Abstract
Purpose
The prospective multicenter VARIANZ study aimed to identify resistance biomarkers for HER2-targeted treatment in advanced gastric and esophago-gastric junction cancer (GC, EGJC). HER2 test deviations were found in 90 (22.3%) of 404 cases (central versus local testing) and were associated with negative impact on survival for trastuzumab-treated patients. Here, we investigated methodological and biological variables that may promote deviating HER2 test results.
Methods
We analyzed HER2 testing procedures and participation in quality assurance programs of 105 participating local pathology laboratories. Furthermore, tumor localization and histological subtypes were compared between patients with centrally confirmed (central HER2 + /local HER2 + , n = 68) and unconfirmed HER2 status (central HER2 −/local HER2 + , n = 68).
Results
For central HER2 testing, concordance between in situ hybridization (ISH) and immunohistochemistry (IHC) was 98.3%, with IHC sensitivity of 93.3% (84 IHC + of 90 ISH +), specificity of 99.5% (389 IHC- of 391 ISH-), and a positive diagnosis rate of 97.7%. Central confirmation of the local HER2 IHC scores were seen for the majority of locally HER2- IHC 0/1 (172/178; 96.6%), but less frequently for locally IHC3 + (57/124; 46.0%) cases. Deviation rate was not associated with IHC antibody platform used in the local pathology institute neither with participation in quality-assuring tests. Regarding tumor characteristics, deviating test results were more frequently found in GC vs. EGJC (69.1% vs. 39.7%; p = 0.001) and in Laurén diffuse vs. intestinal subtype (23.5% vs. 5.9%, p = 0.004).
Conclusion
Tumor localization and histological subtype have an impact on HER2 test deviation rates. Assessment of HER2 remains challenging for GC and EGJC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, gastric cancer (GC) is the fifth most common cancer and the third leading cause of cancer-related deaths (Siegel et al. 2018). In the Western hemisphere, the majority of patients are diagnosed at advanced stages and median overall survival (mOS) is less than 1 year when patients are treated with platinum–fluoropyrimidine combination chemotherapy (Smyth et al. 2020). The Trastuzumab for Gastric Cancer (ToGA) study established the value of trastuzumab, an anti-HER2-directed monoclonal antibody, for treatment of HER2 + GC and esophago-gastric junction (EGJC). Until today, trastuzumab is the only targeted drug that has shown to improve OS of HER2-positive (HER2 +) GC patients in a randomized controlled phase III trial (Bang et al. 2010a, b). In contrast, some other HER2-targeting drugs have failed to improve survival outcomes in phase III trials (Hecht et al. 2016; Satoh et al. 2014; Tabernero et al. 2018; Thuss-Patience et al. 2017), while novel promising compounds are currently being studied (Bang et al. 2017; Kim et al. 2019; Shitara et al. 2020). HER2 overexpression and/or amplification is reported in 10–27% of the patients with advanced GC (Chua and Merrett 2012; Koopman et al. 2015; Press et al. 2017; Yoon et al. 2012). GC-specific guidelines for HER2 testing have been developed (Rüschoff et al. 2010). In contrast to breast cancer, basolateral HER2 staining in immunohistochemistry (IHC) is considered HER2 + because incomplete membranous staining is common in GC (Hofmann et al. 2008; Rüschoff et al. 2012). Furthermore, GC often shows heterogeneous HER2 expression (Grabsch et al. 2010; Leni et al. 2014; Peng et al. 2015; van Cutsem et al. 2015; Yang et al. 2012), which makes diagnostics even more complicated.
According to current recommendations (Bang et al. 2010a, b; Rüschoff et al. 2010), HER2 is primarily analyzed by IHC. Various antibodies from different commercial providers are available for HER2 IHC testing. For ToGA and other studies, the HercepTest (Dako, Glostrup, Denmark) was used (Dijksterhuis et al. 2020; He et al. 2015; Yoon et al. 2012), while other studies preferred the 4B5 HER2-antibody (Ventana Medical Systems, Tucson, AZ, United States). Concordance between the available antibodies has been demonstrated previously (Asioli et al. 2012; Boers et al. 2011; Cho et al. 2013; Radu et al. 2012; Rüschoff et al. 2010). However, 4B5 has also been reported of being more sensitive, leading to stronger HER2 membrane staining, but also non-specific cytoplasmic staining (Abrahão-Machado et al. 2013; Boers et al. 2011). CB11 (DCS, Hamburg, Germany) is a so far rarely used antibody (Grabsch et al. 2010) that is described as particularly specific, but less sensitive than other clones (Cappellesso et al. 2015; Cho et al. 2012; Schrohl et al. 2011). Currently, no specific HER2 companion diagnostic antibody is recommended for routine use in Europe (Baretton et al. 2019).
Current reports indicate that tumor biopsies are more often tested HER2 + than surgical specimens (Baretton et al. 2019; Kaito et al. 2019), and concordance of HER2 positivity between matched biopsies and surgical specimens or metastatic samples has been demonstrated in 96.1% and 94.9%, respectively (Bozzetti et al. 2011; Wang et al. 2014). However, it is also known that deviating HER2 test results occur when one investigator assessed different biopsies or different parts of a surgical specimen in the same patient (Xu et al. 2019). Additional block analysis increased both the sensitivity (from 63 to 83%) and the accuracy (from 91 to 94%) of IHC as compared with fluorescent in situ hybridization (Asioli et al. 2012).
HER2 + status is more frequently found in intestinal type than in diffuse type GC according to Laurén’s classification (Baretton et al. 2019; Cappellesso et al. 2015; Cho et al. 2013; Chua and Merrett 2012; Gomez-Martin et al. 2013; Gómez-Martin et al. 2012; Grabsch et al. 2010). EGJC tend to be more often HER2 + (24–33%) compared to distal GC (7–21%) (Baretton et al. 2019; Boers et al. 2011; van Cutsem et al. 2015; Yoon et al. 2012) which might be related to a higher rate of intestinal phenotype within EGJC (Shah et al. 2011). However, not all patients with HER2 + GC/EGJC seem to benefit from trastuzumab (Fu et al. 2018; Gomez-Martin et al. 2013; Lordick and Janjigian 2016; Yagi et al. 2019; Yi et al. 2016). The academic network study VARIANZ aimed to discover biomarkers to predict response or resistance to treatment with trastuzumab (Haffner et al. 2021). The majority of patients in VARIANZ were tested twice for tumor HER2 expression: once in local pathology institutes for diagnostic reasons and a second time in the central academic pathology institute as a study procedure. In 22.3% of the cases, central HER2 test results deviated from local tests. A significant survival advantage for patients treated with trastuzumab and a centrally confirmed HER2 + status (HER2 + /HER2 +) compared to a non-confirmed result.
(HER2 −/HER2 +) was reported previously (Haffner et al. 2021). In the present secondary analysis, we aimed to investigate whether deviating HER2 test results might be associated with the HER2 testing methodology or with tumor characteristics.
Methods
Study design
VARIANZ is a prospective, non-interventional multicenter study which recruited 548 patients at 35 German sites from 2014 to 2018. VARIANZ was funded by the German Federal Ministry of Education and Research (grant number: BMBF 01ZX1610E). Main results were published previously (Haffner et al. 2021). Briefly, adult patients receiving the first-line chemotherapy with or without trastuzumab for histologically confirmed advanced GC or EGJC were recruited. The primary endpoint was survival (OS), defined as time from the beginning of first-line chemotherapy until death from disease related cause. VARIANZ was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki. All patients had given written informed consent. Approvals for the study protocol were obtained from ethics committees of all study sites.
HER2 testing
The first HER2 diagnostic test was performed in local pathology institutes to determine the HER2 status and decide for the indication for trastuzumab therapy. The same or another tumor block was sent to the central pathology institute (Leipzig University Medical Center, Department of Pathology, Leipzig, Germany). HER2 expression was assessed centrally on fresh cut slides of the provided tumor block originating from primary tumor biopsies, surgical specimen or metastatic lesions using IHC (CB11 antibody, DCS, HI608C0I, Hamburg, Germany), and chromogenic in situ hybridization (ISH) (Zytomed Systems, C-3022-40, Berlin, Germany) according to established scoring criteria (Hofmann et al. 2008). The central laboratory did not receive the locally stained tissue sections. The IHC assessment was performed on fresh cut and newly stained slides without knowledge of the ISH results (and vice versa). ISH was performed and analyzed for all specimens regardless of the IHC test results. For IHC, all tumor cells per slide were analyzed and for ISH 20 cells were scored. For borderline cases (HER2/CEP17 ratio of 1.8–2.2), 40 more cells were analyzed. For HER2 evaluation, done by two dedicated GI pathologists at the central study pathology institute, no technical support or image analysis system was used.
In the country where this study was conducted, round robin tests of “Qualitätssicherungs-Initiative Pathologie QuIP GmbH” (https://www.quip.eu/de_DE/) are offered and recommended by the German Society of Pathology. For this purpose, QuIP sends unstained slides of gastric cancer to participating centers, on which either IHC or ISH or both are carried out. After evaluating the stained slides and corresponding results are sent back from the participating center to the QuIP. The QuIP then evaluates the section preparations with regard to staining quality and result accuracy.
Survey on HER2 test methodology
Tumor specimens from 105 pathology institutes were sent to the central pathology. All participating pathologists were asked to complete a questionnaire containing information about the tumor tissue (biopsy versus resection specimen; primary tumor versus metastatic site), their participation in round robin tests, and the applied HER2 test method. We asked specifically for the following antibodies for IHC: HercepTest and A0485 (Dako, Glostrup, Denmark), SP3 (Labvision; Thermo Fisher Scientific, Fremont, CA, United States), 4B5 (Ventana Medical Systems, Tucson, AZ, United States), CB11 (Novocastra, Newcastle upon Tyne, Great Britain), UMAB36 (OriGene Technologies, Rockville, United States), and EP3 (Cell Marque, Rocklin, United States).
Statistical methods
Stratification into groups was done according to central and local HER2 test results: HER2 +/HER2 + (central HER2 +/local HER2 +), HER2 +/HER2 − (central HER2 +/local HER2 −), HER2 −/HER2 + (central HER2 −/local HER2 +) and HER2 − /HER2 − (central HER2 −/local HER2 −). Comparative analysis such as sex, initial tumor stage, prior gastric surgery, tumor location, and histopathological subtype according to Laurén’s classification of the different patient cohorts (HER2 + /HER2 + vs. HER2 −/HER2 +) was carried out using the Chi2 test. P < 0.05 was considered statistically significant. Analyses were done with IBM SPSS version 24.0 (IBM Corp., Armonk, NY).
Results
Patient groups
Tumor tissue for central HER2 testing was available for 521 of 548 enrolled patients (Fig. 1). In 404 patients, HER2 status was determined in local and central pathology institutes. In local HER2 testing, 148 out of those 404 patients were rated HER2 positive. The central result differed in particular in the initially IHC3 + tested patients.
Of these 404 patients, 373 patients received first-line therapy and basis documentation was obtained. They were assigned to the four groups HER2 +/HER2 − (n = 9), HER2 + /HER2 + (n = 68; Fig. 1 green), HER2 −/HER2 + (n = 68; Fig. 1 blue), and HER2-/HER2- (n = 220).
Tumor phenotype and localization
Diffuse subtype was less common in the HER2 + /HER2 + versus the HER2 −/HER2 + cohort [5.9% (n = 4) vs. 23.5% (n = 16); p = 0.004]. Laurén´s classification is unknown in a significant proportion of the confirmed and unconfirmed cohorts [39.0% (n = 53)]. Tumor localization was significantly different between the HER2 + /HER2 + and HER2 −/HER2 + cohorts (Table 1). More patients with EGJC were found in the HER2 + /HER2 + group [69.1% (n = 47)], while more GC patients were allocated in the HER2 −/HER2 + group [58.8% (n = 40); p = 0.001]. Centrally confirmed HER2 positivity rate was higher for EGJC (29.4%) and low for GC (10.8%).
There was no difference between the groups regarding local IHC testing (IHC2 + vs. IHC3 +).
Looking at the whole cohort (see Suppl. 1), there is a generally increased occurrence of EGJC in the HER2-positive cohort (p < 0.00001). With regard to the histological subtype, the assessment was not possible due to a high rate of missing information. However, there is the tendency of the increase in the intestinal and the decrease of the diffuse type in the HER2-positive cohort.
HER2 test results
The following analysis of the test results refers to different sub-groups as detailed in the consort diagram (Fig. 1). For better comprehensibility, there is a modified scheme in the supplements (see Suppl. 2).
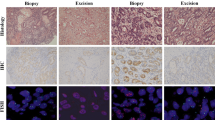
89 (17.1%) of 521 centrally analyzed tumor samples were HER2 + , with an IHC3 + in 70 patients and IHC2 + /ISH + in 19 patients. In 90 of the 404 (22.3%) patients with local and central HER2 test results, local HER2 status was not confirmed. The discordance of IHC results between central and local pathologies is shown in Fig. 2. The analysis included patients for whom a central test result and a concrete local IHC score were available. There was a particularly high discordance in samples scored HER2 IHC3 + locally (Fig. 2c, f) with only 57 samples (46.0%) confirming local HER2 + in the central laboratory.
Comparison of local and central HER2 immunohistochemistry (IHC) scores and corresponding central in situ hybridization (ISH). HER2/CEP17 ratio ≥ 2 indicates HER2 positivity and is shown as orange line. a Tumor samples tested HER2 negative (IHC0/1) by local laboratories (n = 178) are shown. In these probes, central HER2 test was negative in 86.5% (IHC0 (n = 124); IHC1 (n = 30)); 10.7% were scored IHC2 + (n = 19) and 2.8% IHC3 + (n = 5). Corresponding central ISH results are shown in d with 5 of 166 tumors showing a HER2/CEP17 ratio ≥ 2. b Tumor samples with local IHC2 + tests (n = 38). Corresponding central IHC reveals an IHC score 0 in 39.5% (n = 15), IHC1 in 23.7% (n = 9), IHC2 in 28.9% (n = 11), and IHC3 in 7.9% (n = 3). Corresponding central ISH is shown in e with 5 of 35 samples showing an HER2/CEP17 ratio > 2. c Tumor samples with IHC3 + in the local laboratory (n = 124) are shown. Corresponding central IHC results are shown with negative HER2 in 35.5% (IHC0, n = 32 and IHC1, n = 12). 25.0% revealed intermediate HER2 expression (IHC2 + (n = 31)) of which 25.8% (n = 8) were confirmed HER2 + in central ISH (HER2/CEP17 ratio > 2). 39.5% confirmed IHC3 + (n = 49) in central IHC. Corresponding central ISH is shown in f with 57 of 112 samples showing a HER2/CEP17 ratio > 2
Central HER2 ISH analysis was performed in 481 of 521 samples. Concordance between ISH and IHC results was 98.3% (473 of 481 tests). The eight discordant cases were two with positive HER2 IHC3 + but HER2/CEP17 ratio < 2.0 and six with HER2 IHC0/1 and HER2/CEP17 ratio ≥ 2.0 resulting in a sensitivity of 93.3% (84 IHC + of 90 ISH +) and a specificity of 99.5% (389 IHC- of 391 ISH-) and a positive diagnosis rate of 97.7%.
HER2 test platforms
In local pathology laboratories, HercepTest [n = 23 (21.9%)] and 4B5 [n = 19 (18.1%)] were the most commonly used antibodies. Rarely applied antibodies were clones SP3 [n = 10 (9.5%)], CB11 [n = 6 (5.7%)], UMAB36 [n = 6 (5.7%)], A0485 [n = 11 (10.5%)], and EP3 [n = 6 (5.7%)]. 46 of 105 pathology laboratories (43.8%) participated in round robin tests, 25 (23.8%) did not participate, and for 34 (32.4%) participation is unknown despite repeated queries. No associations between HER2 test deviations and the applied IHC antibody (Fig. 3a) or participation in round robin tests on HER2 test deviations were demonstrated (Fig. 3b).
HER2 test platform in routine use. a Antibody used for local HER2 IHC, shown for the HER2 + /HER2 + (green, n = 68) and the HER2-/HER2 + (blue, n = 68) cohorts. b Participation in round robin tests for HER2 in GC, shown for the HER2 + /HER2 + (green, n = 68) and HER2-/HER2 + (blue, n = 68) cohorts; The Chi2 test did not show any significant differences
Tumor material
The majority of tested tumor specimens was from primary biopsies (Fig. 4) followed by resection specimens or metastases, with no significant difference between the groups HER2 + /HER2 + and HER2 −/HER2 + . In 80.3% of the patients, tumor specimens originating from the same location (endoscopic biopsy of the primary tumor, or resection specimen, or biopsy from metastases) were tested for HER2 in both the central and local pathology laboratories (comparable cases, n = 390). For HER2 + /HER2 + and HER2-/HER2 + patients, this concordance of examined tumor specimens was comparable (83.8% vs. 85.3%, respectively).
Discussion
The VARIANZ study has shown that GC patients with deviating HER2 test results had no benefit from HER2-targeted treatment with trastuzumab (Haffner et al. 2021). We wanted to understand the underlying causes for HER2 deviations. Our analyses demonstrates that neither the antibody platform used for immunohistochemistry (IHC) nor participation in round robin tests of local pathology institutes correlated with the HER2 test deviation rate. In contrast, we found that tumor characteristics such as primary tumor location and phenotype had an impact on test deviations: more HER2 test deviations were seen in distal GC compared to EGJC as well as in the diffuse versus intestinal subtype according to Laurén’s classification.
HER2 heterogeneity is common in GC, even in early stages (Kanayama et al. 2018). There is no generally agreed definition for HER2 heterogeneity in gastric cancer. Some authors use the relative number of HER2 + stained tumor cells, but thresholds vary from < 30% (van Cutsem et al. 2015), < 40% (Haffner et al. 2021), to < 60% (Kanayama et al. 2018; Wang et al. 2014) or even < 100% tumor cells stained HER2-positive (Wakatsuki et al. 2018; Yagi et al. 2019). Other authors determined HER2 heterogeneity by deviating HER2 status in a set of primary biopsies (Kaito et al. 2019), of resection specimen (Xu et al. 2019) or in paired specimens from the primary tumor and metastasis (Peng et al. 2015). Although HER2 heterogeneity in gastric cancer has no commonly agreed definition, it is associated with limited trastuzumab benefit and decreased overall survival in trastuzumab-treated patients, as was suggested by several groups (Haffner et al. 2021; Kaito et al. 2019; Wakatsuki et al. 2018). We conclude that for distal gastric cancer location and for the diffuse subtype where HER2 positivity in general is less common (Baretton et al. 2019; He et al. 2015; Huang et al. 2013; Koopman et al. 2015; van Cutsem et al. 2015; Yoon et al. 2012; Barros-Silva et al. 2009; Cappellesso et al. 2015; Cho et al. 2013; Chua and Merrett 2012; Gomez-Martin et al. 2013; Gómez-Martin et al. 2012; Grabsch et al. 2010) weak HER2 expression and intratumoral heterogeneity account for more deviating test results.
Strengths of the presented investigation are the reporting of the centrally performed standardized HER2 tests by both IHC and ISH for all received specimens. Furthermore, we established a large prospective multicenter cohort with valid clinical data in a real-world setting.
Nevertheless, a limitation of our study might be the central use of the HER2-antibody CB11 for IHC, which is not as widely used as the 4B5 clone and the HercepTest. Although less sensitivity was seen for CB11, this clone presented the highest specificity compared to HercepTest and others (Asioli et al. 2012; Cappellesso et al. 2015; Cho et al. 2012; Grillo et al. 2013). In our own study, test results obtained by CB11 were associated with a survival advantage in trastuzumab-treated patients (Haffner et al. 2021). In addition, high concordance between ISH and IHC with CB11 was seen in the VARIANZ (98.3%) and other studies (Barros-Silva et al. 2009; Cho et al. 2012). Nevertheless, for further examination of local and central HER2 determination, the use of a second antibody should be considered as well as application of an automatized scoring system might be considered. Another limitation is that a significant number of local laboratories provided neither specification of the applied antibodies nor information on participation in quality assurance programs such as round robin tests. Finally, central HER2 determination was not necessarily performed on the same tumor block as it was done in local laboratories which adds to the complexity of achieving concordant diagnosis.
Deviating central and local HER2 reports were already reported for various gastric cancer cohorts (Byeon et al. 2017; Huemer et al. 2020; Monges-Ranchin et al. 2016; Press et al. 2017). Discordant results are particularly often found in patients tested locally HER2 + (Haffner et al. 2021; Huemer et al. 2020; Janjigian et al. 2020). Patients with centrally confirmed HER2 + status treated with trastuzumab showed better survival outcomes (Haffner et al. 2021; Huemer et al. 2020). We conclude that a central confirmation of the HER2 status is a correlate of lower HER2 heterogeneity which is an indicator for better treatment efficacy with an anti-HER2-targeted drug such as trastuzumab.
Identification of HER2 + in gastric and EGJ cancer patients remains an important step in the management of patients with advanced GC and EGJC, but is still challenging. Adaption of HER2 thresholds to identify patients benefiting from trastuzumab treatment has been already postulated (Gomez-Martin et al. 2013; Haffner et al. 2021). Our data suggest that only patients with low HER2 heterogeneity may benefit from trastuzumab treatment. Selection of patients with low HER2 heterogeneity, defined as confirmed HER2 + status in paired specimen, might improve survival outcomes with targeted treatment, prevent overtreatment and associated side effects and costs, and may enable successful studies of other promising HER2-targeting drugs.
Data availability
Not applicable.
Code availability
Not applicable.
References
Abrahão-Machado LF, Jácome AAdA, Wohnrath DR, dos Santos JS, Carneseca EC, Fregnani JHTG, Scapulatempo-Neto C (2013) HER2 in gastric cancer: comparative analysis of three different antibodies using whole-tissue sections and tissue microarrays. World J Gastroenterol 19:6438–6446. https://doi.org/10.3748/wjg.v19.i38.6438
Asioli S, Maletta F, Di Verdun CL, Satolli MA, Schena M, Pecchioni C, Botta C, Chiusa L, Molinaro L, Conti L, Viale G, Ingravallo G, Maiorano E, Sapino A (2012) Approaching heterogeneity of human epidermal growth factor receptor 2 in surgical specimens of gastric cancer. Hum Pathol 43:2070–2079. https://doi.org/10.1016/j.humpath.2012.02.017
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Rüschoff J, Kang YK, ToGA Trial Investigators (2010a) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 376(9742):687–697
Bang Y-J, van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, Aprile G, Kulikov E, Hill J, Lehle M, Rüschoff J, Kang Y-K (2010b) Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. The Lancet 376:687–697. https://doi.org/10.1016/S0140-6736(10)61121-X
Bang YJ, Giaccone G, Im SA, Oh DY, Bauer TM, Nordstrom JL, Li H, Chichili GR, Moore PA, Hong S, Stewart SJ, Baughman JE, Lechleider RJ, Burris HA (2017) First-in-human phase 1 study of margetuximab (MGAH22), an Fc-modified chimeric monoclonal antibody, in patients with HER2-positive advanced solid tumors. Ann Oncol 28:855–861. https://doi.org/10.1093/annonc/mdx002
Baretton G, Kreipe HH, Schirmacher P, Gaiser T, Hofheinz R, Berghäuser K-H, Koch W, Künzel C, Morris S, Rüschoff J (2019) HER2 testing in gastric cancer diagnosis: insights on variables influencing HER2-positivity from a large, multicenter, observational study in Germany. Virchows Arch 474:551–560. https://doi.org/10.1007/s00428-019-02541-9
Barros-Silva JD, Leitão D, Afonso L, Vieira J, Dinis-Ribeiro M, Fragoso M, Bento MJ, Santos L, Ferreira P, Rêgo S, Brandão C, Carneiro F, Lopes C, Schmitt F, Teixeira MR (2009) Association of ERBB2 gene status with histopathological parameters and disease-specific survival in gastric carcinoma patients. Br J Cancer 100:487–493. https://doi.org/10.1038/sj.bjc.6604885
Boers JE, Meeuwissen H, Methorst N (2011) HER2 status in gastro-oesophageal adenocarcinomas assessed by two rabbit monoclonal antibodies (SP3 and 4B5) and two in situ hybridization methods (FISH and SISH). Histopathology 58:383–394. https://doi.org/10.1111/j.1365-2559.2011.03760.x
Bozzetti C, Negri FV, Lagrasta CA, Crafa P, Bassano C, Tamagnini I, Gardini G, Nizzoli R, Leonardi F, Gasparro D, Camisa R, Cavalli S, Capelli S, Silini EM, Ardizzoni A (2011) Comparison of HER2 status in primary and paired metastatic sites of gastric carcinoma. Br J Cancer 104:1372–1376. https://doi.org/10.1038/bjc.2011.121
Byeon S-J, Lee HS, Kim M-A, Lee BL, Kim WH (2017) Expression of the ERBB family of ligands and receptors in gastric cancer. Pathobiology 84:210–217. https://doi.org/10.1159/000464250
Cappellesso R, Fassan M, Hanspeter E, Bornschein J, d’Amore ESG, Cuorvo LV, Mazzoleni G, Barbareschi M, Pizzi M, Guzzardo V, Malfertheiner P, Micev M, Guido M, Giacomelli L, Tsukanov VV, Zagonel V, Nitti D, Rugge M (2015) HER2 status in gastroesophageal cancer: a tissue microarray study of 1040 cases. Hum Pathol 46:665–672. https://doi.org/10.1016/j.humpath.2015.02.007
Cho EY, Srivastava A, Park K, Kim J, Lee MH, Do I, Lee J, Kim K-M, Sohn TS, Kang WK, Kim S (2012) Comparison of four immunohistochemical tests and FISH for measuring HER2 expression in gastric carcinomas. Pathology 44:216–220. https://doi.org/10.1097/PAT.0b013e3283513e8b
Cho J, Jeong J, Sung J, Sung CO, Kim K-M, Park CK, Choi MG, Sohn TS, Bae JM, Kim S (2013) A large cohort of consecutive patients confirmed frequent HER2 positivity in gastric carcinomas with advanced stages. Ann Surg Oncol 20(3):S477–S484. https://doi.org/10.1245/s10434-012-2818-0
Chua TC, Merrett ND (2012) Clinicopathologic factors associated with HER2-positive gastric cancer and its impact on survival outcomes–a systematic review. Int J Cancer 130:2845–2856. https://doi.org/10.1002/ijc.26292
Dijksterhuis WPM, Verhoeven RHA, Meijer SL, Slingerland M, Haj Mohammad N, de Vos-Geelen J, Beerepoot LV, van Voorthuizen T, Creemers G-J, van Oijen MGH, van Laarhoven HWM (2020) Increased assessment of HER2 in metastatic gastroesophageal cancer patients: a nationwide population-based cohort study. Gastric Cancer. https://doi.org/10.1007/s10120-020-01039-7
Fu X, Zhang Y, Yang J, Qi Y, Ming Y, Sun M, Shang Y, Yang Y, Zhu X, Gao Q (2018) Efficacy and safety of trastuzumab as maintenance or palliative therapy in advanced HER2-positive gastric cancer. Onco Targets Ther 11:6091–6100. https://doi.org/10.2147/OTT.S174138
Gómez-Martin C, Garralda E, Echarri MJ, Ballesteros A, Arcediano A, Rodríguez-Peralto JL, Hidalgo M, López-Ríos F (2012) HER2/neu testing for anti-HER2-based therapies in patients with unresectable and/or metastatic gastric cancer. J Clin Pathol 65:751–757. https://doi.org/10.1136/jclinpath-2012-200774
Gomez-Martin C, Plaza JC, Pazo-Cid R, Salud A, Pons F, Fonseca P, Leon A, Alsina M, Visa L, Rivera F, Galan MC, Del Valle E, Vilardell F, Iglesias M, Fernandez S, Landolfi S, Cuatrecasas M, Mayorga M, Jose Paulés M, Sanz-Moncasi P, Montagut C, Garralda E, Rojo F, Hidalgo M, Lopez-Rios F (2013) Level of HER2 gene amplification predicts response and overall survival in HER2-positive advanced gastric cancer treated with trastuzumab. J Clin Oncol 31:4445–4452. https://doi.org/10.1200/JCO.2013.48.9070
Grabsch H, Sivakumar S, Gray S, Gabbert HE, Müller W (2010) HER2 expression in gastric cancer: Rare, heterogeneous and of no prognostic value—conclusions from 924 cases of two independent series. Cell Oncol 32:57–65. https://doi.org/10.3233/CLO-2009-0497
Grillo F, Fassan M, Ceccaroli C, Giacometti C, Curto M, Zagonel V, Ceppa P, Nitti D, Castoro C, Fiocca R, Rugge M, Mastracci L (2013) The reliability of endoscopic biopsies in assessing HER2 status in gastric and gastroesophageal junction cancer: a study comparing biopsies with surgical samples. Transl Oncol 6:10–16. https://doi.org/10.1593/tlo.12334
Haffner I, Schierle K, Raimúndez E, Geier B, Maier D, Hasenauer J, Luber B, Walch A, Kolbe K, Riera Knorrenschild J, Kretzschmar A, Rau B, Fischer von Weikersthal L, Ahlborn M, Siegler G, Fuxius S, Decker T, Wittekind C, Lordick F (2021) HER2 expression, test deviations, and their impact on survival in metastatic gastric cancer: results from the prospective multicenter VARIANZ study. J Clin Oncol 39:1468–1478. https://doi.org/10.1200/JCO.20.02761
He XX, Ding L, Lin Y, Shu M, Wen JM, Xue L (2015) Protein expression of HER2, 3, 4 in gastric cancer: correlation with clinical features and survival. J Clin Pathol 68:374–380. https://doi.org/10.1136/jclinpath-2014-202657
Hecht JR, Bang Y-J, Qin SK, Chung HC, Xu JM, Park JO, Jeziorski K, Shparyk Y, Hoff PM, Sobrero A, Salman P, Li J, Protsenko SA, Wainberg ZA, Buyse M, Afenjar K, Houé V, Garcia A, Kaneko T, Huang Y, Khan-Wasti S, Santillana S, Press MF, Slamon D (2016) Lapatinib in combination with capecitabine plus oxaliplatin in human epidermal growth factor receptor 2-positive advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma: TRIO-013/LOGiC–A randomized phase III trial. J Clin Oncol 34:443–451. https://doi.org/10.1200/JCO.2015.62.6598
Hofmann M, Stoss O, Shi D, Büttner R, van de Vijver M, Kim W, Ochiai A, Rüschoff J, Henkel T (2008) Assessment of a HER2 scoring system for gastric cancer: results from a validation study. Histopathology 52:797–805. https://doi.org/10.1111/j.1365-2559.2008.03028.x
Huang D, Lu N, Fan Q, Sheng W, Bu H, Jin X et al (2013) HER2 status in gastric and gastroesophageal junction cancer assessed by local and central laboratories: Chinese results of the HER-EAGLE study. PloS one 8(11): e80290. https://doi.org/10.1371/journal.pone.0080290
Huang S-C, Ng K-F, Lee S-E, Chen K-H, Yeh T-S, Chen T-C (2016) HER2 testing in paired biopsy and excision specimens of gastric cancer: the reliability of the scoring system and the clinicopathological factors relevant to discordance. Gastric Cancer 19:176–182. https://doi.org/10.1007/s10120-014-0453-0
Huemer F, Weiss L, Regitnig P, Winder T, Hartmann B, Thaler J, Piringer G, Schmitt CA, Eisterer W, Gänzer H, Wüstner A, Andel J, Jagdt B, Ulmer H, Greil R, Wöll E (2020) Local and central evaluation of HER2 positivity and clinical outcome in advanced gastric and gastroesophageal cancer-results from the AGMT GASTRIC-5 registry. J Clin Med. https://doi.org/10.3390/jcm9040935
Janjigian YY, Maron SB, Chatila WK, Millang B, Chavan SS, Alterman C, Chou JF, Segal MF, Simmons MZ, Momtaz P, Shcherba M, Ku GY, Zervoudakis A, Won ES, Kelsen DP, Ilson DH, Nagy RJ, Lanman RB, Ptashkin RN, Donoghue MTA, Capanu M, Taylor BS, Solit DB, Schultz N, Hechtman JF (2020) First-line pembrolizumab and trastuzumab in HER2-positive oesophageal, gastric, or gastro-oesophageal junction cancer: an open-label, single-arm, phase 2 trial. Lancet Oncol 21:821–831. https://doi.org/10.1016/S1470-2045(20)30169-8
Kaito A, Kuwata T, Tokunaga M, Shitara K, Sato R, Akimoto T, Kinoshita T (2019) HER2 heterogeneity is a poor prognosticator for HER2-positive gastric cancer. World J Clin Cases 7:1964–1977. https://doi.org/10.12998/wjcc.v7.i15.1964
Kanayama K, Imai H, Usugi E, Shiraishi T, Hirokawa YS, Watanabe M (2018) Association of HER2 gene amplification and tumor progression in early gastric cancer. Virchows Arch 473:559–565. https://doi.org/10.1007/s00428-018-2433-y
Kim T-Y, Han HS, Lee K-W, Zang DY, Rha SY, Park YI, Kim J-S, Lee K-H, Park SH, Song E-K, Jung S-A, Lee N, Kim YH, Cho JY, Bang Y-J (2019) A phase I/II study of poziotinib combined with paclitaxel and trastuzumab in patients with HER2-positive advanced gastric cancer. Gastric Cancer 22:1206–1214. https://doi.org/10.1007/s10120-019-00958-4
Koopman T, Louwen M, Hage M, Smits MM, Imholz ALT (2015) Pathologic diagnostics of HER2 positivity in gastroesophageal adenocarcinoma. Am J Clin Pathol 143:257–264. https://doi.org/10.1309/AJCPCX69HGDDGYCQ
Leni A, Barresi V, Caltabiano R, Caleo A, Bonetti LR, Lanzafame S, Zeppa P, Caruso RA, Tuccari G (2014) Discordance rate of HER2 status in primary gastric carcinomas and synchronous lymph node metastases: a multicenter retrospective analysis. Int J Mol Sci 15:22331–22341. https://doi.org/10.3390/ijms151222331
Lordick F, Janjigian YY (2016) Clinical impact of tumour biology in the management of gastroesophageal cancer. Nat Rev Clin Oncol 13:348–360. https://doi.org/10.1038/nrclinonc.2016.15
Monges-Ranchin G, Terris B, Chenard M-P, Bibeau F, Penault-Llorca FM, Bougrini M, Da Silva C, Fraga E, Doucet L (2016) Concordance of HER2 status between local and central review in gastric and gastroesophageal junction cancers: a French observational study of 394 specimens (HERable study). JCO 34:30. https://doi.org/10.1200/jco.2016.34.4_suppl.30
Peng Z, Zou J, Zhang X, Yang Y, Gao J, Li Y, Li Y, Shen L (2015) HER2 discordance between paired primary gastric cancer and metastasis: a meta-analysis. Chin J Cancer Res 27:163–171. https://doi.org/10.3978/j.issn.1000-9604.2014.12.09
Press MF, Ellis CE, Gagnon RC, Grob TJ, Buyse M, Villalobos I, Liang Z, Wu S, Bang Y-J, Qin S-K, Chung HC, Xu J, Park JO, Jeziorski K, Afenjar K, Ma Y, Estrada MC, Robinson DM, Scherer SJ, Sauter G, Hecht JR, Slamon DJ (2017) HER2 status in advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma for entry to the TRIO-013/LOGiC trial of lapatinib. Mol Cancer Ther 16:228–238. https://doi.org/10.1158/1535-7163.MCT-15-0887
Radu OM, Foxwell T, Cieply K, Navina S, Dacic S, Nason KS, Davison JM (2012) HER2 amplification in gastroesophageal adenocarcinoma: correlation of two antibodies using gastric cancer scoring criteria, H score, and digital image analysis with fluorescence in situ hybridization. Am J Clin Pathol 137:583–594. https://doi.org/10.1309/AJCPXQVS6YGHPDCY
Rüschoff J, Dietel M, Baretton G, Arbogast S, Walch A, Monges G, Chenard M-P, Penault-Llorca F, Nagelmeier I, Schlake W, Höfler H, Kreipe HH (2010) HER2 diagnostics in gastric cancer-guideline validation and development of standardized immunohistochemical testing. Virchows Arch 457:299–307. https://doi.org/10.1007/s00428-010-0952-2
Rüschoff J, Hanna W, Bilous M, Hofmann M, Osamura RY, Penault-Llorca F, van de Vijver M, Viale G (2012) HER2 testing in gastric cancer: a practical approach. Mod Pathol 25:637–650. https://doi.org/10.1038/modpathol.2011.198
Satoh T, Xu R-H, Chung HC, Sun G-P, Doi T, Xu J-M, Tsuji A, Omuro Y, Li J, Wang J-W, Miwa H, Qin S-K, Chung I-J, Yeh K-H, Feng J-F, Mukaiyama A, Kobayashi M, Ohtsu A, Bang Y-J (2014) Lapatinib plus paclitaxel versus paclitaxel alone in the second-line treatment of HER2-amplified advanced gastric cancer in Asian populations: TyTAN–a randomized, phase III study. J Clin Oncol 32:2039–2049. https://doi.org/10.1200/JCO.2013.53.6136
Schrohl A-S, Pedersen HC, Jensen SS, Nielsen SL, Brünner N (2011) Human epidermal growth factor receptor 2 (HER2) immunoreactivity: specificity of three pharmacodiagnostic antibodies. Histopathology 59:975–983. https://doi.org/10.1111/j.1365-2559.2011.04034.x
Shah MA, Khanin R, Tang L, Janjigian YY, Klimstra DS, Gerdes H, Kelsen DP (2011) Molecular classification of gastric cancer: a new paradigm. Clin Cancer Res 17:2693–2701. https://doi.org/10.1158/1078-0432.CCR-10-2203
Shitara K, Bang Y-J, Iwasa S, Sugimoto N, Ryu M-H, Sakai D, Chung H-C, Kawakami H, Yabusaki H, Lee J, Saito K, Kawaguchi Y, Kamio T, Kojima A, Sugihara M, Yamaguchi K (2020) Trastuzumab deruxtecan in previously treated HER2-positive gastric cancer. N Engl J Med 382:2419–2430. https://doi.org/10.1056/NEJMoa2004413
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30. https://doi.org/10.3322/caac.21442
Smyth EC, Nilsson M, Grabsch HI, van Grieken NCT, Lordick F (2020) Gastric cancer. The Lancet 396:635–648. https://doi.org/10.1016/S0140-6736(20)31288-5
Tabernero J, Hoff PM, Shen L, Ohtsu A, Shah MA, Cheng K, Song C, Wu H, Eng-Wong J, Kim K, Kang Y-K (2018) Pertuzumab plus trastuzumab and chemotherapy for HER2-positive metastatic gastric or gastro-oesophageal junction cancer (JACOB): final analysis of a double-blind, randomised, placebo-controlled phase 3 study. Lancet Oncol 19:1372–1384. https://doi.org/10.1016/S1470-2045(18)30481-9
Thuss-Patience PC, Shah MA, Ohtsu A, van Cutsem E, Ajani JA, Castro H, Mansoor W, Chung HC, Bodoky G, Shitara K, Phillips GDL, van der Horst T, Harle-Yge M-L, Althaus BL, Kang Y-K (2017) Trastuzumab emtansine versus taxane use for previously treated HER2-positive locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma (GATSBY): an international randomised, open-label, adaptive, phase 2/3 study. Lancet Oncol 18:640–653. https://doi.org/10.1016/S1470-2045(17)30111-0
van Cutsem E, Bang Y-J, Feng-Yi F, Xu JM, Lee K-W, Jiao S-C, Chong JL, López-Sanchez RI, Price T, Gladkov O, Stoss O, Hill J, Ng V, Lehle M, Thomas M, Kiermaier A, Rüschoff J (2015) HER2 screening data from ToGA: targeting HER2 in gastric and gastroesophageal junction cancer. Gastric Cancer 18:476–484. https://doi.org/10.1007/s10120-014-0402-y
Wakatsuki T, Yamamoto N, Sano T, Chin K, Kawachi H, Takahari D, Ogura M, Ichimura T, Nakayama I, Osumi H, Matsushima T, Suenaga M, Shinozaki E, Hiki N, Ishikawa Y, Yamaguchi K (2018) Clinical impact of intratumoral HER2 heterogeneity on trastuzumab efficacy in patients with HER2-positive gastric cancer. J Gastroenterol 53:1186–1195. https://doi.org/10.1007/s00535-018-1464-0
Wang T, Hsieh ET, Henry P, Hanna W, Streutker CJ, Grin A (2014) Matched biopsy and resection specimens of gastric and gastroesophageal adenocarcinoma show high concordance in HER2 status. Hum Pathol 45:970–975. https://doi.org/10.1016/j.humpath.2013.12.010
Xu C, Liu Y, Jiang D, Ge X, Huang J, Su J, Zhang X, Lu S, Ji Y, Hou J, Liu T, Hou Y (2019) Late stage gastric cancer patients with extra gained HER2 positivity by dual block assessment may not show compromised efficacy to trastuzumab treatment. Aging 11:10052–10060. https://doi.org/10.18632/aging.102415
Yagi S, Wakatsuki T, Yamamoto N, Chin K, Takahari D, Ogura M, Ichimura T, Nakayama I, Osumi H, Shinozaki E, Suenaga M, Fujisaki J, Ishikawa Y, Yamaguchi K, Namikawa K, Horiuchi Y (2019) Clinical significance of intratumoral HER2 heterogeneity on trastuzumab efficacy using endoscopic biopsy specimens in patients with advanced HER2 positive gastric cancer. Gastric Cancer 22:518–525. https://doi.org/10.1007/s10120-018-0887-x
Yang J, Luo H, Li Y, Li J, Cai Z, Su X, Dai D, Du W, Chen T, Chen M (2012) Intratumoral heterogeneity determines discordant results of diagnostic tests for human epidermal growth factor receptor (HER) 2 in gastric cancer specimens. Cell Biochem Biophys 62:221–228. https://doi.org/10.1007/s12013-011-9286-1
Yi JH, Kang JH, Hwang IG, Ahn HK, Baek HJ, Lee SI, Lim DH, Won Y-W, Ji JH, Kim HS, Rha SY, Oh SY, Lee KE, Lim T, Maeng CH, Kim MJ, Kim ST, Lee J, Park JO, Park YS, Lim HY, Kang WK, Park SH (2016) A retrospective analysis for patients with HER2-positive gastric cancer who were treated with trastuzumab-based chemotherapy: in the perspectives of ethnicity and histology. Cancer Res Treat 48:553–560. https://doi.org/10.4143/crt.2015.155
Yoon HH, Shi Q, Sukov WR, Wiktor AE, Khan M, Sattler CA, Grothey A, Wu T-T, Diasio RB, Jenkins RB, Sinicrope FA (2012) Association of HER2/ErbB2 expression and gene amplification with pathologic features and prognosis in esophageal adenocarcinomas. Clin Cancer Res 18:546–554. https://doi.org/10.1158/1078-0432.CCR-11-2272
Funding
Open Access funding enabled and organized by Projekt DEAL. VARIANZ was supported by the German Federal Ministry for Education and Research (BMBF grants 01ZX1310A, 01ZX1310B; 01ZX1310D and 01ZX1310E, 01ZX1610E).
Author information
Authors and Affiliations
Contributions
Conception and design: KK, IH, BL, and FL. Administrative support, sampling of data, and evaluation of tumor specimen: KK, IH, KS, BL, DM, BG, HB, CW, and FL. Writing of the manuscript: KK, IH, and FL. Reviewing and final approval of the manuscript: KK, IH, KS, BL, DM, BG, HB, CW, and FL.
Corresponding author
Ethics declarations
Conflict of interest
All authors have completed a COI form.
Ethical approval
Ethical approval was granted by the University of Leipzig Research Ethics Board (080-14-10032014). VARIANZ was registered at clinicaltrials.gov with registration number NCT02305043.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kolbe, K., Haffner, I., Schierle, K. et al. Deviating HER2 test results in gastric cancer: analysis from the prospective multicenter VARIANZ study. J Cancer Res Clin Oncol 149, 1319–1329 (2023). https://doi.org/10.1007/s00432-022-04208-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04208-6