Abstract
Background
Acute myeloid leukemia (AML) with antecedent hematological disease (s-AML) and treatment-related AML (t-AML) predicts poor prognosis. Intensive treatment protocols of those high-risk patients should consider allogeneic stem cell transplantation (allo-HSCT) in first complete remission (CR). Despite allo-HSCT, relapse rate remains high. Induction chemotherapy with liposomal cytarabine and daunorubicin (CPX-351) has been approved for patients with AML with myeloid-related changes (AML-MRC) or t-AML based on improved survival and remission rates compared to standard 7 + 3 induction.
Patients and methods
110 patients with newly diagnosed s-AML or t-AML at a university hospital were analyzed retrospectively. Median age was 62 years (24–77 years). A total of 65 patients with s-AML after MDS (59%) and 23 patients (20.9%) with t-AML were included. Induction chemotherapy consisted of intermediate-dosed cytarabine (ID-AraC) in combination with idarubicin (patients up to 60 years) or mitoxantrone (patients over 60 years). In patients subsequently undergoing allo-HSCT, reduced conditioning regimens (RIC) were applied prior to transplantation in 47 of 62 patients (76%).
Results
Induction chemotherapy with ID-AraC resulted in an overall response rate of 83% including complete remission (CR/CRi) in 69 patients (63%) with a low rate of early death (2.7%). Most relevant non-hematologic toxicity consisted of infectious complications including sepsis with need of intensive care treatment in five patients (4.5%) and proven or probable invasive fungal disease in eight patients (7.2%). Relapse-free survival (RFS), event-free survival (EFS) and overall survival (OS) of the whole cohort were 19 months (0–167), 10 months (0–234) and 15 months (0–234), respectively (p < 0.0001). A significant improvement of OS was observed in patients who underwent allo-HSCT compared to those without subsequent allo-HSCT: 9 vs. 46 months, p < 0.0001. Rate of transplantation-related mortality (TRM) in the early phase post allo-HSCT was low (0.9% at day 30 and 1.8% at day 90, respectively). RIC conditioning results in OS rate of 60% after 60 months post allo-HSCT (median OS not reached).
Conclusion
S-AML and t-AML patients receiving induction chemotherapy with intermediate-dosed cytarabine showed satisfactory response rate and consolidation therapy with allo-HSCT after full or reduced-intensity conditioning further improved survival in these patients with similar outcome as reported for CPX-351.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incidence of secondary AML (s-AML) following myelodysplastic syndrome (MDS) is increasing with age and risk of transformation depends on stage of MDS as defined by percentage of blasts and genetic aberrations. Furthermore, AML with myeloid-related changes (AML-MRC) can be diagnosed in the absence of MDS history according to the WHO 2016 classification (Arber et al. 2016).
AML with an antecedent hematological disease (s-AML) is associated with unfavorable cytogenetic aberrations (e.g., complex karyotype) (Ostgård et al. 2010). A monosomal karyotype has a negative prognostic impact not only in patients with complex cytogenetic aberrations but also in AML with MDS-related karyotype anomalies (Kayser et al. 2012). Large population-based AML registries confirm a lower rate of complete remission following induction chemotherapy and worse outcome in patients with s-AML (Hulegårdh et al. 2015). During the transformation of MDS to s-AML the majority of patients gain additional cytogenetic or molecular genetic aberrations (e.g., FLT3 mutations) and distinct mutation patterns can be detected during progression of MDS to s-AML (Flach et al. 2011; Fernandez-Mercado et al. 2012).
The presence of TP53 mutations in AML patients with complex cytogenetic aberrations can regularly be observed in combination with a monosomal karyotype and is associated with age, a reduced response rate and worse outcome (Rücker et al. 2012). In patients with complex karyotype and either TP53 or RAS mutations even allogeneic stem cell transplantation (allo-HSCT) is not able to improve survival of these patients. A similar observation has been made in patients with MDS or s-AML harboring more than two unfavorable molecular genetic aberrations (Yoshizato et al. 2017).
AML following previous chemotherapy or radiation treatment (t-AML) can be regularly observed in patients with history of lymphoma (e.g., Hodgkin’s disease) or breast cancer (Bertoli et al. 2016; Linassier et al. 2000). Cytogenetic analyses of t-AML reveal aberrations–e.g., t(8;21) or inv(16)—that are associated with a good prognosis in de novo AML according to the ELN classification (Gustafson et al. 2009; Döhner et al. 2017). Importantly, such cytogenetic findings cannot be attributed to an improved outcome in t-AML patients (Gustafson et al. 2009; Schoch et al. 2004). Furthermore, NPM1 mutations and FLT3 internal tandem duplication (FLT3-ITD) are less frequently detected in patients with t-AML while regularly identified TP53 mutations are associated with a lower response rate to conventional chemotherapy (Kayser et al. 2011). Surprisingly, progenitor cells harboring age-related TP53 mutations seem to be enriched during chemotherapy leading to the worse prognosis of TP53 mutated t-AML patients (Wong et al. 2015).
Induction chemotherapy of elderly AML patients is regularly associated with a lower response rate due to a higher proportion of patients with high-risk characteristics (e.g., antecedent MDS, cytogenetic risk factors) (Bello et al. 2011). A higher rate of early death following induction chemotherapy because of treatment-related complications (e.g., severe infections) has been observed (Krug et al. 2010). Improvement of induction chemotherapy approaches to achieve a better response rate without increased toxicity is an unmet medical need in elderly high-risk AML patients. Intensification of chemotherapy (e.g., induction treatment according to the FLAG protocol) has been demonstrated to improve complete remission rate without increasing mortality in patients with secondary AML (Vulaj et al. 2018). In contrast, the addition of the CD33-directed monoclonal antibody–drug conjugate gemtuzumab-ozogamicin had no clinically relevant impact on the outcome of AML patients with high-risk cytogenetics (Castaigne et al. 2012).
Several clinical trials addressed the question to improve chemotherapy regimens for AML patients. The OSHO study group (East German Study Group of Hematology and Oncology) has implemented intermediate-dosed cytarabine in different age-dependent induction protocols. For younger patients (up to the age of 60 years), response rate and survival of AML patients has been demonstrated to be similar compared to conventional induction regimens (e.g., 7 + 3). Furthermore, there is a substantial benefit in elderly AML patients (60–75 years) after OSHO induction therapy followed by allo-HSCT (Büchner et al. 2012; Niederwieser et al. 2014).
Long-term outcome of high-risk AML is highly dependent on the eligibility to allo-HSCT while the introduction of reduced-intensity conditioning (RIC) regimens allows allo-HSCT in patients up to the age of about 75 years. Large registry analyses could not demonstrate any difference in overall survival of AML and MDS patients comparing myeloablative conditioning (MAC) and RIC regimens (Luger et al. 2012). In the context of the increasing risk of treatment-related mortality (TRM) in patients between the age of 60 and 75 years, the role of RIC regimens has been established and can reduce TRM in elderly AML patients (Ustun et al. 2019; Tauro et al. 2005).
The liposomal formulation of cytarabine and daunorubicin (CPX-351, Vyxeos®) has been approved for induction and consolidation chemotherapy for patients with AML-MRC or t-AML by the US Food and Drug Administration (FDA) and the European Medicine Agency (EMA). CPX-351 has been evaluated in a phase 3 clinical trial in patients with AML-MRC or t-AML undergoing induction chemotherapy with either 7 + 3 regimen (cytarabine plus daunorubicin) or CPX-351 (Lancet et al. 2018).
There was a higher response rate in the CPX-351 cohort as compared to standard 7 + 3 induction chemotherapy resulting in a significant longer overall survival (9.6 vs 6.0 months). Patients subsequently undergoing allo-HSCT demonstrated the clinically most relevant benefit with a survival rate of about 60% two years after allo-HSCT. Recently, these data have been confirmed in a large cohort of 109 high-risk AML patients in France (Chiche et al. 2021).
Here, we report on a retrospective analysis of 110 consecutively treated AML patients with s-AML or t-AML. All these patients were treated with induction chemotherapy containing intermediate-dosed cytarabine (ID-AraC) in combination with either idarubicin or mitoxantrone while most patients underwent subsequent allo-HSCT in first complete remission.
Patients and methods
Patient cohort
A total of 110 consecutively treated patients with either s-AML or t-AML were identified. All these AML patients underwent induction chemotherapy at the Department of Hematology and Oncology, University Hospital Jena, Germany. Diagnosis and start of induction chemotherapy were between 2001 and 2020. The cohort consisted of 23 patients (20.9%) with t-AML including 8 patients with a history of lymphoma treatment and 11 women who developed t-AML following chemotherapy due to breast cancer. Patients´ characteristics are indicated in Table 1. Figure 1S (Supplement) provides clinical details and time course of individual history prior to diagnosis of t-AML.
Informed consent
All patients were included in one of the following AML registries: AML registry of the OSHO study group (East German Study Group of Hematology and Oncology) or in the SAL registry (Study Alliance Leukemia). Patients gave their written informed consent for data acquisition and analysis after pseudonymization in one of the AML registries. The participation in both AML registries has been approved by the Ethical review committee of the University Hospital Jena (Ethical number 4871–07/16 for “retrospective evaluation of therapy response and survival in patients with AML” and 3967–12/13 for SAL registry).
Patient treatment
Induction and consolidation chemotherapy was applied according to the OSHO 2002 (NCT01414231) or the OSHO 2004 (NCT01497002) protocol. In detail, patients up to the age of 60 years were treated with idarubicin (12 mg/m2, day 1–3) and intermediate-dosed cytarabine (1 g/m2 bid, day 1, 3, 5 and 7) as induction chemotherapy while patients over 60 years received mitoxantrone (10 mg/m2, day 1–3) and intermediate-dosed cytarabine (1 g/m2 bid, day 1, 3, 5 and 7) as induction treatment. First consolidation chemotherapy in younger AML patients was identical with induction chemotherapy. Elderly AML patients underwent consolidation treatment with a dose reduction of mitoxantrone (10 mg/m2, day 1 and 2) and intermediate-dosed cytarabine (0.5 g/m2 bid, day 1, 3 and 5) (Büchner et al. 2012; Kahl et al. 2016).
The majority of patients (47/62, 75.8%) subsequently undergoing allo-HSCT received a reduced-intensity conditioning (RIC) based on treosulfan (36/47, 76.6%) or busulfan (8/47, 17.0%) in combination with fludarabine prior to allo-HSCT (Casper et al. 2012; Kröger et al. 2003). In addition, three patients (6.4%) of the RIC subgroup received the FLAMSA protocol before allo-HSCT (Schmid et al. 2008). The remaining patients underwent either myeloablative conditioning (MAC; 10/62, 16.1%) with 12 Gy total body irradiation (TBI) in combination with cyclophosphamide or a non-myeloablative conditioning (NMAC; 5/62, 8.1%) with 2 Gy TBI and fludarabine (Jethava et al. 2017; Niederwieser et al. 2003).
Graft-versus-host-disease (GvHD) prophylaxis consisted of cyclosporine A (CSA) in combination with short-term methotrexate (MTX) or mycophenolate mofetil (MMF), and anti-thymocyte globulin (ATG). Patient characteristics of those patients who subsequently underwent allo-HSCT are summarized in Table 4. Calculation of comorbidity score prior to allo-HSCT was performed according to Sorror (Sorror et al. 2005).
Analysis of toxicity and classification of fungal infections
Toxicity during and after induction chemotherapy was evaluated according to the Common Terminology Criteria and Adverse Events classification (CTCAE v4.0). Fungal infections have been defined according to the EORTC/MSG nomenclature classifying possible, probable and proven invasive fungal disease (IFD) (Pauw et al. 2008).
Cytogenetic and molecular genetic analyses
Karyotype analyses by means of chromosome banding were performed with standard techniques, and karyotypes were described according to the International System for Human Cytogenetic Nomenclature (Brothman et al. 2005). Cytogenetic categorization into favorable, intermediate or adverse risk was performed on the basis of recommended criteria (Döhner et al. 2017).
In all patients with chromosomal aberrations, detection of residual AML cells was established using fluorescence in situ hybridization (FISH) and applied after induction chemotherapy and prior to allo-HSCT. A summary of cytogenetic remission status at particular time points is shown in the supplement (Table S2).
The presence of FLT3-ITD and NPM1 mutations was detected by PCR amplification of the corresponding region using genomic DNA followed by fragment analysis (Scholl et al. 2008,2005).
Statistics
Determination of complete remission (CR) without or with incomplete recovery (CRi), partial remission (PR) and refractory disease (persistence of blasts) was performed according to the current guidelines of the European Leukemia Network (ELN 2017). Overall survival (OS), Event-free survival (EFS) and relapse-free survival (RFS) were also defined using the ELN 2017 recommendations (Döhner et al. 2017). For patients undergoing allo-HSCT, OS and RFS were additionally calculated from the date of allo-HSCT to the date of death.
Statistical analyses were performed using GraphPad Prism 8.0.2 (GraphPad Inc.). Differences between the Kaplan–Meier survival curves were evaluated by Log-rank (Mantel-Cox) test. p values of < 0.05 were considered as statistically significant.
Results
Patient’s characteristics
This analysis comprises 110 patients with a median age of 62 years (range 24–77) who received intensive AML-treatment. The majority of patients (n = 65, 59%) developed AML following antecedent MDS, 15 patients (13.6%) after chronic myelomonocytic leukemia (CMML) and 7 patients (6.3%) following myeloproliferative syndrome (MPN). Detailed clinical characteristics and time course of 23 patients (20.9%) with t-AML are illustrated in Table S1 and Figure S1, respectively. 28 patients (25.4%) received treatment with hypomethylating agents prior to induction chemotherapy.
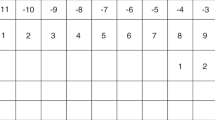
In 67 (43%) and 45 cases (40.9%) with available data, FLT3-ITD or NPM1 mutations could be detected in 10 (14.9%) and 4 patients (8.8%), respectively. According to ELN risk classification 2010, risk score was favorable, intermediate (I or II) and adverse in 4 patients (9.5%), 28 patients (66.6%) and 10 patients (23.8%), respectively. In 68 cases (61.8%) no stratification was possible due to lack of mutational testing. Therefore, additional risk stratification based on cytogenetic data only is demonstrated in Table 1. An overview of our study population including subsequent allo-HSCT in the majority of patients is given in the CONSORT diagram (Fig. 1).
CONSORT diagram response to induction therapy and follow- up after CR. *Including two pts who died until day 30 and one patient who died on day 44 after start of induction chemotherapy. **Both patients received salvage chemotherapy according to Mito-FLAG protocol, one of these pts subsequently underwent allo-HSCT. *** 1 pt died during consolidation after CR; 4 pts died during consolidation after PR/BP
Response to induction chemotherapy
The analysis of overall remission after induction chemotherapy revealed a CR/CRi rate of 62.7% (69 of 110 patients). In 21% (23/110) a PR was observed, 11.8% (13/110) were refractory to induction therapy. In two of these refractory patients, CR could be achieved after salvage therapy by Mito-FLAG protocol. One of both patients further proceeded to allo-HSCT (Fig. 1). The median OS of the whole cohort was 15 months (0–234) and the median EFS was 11 months (0–234) while the median RFS for patients who achieved CR/CRi was 19 months (0–167; all p < 0.0001, Fig. 2). The median follow-up time of all 110 patients was 13 months (1–234). Additionally, cytogenetic remission (FISH) following induction treatment as well as prior to allo-HSCT is shown in Table S2 in the supplement.
Kaplan–Meier estimates for EFS (A), OS (B, D) and RFS (C). A comparison between EFS of whole cohort vs. allo-HSCT vs. no allo-HSCT. B comparison of OS of whole cohort vs. allo-HSCT vs. no allo-HSCT. C RFS for patients achieving CR or CRi is shown for all patients vs. allo-HSCT vs. no allo-HSCT. D OS for patients achieving CR or CRi is demonstrated for all patients vs. allo-HSCT vs. no allo-HSCT
Safety and hematological recovery
During induction, early deaths occurred in 3 (2.7%) patients including 2 patients dying within the first 30 days after start of induction chemotherapy and one patient who died on day 44 in aplasia during the course of induction (Table 2). The 90-day mortality after induction chemotherapy was 7.2% (8/110).
In general, analysis of non-hematologic toxicity showed moderate side effects during induction chemotherapy. In Table 3, non-hematologic toxicity according to CTC classification is listed. Among grade III and IV toxicities, five patients (4.5%) occurred with severe pneumogenic sepsis with need of intensive care treatment. One patient presented with seizures, another patient suffered from heart attack. Classification of invasive fungal disease (IFD) indicated invasive fungal disease in 38 patients (35%). Probable or proven IFD could be documented in only 4.5 and 3%, respectively.
The assessment of hematological reconstitution after induction chemotherapy showed a median time of platelet recovery of at least 50 × 109/l after 29 days (17–122 days) and a median time of white blood count (WBC) recovery > 2.0 × 109/l of 30 days or absolute neutrophil counts > 0.5 × 109/l (21–141 days). 11.9% (13/110) and 10% (11/110) did neither achieve stable reconstitution of platelets or neutrophils (Table 2). Notably, 23 patients (20.9%) received granulocyte colony-stimulating factor (G-CSF) support to accelerate neutrophil recovery in cases of delayed hematologic reconstitution.
Outcome and safety after allogeneic SCT
In total, 62 patients (56.3%) proceeded to allo-HSCT including 66.1% (41/62) in first CR. 15 (24.1%) patients fulfilled criteria for PR and 6 (9.6%) patients had a relapsed or refractory AML at the time of transplantation. The median age at transplantation was 58 years (24–73 years).
Kaplan–Meier analysis showed a median OS of patients who received allo-HSCT of 46 months (0–234 months) vs. 9 months (0–98 months) without allo-HSCT, p < 0.0001. After a median follow-up time of 25.5 months (4–234 months) since diagnosis of AML and 22 months (3–230 months) since date of transplantation, RFS could demonstrate a statistically significant benefit of 57 months (1–167 months) for patients with allo-HSCT compared to 5 months (0–61 months) for those patients who did not underwent allo-HSCT, p < 0.0001 (Table 4). Median EFS was 46 vs. 5 months for patients with or without allo-HSCT, respectively.
The majority of 58% (36/62) received a matched, unrelated graft (MUD). Compared with the group of patients who obtained matched related or mismatched unrelated grafts there was a trend towards a higher RFS for patients receiving a MUD graft (data not shown, p = 0.1209).
Two patients (3.2%) died within the first 90 days following allo-HSCT, both on septic complications. Assessment of non-relapse mortality after allo-HSCT identified 18 patients. These died after a median of 235 days (22–2766 days) post allo-HSCT with major cause of sepsis and severe infections.
Impact of conditioning regimen on survival after allo-HSCT
The vast majority of patients with allo-HSCT (75.8%, 47/62) received RIC protocols prior to allo-HSCT. The comparison of OS between patients who received either RIC or MAC prior to allo-HSCT demonstrated a statistically non-significant advantage in survival for patients following RIC conditioning. The median OS for patients in CR/CRi who received MAC conditioning was 29.5 months, for RIC group OS was about 60% after 60 months post allo-HSCT (median OS not reached, Fig. 3B). In accordance with that, RFS for all patients with CR/CRi prior to transplantation was 52 months, for the MAC conditioned patients 23.5 months while median RFS for the RIC group has not been reached (p = 0.1489, Fig. 3A). comparison of 5-year OS of patients who did not undergo allo-HSCT following CR/CRi after induction chemotherapy with those receiving allo-HSCT with RIC elucidated a clinically relevant difference of 9.5 vs. 60%, respectively.
Risk assessment prior to allo-HSCT according to “Sorror” comorbidity score displayed an extend of comorbidities in the RIC conditioned cohort, while MAC conditioned patients showed much lower comorbidity levels (Table 4).
Discussion
Treatment of AML remains a challenge in both younger and elderly AML patients and there is an increased risk of negative prognostic factors correlating with patients´ age at diagnosis. Antecedent myelodysplastic syndrome (MDS) or de novo AML with myeloid-related changes (AML-MRC) is especially seen in elderly patients which makes an evaluation of the eligibility of allogeneic stem cell transplantation (allo-HSCT) essential.
Recently, clinically relevant improvement of AML therapy could only be achieved either for distinct molecular or cytogenetic subgroups (e.g., midostaurin in FLT3 mutated AML or gemtuzumab ozogamicin for AML with favorable prognosis) or for patients with relapsed/ refractory AML harboring activating FLT3 mutations (e.g., gilteritinib) to replace intensive salvage chemotherapy (Castaigne et al. 2012; Stone et al. 2017; Perl et al. 2019).
Induction chemotherapy of high-risk AML patients with a conventional 7 + 3 regimen has been the standard of care in many AML study groups. The approval of liposomal chemotherapy combining cytarabine and daunorubicin (CPX-351) is currently changing this standard induction chemotherapy for a wide range of high-risk AML patients. Here, a comprehensive monocentric analysis of induction chemotherapy with intermediate-dosed cytarabine according to two well-established and age-adjusted protocols that have been intensively evaluated within the OSHO group is presented.
The distribution of distinct prognostic subgroups according to cytogenetic findings reveals an expected percentage of patients with unfavorable cytogenetics while there are only few patients that can be attributed to the favorable risk subgroup. This observation is in line with several other reports investigating patients with s-AML or t-AML and does also include a relatively low percentage of NPM1 or FLT3 mutations as opposed to younger AML patients with de novo AML. A relevant limitation of our retrospective study is the incomplete data set for molecular genetics (e.g., ASXL1, RUNX1 or TP53) to apply ELN 2017 classification. Thus, we could only stratify our cohort of AML patients according to cytogenetic risk groups with a potential higher percentage of patients attributed to the intermediate risk group. Nevertheless, the whole patient cohort analyzed here comprises high-risk AML patients with either s-AML or t-AML.
Following induction therapy with intermediate-dosed cytarabin an excellent rate of complete remission is demonstrated in this cohort of high-risk AML patients indicating a potential benefit for intermediate-dosed cytarabine compared to its application by continuous infusion. In consideration of previously published clinicals trials evaluating high-dosed cytarabine for induction chemotherapy, we hypothesize that the distinct pharmacokinetic of intermediate-dosed cytarabine as compared to the 7 + 3 regimen might be more effective to overcome primary resistance (Reese and Schiller 2013).
Furthermore, intermediate-dosed cytarabin chemotherapy is associated with a low rate of early death. In detail, only five patients developed sepsis with the need of intensive care treatment and the rather low rate of proven or probable invasive fungal infections might be a result of effective antifungal prophylaxis with posaconazole in the majority of patients.
In this cohort of high-risk AML patients with comparable characteristics concerning the percentage of secondary AML and t-AML patients’ reconstitution of neutrophils and platelets following both OSHO regimens applying intermediate-dosed cytarabine was in time. Importantly, 23 (20.9%) patient received granulocyte colony-stimulating factor (G-CSF) to accelerate neutrophil recovery.
Hematologic reconstitution after induction chemotherapy with CPX-351 is significantly delayed compared with the conventional 7 + 3 induction regimen. The differences in time to recovery of neutrophils and platelets are explained by distinct pharmacokinetic properties of CPX-351 with prolonged exposure to co-encapsulated cytarabine and daunorubicin in this liposomal formulation (Lancet et al. 2018).
The median age of patients in our cohort of high-risk AML patients was about five years below the median age of patients treated with CPX-351 published within the phase 3 trial or in the French AML survey (Lancet et al. 2018; Chiche et al. 2021). This might be one explanation for the lower rate of consolidation treatment with allo-HSCT in both studies (29 vs 35%, respectively). In our study a rather high rate of patients underwent allo-HSCT as recommended for this subset of AML patients being characterized by a high risk of AML relapse especially without allo-HSCT consolidation.
The present data demonstrate the impact of allo-HSCT on survival of high-risk AML patients in first complete remission. This reflects the high relevance of such immunotherapeutic approaches as allo-HSCT for patients with s-AML or t-AML. In general, we could show a low rate of early mortality after allo-HSCT in our patient cohort. While only two patients died of transplantation-related complications until day 90 after allo-HSCT, TRM had to be documented in another 16 patients within a long time period following allo-HSCT. This observation reflects the generally high vulnerability of immunocompromised patients in the context of allo-HSCT that can be associated with TRM even several years after allo-HSCT (Shimoni et al. 2016).
In consideration of age and comorbidities, there was a high rate of patients who received a reduced-intensity conditioning (RIC) regimen prior to allo-HSCT. The development of RIC protocols has substantially improved the eligibility of elderly AML patients for allo-HSCT as a basis to increase the survival of high-risk AML patients. Despite a comparable survival rate for patients undergoing MAC or RIC protocols about two years after allo-HSCT, there is a clinically relevant higher and stable long-term overall survival in the subgroup of patients who underwent RIC prior to allo-HSCT. This emphasizes the clinical benefit of RIC regimens for high-risk AML patients with the potential to cure AML (Casper et al. 2012).
Despite a higher percentage of patients with secondary AML or t-AML can be attributed to the ELN subgroup with an adverse prognosis, outcome of these patients after allo-HSCT is comparable with de novo AML patients of this ELN subgroup (Jentzsch et al. 2020). Furthermore, RIC regimens prior to allo-HSCT can significantly reduce TRM improving the outcome of patients with high-risk AML (Tauro et al. 2005). For patients with normal karyotype t-AML, Samra and colleagues could demonstrate a significantly higher rate of death in remission but no higher relapse rate following induction chemotherapy and allo-HSCT (Samra et al. 2020). This supports our hypothesis that RIC prior to allo-HSCT has a high impact on long-term survival in patients with secondary AML or t-AML.
TP53 mutations are considered to play a key role in mediating resistance to conventional chemotherapy. Furthermore, Walter et al. could show that further mutations (e.g., PTPN11) might contribute to primary resistance of secondary AML. Previously published real-life experience of CPX-351 in a cohort of 103 French high-risk AML patients could confirm the inferior outcome of those patients harboring TP53 or PTPN11 mutations (Chiche et al. 2021; Walter et al. 2012).
Molecular characterization of high-risk AML helps the clinicians to identify patients with potentially refractory AML following conventional induction chemotherapy. This is not only clinically relevant in patients with a reduced performance status resulting in a higher risk of severe morbidity or even early death after induction chemotherapy. Recently established improvement of epigenetic therapy by combination with the BCL-2 inhibitor venetoclax or targeted therapy in IDH1 or IDH2 mutated AML offers reasonable therapeutic option with a significantly lower risk of severe complications as compared to intensive chemotherapy regimens (DiNardo et al. 2020; Roboz et al. 2020; Pollyea et al. 2019).
Induction therapy with intermediated-dose of cytarabine results in comparable rate of complete remission rates with CPX-351. A major finding of this study was the demonstration of a significantly longer overall survival of patients undergoing allo-HSCT as consolidation treatment. Despite the latter aspect is independent of the induction regimen, our data on overall survival following OSHO induction chemotherapy and allo-HSCT reflects a promising approach for this challenging cohort of high-risk AML patients.
Taken together, induction chemotherapy with intermediate-dosed cytarabine according to the OSHO protocols followed by allo-HSCT provides a reasonable strategy for treatment of high-risk AML patients.
References
Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127:2391–2405. https://doi.org/10.1182/blood-2016-03-643544
Bello C, Yu D, Komrokji RS, Zhu W, Wetzstein GA, List AF, Lancet JE (2011) Outcomes after induction chemotherapy in patients with acute myeloid leukemia arising from myelodysplastic syndrome. Cancer 117:1463–1469. https://doi.org/10.1002/cncr.25598
Bertoli S, Sterin A, Tavitian S, Oberic L, Ysebaert L, Bouabdallah R, Vergez F, Sarry A, Bérard E, Huguet F et al (2016) Therapy-related acute myeloid leukemia following treatment of lymphoid malignancies. Oncotarget 7:85937–85947. https://doi.org/10.18632/oncotarget.13262
Brothman AR, Persons DL, Shaffer LG (2009) Nomenclature evolution: Changes in the ISCN from the 2005 to the 2009 edition. Cytogenet Genome Res. 127: 1–4. https://doi.org/10.1159/000279442
Büchner T, Schlenk RF, Schaich M, Döhner K, Krahl R, Krauter J, Heil G, Krug U, Sauerland MC, Heinecke A et al (2012) Acute Myeloid Leukemia (AML): different treatment strategies versus a common standard arm–combined prospective analysis by the German AML Intergroup. J Clin Oncol 30:3604–3610. https://doi.org/10.1200/jco.2012.42.2907
Casper J, Holowiecki J, Trenschel R, Wandt H, Schaefer-Eckart K, Ruutu T, Volin L, Einsele H, Stuhler G, Uharek L et al (2012) Allogeneic hematopoietic SCT in patients with AML following treosulfan/fludarabine conditioning. Bone Marrow Transplant 47:1171–1177. https://doi.org/10.1038/bmt.2011.242
Castaigne S, Pautas C, Terré C, Raffoux E, Bordessoule D, Bastie JN, Legrand O, Thomas X, Turlure P, Reman O et al (2012) Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): a randomised, open-label, phase 3 study. Lancet 379:1508–1516. https://doi.org/10.1016/s0140-6736(12)60485-1
Chiche E, Rahmé R, Bertoli S, Dumas PY, Micol JB, Hicheri Y, Pasquier F, Peterlin P, Chevallier P, Thomas X et al (2021) Real-life experience with CPX-351 and impact on the outcome of high-risk AML patients: a multicentric French cohort. Blood Adv 5:176–184. https://doi.org/10.1182/bloodadvances.2020003159
De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, Pappas PG, Maertens J, Lortholary O, Kauffman CA et al (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis 46:1813–1821. https://doi.org/10.1086/588660
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, Konopleva M, Döhner H, Letai A, Fenaux P et al (2020) Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med 383:617–629. https://doi.org/10.1056/NEJMoa2012971
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, Dombret H, Ebert BL, Fenaux P, Larson RA et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447. https://doi.org/10.1182/blood-2016-08-733196
Fernandez-Mercado M, Yip BH, Pellagatti A, Davies C, Larrayoz MJ, Kondo T, Pérez C, Killick S, McDonald EJ, Odero MD et al (2012) Mutation patterns of 16 genes in primary and secondary acute myeloid leukemia (AML) with normal cytogenetics. PLoS ONE 7:e42334. https://doi.org/10.1371/journal.pone.0042334
Flach J, Dicker F, Schnittger S, Schindela S, Kohlmann A, Haferlach T, Kern W, Haferlach C (2011) An accumulation of cytogenetic and molecular genetic events characterizes the progression from MDS to secondary AML: an analysis of 38 paired samples analyzed by cytogenetics, molecular mutation analysis and SNP microarray profiling. Leukemia 25:713–718. https://doi.org/10.1038/leu.2010.304
Gustafson SA, Lin P, Chen SS, Chen L, Abruzzo LV, Luthra R, Medeiros LJ, Wang SA (2009) Therapy-related acute myeloid leukemia with t(8;21) (q22;q22) shares many features with de novo acute myeloid leukemia with t(8;21)(q22;q22) but does not have a favorable outcome. Am J Clin Pathol 131:647–655. https://doi.org/10.1309/ajcp5ethdxo6ncgz
Hulegårdh E, Nilsson C, Lazarevic V, Garelius H, Antunovic P, Rangert Derolf Å, Möllgård L, Uggla B, Wennström L, Wahlin A et al (2015) Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish Acute Leukemia Registry. Am J Hematol 90:208–214. https://doi.org/10.1002/ajh.23908
Jentzsch M, Grimm J, Bill M, Brauer D, Backhaus D, Goldmann K, Schulz J, Niederwieser D, Platzbecker U, Schwind S (2020) ELN risk stratification and outcomes in secondary and therapy-related AML patients consolidated with allogeneic stem cell transplantation. Bone Marrow Transplant. https://doi.org/10.1038/s41409-020-01129-1
Jethava YS, Sica S, Savani B, Socola F, Jagasia M, Mohty M, Nagler A, Bacigalupo A (2017) Conditioning regimens for allogeneic hematopoietic stem cell transplants in acute myeloid leukemia. Bone Marrow Transplant 52:1504–1511. https://doi.org/10.1038/bmt.2017.83
Kahl C, Krahl R, Becker C, Al-Ali HK, Sayer HG, Schulze A, Herold M, Hänel M, Scholl S, Hochhaus A et al (2016) Long-term follow-up of the AML97 study for patients aged 60 years and above with acute myeloid leukaemia: a study of the East German Haematology and Oncology Study Group (OSHO). J Cancer Res Clin Oncol 142:305–315. https://doi.org/10.1007/s00432-015-2045-8
Kayser S, Döhner K, Krauter J, Köhne CH, Horst HA, Held G, von Lilienfeld-Toal M, Wilhelm S, Kündgen A, Götze K et al (2011) The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 117:2137–2145. https://doi.org/10.1182/blood-2010-08-301713
Kayser S, Zucknick M, Döhner K, Krauter J, Köhne CH, Horst HA, Held G, von Lilienfeld-Toal M, Wilhelm S, Rummel M et al (2012) Monosomal karyotype in adult acute myeloid leukemia: prognostic impact and outcome after different treatment strategies. Blood 119:551–558. https://doi.org/10.1182/blood-2011-07-367508
Kröger N, Bornhäuser M, Ehninger G, Schwerdtfeger R, Biersack H, Sayer HG, Wandt H, Schäfer-Eckardt K, Beyer J, Kiehl M et al (2003) Allogeneic stem cell transplantation after a fludarabine/busulfan-based reduced-intensity conditioning in patients with myelodysplastic syndrome or secondary acute myeloid leukemia. Ann Hematol 82:336–342. https://doi.org/10.1007/s00277-003-0654-9
Krug U, Röllig C, Koschmieder A, Heinecke A, Sauerland MC, Schaich M, Thiede C, Kramer M, Braess J, Spiekermann K et al (2010) Complete remission and early death after intensive chemotherapy in patients aged 60 years or older with acute myeloid leukaemia: a web-based application for prediction of outcomes. Lancet 376:2000–2008. https://doi.org/10.1016/S0140-6736(10)62105-8
Lancet JE, Uy GL, Cortes JE, Newell LF, Lin TL, Ritchie EK, Stuart RK, Strickland SA, Hogge D, Solomon SR et al (2018) CPX-351 (cytarabine and daunorubicin) liposome for injection versus conventional cytarabine plus daunorubicin in older patients with newly diagnosed secondary acute myeloid leukemia. J Clin Oncol 36:2684–2692. https://doi.org/10.1200/jco.2017.77.6112
Linassier C, Barin C, Calais G, Letortorec S, Brémond JL, Delain M, Petit A, Georget MT, Cartron G, Raban N et al (2000) Early secondary acute myelogenous leukemia in breast cancer patients after treatment with mitoxantrone, cyclophosphamide, fluorouracil and radiation therapy. Ann Oncol 11:1289–1294. https://doi.org/10.1023/a:1008375016038
Luger SM, Ringdén O, Zhang MJ, Pérez WS, Bishop MR, Bornhauser M, Bredeson CN, Cairo MS, Copelan EA, Gale RP et al (2012) Similar outcomes using myeloablative vs reduced-intensity allogeneic transplant preparative regimens for AML or MDS. Bone Marrow Transplant 47:203–211. https://doi.org/10.1038/bmt.2011.69
Niederwieser D, Maris M, Shizuru JA, Petersdorf E, Hegenbart U, Sandmaier BM, Maloney DG, Storer B, Lange T, Chauncey T et al (2003) Low-dose total body irradiation (TBI) and fludarabine followed by hematopoietic cell transplantation (HCT) from HLA-matched or mismatched unrelated donors and postgrafting immunosuppression with cyclosporine and mycophenolate mofetil (MMF) can induce durable complete chimerism and sustained remissions in patients with hematological diseases. Blood 101:1620–1629. https://doi.org/10.1182/blood-2002-05-1340
Niederwieser D, Al-Ali HK, Krahl R, Kahl C, Wolf H-H, Kreibich U, Vucinic V, Haehling D, Hegenbart U, Kraemer A et al (2014) Higher Leukemia free survival after post-induction hematopoietic cell transplantation compared to consolidation therapy in patients >60 years with Acute Myelogenous Leukemia (AML): report from the AML 2004 East German Study Group (OSHO). Blood 124:280–280. https://doi.org/10.1182/blood.V124.21.280.280
Ostgård LS, Kjeldsen E, Holm MS, Brown Pde N, Pedersen BB, Bendix K, Johansen P, Kristensen JS, Nørgaard JM (2010) Reasons for treating secondary AML as de novo AML. Eur J Haematol 85:217–226. https://doi.org/10.1111/j.1600-0609.2010.01464.x
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, Montesinos P, Baer MR, Larson RA, Ustun C et al (2019) Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med 381:1728–1740. https://doi.org/10.1056/NEJMoa1902688
Pollyea DA, Tallman MS, de Botton S, Kantarjian HM, Collins R, Stein AS, Frattini MG, Xu Q, Tosolini A, See WL et al (2019) Enasidenib, an inhibitor of mutant IDH2 proteins, induces durable remissions in older patients with newly diagnosed acute myeloid leukemia. Leukemia 33:2575–2584. https://doi.org/10.1038/s41375-019-0472-2
Reese ND, Schiller GJ (2013) High-Dose Cytarabine (HD araC) in the Treatment of Leukemias: a Review. Curr Hematol Malig Rep 8:141–148. https://doi.org/10.1007/s11899-013-0156-3
Roboz GJ, DiNardo CD, Stein EM, de Botton S, Mims AS, Prince GT, Altman JK, Arellano ML, Donnellan W, Erba HP et al (2020) Ivosidenib induces deep durable remissions in patients with newly diagnosed IDH1-mutant acute myeloid leukemia. Blood 135:463–471. https://doi.org/10.1182/blood.2019002140
Rücker FG, Schlenk RF, Bullinger L, Kayser S, Teleanu V, Kett H, Habdank M, Kugler CM, Holzmann K, Gaidzik VI et al (2012) TP53 alterations in acute myeloid leukemia with complex karyotype correlate with specific copy number alterations, monosomal karyotype, and dismal outcome. Blood 119:2114–2121. https://doi.org/10.1182/blood-2011-08-375758
Samra B, Richard-Carpentier G, Kadia TM, Ravandi F, Daver N, DiNardo CD, Issa GC, Bose P, Konopleva MY, Yilmaz M et al (2020) Characteristics and outcomes of patients with therapy-related acute myeloid leukemia with normal karyotype. Blood Cancer J 10:47. https://doi.org/10.1038/s41408-020-0316-3
Schmid C, Schleuning M, Hentrich M, Markl GE, Gerbitz A, Tischer J, Ledderose G, Oruzio D, Hiddemann W, Kolb HJ (2008) High antileukemic efficacy of an intermediate intensity conditioning regimen for allogeneic stem cell transplantation in patients with high-risk acute myeloid leukemia in first complete remission. Bone Marrow Transplant 41:721–727. https://doi.org/10.1038/sj.bmt.1705965
Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T (2004) Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia 18:120–125. https://doi.org/10.1038/sj.leu.2403187
Scholl S, Krause C, Loncarevic IF, Müller R, Kunert C, Wedding U, Sayer HG, Clement JH, Höffken K (2005) Specific detection of Flt3 point mutations by highly sensitive real-time polymerase chain reaction in acute myeloid leukemia. J Lab Clin Med 145:295–304. https://doi.org/10.1016/j.lab.2005.03.005
Scholl S, Theuer C, Scheble V, Kunert C, Heller A, Mügge LO, Fricke HJ, Höffken K, Wedding U (2008) Clinical impact of nucleophosmin mutations and Flt3 internal tandem duplications in patients older than 60 yr with acute myeloid leukaemia. Eur J Haematol 80:208–215. https://doi.org/10.1111/j.1600-0609.2007.01019.x
Shimoni A, Labopin M, Savani B, Volin L, Ehninger G, Kuball J, Bunjes D, Schaap N, Vigouroux S, Bacigalupo A et al (2016) Long-term survival and late events after allogeneic stem cell transplantation from HLA-matched siblings for acute myeloid leukemia with myeloablative compared to reduced-intensity conditioning: a report on behalf of the acute leukemia working party of European group for blood and marrow transplantation. J Hematol Oncol 9:118. https://doi.org/10.1186/s13045-016-0347-1
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B (2005) Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106:2912–2919. https://doi.org/10.1182/blood-2005-05-2004
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, Thiede C, Prior TW, Dohner K, Marcucci G et al (2017) Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med 377:454–464. https://doi.org/10.1056/NEJMoa1614359
Tauro S, Craddock C, Peggs K, Begum G, Mahendra P, Cook G, Marsh J, Milligan D, Goldstone A, Hunter A et al (2005) Allogeneic stem-cell transplantation using a reduced-intensity conditioning regimen has the capacity to produce durable remissions and long-term disease-free survival in patients with high-risk acute myeloid leukemia and myelodysplasia. J Clin Oncol 23:9387–9393. https://doi.org/10.1200/jco.2005.02.0057
Ustun C, Le-Rademacher J, Wang H-L, Othus M, Sun Z, Major B, Zhang M-J, Storrick E, Lafky JM, Chow S et al (2019) Allogeneic hematopoietic cell transplantation compared to chemotherapy consolidation in older acute myeloid leukemia (AML) patients 60–75 years in first complete remission (CR1): an alliance (A151509), SWOG, ECOG-ACRIN, and CIBMTR study. Leukemia 33:2599–2609. https://doi.org/10.1038/s41375-019-0477-x
Vulaj V, Perissinotti AJ, Uebel JR, Nachar VR, Scappaticci GB, Crouch A, Bixby DL, Burke PW, Maillard I, Talpaz M et al (2018) The FOSSIL Study: FLAG or standard 7+3 induction therapy in secondary acute myeloid leukemia. Leuk Res 70:91–96. https://doi.org/10.1016/j.leukres.2018.05.011
Walter MJ, Shen D, Ding L, Shao J, Koboldt DC, Chen K, Larson DE, McLellan MD, Dooling D, Abbott R et al (2012) Clonal architecture of secondary acute myeloid leukemia. N Engl J Med 366:1090–1098. https://doi.org/10.1056/NEJMoa1106968
Wong TN, Ramsingh G, Young AL, Miller CA, Touma W, Welch JS, Lamprecht TL, Shen D, Hundal J, Fulton RS et al (2015) Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature 518:552–555. https://doi.org/10.1038/nature13968
Yoshizato T, Nannya Y, Atsuta Y, Shiozawa Y, Iijima-Yamashita Y, Yoshida K, Shiraishi Y, Suzuki H, Nagata Y, Sato Y et al (2017) Genetic abnormalities in myelodysplasia and secondary acute myeloid leukemia: impact on outcome of stem cell transplantation. Blood 129:2347–2358. https://doi.org/10.1182/blood-2016-12-754796
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no conflicts of interest to declare that are relevant to the content of this article. The authors have no financial or proprietary interests in any material discussed in this article.
Informed consent
All patients were included in one of the following AML registries: AML registry of the OSHO study group (East German Study Group of Hematology and Oncology) or in the SAL registry (Study Alliance Leukemia). Patients gave their written informed consent for data acquisition and analysis after pseudonymization in one of the AML registries. The participation in both AML registries has been approved by the Ethical review committee of the University Hospital Jena.
Research involving human participants and/or animals
The presented study does not include research involving animals or pharacological research in human participants. The presented retrospective study was performed according to the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
432_2021_3733_MOESM1_ESM.pdf
Supplementary file1 Fig. S1 Clinical details and time course of patient’s history prior to diagnosis of t-AML (PDF 298 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fleischmann, M., Schnetzke, U., Frietsch, J.J. et al. Impact of induction chemotherapy with intermediate-dosed cytarabine and subsequent allogeneic stem cell transplantation on the outcome of high-risk acute myeloid leukemia. J Cancer Res Clin Oncol 148, 1481–1492 (2022). https://doi.org/10.1007/s00432-021-03733-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03733-0