Abstract
Background
Lynch-like syndrome (LLS) tumors have similar clinicopathological features to Lynch syndrome (LS) tumors but have no identifiable pathogenic germline mismatch repair gene variant. However, cancer risks in LLS patients and first-degree relatives (FDRs) are not well defined.
Methods
To clarify LLS-associated cancer risks, a systematic review of all studies examining all cancer risks in LLS was performed. Searching of Medline, Embase, Pubmed, Cochrane and CINAHL databases and reference/citation checking identified relevant studies published between January 1, 1980 and February 11, 2021. Joanna Briggs Institute Appraisal Tools assessed the risk of bias.
Results
Six studies (five cohort/one cross-sectional) were eligible for study inclusion. One study found no difference in colorectal cancer (CRC) incidence between LLS and LS patients or CRC risks at aged 70 years. Three studies found CRC incidence in LLS FDRs was higher than the general population but lower than LS FDRs. Two studies showed no difference in CRC diagnosis age between LLS patients and LS patients. Endometrial cancer risks in LLS patients were higher than the general population but lower than LS patients.
Conclusion
Evidence of elevated CRC risks in LLS patients and FDRs supports increased colonoscopy surveillance strategies for LLS patients and FDRs in line with current recommendations for LS. Due to heterogeneity amongst LLS populations, extended intervals between screening may be advised for low-risk families. Studies to resolve the molecular characterization and definition of LLS are needed to clarify cancer risks associated with LLS which in turn may individualize surveillance strategies for LLS patients and families.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lynch syndrome (LS) is an autosomal-dominant inherited syndrome accounting for 2–4% of colorectal and endometrial cancers (Hampel et al. 2006, 2008; Umar et al. 2004). LS is characterized by germline pathogenic variants in one of the DNA mismatch repair (MMR) genes, MSH2, MLH1, MSH6 and PMS2 or large deletions in EPCAM, causing transition read through hypermethylation of MSH2 gene promoter (Carethers 2014). Inactivation of MMR genes via a germline pathogenic variant and an acquired somatic mutation (second hit) results in the accumulation of mutations in regions of repetitive DNA during cell replication. This tumorigenesis mechanism leads to tumors with microsatellite instability (MSI), with accompanying loss of MMR protein and high numbers of somatic mutations (hypermutation), collectively referred to as MMR deficiency (Cancer Genome Atlas 2012; Lynch et al. 2015; Rodriguez-Soler et al. 2013).
In addition to LS, there are sporadic causes of tumor MMR deficiency. MLH1 promoter hypermethylation is the most common cause of MMR deficiency in colorectal cancer (CRC) and endometrial cancer, as characterized by loss of tumor MLH1 and PMS2 protein expression. Distinguishing between MLH1 methylation and LS-related MMR deficiency is clinically important for secondary cancer risk management and for identifying relatives at risk of cancer.
Lynch-like syndrome (LLS) tumors are considered mimics of LS tumors, also demonstrating MSI, loss of MMR protein expression, and absence of MLH1 methylation (Carethers 2014; Hampel et al. 2006). However, in LLS, there is an absence of a germline pathogenic variant in one of the MMR genes or a somatic BRAF V600E mutation (in the absence of MLH1 methylation) (Carethers 2014; Hampel et al. 2006). LLS tumors constitute up to 70% of patients with MSI and MMR deficiency suspected of having LS.(Carethers & Stoffel 2015; Rodriguez-Soler et al. 2013) The prevalence of CRC cases with LLS in population-based studies was estimated to be 2.5% in Spain (Rodriguez-Soler et al. 2013), and 6% in collective data from the United States, Canada and Australia (Win et al. 2015). However, a Japanese hospital-based study found LLS prevalence in CRC cases to be significantly lower (0.2%) (Chika et al. 2017), which may reflect ethnicity differences between countries.
Several potential mechanisms may underlie LLS, including the presence of an atypical germline pathogenic variant or cryptic mutations in MMR genes not identified by current detection methods or germline pathogenic variants in genes outside MMR genes (Buchanan et al. 2014; Carethers 2014; Pico et al. 2020a). The predominant cause of LLS-related MMR deficiency, responsible for up to 80% of LLS cancers, involves double somatic mutations in the same MMR gene, known as biallelic MMR deficiency (Geurts-Giele et al. 2014; Haraldsdottir et al. 2014; Mensenkamp et al. 2014). Mosaicism of a de novo pathogenic variant may also underlie LLS but is rarely described (Guillerm et al. 2020). Moreover, incorrect immunohistochemistry staining has been identified as contributing factor to LLS diagnoses (Haraldsdottir et al. 2014). Subsequently, LLS cases represent a heterogeneous population comprised of sporadic cases related to biallelic MMR deficiency and inherited cases related to undetected LS or germline pathogenic variants in other DNA repair genes (Clendenning et al. 2011; Haraldsdottir et al. 2014; Liu et al. 2016; Mensenkamp et al. 2014; Morak et al. 2010).
While LS-associated cancer risks are well-known (Dominguez-Valentin et al. 2020; International Mismatch Repair 2021), and there are standard CRC surveillance strategies for LS patients and first-degree relatives (FDRs) (Monahan et al. 2020), LLS-associated cancer risks are unclear, with studies showing conflicting results with regards to the age of CRC diagnosis and risks of CRC and other cancers in LLS patients and FDRs (Bucksch et al. 2020; Overbeek et al. 2007; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015). Subsequently, no agreed consensus on cancer screening recommendations for LLS patients and FDRs currently exists (Ladabaum 2020). This uncertainty creates challenges for genetic counseling, conferring different degrees of screening for LLS patients and families, ranging from surveillance guidelines for intermediate-risk individuals (Win et al. 2015), to vigorous LS-recommended guidelines (Monahan et al. 2020; Overbeek et al. 2007). Patients with a LLS diagnosis report variability in the interpretation of their diagnosis, cancer risk management advice and how that is communicated to family members (den Elzen et al. 2021). This present study examined the current evidence for cancer risks in LLS patients and FDRs by systematic review of all relevant studies. The findings of this review may inform future surveillance strategies for LLS patients and FDRs.
Materials and methods
Systematic review of all studies examining LLS-associated cancer risks published from January 1st 1980 to 11th February 2021 was conducted using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria (Moher et al. 2010). The review was registered in PROSPERO (CRD42021238428).
Search strategy
Medical Subject Headings (MeSH) terms were used to search databases: MEDLINE (Ovid), PubMed, EMBASE, Cochrane Library and Cumulative Index of Nursing and Allied Health Literature (CINAHL). An intersection of MeSH terms related to Lynch-like syndrome (‘Lynch-like’ or ‘suspected Lynch’ or ‘Lynch mimic’ or ‘Lynch like’), Lynch syndrome and hereditary nonpolyposis CRC (HNPCC) were used for the search strategy (Supplementary Table 1). Studies pertaining to cancer risks in LLS patients and families were selected for inclusion by identifying relevant abstracts and screening full-text articles for eligibility by two co-authors (SASG and PPN). Manual reference and citation checking was performed to identify relevant studies not found from the search strategy. Discrepancies between reviewers were resolved by a third reviewer (JCR).
Eligibility criteria
Inclusion criteria included studies examining cancer risks in CRC patients with confirmed LLS diagnosis following germline MMR gene mutation analysis and MSI analysis or immunohistochemistry (IHC). Papers not published in English, case studies, reviews, editorials, comparative studies and conference abstracts were excluded.
Data abstraction
Data extraction from full-text articles fulfilling study criteria was performed independently by co-authors (SASG, PPN and MIP) and confirmed by a third reviewer (JCR). A standardized data extraction form was used to summarize participant characteristics and study findings (Alvarez-Lafuente et al. 2004).
Risk of bias assessment
Two reviewers (SASG and PPN) assessed risk of bias using Joanna Briggs Institute (JBI) Critical Appraisal Checklists according to study type (Soldan et al. 1997) with any disagreements resolved by a third reviewer (JCR). The JBI tool comprises 8–11 checklists (depending on study type), with options of “yes”, “no”, “unclear” or “not applicable” for each question. Studies were classified low risk (> 80%), moderate risk (60–80%), or high risk of bias (< 60%) (Chima et al. 2019; Reece et al. 2021). No studies were excluded based on risk of bias assessment for completeness of reporting all relevant study findings (Shea et al. 2017).
Narrative synthesis
A comprehensive narrative synthesis of included studies was conducted summarizing main study characteristics and findings (Green et al. 2006). Data findings were analyzed separately before summarizing results for narrative synthesis. A meta-analysis was not possible due to heterogeneity of data across included studies.
Results
A total of 1665 studies were identified following searching of five databases (Fig. 1). After removal of duplicates, 169 remaining studies were screened based on title/abstract and 159 studies not fulfilling study criteria were removed. The full-text of 12 remaining studies was assessed for eligibility and five studies were removed for examining a different outcome (not cancer risks) (Giri et al. 2019; Pearlman et al. 2019), different research question (cancer screening adherence and perceived cancer risks in LLS CRC cases (Katz et al. 2016), UNC5C mutations in LLS patients (Kury et al. 2014), and validation of an online questionnaire in people undergoing colonoscopy to identify individuals with higher familial and hereditary CRC risks) (Kallenberg et al. 2015). A further study was excluded as it was a comparative study (Mas-Moya et al. 2015). Manually checking reference and citation lists of included papers, identified two further papers for study inclusion, giving a total of six included studies.
The six studies [five cohort (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015; Xu et al. 2020), and one cross-sectional (Overbeek et al. 2007)] were published between 2007 and 2020 (Table 1). Two studies were from Spain (Pico et al. 2020b; Rodriguez-Soler et al. 2013), one from the Netherlands (Overbeek et al. 2007), Germany (Bucksch et al. 2020), China (Xu et al. 2020), and Australia (using Colon Cancer Family Register data from Australia, US and Canada) (Win et al. 2015).
Five studies had low risk of bias (Bucksch et al. 2020; Overbeek et al. 2007; Rodriguez-Soler et al. 2013; Win et al. 2015; Xu et al. 2020), and one had moderate risk (Table 2; Supplementary Tables 2–3) (Rodriguez-Soler et al. 2013). Strengths and limitations of studies are outlined.
Lynch-like syndrome definition
There were minor differences in LLS definitions across studies (Table 1). All studies performed MSI analysis except one(Xu et al. 2020), IHC to identify MMR deficiency of MLH1, MSH2, MSH6, and PMS2 and germline analysis to confirm the absence of a DNA MMR gen,(Bucksch et al. 2020; Overbeek et al. 2007; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015), with three studies confirming the absence of EPCAM germline mutations (Bucksch et al. 2020; Pico et al. 2020b; Xu et al. 2020). Four studies included tumors with loss of MLH1 expression without MLH1 promoter hypermethylation (Overbeek et al. 2007; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015). Two studies examined BRAF V600E mutations: one study including tumors with or without a mutation (Win et al. 2015), and the other including tumors without a mutation (Xu et al. 2020). No studies examining LLS-associated cancer risks screened for the presence of double somatic MMR mutations (Monahan et al. 2020).
LLS-related cancer risks
While the present study aimed to examined to examine cancer risks in LLS, this review predominantly focuses on a comparison of cancer risks in LLS compared to LS probands and FDRs, with less focus on cancer risks in LLS compared to the general population. This was a direct result of the study design of most included studies that mainly examined cancer risks in LLS compared with LS. Further, the most common cancer types examined in included studies were LS-related cancers, particularly CRC and endometrial cancer.
Age of CRC diagnosis
In the Win et al. large population-based study the mean (± SD) age of CRC diagnosis was slightly higher for LLS probands [48.8 (± 12.3) years] than for LS probands [45.0 (± 11.3) years] (Win et al. 2015), consistent with the mean CRC diagnosis age of 44 years for both LLS and LS patients in a smaller Dutch study (Overbeek et al. 2007). Similarly, in a small study (n = 34) examining cancer risk perceptions not included in the review, the mean CRC diagnosis age of LLS patients was 47.6 (± 10.9) years but these were a selected subgroup (Katz et al. 2016).
In contrast, a Spanish study by Pico et al. found the median CRC diagnosis age (SD) in LLS patients was significantly higher [54.9 (14.2) years] than LS patients [48.1 (12.9) years, p = 0.01] (Pico et al. 2020b). However, this may reflect the small study size compared with the Win et al. (2015) study.
In LLS FDRs, Win et al. found the mean CRC diagnosis age as significantly older (57.9 ± 14.8 years) than LS FDRs (49.1 ± 13.1; p < 0.001) (Win et al. 2015), comparable with findings of the smaller Chinese study where the mean age of diagnosis in LLS families was 44.5 ± 13.6 years compared with 37.5 ± 8.6 years in LS families (Xu et al. 2020). However, in the small Spanish study by Rodriguez-Soler et al., the mean CRC diagnosis age between LLS FDRs (53.71 ± 16.8 years) and LS FDRs was not different (48.5 ± 14.13 years; p = 0.23) (Rodriguez-Soler et al. 2013).
Notably, confirmation of CRC diagnoses may potentially influence these results. In the Win et al. study, 43% of CRC diagnoses were confirmed by medical records, with proband and family members interviewed to confirm CRC diagnoses, whereas in the two Spanish studies, cancer diagnoses were confirmed by medical records which are likely to be more reliable (Rodriguez-Soler et al. 2013; Xu et al. 2020).
Risk of any cancer
In the German study by Bucksch et al., the standard incidence ratio (SIR) of any cancer in LLS patients was 2.7 (95% CI 1.2–5.4) which was not significantly different to LS patients (Table 3; SIR = 5.3, 95% CI 3.8–7.3) (Bucksch et al. 2020). However, the cumulative risk of any cancer in LLS patients at 70 years was significantly lower compared to LS patients (log-rank; p = 0.043).
CRC risks
Bucksch et al. found no difference in CRC incidence in LLS patients (SIR = 14.8; 95% CI 5.4–32.2) compared with LS patients (SIR = 24.3, 95% CI 16.2–35.1) or CRC risks in LLS patients at age 70 (21.0%, 95% CI 9.9–41.3%) compared to LS patients (40.9%, 95% CI 28.3–56.4%; log-rank, p = 0.102) (Bucksch et al. 2020). However, this study may be underpowered to identify differences given the small study size, as evidenced by the wide confidence intervals and the inability to find a difference in lifetime CRC risk between LS and Familial Colorectal Cancer Type X (FCCTX) which is inconsistent with a previous study (Samadder et al. 2017).
In males with LLS, Bucksch et al. found CRC incidence was higher (SIR = 25.2, 95% CI 13.4–43.2) than females (SIR = 6.3; 95% CI 0.8–22.7), consistent with Xu et al. where the mean number of males with CRC in LLS families was higher (2.04 ± 1.63) than females (1.54 ± 1.32) (Xu et al. 2020). Similarly, higher incidences of CRC cases in males have been reported in population-based cancer registry data from Europe, Australia and the US (Bray et al. 2018), and in LS families (Sehgal et al. 2014).
Prospective follow-up of participants after their first colonoscopy or at 25 years by Bucksch et al. found LLS index patients had higher CRC risks at 70 years (50%, 95% CI 19.6–88.9%) than their at-risk relatives (13.2%, 95% CI 4.4–35.9%; p = 0.027).(Bucksch et al. 2020) Further, in the Pico et al. prospective follow-up study, CRC incidence was lower in LLS patients and families (0.5%) compared with LS patients and families (1.9%; p = 0.019) and LLS patients were at significantly lower risk of CRC than LS patients (log-rank; p = 0.0001) (Pico et al. 2020b).
In an earlier study, Overbeek et al. found LLS families carried a lower CRC risk (11%) compared with LS families (66%; p < 0.009) (Overbeek et al. 2007). Three later studies found CRC incidence in LLS FDRs was higher than the general population but lower than LS FDRs; in Rodriguez-Soler et al. and Pico et al. studies the CRC SIR was 2.1 in LLS FDRs (Pico et al. 2020b; Rodriguez-Soler et al. 2013), and 6.04 (95% CI 3.58–9.54) (Rodriguez-Soler et al. 2013), and 4.25 (95% CI 3.67–4.90; p < 0.001) (Pico et al. 2020b), respectively, in LS FDRs. Consistent with these findings, the larger Win et al. study found CRC incidence was lower in LLS FDRs (SIR = 3.45 95% CI 2.62–4.57) than LS FDRs but SIRs were higher in magnitude (SIR = 9.67, 95% CI 7.10–13.1) (Win et al. 2015). Notably, both Spanish studies comprised small family cohorts so there was potentially selection bias. Pico et al. also included LS FDRs regardless of whether or not they carried MMR mutations (Pico et al. 2020b), where Rodriguez-Soler et al. only performed genetic testing in people with cancers which may influence study findings (Rodriguez-Soler et al. 2013). In the Win et al. study, as 57% of CRC diagnoses in FDRs were self-reported (Win et al. 2015), if a proportion of these are false-positive diagnoses, this may underestimate true associations.
Stratification by tumor location in the small Chinese cohort found significantly less left-sided CRCs and significantly more rectal tumors in LLS families compared with LS families (Xu et al. 2020). Notably, the study by Mas-Moya et al. also found LLS patients were more likely to have right-sided colon cancers and not have synchronous and metachronous tumors (Mas-Moya et al. 2015), but as this was a comparative study it was not included in the systematic review.
Risks of extra-colonic Lynch syndrome-related cancers
Two small Spanish studies showed conflicting results in extra-colonic LS-related cancer (ECLSRC) risks. Pico et al. found the incidence of ECLSRCs in LLS FDRs was higher than the general population (SIR = 2.04, 95% CI 1.44–2.80) but lower than LS FDRs (SIR = 5.01, 95% CI 4.26–5.84; p < 0.001) (Pico et al. 2020b). However, no difference between LLS families and LS families in frequencies of ovarian, stomach, urinary tract, skin, small intestine, brain and biliary tract cancer were found (p < 0.05). Similarly, Rodriguez-Soler et al. found the incidence of ECLSRCs in LLS FDRs was not higher than the general population (SIR = 1.69, 95% CI 0.73–3.34) and lower than LS FDRs (SIR = 2.81, 95% CI 1.03–6.12) (Rodriguez-Soler et al. 2013).
In a prospective follow-up, Pico et al. found the appearance of new cases of ECLSRCs after an index case diagnosis was lower in LLS patients and families (0.3%) compared with LS patients and families (2%; p 0.006) (Pico et al. 2020b).
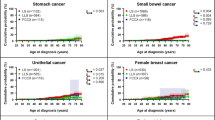
Endometrial cancer risks
Bucksch et al. found endometrial cancer incidence in LLS patients (SIR = 14.5; 95% CI 4.7–33.8) was significantly lower than in LS patients (SIR = 57.8, 95% CI 36.7–86.8) (Bucksch et al. 2020), consistent with increased LS-related endometrial cancer risks (Hampel et al. 2006). Cumulative endometrial cancer risk at 70 years was also significantly lower in LLS patients compared to LS patients (log-rank; 0.002).
While Pico et al. found the frequency of endometrial cancer in LLS FDRs was high (20%), it was significantly lower than LS FDRs (48.4%; p = 0.001) (Pico et al. 2020b). Bucksch et al. also found endometrial cancer risks in index LLS patients at 70 years were lower (4.0%, 95% CI 1.0–15.3%) than LLS relatives (23.1%, 95% CI 8.1–55.8%; p = 0.01) (Bucksch et al. 2020).
Urothelial cancer risks
Bucksch et al. found the incidence of urothelial cancer in LLS patients was higher than the general population (SIR = 6.6; 95% CI 1.8–16.8) and not significantly different to LS patients (SIR = 27.7, 95% CI 12.7–52.6); however, cumulative risk at 70 years was lower in LLS patients compared to LS patients (log-rank; p = 0.015) (Bucksch et al. 2020). Further, women from LLS families with MSH2 protein deficiency had higher urothelial cancer risks than from LLS families with MLH1 or MSH6 protein deficiency (p = 0.003) (Bucksch et al. 2020).
Pancreatic cancer risks
Pico et al. found 6 of the 40 extra-colonic tumors in LLS FDRs were pancreatic tumors (15%), significantly higher than in LS FDRs (3.3%; p = 0.003) (Pico et al. 2020b). Similarly, Xu et al. found 1 pancreatic cancer case in 29 extra-colonic tumors (3.5%) in LLS families and no cases in LS families (Xu et al. 2020).
Stomach cancer risks
One study reporting stomach cancer incidence in LLS patients found the incidence (SIR = 6.1; 95% CI 1.7–15.7) was similar to LS patients (SIR = 6.1, 95% CI 2.8–11.6) (Bucksch et al. 2020). Stomach cancer incidence was also higher in males with LLS (SIR = 7.7; 95% CI 1.6–22.5), similar to males with LS (SIR = 5.2, 95% CI 1.7–12.2).
Small bowel cancer risks
Bucksch et al. found the incidence of small bowel cancer in LLS patients was comparable to the general population (SIR = 11.9, 95% CI 0.3–66.3) and significantly lower than in LS patients (SIR = 126.0, 95% CI 79.9–189.0) (Bucksch et al. 2020). However, the number of cases was small as indicated by the wide confidence intervals. Nevertheless, cumulative cancer risks at 70 years were significantly lower in LLS patients than LS patients (log-rank; 0.004).
Surveillance recommendations
Rodriguez-Soler et al. recommended cancer surveillance for LLS families to be commenced at similar age as LS families albeit with longer intervals between surveillance, given the age of CRC diagnosis between LS and LLS patients was similar while the CRC risks were lower in LLS families than LS families (Table 3) (Rodriguez-Soler et al. 2013). Pico et al. recommended cancer screening for FDRs of LLS patients and gynaecologic surveillance of female LLS patients and FDRs, due to higher CRC and gynaecological cancer risks in LLS compared with the general population (Pico et al. 2020b). Win et al. suggested compliance with general age-dependent screening recommendations but for CRC screening of FDRs of CRC cases to commence screening earlier (40 years) due to the younger age of CRC diagnosis in LLS probands and higher CRC risk in LLS FDRs (Win et al. 2015). Xu et al. recommended commencing screening at an early (unspecified) age, taking family history and higher rectal cancer risks into consideration (Xu et al. 2020).
Discussion
Clinicopathological characteristics of LLS tumors are similar to LS tumors. However, while cancer risks in LS patients and FDRs are well established, LLS-related cancer risks are less certain (Buchanan et al. 2014; Pico et al. 2020a). The present study represents the first systematic review to examine cancer risks in individuals with LLS and families to help address clinically related ambiguities and surveillance strategies. Review of six included studies (five cohort and one cross-sectional) found CRC incidence in LLS patients was similar to LS patients (Bucksch et al. 2020); however, CRC incidence in LLS FDRs was lower than LS FDRs but higher than the general population (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015). Studies also found the age of CRC diagnosis was comparable between LS and LLS patients (Overbeek et al. 2007; Win et al. 2015), and FDRs (Rodriguez-Soler et al. 2013), but these findings were inconsistent across studies (Pico et al. 2020b; Rodriguez-Soler et al. 2013; Xu et al. 2020).
Notably, two studies found endometrial cancer risks in LLS patients and FDRs were lower than LS patients and FDRs but significantly higher than the general population (Bucksch et al. 2020; Pico et al. 2020b). The incidence of urothelial and stomach cancer in LLS patients was also high, comparable to LS patients, advising vigilance for related symptoms, particularly in females with MSH2 protein deficiency due to associated risks (Bucksch et al. 2020). While two studies indicated pancreatic cancer risks may be elevated in LLS families (Pico et al. 2020b; Xu et al. 2020), surveillance for pancreatic cancer is currently only recommended for high-risk individuals in a research setting (Pico et al. 2020b).
Critically, it is important to consider findings of this review in the context of the shortcomings of the current definition of the molecular phenotype of LLS. Although there are a number of potential causes of LLS, there is the possibility of heterogeneity across different LLS populations due to the differing definitions used in studies examining LLS-related cancer risks (Clendenning et al. 2011; Haraldsdottir et al. 2014; Liu et al. 2016; Mensenkamp et al. 2014; Morak et al. 2010). In particular, studies suggest up to 80% of cases suspected to have LLSs have double somatic MMR mutations (biallelic MMR deficiency) (Geurts-Giele et al. 2014; Haraldsdottir et al. 2014; Mensenkamp et al. 2014), with the most recent NCCN guidelines (Genetic/Familial High-Risk Assessment: Colorectal, version 1.2021) not available prior to the included studies, recommending screening for double somatic mutations in people with unexplained MMR deficiency. Importantly, Pearlman et al. also found people with LS were more likely to be afflicted with LS-related tumors than people with double somatic mutations and also meet Amsterdam II criteria (Pearlman et al. 2019). Other studies indicated current analytic techniques may not identify cryptic or complex MMR genetic variants (Clendenning et al. 2011; Morak et al. 2010; Pope et al. 2021), or variants in MMR regulatory regions rarely screened (Liu et al. 2016). However, as studies examining LLS-related cancer risks did not screen for the presence of double somatic mutations or these variants, we could only report the findings from available studies and acknowledge that LLS populations comprise a heterogeneous population with a large number of cases with double somatic mutations. Future studies should aim to examine the LLS-related cancer risks for patients with confirmed double somatic MMR mutations.
Clarifying the definition of LLS may be possible through advances in genetic testing strategies, as indicated by a recent study using a gene panel designed ad hoc in combination with pathogenicity variant assessment to identify potentially causal LLS genes (deleterious MMR mutations) (Damaso et al. 2020). This is particularly pertinent for older studies included in the review using less accurate genetic technology than newer studies (Overbeek et al. 2007; Rodriguez-Soler et al. 2013), but as three of the six included studies were published within the last year (Bucksch et al. 2020; Pico et al. 2020b; Xu et al. 2020), the findings of this review are likely to be relevant for some time until there is a broader implementation of tumor testing to resolve LLS diagnosis.
Despite the acknowledged limitations regarding included studies failing to identify double somatic mutations in LLS patients, our findings support regular colonoscopy screening of index cases in LLS patients and implementing early cancer screening in LLS FDRs due to earlier ages of CRC diagnoses and elevated CRC risks in LLS patients and FDRs (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015). Monahan et al. currently recommends 2-yearly colonoscopy screening for CRC (as opposed to FIT/FOBT) for LLS individuals with unexplained MMR deficiency that do not have double somatic mutations and FDRs up to 75 years commencing at 25 years, consistent with recommendations for MLH1 and MSH2 pathogenic variant carriers (Monahan et al. 2020). However, as two studies found the age of CRC diagnosis was older in LLS patients (Pico et al. 2020b), and LLS FDRs (Win et al. 2015), than LS patients and FDRs, colonoscopy surveillance could potentially commence later, consistent with Monahan et al. recommendations for MSH6 and PMS2 pathogenic variant carriers (at 35 years) (Monahan et al. 2020). Further, longer intervals between colonoscopy may be advised due to lower CRC risks in LLS FDRs than LS FDRs (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015), consistent with the Buchanan et al. review that favored increased intervals > 2 years between screening (Buchanan et al. 2014). Importantly, family history of cancer needs to be considered and clinical recommendations devised based on individual LLS families which may result in personalized colonoscopy surveillance strategies for certain LLS families (Bucksch et al. 2020; Xu et al. 2020). Moreover, Monaghan et al. recommend individuals with double somatic MMR mutations be followed up based on family history of cancer, not LLS guidelines (Monahan et al. 2020).
Strengths of this study include the strict adherence to PRISMA guidelines (Page et al. 2021), and strict study eligibility criteria to identify and include relevant articles. Search strategies, data extractions and risk of bias assessment were performed by two independent reviewers, with a third person resolving any discrepancies. Included studies used appropriate and uniform methods for identifying MMR-deficient tumors and genetic phenotyping to define LLS and LS patients (Bucksch et al. 2020; Overbeek et al. 2007; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015). Consequently, comparisons across studies are unlikely to be affected by the methodology used across studies. Further, five included studies had a low risk of bias (Bucksch et al. 2020; Overbeek et al. 2007; Pico et al. 2020b; Win et al. 2015; Xu et al. 2020).
The study is limited by the scarcity of relevant studies examining LLS-related cancer risks eligible for inclusion and heterogeneity between included studies related to cancer diagnosis assessments, follow-up times and subgroups of participants. As mentioned, none of the included studies screened for the presence of double somatic mutations and, especially for older studies, the extent of germline MMR gene testing to identify more challenging mutations such as the inversion of exons 1–7 in MSH2 is unclear. Consequently, it was not feasible to conduct a meta-analysis to quantitate cancer risks. While two studies examined prospective follow-up (Bucksch et al. 2020; Pico et al. 2020b), only Bucksch et al. reported intensified colonoscopy surveillance of participants (Bucksch et al. 2020), and Pico et al. acknowledged decreased adherence to follow-up in LLS FDRs, potentially due to an unclear LLS diagnosis (Carayol et al. 2002), may limit study findings (Pico et al. 2020b). Median follow-up was relatively short (3–8.3 years) (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013; Win et al. 2015), so cancers may not have been detected during this time. Further, some studies had only small numbers of cases, particularly for extra-colonic cancers (Bucksch et al. 2020; Pico et al. 2020b; Rodriguez-Soler et al. 2013), influencing reported cancer risks and screening recommendations. Study findings may also not be generalizable to non-Caucasian populations as the review did not include any studies from non-Westernized countries.
Conclusion
Systematic review of relevant articles in the literature found LLS patients and FDRs are at increased risk of developing CRC and potentially at an earlier age to the general population, supporting recommendations of increased colonoscopy surveillance for LLS patients and FDRs, in line with LS guidelines. However, commencing screening at a later age and extending the time between screening may be considered for low-risk LLS families. Future studies focused on molecularly characterized LLS cases will help resolve the germline and somatic etiological heterogeneity and enable studies to refine cancer risks for double somatic MMR mutation cases, leading to more personalized surveillance strategies for individual patients and families.
Data and materials availability
All data are available for this study.
References
Alvarez-Lafuente R, De Las Heras V, Bartolome M, Picazo JJ, Arroyo R (2004) Beta-interferon treatment reduces human herpesvirus-6 viral load in multiple sclerosis relapses but not in remission. Eur Neurol 52(2):87–91
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. https://doi.org/10.3322/caac.21492
Buchanan DD, Rosty C, Clendenning M, Spurdle AB, Win AK (2014) Clinical problems of colorectal cancer and endometrial cancer cases with unknown cause of tumor mismatch repair deficiency (suspected Lynch syndrome). Appl Clin Genet 7:183–193. https://doi.org/10.2147/TACG.S48625
Bucksch K, Zachariae S, Aretz S, Buttner R, Holinski-Feder E, Holzapfel S, Huneburg R, Kloor M, von Knebel Doeberitz M, Morak M, Moslein G, Nattermann J, Perne C, Rahner N, Schmiegel W, Schulmann K, Steinke-Lange V, Strassburg CP, Vangala DB, Weitz J, Loeffler M, Engel C, German Consortium for Familial Intestinal, C (2020) Cancer risks in Lynch syndrome, Lynch-like syndrome, and familial colorectal cancer type X: a prospective cohort study. BMC Cancer 20(1):460. https://doi.org/10.1186/s12885-020-06926-x
Cancer Genome Atlas N (2012) Comprehensive molecular characterization of human colon and rectal cancer. Nature 487(7407):330–337. https://doi.org/10.1038/nature11252
Carayol J, Khlat M, Maccario J, Bonaiti-Pellie C (2002) Hereditary non-polyposis colorectal cancer: current risks of colorectal cancer largely overestimated. J Med Genet 39(5):335–339. https://doi.org/10.1136/jmg.39.5.335
Carethers JM (2014) Differentiating lynch-like from lynch syndrome. Gastroenterology 146(3):602–604. https://doi.org/10.1053/j.gastro.2014.01.041
Carethers JM, Stoffel EM (2015) Lynch syndrome and Lynch syndrome mimics: the growing complex landscape of hereditary colon cancer. World J Gastroenterol 21(31):9253–9261. https://doi.org/10.3748/wjg.v21.i31.9253
Chika N, Eguchi H, Kumamoto K, Suzuki O, Ishibashi K, Tachikawa T, Akagi K, Tamaru JI, Okazaki Y, Ishida H (2017) Prevalence of lynch syndrome and lynch-like syndrome among patients with colorectal cancer in a Japanese hospital-based population. Jpn J Clin Oncol 47(2):191. https://doi.org/10.1093/jjco/hyw200
Chima S, Reece JC, Milley K, Milton S, McIntosh JG, Emery JD (2019) Decision support tools to improve cancer diagnostic decision making in primary care: a systematic review. Br J Gen Pract 69(689):e809–e818. https://doi.org/10.3399/bjgp19X706745
Clendenning M, Buchanan DD, Walsh MD, Nagler B, Rosty C, Thompson B, Spurdle AB, Hopper JL, Jenkins MA, Young JP (2011) Mutation deep within an intron of MSH2 causes Lynch syndrome. Fam Cancer 10(2):297–301. https://doi.org/10.1007/s10689-011-9427-0
Damaso E, Gonzalez-Acosta M, Vargas-Parra G, Navarro M, Balmana J, Ramon YCT, Tuset N, Thompson BA, Marin F, Fernandez A, Gomez C, Velasco A, Solanes A, Iglesias S, Urgel G, Lopez C, Del Valle J, Campos O, Santacana M, Matias-Guiu X, Lazaro C, Valle L, Brunet J, Pineda M, Capella G (2020) Comprehensive constitutional genetic and epigenetic characterization of lynch-like individuals. Cancers (basel). https://doi.org/10.3390/cancers12071799
den Elzen N, Joseland SL, Saya S, Jonnagadla S, Isbister J, Winship I, Buchanan DD (2021) “Left in limbo”: exploring how patients with colorectal cancer interpret and respond to a suspected Lynch syndrome diagnosis. Hered Cancer Clin Pract 19(1):43. https://doi.org/10.1186/s13053-021-00201-1
Dominguez-Valentin M, Sampson JR, Seppala TT, Ten Broeke SW, Plazzer JP, Nakken S, Engel C, Aretz S, Jenkins MA, Sunde L, Bernstein I, Capella G, Balaguer F, Thomas H, Evans DG, Burn J, Greenblatt M, Hovig E, de Vos-Tot-Nederveen-Cappel WH, Sijmons RH, Bertario L, Tibiletti MG, Cavestro GM, Lindblom A, Della Valle A, Lopez-Kostner F, Gluck N, Katz LH, Heinimann K, Vaccaro CA, Buttner R, Gorgens H, Holinski-Feder E, Morak M, Holzapfel S, Huneburg R, Knebel Doeberitz MV, Loeffler M, Rahner N, Schackert HK, Steinke-Lange V, Schmiegel W, Vangala D, Pylvanainen K, Renkonen-Sinisalo L, Hopper JL, Win AK, Haile RW, Lindor NM, Gallinger S, Le Marchand L, Newcomb PA, Figueiredo JC, Thibodeau SN, Wadt K, Therkildsen C, Okkels H, Ketabi Z, Moreira L, Sanchez A, Serra-Burriel M, Pineda M, Navarro M, Blanco I, Green K, Lalloo F, Crosbie EJ, Hill J, Denton OG, Frayling IM, Rodland EA, Vasen H, Mints M, Neffa F, Esperon P, Alvarez K, Kariv R, Rosner G, Pinero TA, Gonzalez ML, Kalfayan P, Tjandra D, Winship IM, Macrae F, Moslein G, Mecklin JP, Nielsen M, Moller P (2020) Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the Prospective Lynch Syndrome Database. Genet Med 22(1):15–25. https://doi.org/10.1038/s41436-019-0596-9
Geurts-Giele WR, Leenen CH, Dubbink HJ, Meijssen IC, Post E, Sleddens HF, Kuipers EJ, Goverde A, van den Ouweland AM, van Lier MG, Steyerberg EW, van Leerdam ME, Wagner A, Dinjens WN (2014) Somatic aberrations of mismatch repair genes as a cause of microsatellite-unstable cancers. J Pathol 234(4):548–559. https://doi.org/10.1002/path.4419
Giri VN, Hegarty SE, Hyatt C, O’Leary E, Garcia J, Knudsen KE, Kelly WK, Gomella LG (2019) Germline genetic testing for inherited prostate cancer in practice: implications for genetic testing, precision therapy, and cascade testing. Prostate 79(4):333–339. https://doi.org/10.1002/pros.23739
Green BN, Johnson CD, Adams A (2006) Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med 5(3):101–117. https://doi.org/10.1016/S0899-3467(07)60142-6
Guillerm E, Svrcek M, Bardier-Dupas A, Basset N, Coulet F, Colas C (2020) Molecular tumor testing in patients with Lynch-like syndrome reveals a de novo mosaic variant of a mismatch repair gene transmitted to offspring. Eur J Hum Genet 28(11):1624–1628. https://doi.org/10.1038/s41431-020-0689-6
Hampel H, Frankel W, Panescu J, Lockman J, Sotamaa K, Fix D, Comeras I, La Jeunesse J, Nakagawa H, Westman JA, Prior TW, Clendenning M, Penzone P, Lombardi J, Dunn P, Cohn DE, Copeland L, Eaton L, Fowler J, Lewandowski G, Vaccarello L, Bell J, Reid G, de la Chapelle A (2006) Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients [Research Support, NIH, Extramural Research Support, Non-US Gov’t]. Cancer Res 66(15):7810–7817. https://doi.org/10.1158/0008-5472.CAN-06-1114
Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, Clendenning M, Sotamaa K, Prior T, Westman JA, Panescu J, Fix D, Lockman J, LaJeunesse J, Comeras I, de la Chapelle A (2008) Feasibility of screening for Lynch syndrome among patients with colorectal cancer [Comparative Study Multicenter Study Research Support, NIH, Extramural Research Support, Non-US Gov’t]. J Clin Oncol 26(35):5783–5788. https://doi.org/10.1200/JCO.2008.17.5950
Haraldsdottir S, Hampel H, Tomsic J, Frankel WL, Pearlman R, de la Chapelle A, Pritchard CC (2014) Colon and endometrial cancers with mismatch repair deficiency can arise from somatic, rather than germline, mutations. Gastroenterology 147(6):1308-1316.e1301. https://doi.org/10.1053/j.gastro.2014.08.041
International Mismatch Repair C (2021) Variation in the risk of colorectal cancer in families with Lynch syndrome: a retrospective cohort study. Lancet Oncol 22(7):1014–1022. https://doi.org/10.1016/S1470-2045(21)00189-3
Kallenberg FG, Ijspeert JE, Bossuyt PM, Aalfs CM, Dekker E (2015) Validation of an online questionnaire for identifying people at risk of familial and hereditary colorectal cancer. Fam Cancer 14(3):401–410. https://doi.org/10.1007/s10689-015-9792-1
Katz LH, Burton-Chase AM, Advani S, Fellman B, Polivka KM, Yuan Y, Lynch PM, Peterson SK (2016) Screening adherence and cancer risk perceptions in colorectal cancer survivors with Lynch-like syndrome. Clin Genet 89(3):392–398. https://doi.org/10.1111/cge.12653
Kury S, Garrec C, Airaud F, Breheret F, Guibert V, Frenard C, Jiao S, Bonneau D, Berthet P, Bossard C, Ingster O, Cauchin E, Bezieau S (2014) Evaluation of the colorectal cancer risk conferred by rare UNC5C alleles. World J Gastroenterol 20(1):204–213. https://doi.org/10.3748/wjg.v20.i1.204
Ladabaum U (2020) What is lynch-like syndrome and how should we manage it? Clin Gastroenterol Hepatol 18(2):294–296. https://doi.org/10.1016/j.cgh.2019.08.009
Liu Q, Thompson BA, Ward RL, Hesson LB, Sloane MA (2016) Understanding the pathogenicity of noncoding mismatch repair gene promoter variants in lynch syndrome. Hum Mutat 37(5):417–426. https://doi.org/10.1002/humu.22971
Lynch HT, Snyder CL, Shaw TG, Heinen CD, Hitchins MP (2015) Milestones of Lynch syndrome: 1895–2015. Nat Rev Cancer 15(3):181–194. https://doi.org/10.1038/nrc3878
Mas-Moya J, Dudley B, Brand RE, Thull D, Bahary N, Nikiforova MN, Pai RK (2015) Clinicopathological comparison of colorectal and endometrial carcinomas in patients with Lynch-like syndrome versus patients with Lynch syndrome. Hum Pathol 46(11):1616–1625. https://doi.org/10.1016/j.humpath.2015.06.022
Mensenkamp AR, Vogelaar IP, van Zelst-Stams WA, Goossens M, Ouchene H, Hendriks-Cornelissen SJ, Kwint MP, Hoogerbrugge N, Nagtegaal ID, Ligtenberg MJ (2014) Somatic mutations in MLH1 and MSH2 are a frequent cause of mismatch-repair deficiency in Lynch syndrome-like tumors. Gastroenterology 146(3):643-646.e648. https://doi.org/10.1053/j.gastro.2013.12.002
Moher D, Liberati A, Tetzlaff J, Altman DG, Group, P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Monahan KJ, Bradshaw N, Dolwani S, Desouza B, Dunlop MG, East JE, Ilyas M, Kaur A, Lalloo F, Latchford A, Rutter MD, Tomlinson I, Thomas HJW, Hill J, Hereditary CRC, g. e. c. g. (2020) Guidelines for the management of hereditary colorectal cancer from the British Society of Gastroenterology (BSG)/Association of Coloproctology of Great Britain and Ireland (ACPGBI)/United Kingdom Cancer Genetics Group (UKCGG). Gut 69(3):411–444. https://doi.org/10.1136/gutjnl-2019-319915
Morak M, Laner A, Bacher U, Keiling C, Holinski-Feder E (2010) MUTYH-associated polyposis - variability of the clinical phenotype in patients with biallelic and monoallelic MUTYH mutations and report on novel mutations [Research Support, Non-US Gov’t]. Clin Genet 78(4):353–363. https://doi.org/10.1111/j.1399-0004.2010.01478.x
Overbeek LI, Kets CM, Hebeda KM, Bodmer D, van der Looij E, Willems R, Goossens M, Arts N, Brunner HG, van Krieken JH, Hoogerbrugge N, Ligtenberg MJ (2007) Patients with an unexplained microsatellite instable tumour have a low risk of familial cancer. Br J Cancer 96(10):1605–1612. https://doi.org/10.1038/sj.bjc.6603754
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. https://doi.org/10.1016/j.jclinepi.2021.03.001
Pearlman R, Haraldsdottir S, de la Chapelle A, Jonasson JG, Liyanarachchi S, Frankel WL, Rafnar T, Stefansson K, Pritchard CC, Hampel H (2019) Clinical characteristics of patients with colorectal cancer with double somatic mismatch repair mutations compared with Lynch syndrome. J Med Genet 56(7):462–470. https://doi.org/10.1136/jmedgenet-2018-105698
Pico MD, Castillejo A, Murcia O, Giner-Calabuig M, Alustiza M, Sanchez A, Moreira L, Pellise M, Castells A, Carrillo-Palau M, Ramon YCT, Gisbert-Beamud A, Llort G, Yague C, Lopez-Fernandez A, Alvarez-Urturi C, Cubiella J, Rivas L, Rodriguez-Alcalde D, Herraiz M, Garau C, Dolz C, Bujanda L, Cid L, Poves C, Garzon M, Salces I, Ponce M, Hernandez-Villalba L, Alenda C, Balaguer F, Soto JL, Jover R (2020a) Clinical and pathological characterization of lynch-like syndrome. Clin Gastroenterol Hepatol 18(2):368-374.e361. https://doi.org/10.1016/j.cgh.2019.06.012
Pico MD, Sanchez-Heras AB, Castillejo A, Giner-Calabuig M, Alustiza M, Sanchez A, Moreira L, Pellise M, Castells A, Llort G, Yague C, Ramon YCT, Gisbert-Beamud A, Cubiella J, Rivas L, Herraiz M, Garau C, Salces I, Carrillo-Palau M, Bujanda L, Lopez-Fernandez A, Alvarez-Urturi C, Lopez MJ, Alenda C, Zapater P, Lacueva FJ, Balaguer F, Soto JL, Murcia O, Jover R (2020b) Risk of cancer in family members of patients with lynch-like syndrome. Cancers (basel). https://doi.org/10.3390/cancers12082225
Pope BJ, Clendenning M, Rosty C, Mahmood K, Georgeson P, Joo JE, Walker R, Hutchinson RA, Jayasekara H, Joseland S, Como J, Preston S, Spurdle AB, Macrae FA, Win AK, Hopper JL, Jenkins MA, Winship IM, Buchanan DD (2021) Germline and tumor sequencing as a diagnostic tool to resolve suspected lynch syndrome. J Mol Diagn 23(3):358–371. https://doi.org/10.1016/j.jmoldx.2020.12.003
Reece JC, Neal EFG, Nguyen P, McIntosh JG, Emery JD (2021) Delayed or failure to follow-up abnormal breast cancer screening mammograms in primary care: a systematic review. BMC Cancer 21(1):373. https://doi.org/10.1186/s12885-021-08100-3
Rodriguez-Soler M, Perez-Carbonell L, Guarinos C, Zapater P, Castillejo A, Barbera VM, Juarez M, Bessa X, Xicola RM, Clofent J, Bujanda L, Balaguer F, Rene JM, de Castro L, Marin-Gabriel JC, Lanas A, Cubiella J, Nicolas-Perez D, Brea-Fernandez A, Castellvi-Bel S, Alenda C, Ruiz-Ponte C, Carracedo A, Castells A, Andreu M, Llor X, Soto JL, Paya A, Jover R (2013) Risk of cancer in cases of suspected lynch syndrome without germline mutation. Gastroenterology 144(5):926-932.e921. https://doi.org/10.1053/j.gastro.2013.01.044 (quiz e913–924)
Samadder NJ, Smith KR, Wong J, Thomas A, Hanson H, Boucher K, Kopituch C, Cannon-Albright LA, Burt RW, Curtin K (2017) Cancer risk in families fulfilling the amsterdam criteria for lynch syndrome. JAMA Oncol 3(12):1697–1701. https://doi.org/10.1001/jamaoncol.2017.0769
Sehgal R, Sheahan K, O’Connell PR, Hanly AM, Martin ST, Winter DC (2014) Lynch syndrome: an updated review. Genes (basel) 5(3):497–507. https://doi.org/10.3390/genes5030497
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. https://doi.org/10.1136/bmj.j4008
Soldan SS, Berti R, Salem N, Secchiero P, Flamand L, Calabresi PA, Brennan MB, Maloni HW, McFarland HF, Lin HC, Patnaik M, Jacobson S (1997) Association of human herpes virus 6 (HHV-6) with multiple sclerosis: increased IgM response to HHV-6 early antigen and detection of serum HHV-6 DNA. Nat Med 3(12):1394–1397
Umar A, Boland CR, Terdiman JP, Syngal S, de la Chapelle A, Ruschoff J, Fishel R, Lindor NM, Burgart LJ, Hamelin R, Hamilton SR, Hiatt RA, Jass J, Lindblom A, Lynch HT, Peltomaki P, Ramsey SD, Rodriguez-Bigas MA, Vasen HF, Hawk ET, Barrett JC, Freedman AN, Srivastava S (2004) Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst, 96(4):261–268. http://www.ncbi.nlm.nih.gov/pubmed/14970275
Win AK, Buchanan DD, Rosty C, MacInnis RJ, Dowty JG, Dite GS, Giles GG, Southey MC, Young JP, Clendenning M, Walsh MD, Walters RJ, Boussioutas A, Smyrk TC, Thibodeau SN, Baron JA, Potter JD, Newcomb PA, Le Marchand L, Haile RW, Gallinger S, Lindor NM, Hopper JL, Ahnen DJ, Jenkins MA (2015) Role of tumour molecular and pathology features to estimate colorectal cancer risk for first-degree relatives. Gut 64(1):101–110. https://doi.org/10.1136/gutjnl-2013-306567
Xu Y, Huang Z, Li C, Zhu C, Zhang Y, Guo T, Liu F, Xu Y (2020) Comparison of molecular, clinicopathological, and pedigree differences between lynch-like and lynch syndromes. Front Genet 11:991. https://doi.org/10.3389/fgene.2020.00991
Acknowledgements
We thank University of Melbourne library staff for their valuable assistance in the systematic review literature search.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. D.D.B. is supported by a NHMRC Investigator Grant (GNT1194896) and the University of Melbourne Dame Kate Campbell Fellowship.
Author information
Authors and Affiliations
Contributions
JCR and DDB designed and conceptualized the study plan. SASG and PPN identified the articles and screened the titles and abstracts. SASG, PPN and MIP screened the full-text articles. SASG, PPN, MIP and JCR extracted the data. SASG, PPN, DDB, MIP and JCR analyzed and interpreted the data. JCR, SASG, PPN, MIP and DDB wrote the manuscript. JCR, SASG, PPN, MIP and DDB reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Ethical approval was not required for this systematic review as data were acquired from published studies.
Informed consent
Consent to participate was not required for this systematic review as data were acquired from published studies.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nugroho, P.P., Ghozali, S.A.S., Buchanan, D.D. et al. Risk of cancer in individuals with Lynch-like syndrome and their families: a systematic review. J Cancer Res Clin Oncol 149, 25–46 (2023). https://doi.org/10.1007/s00432-022-04397-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04397-0