Abstract
Purpose
This study aimed to retrospectively evaluate the genetic association of null variants of glutathione S-transferases GSTM1 and GSTT1 with relapse incidence in children with hematological malignancies (HMs) undergoing busulfan (BU)- containing allogeneic hematopoietic stem cell transplantation (HSCT) and to assess the impact of these variants on BU-induced cytotoxicity on the immortalized lymphoblastoid cell lines (LCLs) and tumor THP1 GST gene-edited cell models.
Methods
GSTM1- and GSTT1-null alleles were genotyped using germline DNA from whole blood prior to a conditioning BU-based regimen. Association of GSTM1- and GSTT1-null variants with relapse incidence was analyzed using multivariable competing risk analysis. BU-induced cell death studies were conducted in GSTs- null and non-null LCLs and CRISPR–Cas9 gene-edited THP1 leukemia cell lines.
Results
Carrying GSTM1/GSTT1 double null genotype was found to be an independent risk factor for post-HSCT relapse in 86 children (adjusted HR: 6.52 [95% Cl, 2.76–15.42; p = 1.9 × 10–5]). BU-induced cell death preferentially in THP1GSTM1(non−null) and LCLsGSTM1(non−null) as shown by decreased viability, increased necrosis and levels of the oxidized form of glutathione compared to null cells, while GSTT1 non-null cells showed increased baseline proliferation.
Conclusion
The clinical association suggests that GSTM1/GSTT1 double null genotype could serve as genetic stratification biomarker for the high risk of post-HSCT relapse. Functional studies have indicated that GSTM1 status modulates BU-induced cell death. On the other hand, GSTT1 is proposed to be involved in baseline cell proliferation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Survival rates of children with hematological malignancies (HMs) undergoing allogeneic hematopoietic stem cell transplantation (HSCT) have improved over the years achieving 91% estimated 2-year overall survival. The improvement is mainly attributed to reduced HSCT-related toxicity and mortality. The incidence of post-HSCT relapse remains a significant complication and varies from 12 to 33% after 2 years (Peters et al. 2021). Risk factors that influence transplant success are on the one hand host- and disease related, such as disease genetics and remission status before HSCT, and on the other hand, transplant related, such as conditioning regimen and treatment-related toxicities including for example severe graft-versus-host disease (GvHD), sinusoidal obstruction syndrome (SOS), and infections (Barrett and Battiwalla 2010; Hamilton and Copelan 2012; Shah et al. 2014).
A bifunctional alkylating agent busulfan (BU) is still often used in conditioning regimens prior to HSCT in children and adolescents (Philippe et al. 2016) and is commonly administered along with other chemotherapeutics, e.g., cyclophosphamide (CY) and fludarabine (FLU) (Ciurea and Andersson 2009; Hao et al. 2020). At least in acute myeloid leukemia (AML), BU has shown lower long-term adverse effects, consequently replacing total body irradiation (TBI) in the conditioning regimen (Lee et al. 2020). In acute lymphoblastic leukemia (ALL), although the recently published results showed lower rates of relapse after TBI-containing conditioning, the results obtained with BU in association with FLU and thiotepa were encouraging and indicate an opportunity to find genetic subgroups of patients who might benefit from the TBI-free conditioning (Peters et al. 2021).
BU is metabolized via conjugation with glutathione (GSH) in the liver, which is predominantly catalyzed by glutathione S-transferase alpha1 (GSTA1) (Czerwinski et al. 1996). In hematopoietic cells (HCs), where GSTA1 is not expressed (Czerwinski et al. 1997), other GST isoenzymes, particularly Mu1 (GSTM1, 46% of the BU conjugating activity of GSTA1 (Czerwinski et al. 1996)) might play the most important role. The role of GSTT1 in BU conjugation is not yet known, but has been mostly reported to have combined effects with GSTM1 on clinical outcomes (Kim et al. 2011; Myers et al. 2017). In addition to their protective role of the conjugation of BU in HCs, they might contribute to multiple cellular processes such as regulation of cell proliferation and apoptosis through the interaction with protein kinases such as apoptosis signal-regulating kinase 1 (ASK1). Under stress conditions, the interaction of the GSTM1:ASK1 complex is dissociated and results in activation of ASK1 that activates the c-Jun N-terminal kinase (JNK) and mitogen-activated protein kinase p38 (MAPK p38) pathways, leading to upstream cytokine- and stress-induced apoptosis (Board and Menon 2013; Tew and Townsend 2012). However, the impact of apoptosis through kinases on BU-dependent cytotoxicity is poorly understood and even less whether those GST genes naturally knocked down might interfere in the post-HSCT relapse potential.
GSTM1 and GSTT1 genes can be homozygously deleted (presented as GSTM1-null and GSTT1-null) and thus completely deprived of the enzyme activities in a high percentage of individuals (the average % in Europe are 51 and 19, respectively) (Saitou and Ishida 2015). In AML adult patients, Weiss et al. (Weiss et al. 2007) showed a perfect concordance of those variants in malignant and germline DNA, which suggests that the germline genotype drives protein expression in malignant cells. Although these variants have been associated with a higher risk of leukemia development (Li et al. 2018), there are conflicting reports on the association of the GSTM1-null and GSTT1-null variants with relapse in patients with HMs (Balta et al. 2003; Franca et al. 2012; Stanulla et al. 2000; Takanashi et al. 2003). To date, there is no evidence available for the association of germline GSTM1-null and GSTT1-null variants with post-HSCT relapse in children with HMs.
Because GSTM1 and GSTT1 are the main remaining GSTs in HCs, we hypothesized that the absence of either or both proteins should affect BU cytotoxicity through conjugation-dependent or -independent ways, interfering in the HSCT outcomes. Hence, a genetic association study based on germline GSTT1- and GSTM1-null variants was undertaken. Further, we conducted in vitro functional analyses to understand the role of these variants in survival and BU-induced apoptosis and necrosis of the immortalized and tumor lymphoblastoid cell lines (LCLs).
Materials and methods
Clinical association study
Patients and treatment
Pediatric patients with ALL, AML or myelodysplastic syndrome (MDS) who had undergone allogeneic HSCT between 2000 and 2013 were enrolled in the study. The Institutional Review Board or ethics committees approved the study and all patients and/or parents provided informed consent. The present study is a subset of the multicentric study under the umbrella of the European Society for Blood and Marrow Transplantation (EBMT) (Clinicaltrials.gov identifier: NCT01257854) (Ansari et al. 2017).
I.v. BU (Busulfex, Otsuka Pharmaceuticals, Saint-Laurent, Montreal, QC, Canada or Busilvex, Pierre Fabre Laboratory, Paris, France) administration was given as a 2 h infusion to the patients, every 6 h for a total of 16 doses. The first BU dose was age and weight based and pharmacokinetic (PK)-guided dose adjustment was performed to obtain a cumulative area under the curve (CumAUC) between 59.2 and 98.56 mg*h/L as reported previously (Ansari et al. 2017).
The primary diagnosis of HMs was made at the referring institution. Patients were considered to be in remission after chemotherapy if they presented < 5% blasts in the normal cellular bone marrow. Relapse in MDS was defined as > 5% and ≤ 20% of blasts at the bone marrow examination after engraftment and/or reappearance of major dysplastic features associated with cytopenias and/or mixed chimerism > 5% and/or detection of the same cytogenetic abnormality present at diagnosis. Relapse in AML and ALL was defined as the presence of blasts in the bone marrow > 5%, confirmed by flow cytometry; detection of the gene fusion present at diagnosis; or according to minimal residual disease (MRD) results after the transplantation if available. Disease remission status was defined by the number of bone marrow remission or relapse events before HSCT.
Cumulative relapse incidence, event-free survival (EFS), and overall survival (OS) were defined according to the standard guidelines of EBMT and as detailed in our recent report (Ansari et al. 2017). EFS was calculated from the time of transplant until death, relapse, or graft failure, whichever occurred first. OS was calculated from the time of transplant until death from any cause.
Genotyping and statistical analysis
Genotyping of GSTM1-null and GSTT1-null variants was performed on germline DNA, extracted from whole blood or peripheral mononuclear cells of all patients before the first HSCT as described by Lin et al. (1998).
Pearson Chi-square test was used to analyze the differences in demographics between groups with and without GST-null variants. Estimated cumulative relapse incidence by competing risk analysis with non-relapse mortality as a competing event and the difference among groups were estimated by Gray’s test (Gray 1988). The Fine–Gray model was used for competing risk regression in multivariable analysis to obtain adjusted p values for all the variables in relation to the genotype groups (Fine and Gray 1999). The potential risk factors with a p value ≤ 0.25 in the univariable competing risk analysis were retained in the multivariable analysis by including the GST genotype factor with the lowest p value. The final multivariable analysis included: diagnosis (ALL, AML and MDS), disease status [1st complete remission (CR), a higher degree of CRs and absence of CR], conditioning regimen (standard regimen with two alkylating agents and intensified regimen with three alkylating agents), AUC after the first dose of busulfan (1st BU dose AUC categorized into below 3.7, between 3.7 and 6.16, and above 6.16 mg*h/L) and BU CumAUC (below 59.2, between 59.2 and 98.6, and above 98.6 mg*h/L) as categorical variables. Cumulative incidences of OS and EFS were estimated in relation to the genotype groups, using Kaplan–Meier framework and log-rank test. Univariate Cox regression was used to estimate hazard ratios.
All statistical analyses on clinical data were performed using SPSS (RRID: SCR_002865, Version 24.0. Armonk, NY: IBM Corp.) and R Project for Statistical Computing (version 3.6.2, RRID: SCR_001905) with Rcmdr package (version 2.6.1). Statistical power calculations according to GST variants were conducted in G*Power–Statistical Power Analyses for Windows and Mac, version 3.1.9.2 (RRID: SCR_013726; Dusseldorf, Germany).
In vitro functional studies of the associated variants
Cell models design and cell characterization
A set of 56 immortalized non-malignant lymphoblastoid cell lines (LCLs), acquired in 2012 from International HapMap Consortium’s CEPH Families Reference Panel 142,011/147712 (Coriell Cell Repository, Camden, NJ, USA), and a human monocytic leukemia cell line (THP1; acquired in 2018 from ATCC, Cat# TIB-202, RRID: CVCL_0006; Manassas, Virginia, USA), derived from a 1-year-old patient, were used for baseline and BU-induced functional assessment of GSTM1-null and GSTT1-null variants. The cells were immediately stored at − 196 °C and were not used prior to the start of experiments. The cell lines were thawed and cultured in Roswell Park Memorial Institute Medium (RPMI) 1640 medium (Gibco, Carlsbad, CA) supplemented with 10% fetal bovine serum (HyClone, South Logan, UT) and 1% penicillin–streptomycin (Gibco) and incubated at 37 °C, 5% CO2-humidified atmosphere according to the manufacturer’s recommendations. The number of passages between thawing and use in each in vitro experiment achieved the range between 5 and 15 times. The IDs of investigated LCLs used for each particular in vitro experiment are listed in Supplementary Table 1.
THP1 GSTM1- and GSTT1-knockout cell lines (THP1GSTM1(−/−) and THP1GSTT1(−/−)) were prepared from parental THP1 representing non-null genotype for GSTM1 (THP1GSTM1(+/+)) and GSTT1 (THP1GSTT1(+/+)) using CRISPR/Cas9 gene-editing method. Plasmid PX458 containing 5’-TGATACTGGGGTACTGGGAC-3’ gRNA (GSTM1) or 5’-TGAAGGACGGGGACTTCACC-3’ gRNA (GSTT1) (prepared by GeneScript, The Netherlands) was transfected into THP1 cells. 10,000 cells were fluorescence-activated cell sorted (FACS) in 24-well plates based on the presence of green fluorescence protein (GFP) 48 h post-transfection. After 48–72 h of recovery, THP1 cells were single-cell cloned in 96-well plates using FACS. Gene-modified clones were genotyped for the presence of deleterious mutations using Sanger sequencing and confirmed by Western blot for the success of gene knockout. Five clones of the same genotype were pooled in a population.
DNA and proteins of the selected cell lines (LCLs, THP1GSTM1(−/−) and THP1GSTT1(−/−) cell models) were extracted using DNeasy Blood and Tissue Kit (Qiagen, Hilden, Germany) and standard protein extraction protocol for western blot using RIPA lysis buffer (Sigma-Aldrich, Germany), respectively. The intracellular concentration of extracted proteins was measured using Bradford assay from Bio-Rad (Hercules, CA) according to the manufacturer’s recommendations. Aliquots containing 20 μg of proteins, sample reducing agent and LDS sample buffer (Thermo Fisher Scientific, USA) were subjected to electrophoresis by using Invitrogen Novex Tris–Glycine Gels (Thermo Fisher Scientific, USA). Dry transfer to a nitrocellulose membrane was performed with the iBlot dry blotting system (ThermoFisher Scientific, USA). A membrane was blocked using 5% milk in PBS and 0.05% Tween 20. The following primary antibodies were used for protein labeling: ß-Actin Mouse monoclonal antibody (Abcam Cat# ab6276, RRID: AB_2223210); GSTP1 Monoclonal Antibody Rabbit (DSHB Cat# CPTC-GSTP1-1, RRID: AB_2617266); GSTM1 Monoclonal Antibody Mouse (Thermo FisherScientific Cat# MA5-17,085, RRID: AB_2538556) and GSTT1 Polyclonal antibody Rabbit (Thermo FisherScientific Cat# PA5-22,011, RRID: AB_11154445). Lumi-Light WB Substrate (Roche, CH) was used for the detection of the secondary antibody linked with horseradish peroxidase (HRP). Band intensities were identified using Syngene G-Box System (Syngene, Frederick, MD, USA).
The glutathione transferase activity (Glutathione S-transferase [GST] Assay Kit, Sigma-Aldrich, USA) was measured on cell lysates obtained from one million cells (THP1GSTM1(−/−) and THP1GSTM1(+/+)) by measuring absorbance at 340 nm every minute for 10 min in a 200 μl well of a 96-well plate using Spectramax ID3 Multi-Mode microplate reader (Molecular Devices, USA) according to the manufacturer’s recommendations. GST activity was calculated as the following: [Δ340nm (min) * total volume of the reaction (ml)]/[5.3 mM−1 * volume of enzyme] corrected according to the protein concentration in mg/ml obtained by using a Pierce™ BCA Protein Assay Kit (ThermoFisher Scientific, USA) according to the manufacturer’s guidelines.
The results of the characterization of CRISPR–Cas9 THP1 gene-edited cell models with target proteins (GSTM1, GSTT1 and GSTP1) and GST activity are presented in Supplementary Fig. 1 (A–C).
DNA samples from LCLs were genotyped for GSTM1-null and GSTT1-null variants using multiplex real-time PCR amplification in the presence of SYBR Green I and genotype discrimination by melting curve analysis in a StepOnePlus™ Real-Time PCR System (Applied Biosystems™, Foster City, CA, USA) with BCL2 (BCL2 apoptosis regulator) gene as an internal control as described earlier (Marin et al. 2010). The genotyping method used cannot differentiate the heterozygous individuals from homozygous non-null carriers (furtherly marked as GSTM1( +) and GSTT1( +)) except when using Sanger sequencing.
Cell viability, apoptosis, necrosis, GSSG/GSH measurements, and caspase activities
Intracellular ATP concentrations (CellTiter 2.0 Luminescent Cell Viability Assay (Promega Corporation, Madison, WI)) were screened in 56 LCLs and CRISPR–Cas9 gene-edited cell models: THP1GSTM1(−/−), THP1GSTM1(+/+), THP1GSTT1(−/−), THP1GSTT1(+/+); at 48 h of treatment with 100, 200, 400, 800 and 1600 µM concentrations of BU (Sigma-Aldrich, Germany) reconstituted with DMSO (Sigma), 1% of DMSO (as control) and at baseline (medium only). For validation of the first screening, ATP-independent cell viability follow-up (72 h) was performed at BU concentrations of 100, 250 and 500 µM in three GSTM1( +) and four GSTM1(-/-) LCLs (Supplementary Table 1) and at baseline in THP1GSTT1(−/−) and THP1GSTT1(+/+) using RealTime-GloMT Cell Viability Assay (Promega, USA).
Annexin V/PI assay (BD Biosciences) was used to measure live, early and late apoptotic and necrotic cells. Prior to FACS, ten GSTM1( +) and ten GSTM1(-/-) LCLs (Supplementary Table 1) were treated for 48 h with BU (1% DMSO) at 250, 500 and 1000 µM and two samples of each cell line were used as controls (1% DMSO and untreated). One million cells were labeled according to the manufacturer’s protocol. FACS analysis was performed using the CyAN ADP system (Beckman Coulter, UK). Results were analyzed by Kaluza analysis software, version 1.3 (Beckman Coulter, UK). Apoptosis and necrosis were followed for 72 h in six GSTM1( +) and six GSTM1(-/-) LCLs (Supplementary Table 1) treated with 500 µM BU using RealTime-Glo MTAnnexin V Apoptosis and Necrosis Assay (Promega).
Concentrations of the total (GSHT) (GSH-Glo Glutathione Assays, Promega, USA) and oxidized intracellular glutathione (GSSG) (GSH/GSSG-Glo Glutathione Assays, Promega, USA) were measured according to the manufacturers’ recommendations. Prior to measurement, cells from five GSTM1( +) and five GSTM1(−/−) LCLs and CRISPR–Cas9 gene-edited THP1 cell models were incubated for 48 h at 500 µM BU and 1% DMSO (control). Results are expressed as the relative proportion of GSSG to GSHT.
Caspase-Glo 3/7 assay (Promega) was used to measure the total activity of caspases-3 and -7 in a subset of 12 LCLs (Supplementary Table 1) and CRISPR–Cas9 gene-edited THP1 cell models at 48 h BU post-treatment (250, 500 and 1000 μM).
Chemiluminescent signals were measured using Victor3 (Perkin Elmer, Inc., USA). All BU-based data were normalized relative to the negative controls with 1% DMSO.
Statistical analyses in in vitro functional studies
The cell-based experiments (IC50 distribution, end-point apoptosis and necrosis, real-time monitoring of viability, apoptosis and necrosis, Caspase3/7 activities; and [GSSG/GSHT] ratios) were performed at least in duplicate and results are reported as observed means ± SD stratified by GST-null and GST-non-null variants. Statistical differences between genotypes were assessed using Mann–Whitney, t tests, or two-way ANOVA according to the normality of the distribution and compared to untreated controls using GraphPad Prism 7 software (RRID: SCR_002798). We considered p < 0.05 to be statistically significant in all analyses.
Results
GSTM1- and GSTT1-double null genotypes are associated with higher relapse incidence
Eighty-six children with malignancies aged 5 months–18 years (female/male, 44/42), who received myeloablative conditioning containing four-times-daily i.v. BU followed by HSCT, were enrolled in this study. The patients’ baseline characteristics at the time of their HSCT are summarized in Table 1. The number of patients who had experienced relapse was 16 (18.6% of included patients) with the median time to onset 203 days (range 35 to 817) and 12 (14.0%) patients died with the median time to onset 221 days (range 15 to 979). The median CumAUC of BU achieved 56.96 mg*h/L (concentration range 30.50–115.23 mg*h/L).
Regarding the genotype frequency, 49 patients were GSTM1-null (57.0%), 24 GSTT1-null (27.9%) and 9 had null genotypes in both GSTM1 and GSTT1 genes (10.5%). Characteristics of these patients according to GSTM1-null and GSTT1-null variants are shown in Supplementary Table 2.
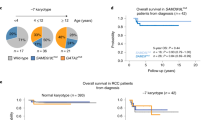
Relapse was associated with GSTT1-null compared to GSTT1-non-null subgroups (42.1% vs 16.1%) in the univariable analysis (p = 0.04, Fig. 1A, Table 2A). The GSTM1-null was not associated with relapse (Fig. 1B, Table 2A). However, patients carrying null genotypes in both GSTM1 and GSTT1 genes showed significantly increased risk of relapse compared to other genotype subgroups ([GSTM1-non-null/GSTT1-non-null, GSTM1-non-null/GSTT1-null and GSTM1-null/GSTT1-non-null]; p = 0.012, Fig. 1C, Table 2A) and this risk remained significant when other genotype subgroups were grouped together (using a gene–gene interaction model; 77.8% vs. 19.0%; p = 0.002, Fig. 1D, Table 2B). Significantly lower EFS was observed in the group of patients carrying (−/−) alleles in both GSTM1 and GSTT1 genes in comparison to others (54.2% vs. 11.1%, p < 0.001, Supplementary Fig. 2A). When gene variants were analyzed independently, none of them affected the EFS (data not presented). OS was not significantly associated with GST-null variants (using gene–gene interaction model; 67,1% vs. 37,0%, p = 0.401, Supplementary Fig. 2B).
Cumulative incidence plots of relapse in univariable competing risk analyses stratified by GST-null variants. Results are plotted for (A) GSTT1(−/−) group versus groups GSTT1( ±) and GSTT1(+ / +) together presented as GSTT1( +); (B) GSTM1(−/−) group versus groups GSTM1( ±) and GSTM1(+ / +) together presented as GSTM1( +); (C) combined GSTM1(−/−)/GSTT1(−/−) versus other genotype combinations [GSTM1(−/−)/GSTT1( +), GSTM1( +)/GSTT1(−/−) and GSTM1( +)/GSTT1( +)]; (D) combined GSTM1(−/−)/GSTT1(−/−) versus grouped other genotype combinations [GSTM1( +)/GSTT1( +)]. p values for the difference in cumulative incidence of relapse were calculated with Gray’s test with death as a competing event. HR, hazard ratio; GSTM1-null and GSTT1-null are presented as GSTM1(−/−) and GSTT1(−/−), respectively. GSTM1 non-null and GSTT1 non-null genotypes are presented as GSTM1( +) and GSTT1( +), respectively
Relapse was compared between GSTM1-null and GSTT1-null variants combined with other possible risk factors (Table 2B). GSTM1/GSTT1 double null status was independently associated with relapse with an HR of 6.52 [95% Cl, 2.76 – 15.42; p = 1.9 × 10–5]. 25%, 9.7% and 23.3% of patients with ALL, MDS and AML, respectively, were relapsed. Among them, all relapsed patients with the GSTT1-null genotype had ALL (Supplementary Table 3).
LCL sensitivity to BU is associated with GSTM1, but not with GSTT1 genotypes
Significantly higher cell viability after treatment with BU was observed in LCLs with GSTM1-null genotype (1.8-fold, p = 0.013) and THP1GSTM1(−/−) cells (1.5-fold, p = 0.0006) compared to GSTM1-non-null by 48 h end point (Fig. 2A, B, respectively) and the results were confirmed by 72-h kinetic measurements in LCLs (Supplementary Fig. 3). GSTT1-null, alone or in combination with GSTM1-null, did not show a significant association with BU-IC50 in LCLs and THP1GSTT1(−/−) cell lines (Fig. 2C, D, respectively). No difference in baseline cell proliferation was seen between GSTM1-null and GSTM1- non-null cells (Fig. 3A), while the proliferation of GSTT1-null cells was significantly decreased in comparison to GSTT1-non-null carriers in LCLs carrying GSTT1-null genotype and THP1GSTT1(−/−) [p = 0.03 (LCL, 48 h end-point measurement, Fig. 3B) and p < 0.05 (THP1GSTT1(−/−), 72 h kinetic plot, Fig. 3C)].
IC50-values for BU in GSTM1-null and GSTT1-null LCLs, THP1GSTM1(−/−) and THP1GSTT1(−/−) cells. IC50 values for BU were stratified according to GSTM1- (A) and GSTT1-null variants (C) in LCLs and CRISPR–Cas9 gene-edited THP1GSTM1(−/−) (B) and THP1GSTT1(−/−) (D) cell models. Concentration–response titration points were fitted to a Hill equation for BU. The 50% inhibitory concentrations of BU (BU-IC50) were determined by dose–response curve fitting using Prism 5.02 software (GraphPad SoftwareInc., CA. USA). The coefficient of determination (R2) of each plate was used to assess experimental reproducibility and was set to be above 0.95. Independent experiments were repeated at least three times. Non-parametric unpaired t test was used in LCLs (A, C). Pairwise comparisons by t test between GST(−/−) variants in THP1-CRISPR–Cas9 models (B., D.) were used. In THP1-CRISPR–Cas9 cell models (B., D.), dots represented are specific clones with identified GST(−/−) variants (+ / + vs. −/−) based on Sanger DNA-sequencing. p values below 0.05 were considered statistically significant. ns, not significant. GSTM1-null and GSTT1-null are presented as GSTM1(−/−) and GSTT1(−/−), respectively. GSTM1 non-null and GSTT1 non-null genotypes are presented as GSTM1( +) and GSTT1( +), respectively
Baseline cell growth against GSTM1-null and GSTT1-null genotypes in LCLs and THP1GSTT1(−/−) cells. Baseline cell growth was assessed against GSTM1-null (A) and GSTT1-null (B) genotypes in LCLs at 48 h end-point analysis and the (C) RealTime Cell Viability assay–Kinetics plot was performed for 72 h stratified by GSTT1-null genotype at baseline (proliferation profile) in THP1GSTT1(−/−) cell models. (A, B) On the y-axis, the basal cell growth rate (r) was calculated using the following formula, appropriate for the usual exponential kinetics of cell growth (N; the number of cells) after the defined time (t; h): Nt = No.2tr. (C) Measurement of baseline reducing the potential of viable cells according to GSTT1(−/−) variant in CRISPR–Cas9 gene-edited cell models was performed. The unpaired t test between GST genotypes in LCLs (A., B.) and Pairwise comparisons by t test between GSTT1 genotypes in THP1-CRISPR–Cas9 models were used. p values below 0.05 were considered statistically significant. GSTM1-null and GSTT1-null are presented as GSTM1(−/−) and GSTT1(−/−), respectively. GSTM1 non-null and GSTT1 non-null genotypes are presented as GSTM1( +) and GSTT1( +), respectively
GSTM1-null genotype is associated with increased apoptosis and decreased primary necrosis after BU treatment
In a subgroup of ten GSTM1-null LCLs, we observed increased early apoptosis and a decreased primary necrosis (p = 0.026 and 0.006, respectively) at 48 h post-treatment with 250, 500 and 1000 µM of BU in comparison to ten GSTM1-non-null LCLs (Fig. 4A–D). No significant differences between both GSTM1 genotype groups were observed for the number of live cells and apoptotic cells at a later stage (the mix of necrotic and real apoptotic cells). Apoptosis was further assessed through measurement of caspase 3/7 activity according to GST(−/−) variants showing significantly higher activation in GSTM1-null LCLs and THP1GSTM1(−/−) at 250, 500 and 1000 µM BU in comparison to GSTM1-non-null cells (p < 0.05; Fig. 4E), while no differences were observed at baseline. BU-induced activation of caspase 3/7 was not significant in GSTT1-null LCLs (p = 0.21), while in THP1GSTT1(−/−) was significantly decreased (p = 0.002; Fig. 4E) in comparison to GSTT1-non-null cells.
Number of necrotic and apoptotic cells in LCLs and caspase 3/7 activity in LCLs, THP1GSTM1(−/−) and THP1GSTT1(−/−) cells. Flow cytometric analysis (FACS) by using Annexin V/PI assay was used to assess primary necrosis (A), late apoptosis (B), live cells (C) and early apoptosis (D) in LCLs stratified according to GSTM1-null variants; and caspase 3/7 activity (E) in LCLs and THP-CRISPR–Cas9 models stratified according to GST-null variants at 250, 500 and 1000 μM BU 48 h post-treatment. Statistical analysis was performed by two-way ANOVA considering 250, 500 and 1000 μM BU concentrations (genotype and treatment factors); t tests between GST(−/−) variants in each condition separately were used; no statistically significant differences were observed between GSTM1 + and GSTM1(−/−) LCLs and THP-CRISPR–Cas9 models in either 1% DMSO or medium only; p values below 0.05 were considered statistically significant. GSTM1-null and GSTT1-null are presented as GSTM1(−/−) and GSTT1(−/−), respectively. GSTM1 non-null and GSTT1 non-null genotypes are presented as GSTM1( +) and GSTT1( +), respectively
Cell death mechanisms were further followed by kinetic plots. We observed higher apoptotic rates in GSTM1-null cells (THP1GSTM1(−/−), LCLs) through the whole 72 h of follow-up after BU treatment when compared to GSTM1-non-null cells from unrelated individuals (Supplementary Figs. 4A and 4C, p < 0.0001 and p = 2.6E-05, respectively). In contrast, we observed lower necrotic rates in GSTM1-null cells (THP1GSTM1(−/−), LCLs) that were increasing after 26 h of BU treatment when compared to GSTM1-non-null cells (Supplementary Figs. 4B, D, p < 0.001 and 1.4E-05, respectively). Apoptosis at the same time points was lower in these cells accounting for the faster cell death, mainly as a result of primary necrosis.
[GSSG/GSHT] ratios are higher in GSTM1-non-null LCLs and THP1GSTM1(+/+) cells after BU treatment compared to GSTM1-null while total GSH levels remain unchanged
At baseline, no differences in [GSSG/GSHT] ratios were observed between null and non-null LCLs and THP1 cells for the GSTM1 gene. However, 48 h after 500 μM BU treatment, [GSSG/GSHT] ratios were increased 1.6- (p = 0.02, LCLs) and 1.3-fold (p = 0.005, THP1) in GSTM1 non-null compared to GSTM1-null (Fig. 5A, C, respectively). A similar trend was observed after the 250 μM BU treatment (48 h) in THP1GSTM1(−/−) in comparison to THP1GSTM1(+/+) cells (Fig. 5C). In THP1, no significant difference was observed according to GSTT1 genotype after the treatment with BU or at baseline (Fig. 5D). In addition, we observed a significant increase in total GSH levels after the 500 μM BU treatment, irrespective of the GSTM1 genotype (Fig. 5B, p=0.001), thus indicating the potential for BU-related induction of GSH synthesis.
Glutathione levels in LCLs stratified according to GSTM1-null variant, THP1GSTM1(−/−) and THP1GSTT1(−/−) cells. [GSSG/GSHT] ratio (A) and GSHT (B) in LCLs were calculated stratified according to GSTM1-null variant; and [GSSG/GSHT] ratios in CRISPR–Cas9 edited THP1GSTM1(−/−) (C) and THP1GSTT1(−/−) (D) cell models after the treatment with 500 μM BU. Statistical analysis was performed by the two-way ANOVA considering 250 or 500 μM BU concentration (genotype factor); t tests between GST(−/−) variants in each condition separately were used; no statistically significant differences were observed between GST(−/−) variants in LCLs and THP-CRISPR–Cas9 models in either 1% DMSO or medium; p values below 0.05 were considered statistically significant. GSTM1-null and GSTT1-null are presented as GSTM1(−/−) and GSTT1(−/−), respectively. GSTM1 non-null and GSTT1 non-null genotypes are presented as GSTM1( +) and GSTT1( +), respectively
Discussion
Our clinical association study performed in 86 children with HMs undergoing HSCT following BU-based conditioning regimens demonstrated that patients harboring homozygous deletions in both GSTM1 and GSTT1 genes presented a high risk of relapse (HRrelapse 7.2 [95% Cl, 2.2–23.9; p = 0.002]) and a lower EFS (HREFS 4.092 [95% Cl, 1.829–9.152; p = 0.001]). After adjustment for known risk factors (diagnosis, disease status, the intensity of conditioning regimen and BU exposure), the association remained significant demonstrating that the deletion of both GST genes is an independent risk factor for relapse (adjusted HR 6.52 [95% CI, 2.8–15.4; p = 1.9 × 10–5]). Although it is a small cohort, this is the first report on the risk of post-HSCT relapse in relation to the germline GSTM1- and GSTT1-null variants in children with HMs. Until now, only one study conducted in BU/CY-based HSCT settings although in adults showed increased relapse rates in patients carrying GSTM1-null genotype, while no association was identified with GSTT1-null genotype (Terakura et al. 2020). Concerning non-transplant-based studies in pediatric or adult patients, a similar association between GSTM1/GSTT1 double null carriers and increased risk of relapse (Barragan et al. 2007; Borst et al. 2012; Takanashi et al. 2003, Xiao Q. et al. 2014), lower complete remission rate (Xiao Z. et al. 2008) and lower EFS were demonstrated (Chen et al. 1997; Hall et al. 1994; Leonardi et al. 2017; Rocha et al. 2005; Stanulla et al. 2000; Takanashi et al. 2003; Teachey and Hunger 2013; Woo et al. 2000; Zhang et al. 2017). There are nevertheless a few studies showing no such association (Franca et al. 2012; Zareifar et al. 2013), in which the small number of patients or the different treatment regimens may have mainly precluded defining a relationship between GST variants.
Based on the known detoxifying role of GSTs, our results from the clinical association are contradictory. Although GSTA1 is the main enzyme involved in BU detoxification, GSTM1 is also highly expressed in the liver and recognized as involved in BU conjugation (Ansari et al. 2017; Bremer et al. 2015; Czerwinski et al. 1996; Kim et al. 2011), precluding the BU to cross-link with the DNA strands. Functional variants of the genes coding for GSTs may then interfere in HSCT by affecting BU metabolism. It is known that low BU exposure (CumAUC < 59 mg × h/L) is associated with graft failure and relapse (Ansari et al. 2017; Bartelink et al. 2016; Philippe et al. 2016), whereas high BU exposure (CumAUC > 98.6 mg × h/L) could reduce post-HSCT relapse in leukemia at the cost of an increase in organ toxicities, and therefore transplantation-related mortality (Ansari et al. 2017; Bartelink et al. 2016; McCune et al. 2002; McCune and Holmberg 2009; Philippe et al. 2016). However, at the level of HCs, less is known about the direct effect of BU.
We compared BU-related cell death mechanisms in LCLs and THP1 with and without GSTM1 and/or GSTT1 genes after exposure to BU. LCLs were chosen as the in vitro model to resemble heterogeneity seen in a clinical cohort. Since each LCL is derived from a different individual genetic background, the studied effect due to BU is specifically related to the GSTM1- and GSTT1-null and –non-null genotypes. The acute monocytic leukemia (THP1) cell model was selected for the production of the CRISPR–Cas9 GSTM1- and/or GSTT1 knockout model, as we have the most patients with a relapsed AML (Supplementary Table 3). Selection of these two cell models aids in evaluating BU-dependent and -independent GSTT1 and GSTM1 effects. We demonstrated that only GSTM1-null (but not GSTT1-null) is associated with higher resistance to BU as determined by higher BU-IC50 values of GSTM1-null LCLs and THP1(GSTM1−/−) in comparison to GSTM1-non-null cells. This could be due to a change in the redox equilibrium as demonstrated by lower levels of oxidized GSH, lower primary necrosis and higher early apoptosis. An increase of GSTM1-null LCL’s viability was confirmed either by continuous follow-up of redox potential within 72 h. Apoptosis/necrosis kinetic results demonstrate that BU-induced apoptotic processes are more pronounced in GSTM1-null LCLs. In contrast, primary necrotic cell death was more pronounced in GSTM1-non-null cells when comparing with the GSTM1-null cells. In addition, primary necrosis was significantly induced at an earlier stage in GSTM1-non-null cells. These results show that GSTM1-null variants can modulate BU-induced cell death, which were supplemented further by increased activation of known apoptotic markers caspase-3 or -7 in GSTM1-null LCLs and THP1 in comparison to GSTM1-non-null cells. Importantly, observed reduced rates of GSTM1-dependent cell death cannot be attributed to the increased baseline cell proliferation.
The findings of higher primary necrosis, lower early apoptosis and lower cell viability in GSTM1-non-null HCs compared to GSTM1-null cells treated with BU were unexpected. Contrary to our observations, many studies showed associations between increased expression or activity of GSTs and resistance mechanisms against a range of cytotoxic drugs (Hoban et al. 1992; Smith et al. 1989). These results could potentially be explained by not only direct detoxification with GSH, but also through negative regulation of pro-apoptotic protein kinases, such as apoptosis signal-regulating kinase 1 (ASK1) (Board and Menon 2013; Tew and Townsend 2012). For instance, stress conditions cause the release of ASK1 from GSTM1, thereby leading to induction of apoptosis, which was shown in our experiments after induction with BU. In addition, GSTM1-null cells carrying more free ASK1 for phosphorylation activation are expected to have more apoptosis upon BU-induced stress in comparison to GSTM1-null cells which is in accordance with our in vitro results.
However, the observed paradox in increased cell death of GSTM1 well-expressed cells upon BU treatment could additionally be explained by findings of the study of DeLeve et al. (2000), demonstrating that in murine hepatocytes BU is cytotoxic also through oxidative stress caused by BU metabolites (BU glutathione S-conjugate thiophenium ion, GS+THT) and by the depletion of GSH in addition to DNA alkylation. The toxic metabolites of BU/GSH metabolism are mainly oxidized by flavin-containing monooxygenases (FMOs, e.g., FMO3) and cytochromes (CYPs, e.g., CYP3A4) (El-Serafi et al. 2017) to water-soluble non-toxic metabolites [e.g., sulfolane (Uppugunduri et al. 2017)]. However, CYP3A4 and FMO3 are mainly expressed in the liver (accounting for 54% of overall tetrahydrothiophene [THT] disappearance, the metabolite of BU), and less in LCLs, as observed in our laboratory (data not shown) and by others (https://www.proteinatlas.org). After RNA sequencing in LCLs, very low or no gene expressions of CYP 2D6, 2C19, 2C9, 2B6, 2C8, 4A11, 3A4, FMO1 and FMO3 were identified. In this context, the oxidative burst caused by electrophilic molecules from BU–GSH conjugation (Udensi and Tchounwou 2014; Zmorzynski et al. 2015) in addition to the absence of CYP3A4 and FMO3 could be a reason for the lower sensitivity of GSTM1-null HCs to BU, as observed in LCLs and THP1. In contrast, higher total expressions of CYPs and FMOs in hepatocytes (El-Serafi et al. 2017) could explain why GSTA1-slow BU metabolizing individuals in addition to the absence of GSTM1 activity show potentially more treatment-related toxicities [e.g., SOS (Srivastava et al. 2004) and aGvHD (Elhasid et al. 2010)] than carriers with normal GST’s enzyme activities. A hypothetical comparative model of the difference in BU fate between hepatocytes and lymphocytes is suggested in Supplementary Fig. 5 and warrants further investigation.
The genetically determined different cell fate after BU exposure might explain the apparently discordant results between the relapse incidence in patients carrying GSTM1-null genotype (in combination with GSTT1-null) and the cellular resistance to BU in GSTM1-null LCLs and THP1GSTM1(−/−). The higher rates of necrosis in GSTM1-non-null cells might predict a pro-inflammatory cell death of the malignant cells, resulting in enhanced immunogenicity (Sachet et al. 2017). Unlike the other chemotherapeutic regimens including autologous transplantation, the efficacy of the allogeneic transplantation relies on the graft-versus-leukemia effect, especially in HMs (Horowitz et al. 1990; Yeshurun et al. 2019), but that theory should be further explored.
Another relevant observation is the significantly increased post-HSCT relapse in GSTT1-null when combined with GSTM1-null genotype in children with HMs. The link between GSTT1 and post-HSCT relapse is not clear yet. Our in vitro observations cannot be attributed to the BU-related differences in IC50 values or [GSSG/GSHT] ratios. Other pharmacogenomics studies also demonstrated that genetic variations in GSTT1 are not associated with BU clearance or liver toxicity (Gaziev et al. 2010; Goekkurt et al. 2007; Kim et al. 2011; Srivastava et al. 2004). Nevertheless, we observed faster baseline proliferation in GSTT1-non-null LCLs/THP1 and a slightly higher baseline increase of caspase 3/7 activation compared to those with GSTT1-null genotype, indicating GSTT1 potential involvement of BU- independent mechanisms in the relapse development.
The results of the present clinical study are limited by the retrospective study design and relatively small pediatric sample size with no clinical validation cohort. However, the sample size of 86 patients has at least 80% power with 10% of observed combined GSTM1/GSTT1 double null variants’ frequency and relapse incidence with the estimated observed effect size of ≥ 7.0 and alpha value of 0.05. The primary diagnosis of HMs was made at the referring institution and was not centrally reviewed. Well-known risk factors such as somatic genetic/cytogenetics abnormalities, the donor DNA and the initial response to the treatment (e.g., MRD) were not available. However, as described in Supplementary Table 2, similar characteristics were present between the GST genetic subgroups (p values > 0.05). The GST-null variants were not associated with the status of the disease before HSCT and we assume that the germline genotype impact on protein expression was present in malignant cells as shown by Weiss et al. (2007). The majority of cases in our study underwent a BU–CY conditioning regimen; however, it is not known if this association is specific to a BU–CY conditioning regimen only or unspecific to other chemotherapeutics used in the HSCT setting (e.g., Thio or Mel) (Hao et al. 2020). For instance, active metabolites of CY (e.g., acrolein) are also eliminated by GSH conjugation catalyzed by GSTs (Uppugunduri et al. 2017). This needs to be evaluated in the future with a focus on whether GSTs play a major role in determining clinical outcomes. This aspect is currently being evaluated by our group using a cohort from multiple centers with the usage of multiple conditioning regimens. Furthermore, the transplant-related mortality or combined toxicities were not associated with the GSTM1- and GSTT1-null variants (data are not shown), suggesting compensation of BU conjugation by other GSTs, especially GSTA1, which is mainly expressed in hepatocytes and other somatic cells.
Conclusions
In summary, we report that GSTM1/GSTT1 double null genotypes could serve as genetic biomarkers for identifying pediatric patients with HMs at higher risk of relapse after an allogeneic HSCT following BU-containing conditioning. On the other hand, the absence of those markers might predict the patients who more likely will respond to the chemotherapy-based conditioning. Functional studies indicated different mechanisms of cell death upon exposure to BU based on the presence or absence of GST-null alleles and the in vivo impact of those findings must be further explored.
Data availability
All data presented are provided freely in this manuscript including any supplementary data. The raw datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Change history
30 October 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00432-021-03830-0
References
Ansari M et al (2017) GSTA1 diplotypes affect busulfan clearance and toxicity in children undergoing allogeneic hematopoietic stem cell transplantation: a multicenter study. Oncotarget 8:90852–90867
Balta G, Yuksek N, Ozyurek E, Ertem U, Hicsonmez G, Altay C, Gurgey A (2003) Characterization of MTHFR, GSTM1, GSTT1, GSTP1, and CYP1A1 genotypes in childhood acute leukemia. Am J Hematol 73:154–160
Barragan E, Collado M, Cervera J, Martin G, Bolufer P, Roman J, Sanz MA (2007) The GST deletions and NQO1*2 polymorphism confers interindividual variability of response to treatment in patients with acute myeloid leukemia. Leuk Res 31:947–953
Barrett AJ, Battiwalla M (2010) Relapse after allogeneic stem cell transplantation. Expert Rev Hematol 3:429–441
Bartelink IH et al (2016) Association of busulfan exposure with survival and toxicity after haemopoietic cell transplantation in children and young adults: a multicentre, retrospective cohort analysis. Lancet Haematol 3:e526–e536
Board PG, Menon D (2013) Glutathione transferases, regulators of cellular metabolism and physiology. Biochim Biophys Acta 1830:3267–3288
Borst L, Buchard A, Rosthoj S, Wesolowska A, Wehner PS, Wesenberg F, Dalhoff K, Schmiegelow K (2012) Gene dose effects of GSTM1, GSTT1 and GSTP1 polymorphisms on outcome in childhood acute lymphoblastic leukemia. J Pediatr Hematol Oncol 34:38–42
Bremer S, Floisand Y, Brinch L, Gedde-Dahl T, Bergan S (2015) Glutathione transferase gene variants influence busulfan pharmacokinetics and outcome after myeloablative conditioning. Ther Drug Monit 37:493–500
Chen CL, Liu Q, Pui CH, Rivera GK, Sandlund JT, Ribeiro R, Evans WE, Relling MV (1997) Higher frequency of glutathione S-transferase deletions in black children with acute lymphoblastic leukemia. Blood 89:1701–1707
Ciurea SO, Andersson BS (2009) Busulfan in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 15:523–536
Czerwinski M, Gibbs JP, Slattery JT (1996) Busulfan conjugation by glutathione S-transferases alpha, mu, and pi. Drug Metab Dispos 24:1015–1019
Czerwinski M, Kiem HP, Slattery JT (1997) Human CD34+ cells do not express glutathione S-transferases alpha. Gene Ther 4:268–270
DeLeve LD, Wang X (2000) Role of oxidative stress and glutathione in busulfan toxicity in cultured murine hepatocytes. Pharmacology 60:143–154
Elhasid R, Krivoy N, Rowe JM, Sprecher E, Adler L, Elkin H, Efrati E (2010) Influence of glutathione S-transferase A1, P1, M1, T1 polymorphisms on oral busulfan pharmacokinetics in children with congenital hemoglobinopathies undergoing hematopoietic stem cell transplantation. Pediatr Blood Cancer 55:1172–1179
El-Serafi I, Terelius Y, Abedi-Valugerdi M, Naughton S, Saghafian M, Moshfegh A, Mattsson J, Potacova Z, Hassan M (2017) Flavin-containing monooxygenase 3 (FMO3) role in busulphan metabolic pathway. PLoS ONE 12:e0187294
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Franca R et al (2012) Glutathione S-transferase homozygous deletions and relapse in childhood acute lymphoblastic leukemia: a novel study design in a large Italian AIEOP cohort. Pharmacogenomics 13:1905–1916
Gaziev J et al (2010) Novel pharmacokinetic behavior of intravenous busulfan in children with thalassemia undergoing hematopoietic stem cell transplantation: a prospective evaluation of pharmacokinetic and pharmacodynamic profile with therapeutic drug monitoring. Blood 115:4597–4604
Goekkurt E, Stoehlmacher J, Stueber C, Wolschke C, Eiermann T, Iacobelli S, Zander AR, Ehninger G, Kroger N (2007) Pharmacogenetic analysis of liver toxicity after busulfan/cyclophosphamide-based allogeneic hematopoietic stem cell transplantation. Anticancer Res 27:4377–4380
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16:1141–1154
Hall AG, Autzen P, Cattan AR, Malcolm AJ, Cole M, Kernahan J, Reid MM (1994) Expression of mu class glutathione S-transferase correlates with event-free survival in childhood acute lymphoblastic leukemia. Cancer Res 54:5251–5254
Hamilton BK, Copelan EA (2012) Concise review: the role of hematopoietic stem cell transplantation in the treatment of acute myeloid leukemia. Stem Cells 30:1581–1586
Hao C, Ma X, Wang L, Zhang W, Hu J, Huang J, Yang W (2020) Predicting the presence and mechanism of busulfan drug-drug interactions in hematopoietic stem cell transplantation using pharmacokinetic interaction network-based molecular structure similarity and network pharmacology. Eur J Clin Pharmacol 77(4):595–605
Hoban PR, Robson CN, Davies SM, Hall AG, Cattan AR, Hickson ID, Harris AL (1992) Reduced topoisomerase II and elevated alpha class glutathione S-transferase expression in a multidrug resistant CHO cell line highly cross-resistant to mitomycin C. Biochem Pharmacol 43:685–693
Horowitz MM et al (1990) Graft-versus-leukemia reactions after bone marrow transplantation. Blood 75:555–562
Kim SD et al (2011) Influence of GST gene polymorphisms on the clearance of intravenous busulfan in adult patients undergoing hematopoietic cell transplantation. Biol Blood Marrow Transplant 17:1222–1230
Lee CJ et al (2020) Late effects after ablative allogeneic stem cell transplantation for adolescent and young adult acute myeloid leukemia. Blood Adv 4:983–992
Leonardi DB, Abbate M, Riccheri MC, Nunez M, Alfonso G, Gueron G, De Siervi A, Vazquez E, Cotignola J (2017) Improving risk stratification of patients with childhood acute lymphoblastic leukemia: Glutathione-S-Transferases polymorphisms are associated with increased risk of relapse. Oncotarget 8:110–117
Li M, Zheng M, Chen H, Yu H (2018) Effects of GST variants on the risk odds of hematological malignancy: a meta-analysis. J Cell Biochem 120(5):8570–8580
Lin DX, Tang YM, Peng Q, Lu SX, Ambrosone CB, Kadlubar FF (1998) Susceptibility to esophageal cancer and genetic polymorphisms in glutathione S-transferases T1, P1, and M1 and cytochrome P450 2E1. Cancer Epidemiol Biomarkers Prev 7:1013–1018
Marin F, Garcia N, Munoz X, Capella G, Gonzalez CA, Agudo A, Sala N (2010) Simultaneous genotyping of GSTT1 and GSTM1 null polymorphisms by melting curve analysis in presence of SYBR Green I. J Mol Diagn 12:300–304
McCune JS, Holmberg LA (2009) Busulfan in hematopoietic stem cell transplant setting. Expert Opin Drug Metab Toxicol 5:957–969
McCune JS, Gooley T, Gibbs JP, Sanders JE, Petersdorf EW, Appelbaum FR, Anasetti C, Risler L, Sultan D, Slattery JT (2002) Busulfan concentration and graft rejection in pediatric patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 30:167–173
Myers AL, Kawedia JD, Champlin RE, Kramer MA, Nieto Y, Ghose R, Andersson BS (2017) Clarifying busulfan metabolism and drug interactions to support new therapeutic drug monitoring strategies: a comprehensive review. Expert Opin Drug Metab Toxicol 13:901–923
Peters C et al (2021) Total body irradiation or chemotherapy conditioning in childhood all: a multinational, randomized, noninferiority phase III study. J Clin Oncol 39:295–307
Philippe M, Goutelle S, Guitton J, Fonrose X, Bergeron C, Girard P, Bertrand Y, Bleyzac N (2016) Should busulfan therapeutic range be narrowed in pediatrics? Experience from a large cohort of hematopoietic stem cell transplant children. Bone Marrow Transplant 51:72–78
Rocha JC et al (2005) Pharmacogenetics of outcome in children with acute lymphoblastic leukemia. Blood 105:4752–4758
Sachet M, Liang YY, Oehler R (2017) The immune response to secondary necrotic cells. Apoptosis 22:1189–1204
Saitou M, Ishida T (2015) Distributions of the GSTM1 and GSTT1 null genotypes worldwide are characterized by latitudinal clines. Asian Pac J Cancer Prev 16:355–361
Shah NN, Borowitz MJ, Steinberg SM, Robey NC, Gamper CJ, Symons HJ, Loeb DM, Wayne AS, Chen AR (2014) Factors predictive of relapse of acute leukemia in children after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant 20:1033–1039
Smith MT, Evans CG, Doane-Setzer P, Castro VM, Tahir MK, Mannervik B (1989) Denitrosation of 1,3-bis(2-chloroethyl)-1-nitrosourea by class mu glutathione transferases and its role in cellular resistance in rat brain tumor cells. Cancer Res 49:2621–2625
Srivastava A, Poonkuzhali B, Shaji RV, George B, Mathews V, Chandy M, Krishnamoorthy R (2004) Glutathione S-transferase M1 polymorphism: a risk factor for hepatic venoocclusive disease in bone marrow transplantation. Blood 104:1574–1577
Stanulla M, Schrappe M, Brechlin AM, Zimmermann M, Welte K (2000) Polymorphisms within glutathione S-transferase genes (GSTM1, GSTT1, GSTP1) and risk of relapse in childhood B-cell precursor acute lymphoblastic leukemia: a case-control study. Blood 95:1222–1228
Takanashi M, Morimoto A, Yagi T, Kuriyama K, Kano G, Imamura T, Hibi S, Todo S, Imashuku S (2003) Impact of glutathione S-transferase gene deletion on early relapse in childhood B-precursor acute lymphoblastic leukemia. Haematologica 88:1238–1244
Teachey DT, Hunger SP (2013) Predicting relapse risk in childhood acute lymphoblastic leukaemia. Br J Haematol 162:606–620
Terakura S et al (2020) Analysis of glutathione S-transferase and cytochrome P450 gene polymorphism in recipients of dose-adjusted busulfan-cyclophosphamide conditioning. Int J Hematol 111:84–92
Tew KD, Townsend DM (2012) Glutathione-s-transferases as determinants of cell survival and death. Antioxid Redox Signal 17:1728–1737
Udensi UK, Tchounwou PB (2014) Dual effect of oxidative stress on leukemia cancer induction and treatment. J Exp Clin Cancer Res 33:106
Uppugunduri CRS et al (2017) The association of combined GSTM1 and CYP2C9 genotype status with the occurrence of hemorrhagic cystitis in pediatric patients receiving myeloablative conditioning regimen prior to allogeneic hematopoietic stem cell transplantation. Front Pharmacol 8:451
Weiss JR, Baer MR, Ambrosone CB, Blanco JG, Hutson A, Ford LA, Moysich KB (2007) Concordance of pharmacogenetic polymorphisms in tumor and germ line DNA in adult patients with acute myeloid leukemia. Cancer Epidemiol Biomarkers Prev 16:1038–1041
Woo MH et al (2000) Glutathione S-transferase genotypes in children who develop treatment-related acute myeloid malignancies. Leukemia 14:232–237
Xiao Z, Yang L, Xu Z, Zhang Y, Liu L, Nie L, Li L, Wang J, Hao Y (2008) Glutathione S-transferases (GSTT1 and GSTM1) genes polymorphisms and the treatment response and prognosis in Chinese patients with de novo acute myeloid leukemia. Leuk Res 32:1288–1291
Xiao Q, Deng D, Li H, Ye F, Huang L, Zhang B, Ye B, Mo Z, Yang X, Liu Z (2014) GSTT1 and GSTM1 polymorphisms predict treatment outcome for acute myeloid leukemia: a systematic review and meta-analysis. Ann Hematol 93:1381–1390
Yeshurun M et al (2019) The impact of the graft-versus-leukemia effect on survival in acute lymphoblastic leukemia. Blood Adv 3:670–680
Zareifar S, Monabati A, Saeed A, Fakhraee F, Cohan N (2013) The association of glutathione S-transferase gene mutations (including GSTT1 and GSTM1) with the prognostic factors and relapse in acute lymphoblastic leukemia. Pediatr Hematol Oncol 30:568–573
Zhang HY, Zhang J, Wu T, Bai H (2017) Polymorphism of glutathione S-transferases and genetic sensitivity of childhood acute lymphoblastic leukemia: a meta-analysis. Zhongguo Shi Yan Xue Ye Xue Za Zhi 25:16–23
Zmorzynski S, Swiderska-Kolacz G, Koczkodaj D, Filip AA (2015) Significance of polymorphisms and expression of enzyme-encoding genes related to glutathione in hematopoietic cancers and solid tumors. Biomed Res Int 2015:853573
Acknowledgements
We warmly thank the patients and their parents for consenting to participate in this study. We also thank Laurence Lesne, Mary Khoshbeen, Denis Marino, Rodolfo Lo Piccolo, Benedict Dupraz, Anuj Kumar Tyagi and Eva Choong for the help in this study as well as the Swiss Pediatric Oncology Group.
Funding
Open Access funding provided by Université de Genève. This study was performed thanks to the contribution of the Swiss National Science Foundation (ME9870/320030-153389, PI: Marc Ansari), the OAK foundation (OCAY-17-642, PI: Marc Ansari) and the CANSEARCH foundation (PI: Marc Ansari).
Author information
Authors and Affiliations
Consortia
Contributions
SJM, CRSU, MA designed the study; SJM, VM, CRSU executed cell viability experiments; SJM, CRSU isolated DNA/mRNA and genotyping from cell lines; SJM, VM contributed to apoptosis and necrosis-based experiments and produced CRISPR–Cas9 THP1 knockout cell models; SJM executed real-time viability and apoptosis/necrosis, caspase 3/7 and GSH -based experiments and western blotting; SJM, CRSU, SR: GST activity; MA, MAR, YC, JJB, RGMB, JHD, CP, SC, HB, MK contributed to patients’ sample and clinical data processing; SJM executed computational and statistical analysis of clinical data that were verified by MA, TN, CRSU, HB; SJM, MA, VM, TN, CRSU contributed to interpretation of results; SJM drafted the manuscript; all authors revised the study critically. MA had final responsibility for the decision to submit for publication. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests related to the submitted work.
Ethics approval
The Institutional Review Board or ethics committees approved the study.
consent to participate
All patients and/or parents provided informed consent.
Consent for publication
All authors are aware of the study and approve of this submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to correction in the author names and affiliation.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jurkovic Mlakar, S., Uppugunduri, S.C.R., Nava, T. et al. GSTM1 and GSTT1 double null genotypes determining cell fate and proliferation as potential risk factors of relapse in children with hematological malignancies after hematopoietic stem cell transplantation. J Cancer Res Clin Oncol 148, 71–86 (2022). https://doi.org/10.1007/s00432-021-03769-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03769-2