9):1123–1130
Blackburn SD, Shin H, Freeman GJ, Wherry EJ (2008) Selective expansion of a subset of exhausted CD8 T cells by alphaPD-L1 blockade. Proc Natl Acad Sci USA 105(39):15016–15021
Blank CU, Haining WN, Held W, Hogan PG, Kallies A, Lugli E, Lynn RC, Philip M, Rao A, Restifo NP et al (2019) Defining “T cell exhaustion.” Nat Rev Immunol 19(11):665–674
Castle JC, Kreiter S, Diekmann J, Löwer M, van de Roemer N, de Graaf J, Selmi A, Diken M, Boegel S, Paret C et al (2012) Exploiting the mutanome for tumor vaccination. Cancer Res 72(5):1081–1091
Chen F, Zou Z, Du J, Su S, Shao J, Meng F, Yang J, Xu Q, Ding N, Yang Y et al (2019) Neoantigen identification strategies enable personalized immunotherapy in refractory solid tumors. J Clin Investig 129(5):2056–2070
Chen GM, Chen C, Das RK, Gao P, Chen CH, Bandyopadhyay S, Ding YY, Uzun Y, Yu W, Zhu Q et al (2021) Integrative bulk and single-cell profiling of premanufacture T-cell populations reveals factors mediating long-term persistence of CAR T-cell therapy. Cancer Discov 11(9):2186–2199
Creelan BC, Wang C, Teer JK, Toloza EM, Yao J, Kim S, Landin AM, Mullinax JE, Saller JJ, Saltos AN et al (2021) Tumor-infiltrating lymphocyte treatment for anti-PD-1-resistant metastatic lung cancer: a phase 1 trial. Nat Med 27(8):1410–1418
Cullen SP, Brunet M, Martin SJ (2010) Granzymes in cancer and immunity. Cell Death Differ 17(4):616–623
De Plaen E, Lurquin C, Van Pel A, Mariamé B, Szikora JP, Wölfel T, Sibille C, Chomez P, Boon T (1988) Immunogenic (tum-) variants of mouse tumor P815: cloning of the gene of tum- antigen P91A and identification of the tum- mutation. Proc Natl Acad Sci USA 85(7):2274–2278
Ding Z, Li Q, Zhang R, Xie L, Shu Y, Gao S, Wang P, Su X, Qin Y, Wang Y et al (2021) Personalized neoantigen pulsed dendritic cell vaccine for advanced lung cancer. Signal Transduct Target Ther 6(1):26
Drent E, Poels R, Ruiter R, van de Donk N, Zweegman S, Yuan H, de Bruijn J, Sadelain M, Lokhorst HM, Groen RWJ et al (2019) Combined CD28 and 4–1BB costimulation potentiates affinity-tuned chimeric antigen receptor-engineered T cells. Clin Cancer Res 25(13):4014–4025
Dudley ME, Wunderlich JR, Robbins PF, Yang JC, Hwu P, Schwartzentruber DJ, Topalian SL, Sherry R, Restifo NP, Hubicki AM et al (2002) Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science 298(5594):850–854
Dudley ME, Yang JC, Sherry R, Hughes MS, Royal R, Kammula U, Robbins PF, Huang J, Citrin DE, Leitman SF et al (2008) Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. J Clin Oncol 26(32):5233–5239
Eyquem J, Mansilla-Soto J, Giavridis T, van der Stegen SJ, Hamieh M, Cunanan KM, Odak A, Gönen M, Sadelain M (2017) Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature 543(7643):113–117
Farhood B, Najafi M, Mortezaee K (2019) CD8(+) cytotoxic T lymphocytes in cancer immunotherapy: a review. J Cell Physiol 234(6):8509–8521
Fridman WH, Pagès F, Sautès-Fridman C, Galon J (2012) The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer 12(4):298–306
Friese C, Harbst K, Borch TH, Westergaard MCW, Pedersen M, Kverneland A, Jönsson G, Donia M, Svane IM, Met Ö (2020) CTLA-4 blockade boosts the expansion of tumor-reactive CD8(+) tumor-infiltrating lymphocytes in ovarian cancer. Sci Rep 10(1):3914
Goodman AM, Kato S, Bazhenova L, Patel SP, Frampton GM, Miller V, Stephens PJ, Daniels GA, Kurzrock R (2017) Tumor mutational burden as an independent predictor of response to immunotherapy in diverse cancers. Mol Cancer Ther 16(11):2598–2608
Grant MJ, Herbst RS, Goldberg SB (2021) Selecting the optimal immunotherapy regimen in driver-negative metastatic NSCLC. Nat Rev Clin Oncol 18(10):625–644
Gross L (1943) Intradermal immunization of C3H mice against a sarcoma that originated in an animal of the same line. Can Res 3(5):326–333
Heather JM, Chain B (2016) The sequence of sequencers: The history of sequencing DNA. Genomics 107(1):1–8
Helft J, Böttcher J, Chakravarty P, Zelenay S, Huotari J, Schraml BU, Goubau D (2015) Reis e sousa C: GM-CSF mouse bone marrow cultures comprise a heterogeneous population of CD11c(+)MHCII(+) macrophages and dendritic cells. Immunity 42(6):1197–1211
Hellmann MD, Callahan MK, Awad MM, Calvo E, Ascierto PA, Atmaca A, Rizvi NA, Hirsch FR, Selvaggi G, Szustakowski JD et al (2018) Tumor mutational burden and efficacy of nivolumab monotherapy and in combination with ipilimumab in small-cell lung cancer. Cancer Cell 33(5):853-861.e854
Heymach J, Krilov L, Alberg A, Baxter N, Chang SM, Corcoran RB, Dale W, DeMichele A, Magid Diefenbach CS, Dreicer R et al (2018) Clinical cancer advances 2018: annual report on progress against cancer from the American society of clinical oncology. J Clin Oncol 36(10):1020–1044
Ho PC, Bihuniak JD, Macintyre AN, Staron M, Liu X, Amezquita R, Tsui YC, Cui G, Micevic G, Perales JC et al (2015) Phosphoenolpyruvate is a metabolic checkpoint of anti-tumor T cell responses. Cell 162(6):1217–1228
Howitt BE, Shukla SA, Sholl LM, Ritterhouse LL, Watkins JC, Rodig S, Stover E, Strickland KC, D’Andrea AD, Wu CJ et al (2015) Association of polymerase e-mutated and microsatellite-instable endometrial cancers with neoantigen load, number of tumor-infiltrating lymphocytes, and expression of PD-1 and PD-L1. JAMA Oncol 1(9):1319–1323
Jiang T, Shi T, Zhang H, Hu J, Song Y, Wei J, Ren S, Zhou C (2019) Tumor neoantigens: from basic research to clinical applications. J Hematol Oncol 12(1):93
Kim B, Won D, Jang M, Kim H, Choi JR, Kim TI, Lee ST (2019) Next-generation sequencing with comprehensive bioinformatics analysis facilitates somatic mosaic APC gene mutation detection in patients with familial adenomatous polyposis. BMC Med Genom 12(1):103
Klebanoff CA, Gattinoni L, Palmer DC, Muranski P, Ji Y, Hinrichs CS, Borman ZA, Kerkar SP, Scott CD, Finkelstein SE et al (2011) Determinants of successful CD8+ T-cell adoptive immunotherapy for large established tumors in mice. Clin Cancer Res 17(16):5343–5352
Kochenderfer JN, Wilson WH, Janik JE, Dudley ME, Stetler-Stevenson M, Feldman SA, Maric I, Raffeld M, Nathan DA, Lanier BJ et al (2010) Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood 116(20):4099–4102
Krenciute G, Prinzing BL, Yi Z, Wu MF, Liu H, Dotti G, Balyasnikova IV, Gottschalk S (2017) Transgenic expression of IL15 Improves antiglioma activity of IL13Rα2-CAR T cells but results in antigen loss variants. Cancer Immunol Res 5(7):571–581
Krishna S, Lowery FJ, Copeland AR, Bahadiroglu E, Mukherjee R, Jia L, Anibal JT, Sachs A, Adebola SO, Gurusamy D et al (2020) Stem-like CD8 T cells mediate response of adoptive cell immunotherapy against human cancer. Science 370(6522):1328–1334
Lang F, Schrörs B, Löwer M, Türeci Ö, Sahin U (2022) Identification of neoantigens for individualized therapeutic cancer vaccines. Nat Rev Drug Discov 21(4):261–282
Lauss M, Donia M, Harbst K, Andersen R, Mitra S, Rosengren F, Salim M, Vallon-Christersson J, Törngren T, Kvist A et al (2017) Mutational and putative neoantigen load predict clinical benefit of adoptive T cell therapy in melanoma. Nat Commun 8(1):1738
Lawrence MS, Stojanov P, Polak P, Kryukov GV, Cibulskis K, Sivachenko A, Carter SL, Stewart C, Mermel CH, Roberts SA et al (2013) Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499(7457):214–218
Lhuillier C, Rudqvist NP, Yamazaki T, Zhang T, Charpentier M, Galluzzi L, Dephoure N, Clement CC, Santambrogio L, Zhou XK et al (2021) Radiotherapy-exposed CD8+ and CD4+ neoantigens enhance tumor control. J Clin Investig 131(5):e138740
Li L, Goedegebuure SP, Gillanders WE (2017) Preclinical and clinical development of neoantigen vaccines. Anna Oncol 28(12):xii11–xii17
Li C, Jiang P, Wei S, Xu X, Wang J (2020) Regulatory T cells in tumor microenvironment: new mechanisms, potential therapeutic strategies and future prospects. Mol Cancer 19(1):116
Mantovani A, Marchesi F, Malesci A, Laghi L, Allavena P (2017) Tumour-associated macrophages as treatment targets in oncology. Nat Rev Clin Oncol 14(7):399–416
Mantovani A, Allavena P, Marchesi F, Garlanda C (2022) Macrophages as tools and targets in cancer therapy. Nat Revi Drug Discov. 1–22.
Martinez M, Moon EK (2019) CAR T cells for solid tumors: new strategies for finding, infiltrating, and surviving in the tumor microenvironment. Front Immunol 10:128
Martínez-Reyes I, Chandel NS (2021) Cancer metabolism: looking forward. Nat Rev Cancer 21(10):669–680
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, Bader P, Verneris MR, Stefanski HE, Myers GD et al (2018) Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med 378(5):439–448
Mirzaei HR, Rodriguez A, Shepphird J, Brown CE, Badie B (1850) Chimeric antigen receptors T cell therapy in solid tumor: challenges and clinical applications. Front Immunol 2017:8
Morgan RA, Dudley ME, Wunderlich JR, Hughes MS, Yang JC, Sherry RM, Royal RE, Topalian SL, Kammula US, Restifo NP et al (2006) Cancer regression in patients after transfer of genetically engineered lymphocytes. Science 314(5796):126–129
Ott PA, Hu-Lieskovan S, Chmielowski B, Govindan R, Naing A, Bhardwaj N, Margolin K, Awad MM, Hellmann MD, Lin JJ et al (2020) A phase Ib trial of personalized neoantigen therapy plus anti-PD-1 in patients with advanced melanoma, non-small cell lung cancer, or bladder cancer. Cell 183(2):347-362.e324
Pardoll DM (2012) The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer 12(4):252–264
Pauken KE, Wherry EJ (2015) Overcoming T cell exhaustion in infection and cancer. Trends Immunol 36(4):265–276
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe S et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375:1823–1833 (1533-4406 (Electronic))
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe S et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375(19):1823–1833
Reina-Campos M, Scharping NE, Goldrath AW (2021) CD8(+) T cell metabolism in infection and cancer. Nat Rev Immunol 21(11):718–738
Restifo NP, Dudley ME, Rosenberg SA (2012) Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol 12(4):269–281
Roney K (2019) Bone marrow-derived dendritic cells. Methods Mol Biol 1960:57–62
Rooney MS, Shukla SA, Wu CJ, Getz G, Hacohen N (2015) Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 160(1–2):48–61
Sahin U, Derhovanessian E, Miller M, Kloke BP, Simon P, Löwer M, Bukur V, Tadmor AD, Luxemburger U, Schrörs B et al (2017) Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer. Nature 547(7662):222–226
Schoenfeld JD, Giobbie-Hurder A, Ranasinghe S, Kao KZ, Lako A, Tsuji J, Liu Y, Brennick RC, Gentzler RD, Lee C et al (2022) Durvalumab plus tremelimumab alone or in combination with low-dose or hypofractionated radiotherapy in metastatic non-small-cell lung cancer refractory to previous PD(L)-1 therapy: an open-label, multicentre, randomised, phase 2 trial. Lancet Oncol 23(2):279–291
Schumacher TN, Schreiber RD (2015) Neoantigens in cancer immunotherapy. Science 348(6230):69–74
Seliktar-Ofir S, Merhavi-Shoham E, Itzhaki O, Yunger S, Markel G, Schachter J, Besser MJ (2017) Selection of shared and neoantigen-reactive T cells for adoptive cell therapy based on CD137 separation. Front Immunol 8:1211
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer Statistics. CA Cancer J Clin 71(1):7–33
Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, Dechaphunkul A, Imamura F, Nogami N, Kurata T et al (2018) Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 378(2):113–125 (1533-4406 (Electronic))
Sun J, Zhang J, Hu H, Qin H, Liao X, Wang F, Zhang W, Yin Q, Su X, He Y et al (2021) Anti-tumour effect of neo-antigen-reactive T cells induced by RNA mutanome vaccine in mouse lung cancer. J Cancer Res Clin Oncol 147(11):3255–3268
Thommen DS, Schumacher TN (2018) T cell dysfunction in Cancer. Cancer Cell 33(4):547–562
Thompson JA (2018) New NCCN guidelines: recognition and management of immunotherapy-related toxicity. J Natl Compr Cancer Netw JNCCN 16(5s):594–596
Togashi Y, Shitara K, Nishikawa H (2019) Regulatory T cells in cancer immunosuppression—implications for anticancer therapy. Nat Rev Clin Oncol 16(6):356–371
Tran E, Turcotte S, Gros A, Robbins PF, Lu YC, Dudley ME, Wunderlich JR, Somerville RP, Hogan K, Hinrichs CS et al (2014) Cancer immunotherapy based on mutation-specific CD4+ T cells in a patient with epithelial cancer. Science 344(6184):641–645
Tran E, Robbins PF, Lu YC, Prickett TD, Gartner JJ, Jia L, Pasetto A, Zheng Z, Ray S, Groh EM et al (2016) T-cell transfer therapy targeting mutant KRAS in cancer. N Engl J Med 375(23):2255–2262
Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA Jr, Kinzler KW (2013) Cancer genome landscapes. Science 339(6127):1546–1558
Vredevoogd DW, Kuilman T, Ligtenberg MA, Boshuizen J, Stecker KE, de Bruijn B, Krijgsman O, Huang X, Kenski JCN, Lacroix R et al (2019) Augmenting immunotherapy impact by lowering tumor TNF cytotoxicity threshold. Cell 178(3):585-599.e515
Ward JP, Gubin MM, Schreiber RD (2016) The role of neoantigens in naturally occurring and therapeutically induced immune responses to cancer. Adv Immunol 130:25–74
Wölfel T, Hauer M, Schneider J, Serrano M, Wölfel C, Klehmann-Hieb E, De Plaen E, Hankeln T (1995) Meyer zum Büschenfelde KH, Beach D: A p16INK4a-insensitive CDK4 mutant targeted by cytolytic T lymphocytes in a human melanoma. Science 269(5228):1281–1284
Wolfl M, Kuball J, Ho WY, Nguyen H, Manley TJ, Bleakley M, Greenberg PD (2007) Activation-induced expression of CD137 permits detection, isolation, and expansion of the full repertoire of CD8+ T cells responding to antigen without requiring knowledge of epitope specificities. Blood 110(1):201–210
Yarchoan M, Johnson BA 3rd, Lutz ER, Laheru DA, Jaffee EM (2017) Targeting neoantigens to augment antitumour immunity. Nat Rev Cancer 17(4):209–222
Zabel M, Tauber PA, Pickl WF (2019) The making and function of CAR cells. Immunol Lett 212:53–69
Zacharakis N, Chinnasamy H, Black M, Xu H, Lu YC, Zheng Z, Pasetto A, Langhan M, Shelton T, Prickett T et al (2018) Immune recognition of somatic mutations leading to complete durable regression in metastatic breast cancer. Nat Med 24(6):724–730
Zheng R, Zhang S, Zeng H, Wang S, Sun K, Chen R, Li L, Wei W, He J (2022) Cancer incidence and mortality in China, 2016. J Natll Cancer Center. 2(1):1–9
Zou W, Wolchok JD, Chen L (2016) PD-L1 (B7–H1) and PD-1 pathway blockade for cancer therapy: mechanisms, response biomarkers, and combinations. Sci Transl Med 8(328):328324
Acknowledgements
We appreciate the help of neoantigen screening and data analysis by the P&PMed Biotechnology Co. Ltd. (Shanghai, China. http://www.pnp-med.com/).
Funding
This research was funded by Shanghai Science and Technology Committee Scientific Research Project (Grant number 19411950400) for Qiang Li, Youth Scientific Research Foundation of Affiliated Hospital of Qingdao University (Grant Number: QDFYQN202101014) for Haiyan Hu and Health & Medicine and Scientific Technology Development Program of Shandong Province (Grant Number: 202203020560) for Jiaxing Sun.
Author information
Authors and Affiliations
Contributions
QL, XS and JS: designed the study. JS, HQ and HH: conducted experiments and analyzed data. HQ and XL: performed and analyzed the histomorphology. PZ and WH: performed data curation. JS and HQ: wrote the paper with input from all authors. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical approval
This study was conducted with the approval of the Ethics Committee of Tongji University (TJBB03721106). All experimental methods and clinical treatment were carried out in accordance with the approved guidelines.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
432_2023_4683_MOESM1_ESM.tif
Supplementary Supplementary Figure 1. Different cytokine production and immune response assessment in T Cells and neoantigen-reactive T (NRT) cells. file1 (TIF 1449 KB)
432_2023_4683_MOESM2_ESM.tif
Supplementary Supplementary Figure 2. Different expression of the inhibitory marker programmed cell death protein 1 on T and NRT cells after REP file2 (TIF 1386 KB)
432_2023_4683_MOESM3_ESM.tif
Supplementary Supplementary Figure 3. Differential levels of effector T cells in peripheral blood mononuclear cells (PBMCs) after adoptive cell therapy. file3 (TIF 1564 KB)
432_2023_4683_MOESM4_ESM.tif
Supplementary Supplementary Figure 4. Different amounts of immunosuppressive cells in tumor tissues after adoptive cell therapy (ACT). file4 (TIF 2451 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, H., Hu, H., Liao, X. et al. Antitumor effect of neoantigen-reactive T cells combined with PD1 inhibitor therapy in mouse lung cancer. J Cancer Res Clin Oncol 149, 7363–7378 (2023). https://doi.org/10.1007/s00432-023-04683-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-023-04683-5