Abstract
Background
The use of immune checkpoint inhibitors (ICI) has transformed cancer treatment. Subsequent ICI use has become increasingly common following disease progression. We aim to evaluate the safety and tolerability of the sequential ICI treatment modality.
Methods
Retrospective review of confirmed carcinoma from January 2014 to December 2018. Patients were categorized into “initial ICI arm” and “sequential ICI arm” defined as patients receiving single, dual or chemo-immunotherapy ICI following an initial ICI regimen. Primary outcome was the development of a new or recurrent immune related adverse event (irAE) during sequential therapy. Secondary outcomes were the number of cycles prior to the development of irAE and grade of irAE.
Results
A total of 483 patients received ICI during the timeframe. Of those, 22 patients received sequential ICI. The diagnoses included ten lung cancer, seven melanoma, four renal cell carcinoma and one bladder cancer. 16 patients received single agent ICI following the initial ICI, three patients received dual ICI following the initial ICI, one patient received chemotherapy-immunotherapy following initial ICI, and two patients received chemo-immunotherapy after dual ICI. Four patients developed new irAE and one patient developed the same irAE on sequential treatment. A higher proportion of patients experienced grade 3 irAE in the sequential arm compared to the initial ICI arm (p = 0.03). No statistical difference was found between the development of irAE and the number of cycles prior to development of irAE in either treatment groups (p = 0.5).
Conclusion
Our data shows overall safety of sequencing ICI when close monitoring was employed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of immune checkpoint inhibitors (ICI) has transformed cancer treatment and has become a regular treatment option for many oncologists. ICI’s stimulate the immune system’s antitumor response and suppress the cytotoxic T-lymphocyte antigen-4 (CTLA-4), programmed cell death 1, or ligand 1 (PD-1/PDL-1) (Larkin et al. 2019). Presently, ICI treatment is FDA approved to treat many types and stages of malignancies including colorectal cancer, pleural mesothelioma, breast cancer, bladder cancer, endometrial carcinoma, esophageal squamous cell carcinoma, lung cancer, renal cell carcinoma, Merkel cell carcinoma, hepatocellular carcinoma, lymphoma, cervical cancer, gastric cancer, head and neck cancer, and urothelial carcinoma (Twomey and Zhang 2021). ICI utilization has greatly increased due to the clinical benefits and significant improvements in progression free survival and overall survival (Postow et al. 2015). Different treatment strategies with sequential and combination ICI are being investigated and have shown to be effective with a higher immunogenic effect compared to single agent ICI in certain cancers (Winer et al. 2019; Curran et al. 2010).
The significant benefits of ICI must be weighed against their toxicities, most notably immune related adverse events (irAEs) (Gunturu et al. 2022). Any organ can be affected by irAEs and they occur with varying degrees of severity. Generally, treatment with ICI can continue with grade 1 irAEs with close monitoring. Grade 2 irAEs may warrant temporary discontinuation of ICI until toxicity reverts to grade 1 or less, and irAEs above grade 2 generally warrant suspension or permanent discontinuation of ICI therapy (Brahmer et al. 2018) in addition to corticosteroids or other immune suppressing medications. Data on the safety and efficacy of ICI in patients who previously develop irAEs has been extensively reported (Zhao et al. 2021). Following disease progression on ICI, the use of a subsequent ICI has become increasingly common for patients with severe disease, but the safety and efficacy of sequential therapy have not been well studied.
We conducted a retrospective review of patients who received a second ICI treatment either as a monotherapy or in combination with another ICI or chemotherapy and evaluated the safety and tolerability of sequential treatment modality.
Methods
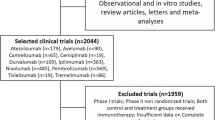
This was a retrospective study that included all patients with a histology-confirmed carcinoma who received subsequent ICI following initial ICI therapy. ICI regimens included anti-CTLA-4 (ipilimumab), anti-PD1/PDL1 (nivolumab, pembrolizumab, durvalumab, atezolizumab), dual anti-CTLA-4 and anti-PD-L1 (ipilimumab and nivolumab) or chemotherapy-ICI combination between January 1, 2014 and December 18, 2018. We collected baseline patients and tumor characteristics, details of the ICI regimen used and irAEs data. Prior to initiating the study, approval was obtained from the Beth Israel Lahey Health Institutional Review Board.
We defined and graded the severity of irAEs according to the Common Terminology Criteria for Adverse Events Version 4.0. We categorized patients into “Initial ICI” arm and “Sequential ICI” arm defined as patients receiving a second ICI either as a single, dual ICI or a chemotherapy-ICI combination. Common side effects included skin toxicities, gastrointestinal (GI) toxicity, pneumonitis and endocrinopathy. Skin toxicity was defined to include maculopapular rash, dermatitis, and bullous pemphigoid. GI toxicity included colitis and hepatitis. Endocrinopathy included thyroiditis and adrenal insufficiency.
The primary outcome was the development of a new or recurrent irAEs during sequential therapy. Secondary outcomes were number of cycles prior to the development of irAEs and grade of irAEs in patients receiving sequential therapy.
Statistical analysis
Statistical analysis was performed using R statistical software (v4.0.3). Descriptive and univariate analyses were conducted to provide an overview of study population characteristics. We analyzed the primary and secondary outcomes via Fisher’s exact test and Wilcoxon rank sum test when appropriate. We set p value of < 0.05 to define statistically significant outcomes.
Results
A total of 483 patients received ICI in the time frame. Of those, 22 patients received sequential ICI as shown in Table 1. 16 patients (72%) received single agent ICI following the initial ICI, three patients (14%) received dual ICI following the initial ICI, one patient (5%) received chemotherapy-ICI following initial ICI, and two patients (9%) received chemo-ICI after dual ICI.
All patient except one received sequential ICI due to disease progression. Patient 12 received sequential nivolumab after ipilimumab following the development of severe colitis.
Of the 22 patients, the diagnoses included lung cancer (n = 10), melanoma (n = 7), renal cell carcinoma (n = 4) and bladder cancer (n = 1). Histological subtypes of lung cancer were adenocarcinoma (n = 7) and squamous cell carcinoma (n = 3). Histological subtypes in renal cell carcinoma were clear cell (n = 3) and papillary (n = 1) and urothelial carcinoma in bladder cancer (n = 1).
The most common initial ICI used was nivolumab (n = 12, 52%) followed by ipilimumab (n = 7, 30%), Combined nivolumab and ipilimumab (n = 2, 8.7%), atezolizumab (n = 1, 4.3%), and durvalumab (n = 1, 4.3%). None of the patients received pembrolizumab as an initial ICI. However, pembrolizumab accounted for 59% (n = 13) followed by nivolumab for 41% (n = 9) of sequential ICI. Table 2 summarizes the diagnostic, therapeutic and irAEs details.
Overall, 9 patients (41%) had irAEs after the initial exposure to ICI resulting in 10 irAEs. Initial irAEs included skin toxicity (n = 6, 60%), endocrinopathy (n = 2, 20%), colitis (n = 1, 10%), and conjunctivitis (n = 1, 10%). In patients receiving initial ICI five (50%) had grade 1 irAEs, four (40%) had grade 2 irAE and one (10%) had grade 3 irAEs. Table 3 summarizes the details of irAEs.
In patients receiving sequential treatment, seven of the 22 developed irAEs. Of these seven, skin toxicity accounted for 43% (n = 3), pneumonitis for 29% (n = 2), and endocrinopathy for 29% (n = 2). As for grading, two patients (29%) in the sequential group had grade 1 irAEs, five patients (71%) had grade 3 irAE and none developed grade 2 irAEs. One patient with melanoma developed grade 1 dermatitis with initial ipilimumab use and then developed grade 3 adrenalitis on sequential nivolumab use. Another patient with papillary renal cell carcinoma had a higher grade (3 vs 2) of the same irAEs (hypothyroidism) with the sequential use of nivolumab. No statistical difference was found between the development of irAEs and the number of cycles prior to development of irAEs in either treatment groups (p = 0.5).
Interestingly, a higher proportion of patients experienced grade 3 irAEs in the sequential ICI group (n = 5, 71%) compared to the initial ICI group (n = 1, 10%) (p = 0.03). As shown in Table 4. Notably one patient with hypothyroidism developed the same but a higher grade irAE, two patients developed new grade 3 irAEs only with sequential treatment (pneumonitis, bullous pemphigoid) with the other two patients developing a different higher grade irAEs on sequential therapy as shown in Table 2.
Discussion
ICI revolutionized the treatment and prognosis of many cancer patients. Despite major advances, developing treatment strategies to maximize efficacy of ICI treatments while balancing toxicity profiles remain one of the biggest challenges faced by medical oncologists today. The incidence of grade 3 and 4 irAEs has been reported to be 14% after anti-PD-1 monotherapy (Topalian et al. 2012), 23% after anti-CTLA-4 monotherapy (Boutros et al. 2016) and 53% after combination therapy (Wolchok et al. 2013).
Studies exploring the safety of ICI rechallenge after the development of irAEs are not conclusive with some studies demonstrating ICI rechallenge is safe and efficacious by comparing the incidence of irAEs with initial and secondary rechallenge of ICI (Abu-Sbeih et al. 2019; Ravi et al. 2020). A recent metanalysis showed that patients rechallenged with ICI had higher incidence for all-grade irAEs (OR 3.81, p < 0.0001), but similar incidence for high grade irAEs (p > 0.05) (Zhao et al. 2021). However, the utility and safety of sequential immunotherapy is not yet known, and studies are still lacking.
Preclinical data has shown that some anti-PD-1/PDL-1 bind to different epitopes (Martini et al. 2017). This has been used as the basis to use them as sequential therapy with data suggesting the benefit of the addition of anti-CTLA-4 to anti-PD-1 upon progression of disease on a single ICI (Gide et al. 2018; Babacan and Eroglu 2020; Robert et al. 2014). We report the safety and rate of irAEs of 22 patients receiving sequential ICI.
In our study, sequential ICI therapy was not associated with a higher rate of irAEs but was associated with an increase in irAEs grade if patient had incurred an irAEs.
In our study, all but one of our patients received sequential ICI due to disease progression with one being rechallenged with a different ICI after the development of irAEs.
Most patients in the initial treatment arm developed irAEs after receiving an average of 6 cycles with two patient developing conjunctivitis and dermatitis after 11 and 15 cycles respectively. In the sequential treatment group, irAEs developed after an average of 4 cycles. One patient was lost to follow-up thus possible influencing the analysis. The time to develop irAE was consistent with what is currently reported in the literature (Tang et al. 2021). Nonetheless, there were no statistically significant difference between the number of cycles and the grade of irAEs.
Recent studies show that the rate of irAEs in melanoma patients was about 49% in patients treated with anti-PD1 (Indini et al. 2019). In our melanoma cohort, irAEs rate in initial treatment arms were 85% (n = 6) and 43% (n = 3) in the sequential arm. The difference in irAEs between the two arms could be due to the small number of patients in the initial ICI group, as well as the different ICI used, which is known to have a different irAEs incidence (Weber et al. 2017). In a study of patients with metastatic melanoma who progressed on first line anti-PD-1 therapy treated with ipilimumab and an anti-PD-1, five out of 15 (33%) patients developed grade 3–4 irAEs leading to treatment discontinuation (Mehmi and Hill 2018). In another study in patients with advanced melanoma who had progressed on anti-PDL-1/L1 antibodies received combination pembrolizumab plus ipilimumab followed by Pembrolizumab monotherapy, treatment related adverse events occurred in 62 of 70 patients with grade 3–4 occurring in 19 of 70 patients (27%) (Olson et al. 2021).
In a retrospective study of metastatic renal cell carcinoma, Ravi et al reported a 16% grade ≥ 3 irAEs after rechallenge due to disease progression (72%) or intolerable ICI side effects (23%). (Ravi et al. 2020). Gul et al. reported 45 patients receiving salvage ipilimumab plus nivolumab after anti-PDL-1 therapy with grade 3 irAEs reported in six patients (13%) (Gul et al. 2020). However, in the OMNIVORE trial, patients with advanced renal cell carcinoma with stable disease or disease progression after nivolumab received two doses of ipilimumab. Any grade and grade ≥ 3 treatment related adverse event occurred in 81% and 25% of patients respectively (McKay et al. 2020). In our patients with RCC, incidence of irAEs was 25% in the initial and 50% in the sequential groups respectively.
In a study of bladder urothelial carcinoma patients who received ipilimumab and nivolumab at disease progression reported a grade ≥ 3 irAE of 43% (Keegan et al. 2019). We reported one patient with bladder urothelial carcinoma who received pembrolizumab after atezolizumab without any irAEs.
In our patients with non-small cell lung cancer, irAEs rate in both arms were 20% (n = 2). IrAEs in the initial treatment group were grade 1. In the sequential group, however, one of the patients developed a grade 3 irAE. In a retrospective study, evaluating the safety and efficacy of pembrolizumab after nivolumab. 12 patients with NSCLC were analyzed. The nivolumab group had grade 1 and grade ≥ 2 irAE of seven and eight respectively. While the pembrolizumab group had grade 1 and grade ≥ 2 irAE of 6 and 10 respectively (Fujita et al. 2018).
Given the scarcity of prospective data on ICI rechallenge, there are currently no available evidence-based guidelines on how to safely approach this therapeutic modality. The limited studies are available have suggested methods to minimize recurrence of irAEs in patients rechallenged with ICI.
Studies suggest that a longer delay between ICI discontinuation due to irAE and rechallenge was associated with lower rate of recurrence of irAEs. Furthermore, based on studies that draw attention to the fact that premature discontinuation of ICI due to severe irAEs was not associated with worse outcomes (Schadendorf et al. 2017; Horiguchi et al. 2018). Delyon et al. (2019) waited for disease progression before ICI rechallenge with less reported irAEs in patients with melanoma. However, this has not been confirmed in nonmelanoma tumors. Some lung cancer studies suggest resuming ICI after irAE improved outcomes in patients who had not yet achieved response (Santini et al. 2018). In addition, Allouchery et al. showed that the rechallenge with the same ICI drug or the same ICI combination was associated with a lower rate or irAE occurrence (Allouchery et al. 2020).
The decision to rechallenge patients with irAE presents a unique challenge for Oncologists. Until further evidence emerges a multidisciplinary approach should be taken to balance the risk and benefits of rechallenge.
Finally, our study has several limitations. Given the retrospective nature of the study and the small sample size included, our ability to draw definitive conclusions is limited. However, we report findings in an understudied but increasingly encountered scenario in the clinical practice where there is no clear data is available. Further prospective studies are required to validate the findings and establishing treatment guidelines in patients receiving sequential immune checkpoint inhibitor therapy.
Conclusion
Currently, there is insufficient data on the safety and efficacy on the sequential use of ICI after prior ICI. Our data shows overall safety of sequencing ICI when close monitoring was employed. Ideally, prospective studies to investigate the safety and efficacy of sequential therapy are needed.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Abu-Sbeih H, Ali FS, Naqash AR, Owen DH, Patel S, Otterson GA et al (2019) Resumption of immune checkpoint inhibitor therapy after immune-mediated colitis. J Clin Oncol 37(30):2738–2745
Allouchery M, Lombard T, Martin M, Rouby F, Sassier M, Bertin C et al (2020) Safety of immune checkpoint inhibitor rechallenge after discontinuation for grade ≥2 immune-related adverse events in patients with cancer. J Immunother Cancer 8(2):e001622
Babacan NA, Eroglu Z (2020) Treatment options for advanced melanoma after anti-PD-1 therapy. Curr Oncol Rep 22(4):38
Boutros C, Tarhini A, Routier E, Lambotte O, Ladurie FL, Carbonnel F et al (2016) Safety profiles of anti-CTLA-4 and anti-PD-1 antibodies alone and in combination. Nat Rev Clin Oncol 13(8):473–486
Brahmer JR, Lacchetti C, Schneider BJ, Atkins MB, Brassil KJ, Caterino JM et al (2018) Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 36(17):1714–1768
Curran MA, Montalvo W, Yagita H, Allison JP (2010) PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci 107(9):4275–4280
Delyon J, Lourenço N, Vu LT, Allayous C, Baroudjian B, Lebbe C (2019) Recurrence of immune-mediated colitis upon immune checkpoint inhibitor resumption: does time matter? J Clin Oncol 37(36):3563–3564
Fujita K, Uchida N, Kanai O, Okamura M, Nakatani K, Mio T (2018) Retreatment with pembrolizumab in advanced non-small cell lung cancer patients previously treated with nivolumab: emerging reports of 12 cases. Cancer Chemother Pharmacol 81(6):1105–1109
Gide TN, Wilmott JS, Scolyer RA, Long GV (2018) Primary and acquired resistance to immune checkpoint inhibitors in metastatic melanoma. Clin Cancer Res 24(6):1260–1270
Gul A, Stewart TF, Mantia CM, Shah NJ, Gatof ES, Long Y et al (2020) Salvage ipilimumab and nivolumab in patients with metastatic renal cell carcinoma after prior immune checkpoint inhibitors. J Clin Oncol 38(27):3088–3094
Gunturu KS, Pham TT, Shambhu S, Fisch MJ, Barron JJ, Debono D (2022) Immune checkpoint inhibitors: immune-related adverse events, healthcare utilization, and costs among commercial and Medicare Advantage patients. Support Care Cancer 30:4019–4026
Horiguchi M, Uno H, Wei L-J (2018) Patients with advanced melanoma who discontinued treatment with nivolumab and ipilimumab as a result of adverse events lived significantly longer than patients who continued treatment. J Clin Oncol 36(7):720–721
Indini A, Di Guardo L, Cimminiello C, Prisciandaro M, Randon G, De Braud F et al (2019) Immune-related adverse events correlate with improved survival in patients undergoing anti-PD1 immunotherapy for metastatic melanoma. J Cancer Res Clin Oncol 145(2):511–521
Keegan NM, Funt SA, Kania BE, Iyer G, Clement JM, McCoy AS et al (2019) Durable clinical benefit from combination ipilimumab (IPI) and nivolumab (NIVO) in anti-PD-1 therapy resistant, platinum resistant metastatic urothelial carcinoma (mUC). J Clin Oncol 37(7_suppl):481
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Lao CD et al (2019) Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 381(16):1535–1546
Martini DJ, Lalani A-KA, Bossé D, Steinharter JA, Harshman LC, Hodi FS et al (2017) Response to single agent PD-1 inhibitor after progression on previous PD-1/PD-L1 inhibitors: a case series. J Immunother Cancer 5(1):1–5
McKay RR, McGregor BA, Xie W, Braun DA, Wei X, Kyriakopoulos CE et al (2020) Optimized management of nivolumab and ipilimumab in advanced renal cell carcinoma: a response-based phase II study (OMNIVORE). J Clin Oncol 38(36):4240–4248
Mehmi I, Hill J (2018) Ipilimumab with anti PD-1 (nivolumab or pembrolizumab) after progression on first line anti-PD-1 therapy for advanced melanoma. J Clin Oncol 36(15_suppl):e21552-e
Olson DJ, Eroglu Z, Brockstein B, Poklepovic AS, Bajaj M, Babu S et al (2021) Pembrolizumab plus ipilimumab following anti-PD-1/L1 failure in melanoma. J Clin Oncol 39(24):2647–2655
Postow MA, Callahan MK, Wolchok JD (2015) Immune checkpoint blockade in cancer therapy. J Clin Oncol 33(17):1974–1982
Ravi P, Mantia C, Su C, Sorenson K, Elhag D, Rathi N et al (2020) Evaluation of the safety and efficacy of immunotherapy rechallenge in patients with renal cell carcinoma. JAMA Oncol 6(10):1606–1610
Robert C, Ribas A, Wolchok JD, Hodi FS, Hamid O, Kefford R et al (2014) Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet 384(9948):1109–1117
Santini FC, Rizvi H, Plodkowski AJ, Ni A, Lacouture ME, Gambarin-Gelwan M et al (2018) Safety and efficacy of re-treating with immunotherapy after immune-related adverse events in patients with NSCLC. Cancer Immunol Res 6(9):1093–1099
Schadendorf D, Wolchok JD, Hodi FS, Chiarion-Sileni V, Gonzalez R, Rutkowski P et al (2017) Efficacy and safety outcomes in patients with advanced melanoma who discontinued treatment with nivolumab and ipilimumab because of adverse events: a pooled analysis of randomized phase II and III trials. J Clin Oncol 35(34):3807
Tang S-Q, Tang L-L, Mao Y-P, Li W-F, Chen L, Zhang Y et al (2021) The pattern of time to onset and resolution of immune-related adverse events caused by immune checkpoint inhibitors in cancer: a pooled analysis of 23 clinical trials and 8,436 patients. Cancer Res Treat 53(2):339–354
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF et al (2012) Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med 366(26):2443–2454
Twomey JD, Zhang B (2021) Cancer immunotherapy update: FDA-approved checkpoint inhibitors and companion diagnostics. AAPS J 23(2):39
Weber JS, Hodi FS, Wolchok JD, Topalian SL, Schadendorf D, Larkin J et al (2017) Safety profile of nivolumab monotherapy: a pooled analysis of patients with advanced melanoma. J Clin Oncol 35(7):785–792
Winer A, Ghatalia P, Bubes N, Anari F, Varshavsky A, Kasireddy V et al (2019) Dual checkpoint inhibition with ipilimumab plus nivolumab after progression on sequential PD-1/PDL-1 inhibitors pembrolizumab and atezolizumab in a patient with Lynch syndrome, metastatic colon, and localized urothelial cancer. Oncologist 24(11):1416
Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM et al (2013) Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med 369(2):122–133
Zhao Q, Zhang J, Xu L, Yang H, Liang N, Zhang L et al (2021) Safety and efficacy of the rechallenge of immune checkpoint inhibitors after immune-related adverse events in patients with cancer: a systemic review and meta-analysis. Front Immunol 12:730320
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MA, BC, RR, BG, ND, LM, SRD, SM, KSG. The first draft of the manuscript was written by MA and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This is an observational study retrospective study. An IRB official waiver of ethical approval was granted from the IRB of Lahey Hospital and Medical Center. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
No identifiable data was collected or being reported. No consent to participation is needed as approved by the Institutional Review Board.
Consent to publish
No identifiable data was collected or being reported. No consent to publish is needed as approved by the Institutional Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awidi, M., Connell, B., Johnson, D. et al. Safety of sequential immune checkpoint inhibitors after prior immune therapy. J Cancer Res Clin Oncol 149, 2375–2382 (2023). https://doi.org/10.1007/s00432-022-04137-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04137-4