Abstract
Purpose
PSMD14 is an essential protein for proteasomal degradation. Inhibition of this protein disrupts homeostasis and inhibits cancer cell viability. Overexpression of PSMD14 was associated with advanced cancer characteristics and a worse prognosis in various carcinomas. This study aimed to analyze PSMD14 copy number variation, mRNA and protein expression in HNSCC, and its role as an independent prognostic biomarker.
Methods
PSMD14 mRNA expression and copy number variations were analyzed in “The Cancer Genome Atlas (TCGA)” in 510 patients. Protein expression was evaluated using immunohistochemistry in a second cohort including 115 patients. PSMD14 levels were analyzed for correlation with clinicopathological data, overall and disease-free survival.
Results
PSMD14 mRNA expression and copy number variation were high in 44 and 50% of patients, respectively. Protein expression of PSMD14 was high in 56%. In both cohorts, high PSMD14 levels were associated with advanced staging. High PSMD14 mRNA expression was additionally associated with a worse prognosis in univariable analysis. However, after correction for possible confounders, PSMD14 mRNA was not an independent prognostic marker.
Conclusion
PSMD14 is commonly expressed in HNSCC patients and associated with advanced stages. High expression of PSMD14 mRNA was associated with a worse outcome. However, this may be a result of the association of PSMD14 with poor prognosticators. Based on our study, further evaluation of PSMD14 as a prognostic marker and potential therapeutic target is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the sixth most common cancer worldwide, head and neck squamous cell carcinoma (HNSCC) affects approximately 900,000 patients annually. The incidence of this disease is rising, while therapeutic options have only marginally improved (Johnson et al. 2020; Pulte and Brenner 2010). Currently, the only applied biomarker for risk stratification and to guide therapeutic decisions for oropharyngeal squamous cell carcinoma is the detection of HPV (Mirghani and Blanchard 2018; Tawk et al. 2022). Thus, there is an urgent need for novel biomarkers and new therapeutic options in HNSCC.
The 26S proteasome non-ATPase regulatory subunit 14 (PSMD14), also known as Rpn11 or POH1, is an essential component of the 26S proteasome. The proteasome is essential for protein degradation and is involved in protein homeostasis, cell division, and transcriptional regulation. Proteins are marked for proteasomal degradation by polyubiquitination. While ubiquitin is recognized by the 19S regulatory subunit, the 20s core subunit mediates proteolysis (Li et al. 2017). PSMD14 is located in the 19S regulatory subunit and cleaves ubiquitin directly prior to the proteins’ degradation (Shin et al. 2020). Without removal of ubiquitin, the protein is too bulky to enter the proteasome. Thus, inhibition of PSMD14 disrupts protein homeostasis and leads to apoptosis in cancer cells (Li et al. 2017; Jing et al. 2021a, b).
High PSMD14 mRNA and protein expression was associated with a worse prognosis in several cancers, including HNSCC (Jing et al. 2021a; Lv et al. 2019; Wang et al. 2019; Zhu et al. 2018; Luo et al. 2017; Song et al. 2017; Zhang et al. 2020; Lei et al. 2021). However, multivariable analysis was rarely performed, and thus the role as an independent prognostic marker is unclear. Since high expression of PSMD14 is commonly linked to advanced cancer features and studies only occasionally corrected the prognostic value for potential confounders (Jing et al. 2021a; Luo et al. 2017; Zhang et al. 2020; Lei et al. 2021; Sun et al. 2021). Studies investigating the effect of inhibition of PSMD14 show promising results in vitro and in vivo (Li et al. 2017; Jing et al. 2021a, b; Song et al. 2017; Yu et al. 2019).
Since a previous study has shown an association of PSMD14 mRNA and protein expression with advanced stages and prognosis (without correction for confounders), this study aimed to further elucidate whether PSMD14 is an independent prognostic marker in HNSCC. Therefore, PSMD14 copy number variation (CNV) and mRNA expression were evaluated in a primary cohort and protein expression in a second cohort. PSMD14 levels were investigated for their independent association with survival and correlation with clinicopathological data.
Patients and methods
The Cancer Genome Atlas dataset
Patient data were extracted from cBioportal.org from “The Cancer Genome Atlas (TCGA), Firehose Legacy” and supplemented with “TCGA PanCancer Atlas” (Liu et al. 2018) and “TCGA, Nature 2015” (Gatta et al. 2000s) as described before (Schnoell et al. 2021). Eleven patients were excluded due to missing or incomplete data and patients with an overall survival (OS) of less than two months due to possible postoperative complications. mRNA expression (RNA Seq V2 RSEM) was extracted from cBioportal.org on 16 April 2021 and stratified into low and high expression at a cutoff at a z-score > 0 for high expression. Copy number variations (CNV) of PSMD14 were extracted from UCSC Xena on 15 November 2021 (Goldman et al. 2020). Expression was divided into high and low expression at a cutoff at the median CNV.
Tissue microarray dataset
A tissue microarray (TMA) containing 115 patients diagnosed with HNSCC was analyzed for the secondary cohort. Patients were included if they were diagnosed with HNSCC between 2002 and 2012 and received surgery and postoperative radio(chemo)therapy. Exclusion criteria were a second primary carcinoma, distant metastasis, prior cancer treatment, immunosuppression, or external treatment. The study was approved by the ethics committee of the Medical University of Vienna (EK1262/2019).
The TMA was established using a Galileo TMA CK Series—HTS Tissue computer assisted TMA Microarray Platform (Integrated Systems Engineering Srl, Milan, Italy). In short, three cylindrical cores (2 mm in diameter) per patient were taken from representative tumor areas from formalin-fixed, paraffin-embedded tissue. Histology was confirmed by hematoxylin–eosin staining.
Immunohistochemistry
Immunohistochemistry of PSMD14 (HPA002114-25UL, Sigma Aldrich, St. Louis, MO, USA) was visualized using the Lab Vision Ultra kit (Thermo Scientific, Waltham, MA, USA) as described before. The antibody concentration and antibody retrieval buffer were assessed prior to TMA staining. Tissue slides were dewaxed and hydrated and the endogenous hydrogenase was blocked with H2O2. Subsequently, antibody retrieval was performed using EDTA buffer in a microwave. Next, Ultra V Block was applied followed by the incubation with PSMD14 1:500 for 1 h at room temperature. Afterward, the tissue slides were incubated with the primary antibody enhancer and horseradish peroxidase enhancer. Visualization of staining was performed using the UltraVision Plus Detection System DAB Plus Substrate System (Thermo Scientific, Fremont, CA, USA). Tissue was then counterstained with hematoxylin Gill III (Merck, Darmstadt, Germany) and scanned using an Olympus BH-2 microscope (Olympus, Tokyo, Japan). Staining intensity was analyzed using QuPath (Version 0.2.3) as described before (Schnoell et al. 2021). A score was formed to include the staining intensity and percentage of stained cells (3× % of cells with high positive staining + 2× % of cells with moderately positive staining + 1× % of cells with low positive staining). Protein expression was stratified using a score ≥ 30 as cutoff for high PSMD14 expression.
Statistical analysis
Stata (Stata Corp., College Station, TX, USA) and Prism GraphPad software (GraphPad Software, Inc., La Jolla, CA, USA) were used to perform statistical analysis. Correlation between PSMD14 and clinicopathological data were assessed using Fisher’s exact test or Chi-squared test. Overall survival (OS) and disease-free survival (DFS) were calculated from the date of diagnosis to the date of death or recurrence, respectively. Survival was visualized with Kaplan Meier curves. Association with survival was analyzed using log-rank test and a cox-proportional hazard regression model.
Results
Primary dataset (TCGA)
Patient characteristics of the primary dataset are displayed in Table 1, left column. Five hundred and ten patients were included in the TCGA. Three hundred and seventy-eight patients (74%) were male and 307 (60%) had an oropharyngeal tumor. Seventy-six patients (15%) were HPV positive. The median age at diagnosis was 60.5 (53–68) years. The median observation period was 2.9 (1.8–4.6) years. The median OS was 4.7 (1.4–12.8) years and the median DFS was 4.7 (1.1–17.6) years. Most patients were treated with surgery and postoperative radiotherapy (n = 189, 37%).
Association of PSMD14 mRNA expression and CNV with clinicopathological data
To assess the association of PSMD14 mRNA expression and CNV with clinicopathological features, mRNA expression was stratified into high and low expression and correlation analysis was performed using Fisher’s exact test or Chi-squared test.
mRNA expression of PSMD14 was high in 222 patients (44%). High expression of PSMD14 mRNA was associated with locally advanced stages (T3-4, p = 0.001), advanced overall staging (III-IV, p = 0.040) and an HPV negative status (p = 0.011). CNV was high in 252 patients (50%). High CNV was associated with locally advanced stages (T3-4, p = 0.044) and tobacco use (p = 0.014). PSMD14 mRNA expression moderately correlated with CNV (chi2 p < 0.001, r = 0.529).
Analysis of PSM14 mRNA expression and CNV with prognosis
Next, PSMD14 mRNA expression and CNV were investigated for their association with OS and DFS using log-rank test and an uni- and multivariable cox-proportional hazard regression model.
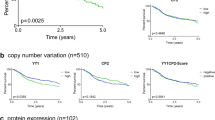
Patients with high PSMD14 mRNA showed a shorter median OS (5.5 vs. 3.1 years, p = 0.013) and DFS (5.1 vs. 4.0 years, p = 0.032; Fig. 2). Patients with a high PSMD14 mRNA expression showed an increased risk for death (HR 1.41, 95% CI 1.07–1.85, p = 0.014) and recurrence (HR 1.36, 95% CI 1.02–1.80, p = 0.033) in univariable analysis (Table 2). Additional analysis of the continuous mRNA z scores revealed an increased risk for death (HR 1.19, 95% CI 1.07–1.32, p = 0.001) and recurrence (HR 1.16, 95% CI 1.04–1.29, p = 0.007). However, these results did not prevail in multivariable analysis after correction for stage, smoker and HPV status. CNV was not associated with OS or DFS (Fig. 2; Table 2).
Secondary dataset (TMA)—analysis of PSMD14 protein expression
To validate the findings of the TCGA cohort, protein expression of PSMD14 was assessed using immunohistochemistry in a secondary cohort and associated with clinicopathological data and patient outcome.
One hundred fifteen patients were included in this dataset. Patient characteristics of the secondary dataset are described in Table 1, right column. The median age at diagnosis was 59 (53–63) years. The median observation period was 8.9 (6.3–11.8) years. The median OS was 9.9 (2.61-not reached) years and the median DFS was 13.1 (2.7-not reached) years. Protein expression was assessed using immunohistochemistry (Fig. 1). The median protein score was 33 (15–60). Patients were stratified at a protein expression score of 30. Sixty-four patients (56%) showed high expression and 51 patients (44%) showed low expression of PSMD14. Within the high and low expression groups, the median expression scores were 53 (38–78) and 12 (6–19), respectively. Eight patients (7%) were PSMD14 negative (expression score < 5).
High PSMD14 protein expression was associated with lymph node metastasis (N1-3, p = 0.002) and advanced stages (III–IV, p = 0.002; Table 3). Protein expression was not associated with OS or DFS (Table 2, Fig. 2).
Discussion
HNSCC is the sixth most frequently diagnosed cancer worldwide. Treatment de-escalation is currently under investigation in HPV positive tumors because of the favorable prognosis (Mirghani and Blanchard 2018; Tawk et al. 2022). To date, there are no other biomarkers in clinical use to identify patients with a more aggressive phenotype. PSMD14 is an essential part of the proteasome and has been linked to prognosis in various cancers (Jing et al. 2021a; Lv et al. 2019; Wang et al. 2019; Zhu et al. 2018; Luo et al. 2017; Song et al. 2017; Zhang et al. 2020; Lei et al. 2021). In HNSCC, a first study has shown an association of PSMD14 mRNA and protein expression with advanced stages and prognosis, however, no correction for confounders was reported. Furthermore, inhibition of PSMD14 has shown promising results in vitro and in vivo (Jing et al. 2021a, b; Lv et al. 2019; Zhang et al. 2020). Therefore, the expression of PSMD14 mRNA, protein and CNV was investigated in two HNSCC cohorts and evaluated as an independent prognostic marker.
PSMD14 mRNA expression and CNV was high in 44 and 50% of patients, respectively, and protein expression of PSMD14 was high in 56%. High PSMD14 mRNA expression was associated with advanced T and N stage and a negative HPV status. In accordance, high CNV values were associated with a high T stage and active smokers. In the secondary dataset, high protein expression was associated with a positive N stage and advanced overall stage. These results are in line with literature. PSMD14 expression was high in 42% of HNSCC (Jing et al. 2021a), 66% of non-small cell lung cancer (Lei et al. 2021) and 64% of ovarian cancer (Sun et al. 2021). Furthermore, high PSMD14 levels were associated with advanced cancer stages in various cancer types (Jing et al. 2021a; Luo et al. 2017; Zhang et al. 2020; Lei et al. 2021; Sun et al. 2021). Since expression of PSMD14 is associated with tumor promotion through interaction with the transcription factor E2F1 (Jing et al. 2021a; Wang et al. 2015), our results further support that PSMD14 plays a role in cancer progression of HNSCC. A first preclinical study shows promising anticancer results of the PSMD14 inhibitor thiolutin in HNSCC (Jing et al. 2021a). Furthermore, inhibition of PSMD14 with o-phenanthroline, thiolutin and capzimin showed anticancer effects in other cancer types (Li et al. 2017; Jing et al. 2021b; Lv et al. 2019; Song et al. 2017). Based on our data, the evaluation of PSMD14 as a therapeutic target is recommended in HNSCC, especially in advanced stages, due to the more common upregulation.
Next, we analyzed the association of PSMD14 with prognosis. High PSMD14 mRNA expression was associated with a shorter median OS and DFS. Furthermore, high categorical and continuous mRNA expression was associated with a worse OS and DFS in univariable analysis. However, since high PSMD14 expression was associated with poor prognostic factors (advance stages, HPV negative status), we further performed multivariable analysis. After correction for possible confounders (including staging, HPV and smoker status), PSMD14 mRNA expression did not show an association with disease outcome. In contrast, when CNV and protein expression were analyzed, there was no association with OS or DFS. While Jing et al. concluded that high PSMD14 protein expression is a prognostic factor in HNSCC and is also associated with advanced stages in their study, no multivariable analysis was reported to correct for confounders (Jing et al. 2021a). Similarly, high expression of PSMD14 is associated with a worse prognosis in multiple myeloma, esophageal, ovarian, breast cancer and osteosarcoma. Although expression is associated with prognosis and occasionally with advanced cancer features in these studies, correction of the prognostic relevance of PSMD14 for potential confounders was not described (Lv et al. 2019; Luo et al. 2017; Song et al. 2017; Sun et al. 2021; Gong and Wei 2021). In accordance with our results, Zhang et al. revealed that PSMD14 is associated with OS and DFS in lung adenocarcinoma. However, after multivariable analysis, PSMD14 failed to show an independent association (Zhang et al. 2020). In contrast, PSMD14 is an independent prognostic factor in hepatocellular carcinoma and non-small cell lung cancer (Wang et al. 2019; Lei et al. 2021). Altogether, these results indicate that PSMD14 plays a role in advanced cancers. The question remains whether PSMD14 may serve as an independent prognostic biomarker in HNSCC or its association with prognosis is a result of upregulation during cancer progression.
There are limitations of this study that need to be discussed. First, mRNA and CNV expression were compared to protein expression in a second cohort. Although correlation of mRNA and protein at the bulk level is assumed, protein expression may be modified by post-transcriptional processes (Liu et al. 2016). Second, interpretation of the results is limited due to the retrospective design. Selection bias may apply; however, the risk was reduced by including a homogenously treated secondary cohort. Third, the stratification for high and low expression was determined using the median as an empiric cutoff. Thus, interpretation of the results in comparison to other studies is difficult as the cutoff may vary. Last, protein expression was analyzed in three TMA cores taken from representative tumor areas using QuPath. However, the distribution of protein expression within the tumor may vary.
In conclusion, the results of this retrospective study indicate that high PSMD14 is associated with advanced stages in HNSCC. Therefore, further evaluation of PSMD14 as a therapeutic target is warranted, especially in these subgroups. While PSMD14 mRNA expression was associated with prognosis in univariable Cox regression, this may result from the association with poor prognosticators.
Availability of supporting data
The datasets of this study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
confidence interval
- CNV:
-
copy number variations
- DFS:
-
Disease-free survival
- HR:
-
hazard ratio
- OS:
-
overall survival
- PSMD14:
-
26S proteasome non-ATPase regulatory subunit 14
- TCGA:
-
The Cancer Genome Atlas
- TMA:
-
tissue microarray
References
Gatta G, Botta L, Sánchez MJ et al (2015) Prognoses and improvement for head and neck cancers diagnosed in Europe in early 2000s: the EUROCARE-5 population-based study. Eur J Cancer 51(15):2130–2143
Goldman MJ, Craft B, Hastie M et al (2020) Visualizing and interpreting cancer genomics data via the Xena platform. Nat Biotechnol 38(6):675–678
Gong Y, Wei Z (2021) Identification of PSMD14 as a potential novel prognosis biomarker and therapeutic target for osteosarcoma. Cancer Rep e1522
Jing C, Duan Y, Zhou M et al (2021a) Blockade of deubiquitinating enzyme PSMD14 overcomes chemoresistance in head and neck squamous cell carcinoma by antagonizing E2F1/Akt/SOX2-mediated stemness. Theranostics 11(6):2655–2669
Jing C, Li X, Zhou M et al (2021b) The PSMD14 inhibitor Thiolutin as a novel therapeutic approach for esophageal squamous cell carcinoma through facilitating SNAIL degradation. Theranostics 11(12):5847–5862
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR (2020) Head and neck squamous cell carcinoma. Nat Rev Dis Prim 6(1):92
Lei J, Liu X, Liu W, Zhang Y, Liu Z (2021) The prognostic value of USP14 and PSMD14 expression in non- small cell lung cancer. Ann Transl Med 9(12):1019–1019
Li J, Yakushi T, Parlati F et al (2017) Capzimin is a potent and specific inhibitor of proteasome isopeptidase Rpn11. Nat Chem Biol 13(5):486–493
Liu Y, Beyer A, Aebersold R (2016) On the dependency of cellular protein levels on mRNA abundance. Cell 165(3):535–550
Liu J, Lichtenberg T, Hoadley KA et al (2018) An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell 173(2):400-416.e11
Luo G, Hu N, Xia X, Zhou J, Ye C (2017) RPN11 deubiquitinase promotes proliferation and migration of breast cancer cells. Mol Med Rep 16(1):331–338
Lv J, Zhang S, Wu H et al (2020) Deubiquitinase PSMD14 enhances hepatocellular carcinoma growth and metastasis by stabilizing GRB2. Cancer Lett 469(October 2019):22–34
Mirghani H, Blanchard P (2018) Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol 8:4–11
Pulte D, Brenner H (2010) Changes in survival in head and neck cancers in the late 20th and early 21st century: a period analysis. Oncologist 15(9):994–1001
Schnoell J, Jank BJ, Kadletz-Wanke L et al (2021) Transcription factors CP2 and YY1 as prognostic markers in head and neck squamous cell carcinoma: analysis of The Cancer Genome Atlas and a second independent cohort. J Cancer Res Clin Oncol 147(3):755–765
Shin JY, Muniyappan S, Tran N-N, Park H, Lee SB, Lee B-H (2020) Deubiquitination reactions on the proteasome for proteasome versatility. Int J Mol Sci 21(15):5312
Song Y, Li S, Ray A et al (2017) Blockade of deubiquitylating enzyme Rpn11 triggers apoptosis in multiple myeloma cells and overcomes bortezomib resistance. Oncogene 36(40):5631–5638
Sun T, Liu Z, Bi F, Yang Q (2021) Deubiquitinase PSMD14 promotes ovarian cancer progression by decreasing enzymatic activity of PKM2. Mol Oncol. https://doi.org/10.1002/1878-0261.13076
Tawk B, Debus J, Abdollahi A (2022) Evolution of a paradigm switch in diagnosis and treatment of HPV-driven head and neck cancer—striking the balance between toxicity and cure. Front Pharmacol 12(January):1–18
Wang B, Ma A, Zhang L et al (2015) POH1 deubiquitylates and stabilizes E2F1 to promote tumour formation. Nat Commun 6(1):8704
Wang B, Xu X, Yang Z et al (2019) POH1 contributes to hyperactivation of TGF-β signaling and facilitates hepatocellular carcinoma metastasis through deubiquitinating TGF-β receptors and caveolin-1. EBioMedicine 41:320–332
Yu W, Li J, Wang Q et al (2019) Targeting POH1 inhibits prostate cancer cell growth and enhances the suppressive efficacy of androgen deprivation and docetaxel. Prostate 79(11):1304–1315
Zhang L, Xu H, Ma C et al (2020) Upregulation of deubiquitinase PSMD14 in lung adenocarcinoma (LUAD) and its prognostic significance. J Cancer 11(10):2962–2971
Zhu R, Liu Y, Zhou H et al (2018) Deubiquitinating enzyme PSMD14 promotes tumor metastasis through stabilizing SNAIL in human esophageal squamous cell carcinoma. Cancer Lett 418:125–134
Funding
Open access funding provided by Medical University of Vienna. Not applicable.
Author information
Authors and Affiliations
Contributions
JS, BJJ and AS contributed to the design of the study, data collection, statistical analysis, and writing of the manuscript. SA, LKW, LK, and GH contributed to the design of the study, data collection and manuscript revision. All authors critically reviewed the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study was approved by the ethics committee of the Medical University of Vienna (EK1262/2019).
Consent for participation and publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schnoell, J., Scheiflinger, A., Al-Gboore, S. et al. The prognostic role of PSMD14 in head and neck squamous cell carcinoma. J Cancer Res Clin Oncol 149, 2483–2490 (2023). https://doi.org/10.1007/s00432-022-04072-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04072-4