Abstract
Purpose
Neuroblastoma (NB) is the most frequent extracranial tumor in children. The detection of bone marrow (BM) involvement is crucial for correct staging and risk-adapted treatment. We compared three methods regarding the detection of NB involvement in BM.
Methods
Eighty-one patients with NB were included in this retrospective study. BM samples were obtained at designated time points at study entry and during treatment or follow-up. The diagnostic tools for BM analysis included cytomorphology (CM), flow cytometry (FCM) and automatic immunofluorescence plus fluorescence in situ hybridization (AIPF).
Results
We analyzed 369 aspirates in 81 patients in whom AIPF, CM, and FCM were simultaneously available. During the observation period, NB cells were detected in 86/369 (23.3%) cases, by CM in 32/369 (8.7%), by FCM in 52 (14.1%), and by AIPF in 72 (19.5%) samples. AIPF and/or FCM confirmed all positive results obtained in CM and detected 11 additional positive BM aspirates in 294 CM negative samples (p < 0,001). Survival of patients with BM involvement at study entry identified solely by FCM/AIPF was 17.4% versus 0% for patients in whom BM involvement was already identified by CM.
Conclusion
The combination of AIPF/FCM yielded the highest detection rate of NB cells in BM. AIPF was the single, most sensitive method in detecting these cells. Although CM did not provide any additional positive results, it is still a useful, readily available and cost-effective tool. The prognostic significance of FCM and AIPF should be confirmed in a prospective study with a larger number of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroblastoma (NB) is the most frequent solid malignancy of childhood outside the central nervous system and represents a biologically heterogeneous group of embryonic tumors arising either from the adrenal gland or primitive sympathetic ganglion cells. The highest incidence is observed in children below the age of 4 years (Schleiermacher et al. 2014; Brodeur and Bagatell 2014; Matthay et al. 2016).
Precise knowledge about the tumor´s characteristics and dissemination is crucial for risk-adapted treatment (Terzic et al. 2017). Neuroblastoma often presents with multilocular bone marrow (BM) involvement that may be difficult to detect as the amount of BM infiltrating tumor cells is usually below 30%, even at diagnosis (Abbasi et al. 2015). Different methods for assessing BM involvement are available either by analyzing the tumor cells by morphological or immunocytological techniques or indirectly, for instance by quantification of NB specific RNA molecules (Beiske et al. 2009; Morandi et al. 2015). Cytomorphological evaluation by light microscopy offers the advantage of being rapidly available and cost-efficient. Obtaining two BM aspirates and two trephine biopsies is currently considered the standard procedure (Burchill et al. 2017), as former studies have demonstrated that the combination of these two methods has yielded the highest rate of detection of NB cells in BM (Franklin and Pritchard 1983; Aronica et al. 1998). However, gaining adequate trephine biopsies particularly in small children can be difficult (Reid and Roald 1999; Morotti et al. 2016; Burchill et al. 2017). In the past few years, immunologically based methods for assessing BM involvement in NB have increased the spectrum of diagnostic tools (Ambros et al. 2003; Morandi et al. 2015; Druy et al. 2018; Popov et al. 2019).
In this retrospective single-center cohort study in a large German pediatric institution specialized in NB research and treatment, three different methods of BM investigation were compared to identify the most sensitive set of tools for the detection of NB in BM.
Materials and methods
Study population
From July, 2009, until April, 2015, 81 patients with NB were referred to the pediatric oncology department at the University Medical Center Greifswald. All patients were to receive either i) immune therapy with dinutuximab beta or ii) salvage chemotherapy after standard first-line or relapse treatment for NB according to the respective national or international protocols or iii) both treatment approaches. Patients were excluded from the analyses if during the observation period BM samples were not consistently investigated by cytomorphology (CM), flow cytometry (FCM) and automated immunofluorescence plus FISH (AIPF).
Diagnostic workups were performed before study entry and repeated every 3–4 months at defined time points according to the respective trial protocol. Each diagnostic procedure included assessment of BM involvement with different methods and imaging studies as outlined below.
The patient disease stage and risk group at diagnosis was determined according to the International Neuroblastoma Staging System (INSS) and the International Risk Group (INRG) classification system (Brodeur et al. 1993; Cohn et al. 2009; Tolbert and Matthay 2018; Sokol and Desai 2019). According to the results of the initial diagnostic procedure, patients were either defined to be in complete remission or with evidence of neuroblastoma disease. Considering survival, the most recent data were collected on September 30, 2020.
For each patient, informed consent was obtained from parents or guardians.
Diagnostic procedures
123 I-mIBG-scintigraphy
123I-mIBG-scans were performed according to the guidelines of the European Association of Nuclear Medicine (EANM). The isotope iodine 123 (123I) was applied according to the dosage card version 01.05.2008 from the EANM. The scans were reviewed by senior physicians at the department of nuclear medicine at University Medicine Greifswald.
Magnetic resonance imaging (MRI) with and without gadolinium
Two different MR scanners, the Siemens MAGNETOM Aera 1.5 Tesla and the Siemens MAGNETOM Symphony 1.5 Tesla were used. Experienced pediatric radiologists reviewed the MRI scans. All scans were presented and discussed in institutional tumor board meetings.
Bone marrow assessment
Due to the heterogeneous distribution of NB cells in the BM, material from at least two different sites of the pelvic bone (mostly posterior iliac crest) was obtained under general anesthesia. BM involvement was regarded as positive if at least one of the methods described below revealed the presence of NB cells. Except for AIPF (CCRI, St. Anna Children’s Cancer Research Institute, Labdia, Labordiagnostik GmbH, Vienna, Austria), all diagnostic tests were performed in specialized laboratories and departments at University Medicine Greifswald, Germany.
Cytomorphology of BM smears by light microscopy
At least 10 smears were obtained from each puncture site. Bone marrow was spread out on slides and prepared with Pappenheim`s staining procedure. In search of single NB cells or tumor nests, 2 × 200 cells were counted on an Olympus BX53 microscope. An experienced and licensed medical-technical assistant examined all slides. Findings were reviewed by at least one pediatric oncologist. The pediatric hematologic-oncologic laboratory subjects itself to yearly quality assurance procedures.
Flow cytometry (FCM)
After aspiration BM samples were stained with monoclonal murine antibodies. FCM analyses were performed on a Bioscience BD FCM Calibur dual laser. In each sample, 2—2.5 × 105 events were analyzed. The analyzing software was BD CellQuest Pro and WinList 3.2. Gated cells were positive for CD56 and disialoganglioside GD2 and negative for CD3 and CD45 (Beiske et al. 2005). Neuroblastoma BM involvement was regarded to be present if > / = 0.01% among all nucleated cells were CD56/GD2 positive. The FCM laboratory takes part in yearly routine quality management procedures.
Automatic immunofluorescence plus FISH (AIPF)
Cytospin preparations of BM mononuclear cells (MNC) were subjected to AIPF, a combined immunocytologic/cytogenetic method to detect minimal residual disease (MRD). The immunocytological and cytogenetic method of Ambros and Méhes is using GD2 and CD56 antibodies to bind to tumor cells, which is visualized and quantified using an automated slide scanning microscope and the RC-Detect Software (both by Metasystems) (Méhes et al. 2001, 2003; Ambros et al. 2003). In cases with less than three GD2/CD56 positive cells per 1 × 106 mononuclear cells (MNC) detected or in cases with unclear results, the suspicious cells were scrutinized with interphase Fluorescent in Situ Hybridization (iFISH).
Besides detecting CD56/GD2 positive cells with a sensitivity of one tumor cell per 1 × 106 MNCs, the presence of e.g. amplified MYCN copies, 17q gain and aneusomies of chromosomes or chromosome arms can be detected to verify immunofluorescence positive cells. More than 106 nucleated cells can be analyzed in one sample (Beiske et al. 2005). The analysis of 3 × 106 MNCs is recommended (Beiske et al. 2005). Samples from different aspiration sites were analyzed separately. AIPF results are available within 48 h after sampling. The laboratory is certified by the International Organization for Standardization, ISO 9001.
Tumor board meetings
The patient disease status and further diagnostic and therapeutic measures were discussed at weekly, interdisciplinary tumor board meetings.
Statistics
For statistical analysis, Pearson´s Chi-squared test was conducted to compare the results of the different methods for BM assessment. P values were adjusted by the Benjamini–Hochberg method (Benjamini et al. 2017; Jafari and Ansari-Pour 2019) to correct for multiple testing. P values lower than 0.05 were considered statistically significant. Every plausible combination of BM study was analyzed through cross-tabulations. For statistical analysis, we used GraphPad software QuickCalcs, 2018 version, and R, 3.6.3 version. Survival of the patients was related to the overall status of disease and particularly to the results of BM involvement at study entry.
Results
Patient characteristics
Between July 2009, and April 2015, 81 patients with NB fulfilling the criteria mentioned above were treated at our institution. Sixty-two received anti-GD2 based immune therapy with dinutuximab beta, three patients received salvage chemotherapy and 16 patients had treatment with both dinutuximab beta and chemotherapy. At diagnosis, 72 patients (88.9%) were classified as high-risk and six (7.4%) as intermediate risk according to the INRG classification system. In three patients the INRG system was not applicable due to missing data. Stage 4 NB was diagnosed in 73 (90.1%) and stage 3 NB in eight (9.9%) patients. MYCN amplification was present in 25 (30.9%) and absent in 44 (54.3%) tumors. The MYCN status was unknown in twelve (14.8%) tumors. At the start of the observation period, 18 (22.2%) patients were in complete remission and 63 (77.8%) patients had measurable disease (Table 1).
For analysis, 369 BM aspirates were obtained and analyzed with CM, FCM and AIPF. Due to the limited number of trephine biopsies, these were excluded from statistical analyses.
The evaluation procedures also included MRI and scintigraphy. In total, 361 mIBG and 354 MRI scans were performed (Table 1).
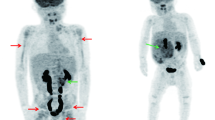
Overall BM involvement in NB
At the patients´ first BM assessment, NB cells were found in 32/81 (39.5%) aspirates. During the observation period in our institution, four different conditions regarding BM involvement were identified: (i) five patients with initially negative BM who occasionally developed BM involvement; (ii) 44 patients who never presented with NB cells in BM; (iii) 11 patients who were permanently positive for NB cells in BM, and (iv) 21 patients in whom NB cells in BM were absent in some, but not in all assessment time points during treatment (Fig. 1). At the patients´ final assessment, NB BM involvement was proven in 18/78 (23.1%) patients. Sixteen of these 18 patients did not survive. Three patients did not have a final BM assessment.
Analysis of BM involvement with three different methods
Bone marrow involvement in 369 aspirates was detected by CM in 32 (8.7%) samples, by FCM in 52 (14.1%) samples, and by AIPF in 72 (19.5%) samples.
In each BM aspirate, 400 cells were reviewed by light microscopy. BM samples with reduced cellularity were found in 37.4%. In 22/32 CM positive samples, more than 1% NB cells were detected. The highest single rate of BM infiltration in a sample was 90%. Cytomorphology was reviewed as negative in 91.3%.
By flow cytometry, 2–2.5 × 105 cells were analyzed in each sample. In 52 positive BM samples, the average rate of NB cells was 1.28% (range 0.01–28.3%, median 0.045%).
The mean number of cells analyzed by AIPF was 4.26 × 106 (range 0.22–9.78, median 4.12). In 72 NB positive samples, the average number of analyzed cells was 3.3 × 106 (range 0.22–9.78, median 2.88). The mean NB cell content in the positive samples was 6.29% (range 0.000012–94.5%, median 0.0067%).
Comparison of FCM with AIPF
Results of FCM and AIPF were available at the same time points in 369 BM samples. Neuroblastoma cells were identified in 86 (23.3%) of these aspirates. FCM and AIPF were simultaneously positive in 38/86 (44.2%) samples. In 34 samples, only AIPF revealed a positive result, in 14 samples only FCM.
When NB cells in BM were detected by FCM, according results with AIPF were obtained in 38/52 samples (73.1%). In 12/14 differing results, the degree of BM infiltration was 0.01% or less.
When NB cells in BM were detected by AIPF, according results with FCM were obtained in 38/72 samples (52.8%). In 34 differing results, the degree of BM infiltration was even lower and on average 0.0028% (median 0.00039%).
Cytomorphology compared to FCM and AIPF
With CM, 337/369 (91.3%) of samples were rated negative. Of these 369 samples, AIPF was negative in 297 (80.5%) and FCM in 317 (86%) samples. Positive results with CM were consistently confirmed by AIPF and/or FCM. In addition, AIPF or FCM identified 54 additional cases of sub-microscopic BM infestation in these 337 cytomorphological negative samples.
In 321 samples, results of CM were compared with the results of the immunological methods FCM and AIPF, when these were either both negative or both positive. FCM and AIPF confirmed all 27 CM positive samples and detected eleven additional BM aspirates with NB cells. In those eleven samples, the degree of BM infiltration was low with a median of 0.02% and a mean of 0.11%. In the 27 positive samples, BM infiltration was higher with a median of 0.5%. Cytomorphology was never positive, when FCM and AIPF were negative. These results were statistically significant (Table 2).
Association of MRI/mIBG with BM studies
There were 369 assessment time points with either mIBG or MRI in combination with BM aspirates. In 136/443 (36.9%), there was no evidence of NB using all diagnostic tools. In 194 MRI and/or mIBG scans with evidence of disease, CM did not contribute additional information as FCM and/or AIPF confirmed all positive results obtained by CM. Furthermore, NB cells were identified by FCM and AIPF in 11 additional CM negative BM samples. These results were statistically significant (Table 3). MRI and mIBG yielded no evidence of disease in 143 assessments. In 7 of these samples, NB cells were identified in BM either by FCM (4), or by AIPF (3) but not by CM.
Survival
Data on survival were available for 76 patients. Forty-six of 81 (56.8%) patients died of NB, 30 (37%) former study patients are alive with and without residual disease. In five patients from abroad, the current status remains unknown.
All eleven patients with NB cell involvement in the BM during the entire study period did not survive. Nine of nine patients did not survive when NB cells in BM were initially detected by CM. In 23 patients, BM involvement at study entry was only identified by FCM or AIPF. Of these, four (17.4%) are alive, 18 (78.3%) did not survive, and one patient was lost to follow-up.
Discussion
Bone marrow involvement in children with NB occurs in about 50%. However, in patients with high-risk or metastatic disease BM involvement may be detected in up to 80% of patients (Tolbert and Matthay 2018). Using highly sensitive techniques, BM involvement at diagnosis was found in even more than 90% of stage 4/M patients (Méhes et al. 2001). Earlier studies compared the use of BM aspirates with trephine biopsies and concluded that the highest yield of detection was reached with the combination of both procedures and that BM trephines are slightly more sensitive than aspirates (Favrot et al. 1986; Mills and Bird 1986; Aronica et al. 1998). The German trial NB 2004 recommended performing either four aspirates from four different sites or two aspirates plus two trephine biopsies in case the aspirates did not appear to be representative (Berthold 2004). In the past two decades, immunologically based methods for assessing BM involvement in NB have widened the spectrum of diagnostic tools (Ambros et al. 2003; Méhes et al. 2003; Beiske et al. 2005; Morandi et al. 2015; Druy et al. 2018; Popov et al. 2019).
In this retrospective, single-center study in one of the largest NB research and treatment institutions in Germany, we compared the results of three different methods for the detection of NB cells in BM in 81 patients. These included CM, FCM and AIPF. This combination of BM analysis has been the standard approach in our institution for more than ten years.
BM cellularity was reduced in 37.4% of the aspirates. This is likely due to the fact that all patients had undergone numerous, previous therapies before treatment in our institution. Nevertheless, a high number of cells were available for analysis. NB cells in BM were most often detected by AIPF (19.5%), followed by FCM (14.1%) and CM (8.7%). During the observation period, the number of patients with BM involvement decreased from 39.5% to 23.1%.
BM infiltration detected by FCM was in a range of 0.01–28.3% (median 0.045%) and by AIPF in a range of 0.000012–94.5% (median 0.0067%) and thus in most samples in a sub-microscopic level of detection. This is supported by the finding that FCM and AIPF were able to identify additional BM samples with NB in aspirates which were unremarkable in light microscopy.
Staining of BM smears for CM is a simple procedure that is well established and widely available (Méhes et al. 2001). However, the microscopic investigation of BM smears is time-consuming, and the interpretation depends on the quality and representativeness of the sample, which may be limited in patients who have been heavily pretreated with chemotherapy (Méhes et al. 2003; Burchill et al. 2017; Popov et al. 2019). Another critical point is the examiner's experience, which may be less outside oncology centers than in experienced laboratories (Reid and Roald 1996). In addition, CM is only able to detect NB cells when BM infiltration exceeds the submicroscopic level (Cheung et al. 1997). Here, we did not systematically re-evaluate all CM-negative BM samples if they were found positive by AIPF, as the samples had already primarily been assessed by two independent, experienced BM morphologists. However, CM negativity was confirmed when selected AIPF-positive samples were re-examined by light microscopy.
FCM and AIPF did not show consistent results in each sample. Inconsistencies were particularly found when the degree of BM infiltration was extremely low in a range of 0.01% or less. As a single method, AIPF identified NB cells most frequently and the combination of AIPF and FCM had the highest yield of detection of NB cells in BM.
In 143 assessments with unremarkable results in MRI and mIBG, we identified only seven BM samples with NB cells (4.9%), and those in fact with FCM and AIPF. In patients, whose tumor treatment has been finished for more than two years, our current algorithm is therefore obtaining BM samples only if there is detectable disease in mIBG/MRI. When the imaging studies reveal unremarkable results, we desist from further invasive diagnostics and procedures involving radiation exposure.
The mortality in the study population was 56.8%. The presence of NB cells in BM identified by CM at study entry reflected a more advanced stage of disease with a poor prognosis. All of these patients did not survive. Mortality was also very high in patients with BM involvement detected only by FCM or AIPF (78.3%) which underlines the importance of these immunological methods.
Retrospective analyses carry several limitations. In recent years, molecular diagnostic tests have also been used to assess the infiltration of NB cells into BM. In 2009, the consensus criteria of the International Neuroblastoma Risk Group Task Force for the detection of NB cells in BM were published (Beiske et al. 2009). Immunocytology for GD2 and reverse transcriptase quantitative polymerase chain reaction (RTqPCR) for tyrosine hydroxylase were recommended. In 2017, the International Neuroblastoma Response Criteria Bone Marrow Working Group recommended the collection of both bilateral BM biopsies and aspirates and their analysis with immunohistochemistry for GD2 and RTqPCR for tyrosine hydroxylase and paired-like homeobox 2B (PHOX2B) (Burchill et al. 2017). Although there may be substantial agreement that biopsies should be added to analysis of BM aspirates, this statement relates to data obtained in the 1980s and 1990s when diagnostic tools to detect minimal disease in aspirates were not well established (Franklin and Pritchard 1983; Verdeguer et al. 1988; Ganick et al. 1988; Thiesse et al. 1991; Hedborg et al. 1992; Brodeur et al. 1993; Monclair et al. 2009). Bone marrow assessment with RTqPCR as recommended by these two guidelines is currently not common clinical practice in Germany. Therefore, a comparison between those approaches and the results of bone marrow assessment analyzed here is not yet possible.
An association of RTqPCR for three different parameters (tyrosine hydroxylase, PHOX2B, doublecortin) in BM at diagnosis with poor outcome was shown (Stutterheim et al. 2008; Viprey et al. 2014). However, the authors also stated that the results of trephine biopsies did not contribute additional information. Its sensitivity is limited and cytology and histology cannot demonstrate sub-microscopic involvement of the BM (Cheung et al. 1997; Stutterheim et al. 2008). Due to the limited number of trephine biopsies obtained in our patients, these were excluded from further analysis.
In summary, AIPF proved to be the single most sensitive method for the detection of BM involvement in NB. The presence of NB cells in BM only detected by AIPF or FACS was able to identify a high-risk population with a poor survival of only 17.4%. Since these are the results of a retrospective study, the diagnostic value and the prognostic significance of FCM and AIPF should be confirmed in a prospective study with a larger number of patients.
Conclusion
The combined use of AIPF and FCM in BM aspirates resulted in the highest detection rate of NB cells. Cytomorphology has the advantage of being quickly available and inexpensive and should therefore not be abandoned. Given these results, the current procedures for assessing the involvement of BM in patients with NB may safely be reduced to CM, FCM, and AIPF. Further studies are needed to clarify the comparative role of AIPF/FCM and PCR-based methods in assessing BM involvement in patients with NB and its relevance to disease control and outcome.
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Code availability
Not applicable.
References
Abbasi MR, Rifatbegovic F, Brunner C et al (2015) Bone marrows from neuroblastoma patients: an excellent source for tumor genome analyses. Mol Oncol 9:545–554. https://doi.org/10.1016/j.molonc.2014.10.010
Ambros PF, Mehes G, Ambros IM, Ladenstein R (2003) Disseminated tumor cells in the bone marrow-chances and consequences of microscopical detection methods. Cancer Lett 197:29–34. https://doi.org/10.1016/S0304-3835(03)00078-8
Aronica PA, Pirrotta VT, Yunis EJ, Penchansky L (1998) Detection of neuroblastoma in the bone marrow: biopsy versus aspiration. J Pediatr Hematol Oncol 20:330–334. https://doi.org/10.1097/00043426-199807000-00010
Beiske K, Ambros PF, Burchill SA et al (2005) Detecting minimal residual disease in neuroblastoma patients-the present state of the art. Cancer Lett 228:229–240. https://doi.org/10.1016/j.canlet.2005.02.053
Beiske K, Burchill SA, Cheung IY et al (2009) Consensus criteria for sensitive detection of minimal neuroblastoma cells in bone marrow, blood and stem cell preparations by immunocytology and QRT-PCR: recommendations by the international neuroblastoma risk group task force. Br J Cancer 100:1627–1637. https://doi.org/10.1038/sj.bjc.6605029
Benjamini Y, Hochberg Y, Chen S-Y et al (2017) A general introduction to adjustment for multiple comparisons. J Thorac Dis 9:1725–1729. https://doi.org/10.21037/jtd.2017.05.34
Berthold F (2004) NB2004 trial protocol for risk adapted treatment of children with neuroblastoma. Version 1, 2004:25
Brodeur GM, Bagatell R (2014) Mechanisms of neuroblastoma regression. Nat Rev Clin Oncol 11:704–713. https://doi.org/10.1038/nrclinonc.2014.168
Brodeur GM, Pritchard J, Berthold F et al (1993) Revisions of the international criteria for neuroblastoma diagnosis, staging, and response to treatment. J Clin Oncol 11:1466–1477. https://doi.org/10.1200/JCO.1993.11.8.1466
Burchill SA, Beiske K, Shimada H et al (2017) Recommendations for the standardization of bone marrow disease assessment and reporting in children with neuroblastoma on behalf of the international neuroblastoma response criteria bone marrow working group. Cancer 123:1095–1105. https://doi.org/10.1002/cncr.30380
Cheung NK, Heller G, Kushner BH et al (1997) Detection of metastatic neuroblastoma in bone marrow: when is routine marrow histology insensitive? J Clin Oncol 15:2807–2817. https://doi.org/10.1200/JCO.1997.15.8.2807
Cohn SL, Pearson AD, London WB et al (2009) The international neuroblastoma risk group (INRG) classification system: an INRG task force report. J Clin Oncol 27:289–297. https://doi.org/10.1200/JCO.2008.16.6785
Druy AE, Shorikov E, Tsaur GA et al (2018) Prospective investigation of applicability and the prognostic significance of bone marrow involvement in patients with neuroblastoma detected by quantitative reverse transcription PCR. Pediatr Blood Cancer 65:e27354. https://doi.org/10.1002/pbc.27354
Favrot MC, Frappaz D, Maritaz O et al (1986) Histological, cytological and immunological analyses are complementary for the detection of neuroblastoma cells in bone marrow. Br J Cancer 54:637–641. https://doi.org/10.1038/bjc.1986.220
Franklin IM, Pritchard J (1983) Detection of bone marrow invasion by neuroblastoma is improved by sampling at two sites with both aspirates and trephine biopsies. J Clin Pathol 36:1215–1218. https://doi.org/10.1136/jcp.36.11.1215
Ganick DJ, Silverman JF, Holbrook CT et al (1988) Clinical utility of fine needle aspiration in the diagnosis and management of neuroblastoma. Med Pediatr Oncol 24:327. https://doi.org/10.1016/S0022-3468(89)80079-X
Hedborg F, Lindgren PG, Johansson I et al (1992) N-myc gene amplification in neuroblastoma: a clinical approach using ultrasound guided cutting needle biopsies collected at diagnosis. Med Pediatr Oncol 20:292–300. https://doi.org/10.1002/mpo.2950200405
Jafari M, Ansari-Pour N (2019) Why, when and how to adjust your P values? Cell J 20:604–607. https://doi.org/10.22074/cellj.2019.5992
Matthay KK, Maris JM, Schleiermacher G et al (2016) Neuroblastoma. Nat Rev Dis Prim 2:16078
Méhes G, Luegmayr A, Ambros IM et al (2001) Combined automatic immunological and molecular cytogenetic analysis allows exact identification and quantification of tumor cells in the bone marrow. Clin Cancer Res 7:1969LP – 1975
Méhes G, Luegmayr A, Kornmüller R et al (2003) Detection of disseminated tumor cells in neuroblastoma: 3 log improvement in sensitivity by automatic immunofluorescence plus FISH (AIPF) analysis compared with classical bone marrow cytology. Am J Pathol 163:393–399. https://doi.org/10.1016/S0002-9440(10)63669-3
Mills AE, Bird AR (1986) Bone marrow changes in neuroblastoma. Pediatr Pathol 5:225–234. https://doi.org/10.3109/15513818609041204
Monclair T, Brodeur GM, Ambros PF et al (2009) The international neuroblastoma risk group (INRG) staging system: an INRG task force report. J Clin Oncol 27:298–303. https://doi.org/10.1200/JCO.2008.16.6876
Morandi F, Corrias MV, Pistoia V (2015) Evaluation of bone marrow as a metastatic site of human neuroblastoma. Ann N Y Acad Sci 1335:23–31. https://doi.org/10.1111/nyas.12554
Morotti A, Barozzino MC, Guerrasio A (2016) Rare bone marrow biopsy complication: a challenging case of sacroiliitis and staphilococcus aureus sepsis. Clin Pract 6:823. https://doi.org/10.4081/cp.2016.823
Popov A, Druy A, Shorikov E et al (2019) Prognostic value of initial bone marrow disease detection by multiparameter flow cytometry in children with neuroblastoma. J Cancer Res Clin Oncol 145:535–542. https://doi.org/10.1007/s00432-018-02831-w
Reid MM, Roald B (1996) Central review of bone marrow biopsy specimens from patients with neuroblastoma. J Clin Pathol 49:691–692. https://doi.org/10.1136/jcp.49.8.691
Reid MM, Roald B (1999) Deterioration in performance in obtaining bone marrow trephine biopsy cores from children. European neuroblastoma study group. J Clin Pathol 52:851–852. https://doi.org/10.1136/jcp.52.11.851
Schleiermacher G, Janoueix-Lerosey I, Delattre O (2014) Recent insights into the biology of neuroblastoma. Int J Cancer 135:2249–2261. https://doi.org/10.1002/ijc.29077
Sokol E, Desai A (2019) The evolution of risk classification for neuroblastoma. Children 6:27. https://doi.org/10.3390/children6020027
Stutterheim J, Gerritsen A, Zappeij-Kannegieter L et al (2008) PHOX2B is a novel and specific marker for minimal residual disease testing in neuroblastoma. J Clin Oncol 26:5443–5449. https://doi.org/10.1200/JCO.2007.13.6531
Terzic T, Cordeau M, Herblot S et al (2017) Expression of disialoganglioside (GD2) in neuroblastic tumors: a prognostic value for patients treated with anti-GD2 immunotherapy. Pediatr Dev Pathol 21:355–362. https://doi.org/10.1177/1093526617723972
Thiesse P, Kaemmerlen P, Bouffet E et al (1991) Percutaneous fine needle guided biopsies of the primary tumor in extensive neuroblastoma. Prog Clin Biol Res 366:503–507
Tolbert VP, Matthay KK (2018) Neuroblastoma: clinical and biological approach to risk stratification and treatment. Cell Tissue Res 372:195–209. https://doi.org/10.1007/s00441-018-2821-2
Verdeguer A, Castel V, Torres V et al (1988) Fine-needle aspiration biopsy in children: experience in 70 cases. Med Pediatr Oncol 16:98–100. https://doi.org/10.1002/mpo.2950160206
Viprey VF, Gregory WM, Corrias MV et al (2014) Neuroblastoma mRNAs predict outcome in children with stage 4 neuroblastoma: a European HR-NBL1/SIOPEN study. J Clin Oncol 32:1074–1083. https://doi.org/10.1200/JCO.2013.53.3604
Acknowledgements
The authors wish to thank Andrea Plath, Sascha Troschke-Meurer, Marcus Vollmer and Andreas Zinke for their support und discussions.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
FS collected and analyzed all data, performed the statistics, drafted the initial manuscript, and reviewed the final version. ST, MB, NS, PA, IA and UG were involved in data collection and reviewed the manuscript. HL and KE conceptualized and designed the study. KE, GH and FS supervised the data collection, reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Informed consent
Written informed consent was obtained from all patients, their legal guardians or parents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schriegel, F., Taschner-Mandl, S., Bernkopf, M. et al. Comparison of three different methods to detect bone marrow involvement in patients with neuroblastoma. J Cancer Res Clin Oncol 148, 2581–2588 (2022). https://doi.org/10.1007/s00432-021-03780-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03780-7