Abstract
Objective
Five commonly used global health assessment tools have been evaluated to identify and assess the preoperative frailty status and its relationship with perioperative in-hospital complications and transfusion rates in older women with endometrial cancer (EC).
Methods
Preoperative frailty status was examined by the G8 questionnaire, the Eastern Cooperative Oncology Group performance status, the Charlson Comorbidity Index and the American Society of Anesthesiologists Physical Status System, as well as the Lee-Schonberg prognostic index. The main outcome measures were perioperative laboratory values, intraoperative surgical parameters and immediately postoperative complications.
Results
153 consecutive women ≥ 60 years with all stages of EC, who received primary elective surgery at the University Medical Center Mainz between 2008 and 2019 were classified with selected global health assessment tools according to their preoperative performance status. In contrast to conventional prognostic parameters like older age and higher BMI, increasing frailty was significantly associated with preoperative anemia and perioperative transfusions (p < 0.05). Moreover, in patients preoperatively classified as frail significantly more postoperative complications (G8 Score: frail: 20.7% vs. non-frail: 6.7%, p = 0.028; ECOG: frail: 40.9% vs. non-frail: 2.8%, p = 0.002; and CCI: frail: 25.0% vs. non-frail: 7.4%, p = 0.003) and an increased length of hospitalization were recorded. According to propensity score matching, the risk for developing postoperative complications for frail patients was approximately two-fold higher, depending on which global health assessment tool was used.
Conclusions
Preoperatively assessed frailty significantly predicts post-surgical morbidity rates in contrast to conventionally used single prognostic parameters such as age or BMI. A standardized preoperative assessment of frailty in the routine work-up might be beneficial in older cancer patients before major surgery to include these patients in a prehabilitation program with nutrition counseling and physiotherapy to adequately assess the perioperative risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The complex concept of frailty and its increasing relevance in the ageing population require the recognition of the importance of global health assessment tools in everyday clinical practice (Lin et al. 2016; Birkelbach et al. 2019). Frailty, defined as a multidimensional clinical syndrome of age-associated decreased homeostatic reserves and function due to multiple organ systems, combines the dysregulation across various physiologic and molecular pathways with marked vulnerability to adverse health outcomes (Fried 2001; Rodríguez-Mañas et al. 2013). The “phenotype of frailty “results in diminished endurance and strength, a higher risk of falls, disability, hospitalization and mortality (Fried 2001). However, even this description from Fried et al. is the most cited, there is no commonly accepted uniform definition. Although there is no gold standard for detecting frailty, different global health assessment tools have been developed focusing on various aspects of health, especially in the preoperative setting (Table 1).
As the current world population is getting older, there is an increased demand for special diagnostic and treatment algorithms specific to elderly cancer patients to offer multimodal oncological therapy regimens (Mohile et al. 2018). While increased age is often associated with more aggressive and advanced diseases (Bourgin et al. 2017; Emons et al. 2018), its independent role on mortality and morbidity remains controversial (Quaglia et al. 2009; Deiner and Silverstein 2011; El-Haddawi et al. 2002). The population older than 65 years is less likely to have all types of standardized oncological investigations resulting in an overall worse outcome in elderly cancer patients (Rauh-Hain et al. 2015). However, chronological age alone, as the single prognostic factor probably does not reflect the heterogeneity of the ageing process but because of the underrepresentation of elderly participants in clinical trials, only little evidence exists (Lewis et al. 2003).
Endometrial cancer (EC) is the most common gynecologic malignancy in developed countries with an incidence of one to two percent of females in the United States and 54,870 cases per year with 10,170 identified annual deaths (Bourgin et al. 2017; Schmidmayr and Dorn 2021; Chen and Berek 2021). EC primarily affects elderly women as age-standardized incidence rates peak after menopause, between the ages of 60 and 70 years, with a median age of 68 years at diagnosis (Sung et al. 2020). The main risk factors for EC include obesity, mostly in combination with other cardiovascular or metabolic diseases such as hypertension and diabetes mellitus, as well as chronic exogenous unopposed estrogen replacement treatments without progestin (Emons et al. 2018; Sorosky 2012). The keystone of treatment for EC, similar to other cancer types, is primary surgery for curative intended oncologic treatments and is considered a major stressor for patients. The extend of the surgical treatment depends on results of lymph node staging, the disease stage at diagnosis, various histological parameters, the health status of the patient and the present national guidelines (Morice et al. 2016). In general, frail patients are less likely to tolerate and adapt to radical, possibly multi-visceral surgical resections (Revenig et al. 2014; Li et al. 2018). Besides for postoperative complications, frailty also appears to be a risk factor for unplanned readmissions (Rothenberg et al. 2019; Robinson et al. 2011). As the incidence of frailty increases with age (25.5–56.1% in elderly patients vs. 6.9% in younger counterparts) (Amrock and Deiner 2014), frailty assessments become important especially in elderly cohorts with a higher incidence of cancer and an approximately 70% mortality (Sung, et al. 2020).
Therefore, the primary objective of this retrospective, observational cohort study was to evaluate the influence of frailty on perioperative complications in elderly endometrial cancer patients undergoing primary surgical treatment. Consequently, we assessed the predictive abilities of the preoperative frailty status evaluated by five broadly recognized global health assessment tools for the perioperative laboratory values and transfusion rates as well as postoperative complications.
Methods
Study population
This retrospective cohort analysis reports data from women older than 60 years of age treated consecutively at the University Medical Center Mainz—Johannes-Gutenberg University Mainz, Germany, between January 2008 and December 2019. All stages of EC were included. Standardized primary staging operations included hysterectomy with bilateral salpingo-oophorectomy, with or without pelvic and para-aortic lymph node resection, depending on tumor stage and the current national guidelines. The patients’ preoperative frailty status was retrospectively assessed based on the routine pre-surgical patient evaluation.
Frailty assessments
In this study, the preoperative frailty status was assessed by five global health assessment tools (Table 1).
The G8 questionnaire (G8 Score) established in 2011 by Bellera et al. is a geriatric screening tool recommended by the International Society of Geriatric Oncology (SIOG) (Bellera et al. 2012). As a simple, time saving and reproducible questionnaire, the G8 Score aims to identify frail patients, who could benefit from a full Comprehensive geriatric assessment (CGA) after a two-step evaluation (Martinez-Tapia et al. 2017). The scoring system ranges from zero points (heavily impaired—G8-frail) to seventeen points (not impaired at all—G8-non-frail) with an established cut-off value of ≤ 14 points as an indicator of frailty (Hamaker et al. 2012).
The Eastern Cooperative Oncology Group (ECOG) performance status is one of the most commonly used methods to measure physiological reserves and functional status in cancer patients. The degree of functional impairment is divided into six categories, as a simplification of the in 1948 first described Karnofsky status. Five points, the maximum of the score, represent the clinical death, while a value of zero points represents normal unrestricted everyday activities prior to the disease (Rodin and Mohile 2007).
The Charlson Comorbidity Index (CCI) is an assessment of medical comorbidities to measure the estimated 1-year mortality and burden of disease, developed in 1987 (Charlson et al. 1987). Especially as a predictor of surgical mortality the sum of 16 different conditions according to ICD-10 codes has been validated (Molto and Dougados 2014).
The American Society of Anesthesiologists Physical Status System (ASA PS) is an international commonly used subjective rating system to categorize the preoperative overall medical health status of adult patients, first described in 1941 (Saklad 1941). The current ASA PS classification was proposed in 1961 by Dripps et al. (Fitz-Henry 2011), and was actually updated by Böhmer and colleagues (Böhmer et al. 2021). According to the inclusion criteria of the current study, emergency surgeries were excluded, thus ASA Class 5 and 6 were not included in the evaluation.
The Lee-Schonberg prognostic index (Lee-Index) has been “developed in 11,701 community-dwelling adults from the eastern, western and central United States who were interviewed in the Health Retirement Survey in 1998” (Lee et al. 2006). Depending on key health outcomes, the life expectancy calculator estimates the individual 4-year mortality through 15 selected questions.
Data collection
General patient information was gathered from our hospital database, including biological tumor characteristics (tumor stage, histological grading and subtype), relevant lifestyle parameters like age, weight, smoking status and polypharmacy, as well as blood works and postoperative complications. Perioperative clinical and surgical complications were extracted according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10) (WH Organization 2004) corresponding to the Veteran Affairs’ National Surgical Quality Improvement Program (NSQIP) (Khuri et al. 1998; Robinson et al. 2013). Long-term follow-up data were collected through telephone calls, written inquiries to the patients or their physicians, and by checking the available patient clinical records up to February 2021.
The G8 Score was determined retrospectively by adding the biological-calendar age to the Mini Nutritional Assessment (MNA) recorded by oncological nurses, trained in frailty assessment in cooperation with the geriatric department (Vellas et al. 1999; Rubenstein et al. 2001; Anic et al. 2021). The 4-year mortality rate routinely utilized and reproducibly estimated with the Lee-Index was modified afterwards by following the calculation without the cancer diagnosis. Relevant comorbidities were detected by the CCI, with the sum of sixteen different conditions according to ICD-10 codes (WH Organization 2004). ECOG was assigned individually by the operating surgeon during the consultation. The ASA PS was collected from all patients undergoing elective surgery at the anesthesia preoperative clinic of the Department of Anesthesiology.
Statistical analyses
The manuscript was written in accordance with the STROBE-cohort checklist of the EQUATOR network reporting guidelines (Elm et al. 2007). Descriptive statistical analyses were performed with SPSS statistical software program, version 23.0 V5 R (SPSS Inc, Chicago, IL, U.S.A.) and StatalC 16 V5. All data analyses were carried out in an explorative approach.
Categorical data are given in absolute and relative frequencies. Continuous parameters are reported as mean ± standard deviation [SD] for normally distributed data and as medians and interquartile ranges (IQR) for non-parametric data. Differences in binary and ordinal variables between two independent groups were analyzed by the chi-square tests. To assess the usability in a clinical context, we defined the frailty status for each global health assessment tool by dichotomizing the values into two groups: frail and non-frail, respectively (Table 1). To preserve comparability, we furthermore dichotomized the study cohort into two groups, younger and older than the mean biological-calendaric age, as well as two groups with lower and higher BMI than the median, respectively. To investigate its impact on perioperative complications we used the exact chi-square test. A two-tailed p value < 0.05 was considered statistically significant. All analyses should be understood as explorative analyses, thus, no adjustment for multiple testing has been done.
To remove the simultaneous impact of frailty and other predictive factors as baseline confounder variables such as age and BMI especially for EC on the occurrence of perioperative events, we determined a propensity score model.
Results
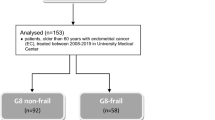
A total of 153 women aged older than 60 years (median 71 ± 7.4 years) were included in this study (for details see Fig. 1 and Table 2). Patients’ characteristics including tumor features, frailty status and lifestyle parameters, as well as postoperative events are presented in Table 2.
Overall, data from a surgical point of view, that no differences were observed in intraoperative parameters between the frail and non-frail cohort, regardless of the used global health assessment tool, were published in a previous study (Anic et al. 2022). Neither the mean incision-suture with 142 ± 82.2 min nor the intraabdominal drainages rate of 64.7% or rate of operative revisions (2.6%) correlated with frailty status. One or more postoperative clinical in-hospital complications were observed in 19 patients (12.5%). Patients classified as frail determined by G8 Score, ECOG and CCI (Table 1), had significantly higher rates of preoperative anemia (hemoglobin < 10 g/dl) compared with non-frail patients, in contrast to the evaluation with ASA PS or Lee-Index (Table 3). Furthermore, the patients classified as frail received significantly more transfusions. Remarkably, age or BMI alone were not associated with anemia or the transfusion rates.
Significant differences were found between the frail or non-frail group with respect to the rates of clinical postoperative complications in total (G8 Score: frail: 20.7% vs. non-frail: 6.7%, p = 0.028; ECOG: frail: 40.9% vs. non-frail: 2.8%, p = 0.002; and CCI: frail: 25.0% vs. non-frail: 7.4%, p = 0.003; respectively), pulmonological complications (CCI: frail: 80.0% vs. non-frail: 20.0%, p = 0.010), wound infections (ECOG: frail: 100.0% vs. non-frail: 0.0%, p < 0.001) as well as multiple complications (G8 Score: frail: 100.0% vs. non-frail: 0.0%, p = 0.029 and ECOG: frail:100.0% vs. non-frail 0.0%, p = 0.010; respectively (Fig. 2)). Additionally, the length of hospital stay was associated with preoperative ECOG and CCI frailty-status.
In propensity score matching, chronological age and BMI did not persist as a statistically significant prognostic factors for complications in the matched groups, independent of G8 Score, CCI and ECOG. The accumulation of postoperative complications did not correlate with age and BMI. Remarkably, the complication rate in the frail cohort was two to three times more common than in the non-frail cohort (G8 Score: HR: 2.12, 95%-CI: [0.012–0.313], p = 0.034; CCI: HR: 2.6, 95%-CI: [0.064–0.459], p = 0.009 and ECOG: HR: 2.6, 95%-CI: [0.087–0.617], p = 0.009; respectively).
Discussion
The aim of this study was to analyze the relationship between the preoperative frailty status, measured by selected commonly used global health assessment tools, and the incidence of postoperative in-hospital complications in a highly selected patient cohort with exclusively women older than 60 years with endometrial cancer, treated in the University Hospital Mainz, Germany.
Three sub-aspects of the perioperative setting were highlighted. Related to the preoperative laboratory values, the G8 Score, ECOG and CCI showed a significant association with anemia. Surgical parameters, such as incision-suture time, drainages and intraoperative blood loss, as well as operative revisions, did not correlate with the preoperative frailty status, which proved to be a quality feature of this study, as all patients underwent the same radical surgery regardless of their preoperative global health status.
Of utmost importance, the perioperative use of blood products was highly associated with the preoperative frailty evaluation. Furthermore, postoperative clinical events, as well as the length of hospital stay correlated significantly with the preoperative frailty status raised by G8 Score and ECOG. This synergistic relationship between a higher ECOG status and the evaluation as a frail person with the G8 Score has already been demonstrated in several studies including oncological patients (Takahashi et al. 2017). One explanation for the significant correlation of the G8 Score with postoperative complications, especially in patients with EC, may be its emphasis on nutritional (three of eight items) and physical performance status (one item). The primary risk factor for developing an EC is obesity (mean BMI in our cohort is 30.19 ± 7.7), which might be perfectly reflected by the G8 Score composed of seven items of the MNA in combination with age (Emons et al. 2018; Vellas et al. 1999).
Our results are also in line with several prospective and retrospective investigations in different surgical disciplines (Birkelbach et al. 2019; Kristjansson et al. 2010; Lee et al. 2010). Birkelbach and colleagues assessed 1186 elderly patients 65 years old or older, evaluated for frailty using Fried’s 5-point frailty assessment before elective non-cardiac surgery examining its independent predictive power in the postoperative complication context (Birkelbach et al. 2019). Kristjansson et al. reported higher rates of serve complications after elective surgery for colorectal cancer in patients categorized as frail with a multidisciplinary CGA within 14 days prior to surgery (Kristjansson et al. 2010). In a series of 178 participants, they assessed the physical and cognitive functioning, comorbidity with polypharmacy, nutrition, as well as emotional status as part of a systematic CGA.
The decision to use the reported five global health assessment tools (G8 Score, ECOG, CCI, ASA PS and Lee-Index) was made considering that a larger pool of publications would enhance the study’s background and allow broader comparability. In addition, we soughed to maintain the interdisciplinarity of the frailty assessment. ECOG is a commonly used classification in oncology, whereas the ASA PS was assigned by anesthesiologists. The G8 Score and the CCI were collected in collaboration with geriatricians. Awareness of the relevance of frailty status especially in the preoperative setting and its multidimensional character could be the basis for a shared decision-making and individualized treatment. However, identifying frail cancer patients with improved risk for pre- and postoperative morbidity should include a patient-centered prehabilitation program, including nutrition counseling, physiotherapy, anticipatorily organizing postoperative home care, as well as avoiding potential preoperative complications such as hypothermia, dehydration or delirium (Mörgeli et al. 2017).
Limitations arise from the retrospective character of our study. This may be relevant especially in terms of incomplete follow-up, which were successfully reduced to a minimum of twelve patients (6.5%) by reaching out to patients and physicians through different channels of communication and an extensive review of clinical records. Moreover, the sample size, with in total 153 women was not very large, which might limit the power of the current trial. Frailty screening was offered to all women 60 years and older with EC seen in the preoperative prearrangement. We tried to minimize the possible systemic error that arises from the large range of surgical interventions and surgeons by operating all patients in one University hospital according to the current national guidelines. Outcome parameters were not rated into minor/major categories and were derived from ICD-10 coded hospital diagnoses so that limitations of routine data use were applicable. Moreover, which global health assessment tool is the most appropriate, would need to be validated in the future.
In conclusion, this is the first report to focus exclusively on elderly EC patients and the association between the preoperative frailty status measured with different global health assessment tools and perioperative parameters. In contrast to conventional prognostic parameters such as higher BMI or advanced age, the preoperative frailty status significantly correlates with preoperative anemia, perioperative transfusion rates and postoperative in-hospital complications. A standardized, possibly multidisciplinary frailty assessment in the preoperative preparation of elderly cancer patients should be established to evaluate the perioperative risk and to individualize the therapy algorithm. Further prospective research should be initiated to recognize the preoperatively frail patient in a standardized manner and to implement a patient-centered interdisciplinary discussion about individualized modified prevention and therapy management.
Data availability
All data generated or analysed during this study are included in this article and its supplementary material files. Further enquiries can be directed to the corresponding author.
Abbreviations
- ASA PS:
-
American Society of Anesthesiologists Physical Status System
- CCI:
-
Charlson Comorbidity Index
- CGA:
-
Comprehensive geriatric assessment
- EC:
-
Endometrial cancer
- ECOG:
-
Eastern Cooperative Oncology Group performance status
- G8 Score:
-
G8 questionnaire
- IQR:
-
Interquartile range
- MNA:
-
Mini Nutritional Assessment
- Lee-Index:
-
Lee-Schonberg prognostic index
- NSQIP:
-
National Surgical Quality Improvement Program
- SIOG:
-
International Society of Geriatric Oncology
- SD:
-
Standard deviation
References
Amrock LG, Deiner S (2014) The implication of frailty on preoperative risk assessment. Curr Opin Anaesthesiol 27(3):330
Anic K et al (2021) G-8 geriatric screening tool independently predicts progression-free survival in older ovarian cancer patients irrespective of maximal surgical effort: results of a retrospective cohort study. Gerontology. https://doi.org/10.1159/000520328
Anic K et al (2022) The preoperative G8 geriatric screening tool independently predicts survival in older patients with endometrial cancer: results of a retrospective single-institution cohort study. J Cancer Res Clin Oncol. https://doi.org/10.1007/s00432-022-03934-1
Bellera C et al (2012) Screening older cancer patients: first evaluation of the G-8 geriatric screening tool. Ann Oncol 23(8):2166–2172
Birkelbach O et al (2019) Routine frailty assessment predicts postoperative complications in elderly patients across surgical disciplines–a retrospective observational study. BMC Anesthesiol 19(1):1–10
Boehmer A, Defosse J, Geldner G, Rossaint R, Zacharowski K, Zwissler B, Wappler F (2021) The updated ASA classification. Anasthesiol Intensivmedizin 62:223–228
Bourgin C, Lambaudie E, Houvenaeghel G, Foucher F, Lévêque J, Lavoué V (2017) Impact of age on surgical staging and approaches (laparotomy, laparoscopy and robotic surgery) in endometrial cancer management. Eur J Surg Oncol 43(4):703–709
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Chen L-m, Berek J (2021) Endometrial carcinoma: epidemiology, risk factors and prevention. ed: UpToDate
Deiner S, Silverstein J (2011) Anesthesia for geriatric patients. Minerva Anestesiol 77(2):180–189
El-Haddawi F, Abu-Zidan FM, Jones W (2002) Factors affecting surgical outcome in the elderly at Auckland Hospital. ANZ J Surg 72(8):537–541
Emons G et al (2018) Interdisciplinary diagnosis, therapy and follow-up of patients with endometrial cancer. Guideline (S3-Level, AWMF Registry Number 032/034-OL, April 2018)–Part 2 with recommendations on the therapy and follow-up of endometrial cancer, palliative care, psycho-oncological/psychosocial care/rehabilitation/patient information and healthcare facilities. Geburtshilfe Frauenheilkd 78(11):1089–1109
Fitz-Henry J (2011) The ASA classification and peri-operative risk. Ann R Coll Surg England 93(3):185–187
Fried LP (2001) Frailty in older adults: evidence for a phenotype. J Gerontol. Med Sci 56:M146–M156
Hamaker ME, Jonker JM, de Rooij SE, Vos AG, Smorenburg CH, van Munster BC (2012) Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: a systematic review. Lancet Oncol 13(10):e437–e444
Khuri SF et al (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228(4):491
Kristjansson SR et al (2010) Comprehensive geriatric assessment can predict complications in elderly patients after elective surgery for colorectal cancer: a prospective observational cohort study. Crit Rev Oncol Hematol 76(3):208–217
Lee SJ, Lindquist K, Segal MR, Covinsky KE (2006) Development and validation of a prognostic index for 4-year mortality in older adults. JAMA 295(7):801–808
Lee DH, Buth KJ, Martin B-J, Yip AM, Hirsch GM (2010) Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation 121(8):973–978
Lewis JH et al (2003) Participation of patients 65 years of age or older in cancer clinical trials. J Clin Oncol 21(7):1383–1389
Li Y et al (2018) Impact of frailty on outcomes after discharge in older surgical patients: a prospective cohort study. CMAJ 190(7):E184–E190
Lin H-S, Watts J, Peel N, Hubbard R (2016) Frailty and post-operative outcomes in older surgical patients: a systematic review. BMC Geriatr 16(1):1–12
Martinez-Tapia C et al (2017) Prognostic value of the G8 and modified-G8 screening tools for multidimensional health problems in older patients with cancer. Eur J Cancer 83:211–219
Mohile SG et al (2018) Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology. J Clin Oncol 36(22):2326
Molto A, Dougados M (2014) Comorbidity indices. Clin Exp Rheumatol 32(5 Suppl 85):131–134
Mörgeli R, Wollersheim T, Spies C, Balzer F, Koch S, Treskatsch S (2017) How to reduce the rate of postoperative complications in frail patients? Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie: AINS 52(11–12):785–797
Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E (2016) Endometrial cancer. The Lancet 387(10023):1094–1108
Quaglia A et al (2009) The cancer survival gap between elderly and middle-aged patients in Europe is widening. Eur J Cancer 45(6):1006–1016
Rauh-Hain JA et al (2015) Management for elderly women with advanced-stage, high-grade endometrial cancer. Obstet Gynecol 126(6):1198–1206
Revenig LM et al (2014) A prospective study examining the association between preoperative frailty and postoperative complications in patients undergoing minimally invasive surgery. J Endourol 28(4):476–480
Robinson TN et al (2011) Accumulated frailty characteristics predict postoperative discharge institutionalization in the geriatric patient. J Am Coll Surg 213(1):37–42
Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC Jr, Moss M (2013) Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 206(4):544–550
Rodin MB, Mohile SG (2007) A practical approach to geriatric assessment in oncology. J Clin Oncol 25(14):1936–1944
Rodríguez-Mañas L et al (2013) Searching for an operational definition of frailty: a Delphi method based consensus statement. The frailty operative definition-consensus conference project. J Gerontol a: Biomed Sci Med Sci 68(1):62–67
Rothenberg KA et al (2019) Association of frailty and postoperative complications with unplanned readmissions after elective outpatient surgery. JAMA Netw Open 2(5):e194330–e194330
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56(6):M366–M372
Saklad M (1941) Grading of patients for surgical procedures. J Am Soc Anesthesiologists 2(3):281–284
Schmidmayr M, Dorn J (2021) "Gebärmutterkrebs–Prävalenz, Bedeutung und Implikationen für die Prävention und Gesundheitsförderung. Prävention und Gesundheitsförderung. Springer, pp 777–785
Sorosky JI (2012) Endometrial cancer. Obstet Gynecol 120(2):383–397
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 71(3):209–249
Takahashi M et al (2017) The G8 screening tool enhances prognostic value to ECOG performance status in elderly cancer patients: a retrospective, single institutional study. PLoS ONE 12(6):e0179694
Vellas B et al (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15(2):116–122
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 85:867–872
W. H. Organization (2004) The International Statistical Classification of Diseases and Health Related Problems ICD-10: Tenth Revision. Volume 1: Tabular List. World Health Organization
Funding
Open Access funding enabled and organized by Projekt DEAL. This study received no external funding.
Author information
Authors and Affiliations
Contributions
Design of the work: KA and MJB. Data acquisition: KA, MJB, FF, MWS, RS, MS, SK, CW, CE, KE, WB, and AH. Data analysis: KA, MJB and CR. Writing of paper: KA and MJB. All authors critically and substantively revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Katharina Anic reports speaker Honoria from Roche Pharma AG and Clovis Oncology. Slavomir Krajnak received speaker Honoria, research funding and travek reimbursement from Vovartis Pharma GmbH Germany. Roxana Schwab reports honoraria and expenses from Roche Pharma AG and AstraZeneca GmbH. Marcus Schmidt reports personal fees from AstraZeneca, BioNTech, Daiichi Sankyo, Eisai, Lilly, MSD, Novartis, Pantarhei Bioscience, Pfizer, Roche, and SeaGen outside the submitted work. Institutional research funding from AstraZeneca, BioNTech, Eisai, Genentech, German Breast Group, Novartis, Palleos, Pantarhei Bioscience, Pierre Fabre, and SeaGen. In addition, M.S. has a patent for EP 2390370 B1 issued and a patent for EP 2951317 B1issued. Annette Hasenburg reports honoraria and expenses from AstraZeneca, FBA Frauenärzte BundesAkademie GmbH, KlarigoVerlag, MedConcept, Med public GmbH, Med update GmbH, Medicultus, Pfizer, Promedicis GmbH, Pierre Fabre Pharma GmbH, Softconsult, Roche Pharma AG, Streamedup! GmbH, Tesaro Bio Germany GmbH. I am consultant to PharmaMar, Promedicis GmbH, Pierre Fabre Pharma GmbH, Roche Pharma AG and Tesaro Bio Germany GmbH. I have received funded research from Celgene. Marco Battista reports honoraria and expenses from Pharma Mar, Astra Zeneca, Tesaro, GSK, Roche, Clovis Oncology. The other authors state that no conflicts of interests are to declare.
Ethical approval
The retrospective cohort study will be conducted in accordance with the “Ethical principles for medical research involving human subjects” of the current version of the Declaration of Helsinki. Data collected for this study were obtained as part of routine medical care. Ethical approval for use of these samples for research purposes was not required for this study in accordance with local/ national guidelines. Written informed consent from participants was required in accordance with local/national guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Anic, K., Flohr, F., Schmidt, M.W. et al. Frailty assessment tools predict perioperative outcome in elderly patients with endometrial cancer better than age or BMI alone: a retrospective observational cohort study. J Cancer Res Clin Oncol 149, 1551–1560 (2023). https://doi.org/10.1007/s00432-022-04038-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04038-6