Abstract
Severe obesity defined as BMI value corresponding to an adult > 40 kg/m2 affects 1–5% of children and adolescents in Europe. The purpose of this study was to assess the occurrence of cardiovascular risk factors in children and adolescents with severe obesity. The analysis included 140 patients (75 female) at the mean age of 14 ± 2.1 SD (range 10–18) years (all recruited in 4 regional reference centers in Poland). Severe obesity was defined as BMI > 35 kg/m2 (children 6–14 years), and BMI > 40 kg/m2 (> 14 years). Fasting plasma samples have been obtained in all patients, and OGTT was performed in all patients. The metabolic risk factors were defined as high blood pressure (BP > 90 percentile for height, age, and sex), HDL cholesterol < 1.03 mmol/L, TG ≥ 1.7 mmol/L, and hyperglycemic state (fasting blood glucose > 5.6 mmol/L, or blood glucose 120′ after oral glucose load > 7.8 mmol/L). Additionally, the MetS z-score was calculated using Metabolic Syndrome Severity Calculator. One hundred twenty-four (89%) participants presented with high BP, 117 (84%) with abnormal lipid profile, and 26 with the hyperglycemic. Only 12 (9%) were free of metabolic complications. More than 60% of patients had more than one cardiovascular risk factor. The high BP was significantly associated with the severity of obesity (F = 9.9, p = 0.002). Patients with at least one metabolic complication presented with significantly younger age of the onset of obesity (the mean age of the patients with no overt obesity complications was 10 years, while the mean age of those who presented at least one was 4.7 ± 3.5 SD years (p = 0.002)). A significant positive association between in the value of the Mets BMI z-score with age was observed (R = 0.2, p < 0.05). There were no differences between girls and boys regarding Mets BMI z-score (1.7 ± 0.8 vs 1.7 ± 0.7, p = 0.8).
Conclusions: The most common metabolic risk factor in children and adolescents with severe obesity was high BP. The most important factor determining presence of obesity complications, and thus the total metabolic risk, seems to be younger (< 5 years) age of onset of obesity.
What is Known? • It is estimated that 1-5% of children and adolescents in Europe suffer from severe obesity corresponding to an adult BMI > 40 kg/m2, and it is the fastest growing subcategory of childhood obesity. • Children with severe obesity face substantial health risk that may persist into adulthood, encompassing chronic conditions, psychological disorders and premature mortality. |
What is new: • The most common complication is high BP that is significantly associated with the severity of obesity (BMI z-score), contrary to dyslipidemia and hyperglycemic state, which do not depend on BMI z-score value. • The most important factor determining presence of obesity complications, and thus the total metabolic risk, seems to be younger (< 5 years) age of onset of obesity. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The term “morbid obesity” was introduced in mid-sixties of the twentieth century in order to justify insurance reimbursement for the cost of intestinal bypass surgery for weight loss in adult people with a BMI over 40 kg/m2 [1]. It defines severe, life-threatening excessive body weight. The terminology related to obesity is continually changing, and to respect for individuals dealing with this condition, it is now recommended rather to use “severe” instead of “morbid obesity” [2]. According to T.J. Cole and T. Lobstein, severe obesity in children can be defined as having a BMI of at least 35 kg m2, which can be also expressed as the 99.8th percentile at the age of 18 years [3]. Kelly et al. have defined severe obesity as BMI equal or above 99th percentile, BMI ≥ 120% of the 95th percentile, and as an absolute BMI ≥ 40 kg/m2 [2]. It is estimated that 1–5% of children and adolescents in Europe suffer from severe obesity corresponding to an adult BMI > 40 kg/m2. In the United States, the prevalence is even higher reaching 4–6% of the general pediatric population [4, 5]. What is particularly significant and worrying is the fastest growing subcategory of childhood obesity [2, 6]. Such a huge persistent excess of fatty tissue leads to the development of complications that increase the risk of heart and blood vessel diseases. Individuals with severe obesity face substantial health risk that may persist into adulthood, encompassing chronic conditions, psychological disorders and premature mortality [7,8,9,10]. The recent study revealed that adolescents with severe obesity face a greater than fourfold higher risk of a cardiovascular events within 30 years compared to normal-weight peers [11]. Nevertheless, typical, overt cardiovascular complications in children are much less common than in adults, despite similar BMI values. These risk factors with a common etiology may form clusters, and their negative effects may not only add up, but intensify. Moreover, each one disorder is not a separate disease, but a signal and an overt manifestation of impaired metabolism. The specific signs and symptoms are usually caused by a common underlying pathology, and their combination confers a risk that is different from the sum of the parts [12]. Therefore, comprehensive diagnostic and treatment, rather than activities aimed at improving individual metabolic parameters, is important.
The study aimed to assess the occurrence of cardiovascular risk factors in children and adolescents with severe obesity, to estimate the frequency of their co-occurrence and formation of clusters. Moreover, an attempt to assess the risk factors leading to the occurrence of single and grouped metabolic complications of obesity in children and adolescents with severe obesity.
Material and methods
Patients included in the analysis were participants of a multicenter project conducted in four specialized medical centers in Poland (Szczecin, Cracow, Zabrze, Rzeszow). This is a prospective multi-center clinical study performed with the sample size targeted is 500 patients aged 1–18 years, with severe obesity of an early origin, hyperphagia, and food-seeking behaviors.
This paper describes preliminary, partial results of the project [13].
Patients
The inclusion criteria were as follows: severe obesity defined as BMI > 35 kg/m2 (children in the age 6–14 years) and BMI > 40 kg/m2 (in older), written informed consent of the patient’s parent/guardian, and patient above the age of 13 years to participate in the study. The group was ethnically homogeneous.
Methods
Anthropometric assessment was performed in all patients (body weight, height, waist circumference measurement, and body composition analysis using the bioelectrical impedance method). Body weight was measured to the nearest 0.1 kg on a certified medical scale, body height was measured to the nearest 0.1 cm on Harpenden stadiometer, waist circumference was measured at the level of midpoint between the lowest rib and iliac crest, and hip circumference was measured at the level of the greatest convexity of the buttocks on the back and with cardboard applied tangentially to the greatest convexity of the abdomen on the front by measuring tape to the nearest 0.5 cm. Bioimpedance measurements were conducted using TANITA MC-580 M S MDD, TANITA MC-780MA-N, and TANITA MC-780 P MA devices. The office blood pressure (BP) was assessed with certified, calibrated oscillometer devices. A cuff size was appropriate to the arm size, while a participant was in a sitting position following a 15-min rest period before the examination. Results were interpreted according to European Society of Hypertension reference values [14]. High BP was defined as values > 90th percentile for sex, age and height [14].
Biochemical markers of cardiovascular risk were measured in each patient in a single fasting blood sample collected in the morning. Glucose, triglyceride (TG), and HDL cholesterol levels were analyzed. In order to more precisely analyze glucose metabolism disorders, patients underwent an oral glucose tolerance test, with the assessment of blood glucose concentration 120 min later after glucose load (75 g). The lipids cut-off values were based on the definition of metabolic syndrome in children and adolescents by IDF consensus report: TG ≥ 1.7 mmol/L and HDL < 1.03 mmol/L [15]. The diagnostic criteria for IFG was a fasting blood glucose of 100–125 mg/dL (5.6–6.9 mmol/L), IGT was defined as a 2-h plasma glucose level between 140 and 199 mg/dl (7.8–11.0 mmol/L) and DM as a fasting glucose level of 126 mg/dL (7.0 mmol/L) or higher (two abnormal readings required) or a two-hour plasma glucose level of more than 200 mg/dL (11.1 mmol/L) (one abnormal reading required) [16]. The MetS BMI z-score was calculated using Metabolic Syndrome Severity Calculator [17, 18].
Ethics approval statement
The study was conducted according to the guidelines of the Declaration of Helsinki “Ethical Principles for Medical Research in Humans” (9 July 2018). The study was approved by the local ethics committee (IRB)-Bioethics Committee of the Jagiellonian University (No. PCN/CBN/0022/KB1/137/I/21/22, KBETUJ 1072.6120.69.2022, KB-006/12/2022).
Results
The analysis included 140 patients (75 female) with severe obesity at the mean age of 14.0 ± 2.0 SD (range 10–18) years at time of the study. The mean BMI z-score in the study group was 3.7 ± 0.4 SD. Female patients presented with significantly lower BMI z-score (3.5 vs. 3.8, p < 0.001), but higher fat mass percent (48.3 ± vs. 44.6, p < 0.001) compared to male. They had also lower mean fasting glucose levels (4.8 vs. 5.0 mmol/L, p < 0.008) and higher mean HDL cholesterol levels (43.7 vs. 40.1 mg/dL, p = 0.01) compared to male patients (Table 1.). The present study revealed that the most common disorder in adolescents with severe obesity was high BP (diagnosed in 124 [89%] of participants) (Fig. 1). One hundred seventeen (84%) presented with abnormal lipid profile (58 [41%] with isolated low HDL, 44 [31%] isolated high TG, and 62 [44%] with both disorders), 26 [18%] with the hyperglycemic state (3 (2%) impaired fasting glucose, 20 (14%) impaired glucose tolerance, and 2 (1%) diabetes mellitus). No significant differences were found in the frequency of disorders depending on sex. Only 12 (9%) were free of the overt metabolic syndrome features (Fig. 1). A single metabolic complication was noticed in 33 (25%) of participants, two were present in 85 (62%), and three (high BP, hyperglycemic state, and dyslipidemia) were in 10 (14%) participants (Fig. 2). The most common combination was high BP and dyslipidemia (59%). High BP and disorders of glucose metabolism were present in 2% of patients and lipid disorders and glucose metabolism disorders in 1%. All three metabolism disorders were present in 14% of patients. Patients with the co-occurrence of 2 or more disorders were characterized by a younger age at the onset of obesity compared to patients with one or no complication (Fig. 3c). The mean age of the patients with no overt obesity complications was 10 ± 2.8 SD years, while the mean age of those who presented with 1.2 or 3 was 4.4 ± 2.0SD, 4.8 ± 2.1 SD, and 4.8 ± 1.8 SD, respectively. The difference was statistically significant when comparing the age of children without complications to those with at least one (p = 0.002). Differences in the age at which obesity occurred were not statistically significant when we compared groups with 1, 2, or 3 complications. The incidence of the number of cardiovascular risk factors increased with increasing BMI z-score but the relationship was not statistically significant (p = 0.2) (Fig. 3a). Similar effect was observed for waist circumference (mean 106.5 cm in those with no disorders and 114.6 cm, 115.8 cm, and 117.8 cm in those with 1, 2, and 3, respectively) (not shown). There was no significant difference regarding the fat mass % (46.6% in those with no disorders, and 46%, 47%, and 46% in those with 1, 2, or 3 respectively) (Fig. 3d). There was no association between birth weight and the number of metabolic complications of obesity.
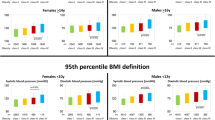
Multivariate regression analysis revealed that high BP was significantly associated with the severity of obesity (BMI z-score) [F(1, 132) = 9.9, p = 0.002]. For dyslipidemia [F(1, 132) = 0.5, p = 0.5, 95% CI] and for hyperglycemic state [F(1, 132) = 0.02, p = 0.9], the association with BMI z-score was not statistically significant (Fig. 4). Patients with high BP had significantly higher BMI z-score compared to patients with normal BP (3.7 ± vs. 3.3 ± , p = 0.001). The Mets BMI z-score increased with the age (R = 0.2, p < 0.05). There were no differences in Mets BMI z-score between girls and boys (1.7 ± 0.8 vs 1.7 ± 0.7, p = 0.8).
The relationship between the occurrence of cardiovascular risk factors and BMI z-score. Statistical significance was demonstrated for the relationship between BMI z-score and high blood pressure (a) (F(1, 132) = 9.9, p = 0.002). For hyperglycemic state [F(1, 132) = 0.02, p = 0.9] (b) and dyslipidemia (c) [F(1, 132) = 0.5, p = 0.5], the relationship with BMI z-score was not statistically significant. 0—no disorder, 1—disorder present. *Statistically significant differences
Discussion
There is no doubt that obesity leads to the development of complications that constitute direct risk factors for heart and vascular diseases. The data from literature show, that in adult patients this cardiovascular risk is greater in people with severe obesity in comparison to moderate obesity [19]. In a cohort of Danish and Finnish subjects, each increase in BMI z-score at 7 years of age (equivalent to a 1.5 to 2.5 kg/m2 increment) was associated with a 5%-10% greater risk of coronary heart disease in adulthood [20]. In few studies conducted among teenagers with severe obesity, it was shown that they have a worse cardiometabolic risk profile including increased numbers of risk factors such as higher BP, dyslipidemia, diabetes mellitus, hyperglycemia, or hyperinsulinemia [9, 11,12,13,14,15,16,17,18,19,20,21,22,23]. It also appears that severely obese patients are predisposed to a greater number of cardiovascular risk factors, known as the metabolic syndrome [24]. The present study revealed that at least metabolic complication occurred in 91.5% of participants. It was only one disorder in 24%, two in 61%, and three in 7% of participants. This is a higher percentage than shown in a similar, but nationwide prospective surveillance study from the Netherlands, that showed at least one cardiovascular risk factor in 67% patients with severe obesity and two, three and more than three risk factors in 17%, 8%, and 2.5%, respectively. The most frequently reported cardiovascular risk factor was arterial hypertension [7]. A study from the USA reported results similar to our study: 84% of pediatric patients (age 5–17) with severe obesity had at least one cardiovascular risk factor [8]. In the study form the Netherlands, the most common complication of obesity in children and adolescents was arterial hypertension [7]. The incidence of high BP among children around the world is increasing in parallel with the increase in body weight [8, 24, 25]. This is also confirmed by the results of the present study, in which high BP was diagnosed in almost 90% of participants. Studies in adults have shown that the risk of hypertension increased according to the higher BMI [24], with the odds of hypertension as great as 4.8 among adults with class III obesity (BMI ≥ 40 kg/m2) when compared to adults with a normal BMI [26]. In the study by Sorof et al. the systolic BP increases progressively to BMI percentile [27]. In a cross-sectional retrospective US cohort, children with severe obesity and mild obesity had an odds ratio of 4 and 2 for hypertension, respectively, compared to children with normal weight [28]. Similarly in a nationwide cross-sectional Israeli cohort, odds ratios for hypertension ranged from 2.1 to 3.4 among girls and boys with severe obesity, and from 1.4 to 1.8 among those with mild obesity, compared to children with overweight [29]. In the most studies that assessed cardiometabolic risk factors according to BMI status, higher mean values of TG, and lower mean values for HDL were observed [21, 30,31,32]. Data from the literature shows that higher prevalence and increasing trends of abnormal values of HDL cholesterol, triglyceride (TG) levels, and systolic and diastolic BP were observed with increasing BMI categories [33,34,35,36,37]. The cross-sectional study by Norris AL who investigated 225 children adolescents with normal weight, overweight, obesity, and severe obesity revealed that values of BP, and the levels of insulin, and lipids worsened with the higher BMI [31]. In the present study, the presence of higher number of the complications increased parallel to BMI z-score; however, it was not statistically significant. The Bogalusa Heart Study established that schoolchildren with overweight were 2.4 to 7.1 times more likely to have elevated total cholesterol, LDL, and TG in comparison to thin peers [8]. The NHANES data indicate this pattern is highly prevalent, present in 42.9% of children with BMI > 95th% percentile. In observational, cross-sectional, retrospective study among Obese Children and Adolescents in Turkey the prevalence of dyslipidemia was 56.7%. A relatively low HDL-C together with a high TG was observed. From the participants, 644 (56.7%) cases met the study criteria for dyslipidemia, including 16% with high TC, 15% with high LDL-C, 36.8% with low HDL-C, and 25.9% with high TG. There was no difference in the frequency of dyslipidemia according to gender (p = 0.15). While dyslipidemia was seen in 62.3% of pubertal children, this was significantly less prevalent (49.4%) in prepubertal children (p < 0.001). Hypertriglyceridemia and low HDL-C were present at significantly higher rates in pubertal children (p < 0.001) [38]. Deeb et al. found that 55.3% of 216 children with obesity and overweight enrolled in the study had dyslipidemia [39]. Brzezinski et al. reported the incidence as approximately 69.9%. At least one of the lipid disorders occurred in 38.23% of girls and 40.51% of boys with overweight and obesity. The most common lipid disorders were decreased high-density lipoprotein cholesterol (HDL-C) levels (present in 20.55% of the girls and 23.79% of the boys) and elevated low-density lipoprotein cholesterol (LDL-C) (present in 15.31% of the girls and 14.25% of the boys) [40]. Nielsen et al. demonstrated the risk of developing lipid disorders is 2.8 times higher in obese children (BMI > 90th percentile) than in children with normal body weight [41]. The rarest disorder in the present study was hyperglycemia. According to the literature data in young adults, each 1-kg/m2 increase in BMI was associated with a 6% higher risk of developing type 2 diabetes before the age of 45 years [42]. In severely obese children and adolescents in cross-sectional studies, prediabetes was detected in 22–36% children and adolescents [43]. In the study by Propst et al. a retrospective electronic chart review was conducted on 1111 obese and morbidly obese children. Prediabetes was found in 19.5% of obese subjects and in 27.3% of morbidly obese ones. Moreover, 39.8% of obese children and 52.4% of morbidly obese ones had type 2 diabetes [44]. The present study is the first attempt to analyze the potential factors contributing to the development of metabolic complications in pediatric patients with severe obesity. There was an association between the age of the onset of obesity and development of cardiovascular risk. Interestingly, the presence and number of risk factors was not associated with fat mass, nor waist circumference. Contrary to adults in whom waist circumference is considered as an independent risk factor for metabolic syndrome, more important than BMI itself [19]. In the present study the incidence of more complications increased parallel to BMI z-score (mean BMI z-score 3.3 in those with no overt cardiovascular risk factors to 3.5, 3.7, and 3.8 in those with 1, 2, or 3 disorders), but the relationship was not statistically significant (p = 0.2).
Limitations of the study
The main study limitation is the relatively modest size of the group. The inclusion criteria focused on children and adolescents with extreme obesity, which naturally impacts the number of patients. Moreover, this is a relatively underrepresented group in existing literature. An important factor to consider is that there was a marked disproportion between the number of children in the complication-free subgroup and those with 1, 2, or 3 disorders. Due to the frequent occurrence of disorders in children and adolescents with severe obesity, it would probably be difficult to gather a sufficiently large group free from cardiovascular risk factors. Another limitation pertains to the fact that biochemical and hormonal tests, as well as BIA measurements, were conducted in different laboratories using different equipment. Nonetheless, all gathered data were compared against center-specific standards.
Conclusions
The most common cardiovascular risk factor in children and adolescents with severe obesity was high BP. Over 60% of patients had more than one cardiovascular risk factor. The most important factor determining presence of obesity complications, and thus the total metabolic cardiovascular risk, seems to be younger (< 5 years) age of onset of obesity.
Data availability
Data can be provided on demand, after a contact with corresponding author.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- DM:
-
Diabetes mellitus
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- OGTT:
-
Oral glucose tolerance test
- TG:
-
Triglycerides
References
Payne JH, DeWind LT, Commons RR (1963) Metabolic observations in patients with jejunocolic shunts. Am J Surg 106(2):273–289
Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, Steinberger J et al (2013) Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches. Circulation 128(15):1689–1712
Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes 7(4):284–294
Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR (2009) Characterizing extreme values of body mass index–for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr 90(5):1314–1320
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK et al (2016) Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 Through 2013–2014. JAMA 315(21):2292
Pinhas-Hamiel O, Hamiel U, Bendor CD, Bardugo A, Twig G, Cukierman-Yaffe T (2022) The global spread of severe obesity in toddlers, children, and adolescents: a systematic review and meta-analysis. Obes Facts 15(2):118–134
Van Emmerik NMA, Renders CM, Van De Veer M, Van Buuren S, Van Der Baan-Slootweg OH, Kist-van Holthe JE et al (2012) High cardiovascular risk in severely obese young children and adolescents. Arch Dis Child 97(9):818–21
Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH (2007) Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr 150(1):12-17.e2
Ice CL, Murphy E, Cottrell L, Neal WA (2011) Morbidly obese diagnosis as an indicator of cardiovascular disease risk in children: results from the CARDIAC Project. Int J Pediatr Obes 6(2):113–119
Zolotarjova J, ten Velde G, Vreugdenhil ACE (2018) Effects of multidisciplinary interventions on weight loss and health outcomes in children and adolescents with morbid obesity. Obes Rev 19(7):931–946
Ryder JR, Xu P, Inge TH, Xie C, Jenkins TM, Hur C et al (2020) Thirty-year risk of cardiovascular disease events in adolescents with severe obesity. Obesity 28(3):616–623
Brambilla P, Lissau I, Flodmark CE, Moreno LA, Widhalm K, Wabitsch M et al (2007) Metabolic risk-factor clustering estimation in children: to draw a line across pediatric metabolic syndrome. Int J Obes 31(4):591–600
Mierzwa M, Bik-Multanowski M, Ranke MB, Brandt S, Flehmig B, Małecka-Tendera E et al (2022) Clinical, genetic, and epidemiological survey of Polish children and adolescents with severe obesity: a study protocol of the Polish-German study project on severe early-onset obesity. Front Endocrinol (Lausanne) 21:13
Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, Invitti C, Litwin M, Mancia G, Pall D, Rascher W, Redon J, Schaefer F, Seeman T, Sinha M, Stabouli S, Webb NJ, Wühl E, Zanchetti A (2016) 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens 34(10):1887–1920. https://doi.org/10.1097/HJH.0000000000001039.
Zimmet P, Alberti KG, Kaufman F, Tajima N, Silink M, Arslanian S, Wong G, Bennett P, Shaw J, Caprio S, IDF Consensus Group (2007) The metabolic syndrome in children and adolescents - an IDF consensus report. Pediatr Diabetes 8(5):299–306
Araszkiewicz A, Bandurska-Stankiewicz E, Borys S et al (2023) 2023 Guidelines on the management of patients with diabetes - a position of Diabetes Poland. Curr Top Diabetes 3(1):1–133. https://doi.org/10.5114/ctd/160061
Gurka MJ, Ice CL, Sun SS, DeBoer MD (2012) A confirmatory factor analysis of the metabolic syndrome in adolescents: an examination of sex and racial/ethnic differences. Cardiovasc Diabetol 11. Available from: https://pubmed.ncbi.nlm.nih.gov/23062212/
Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ et al (2021) Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 143(21):e984. Available from: /pmc/articles/PMC8493650/
Andersen LG, Ängquist L, Eriksson JG, Forsen T, Gamborg M, Osmond C et al (2010) Birth weight, childhood body mass index and risk of coronary heart disease in adults: combined historical cohort studies. PLoS ONE 5(11):e14126
Gidding SS, Nehgme R, Heise C, Muscar C, Linton A, Hassink S (2004) Severe obesity associated with cardiovascular deconditioning, high prevalence of cardiovascular risk factors, diabetes mellitus/hyperinsulinemia, and respiratory compromise. J Pediatr 144(6):766–769
Norris AL, Steinberger J, Steffen LM, Metzig AM, Schwarzenberg SJ, Kelly AS (2011) Circulating oxidized LDL and inflammation in extreme pediatric obesity. Obesity (Silver Spring) 19(7):1415–9. Available from: https://pubmed.ncbi.nlm.nih.gov/21331062/
Bass R, Eneli I (2015) Severe childhood obesity: an under-recognised and growing health problem. Postgrad Med J. 91(1081):639–45. Available from: https://pubmed.ncbi.nlm.nih.gov/26338983/
Rank M, Siegrist M, Wilks DC, Langhof H, Wolfarth B, Haller B et al (2013) The cardio-metabolic risk of moderate and severe obesity in children and adolescents. J Pediatr 163(1):137–42. Available from: http://www.jpeds.com/article/S0022347613000449/fulltext
Flynn J (2013) The changing face of pediatric hypertension in the era of the childhood obesity epidemic. Pediatr Nephrol 28(7):1059–1066
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS (2008) Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg 207(6):928–934
Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ (2004) Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics 113(3):475–482
Parker ED, Sinaiko AR, Kharbanda EO, Margolis KL, Daley MF, Trower NK et al (2016) Change in weight status and development of hypertension. Pediatrics [Internet]. [cited 2023 Sep 18];137(3). Available from: https://pubmed.ncbi.nlm.nih.gov/26908707/
Twig G, Reichman B, Afek A, Derazne E, Hamiel U, Furer A et al (2019) Severe obesity and cardio-metabolic comorbidities: a nationwide study of 2.8 million adolescents. Int J Obes (Lond) [Internet]. [cited 2023 Sep 18];43(7):1391–9. Available from: https://pubmed.ncbi.nlm.nih.gov/30258119/
Rijks JM, Plat J, Mensink RP, Dorenbos E, Buurman WA, Vreugdenhil ACE (2015) Children with morbid obesity benefit equally as children with overweight and obesity from an ongoing care program. J Clin Endocrinol Metab 100(9):3572–3580
Norris AL, Steinberger J, Steffen LM, Metzig AM, Schwarzenberg SJ, Kelly AS (2011) Circulating oxidized LDL and inflammation in extreme pediatric obesity. Obesity 19(7):1415–1419
Kapiotis S, Holzer G, Schaller G, Haumer M, Widhalm H, Weghuber D et al (2006) A proinflammatory state is detectable in obese children and is accompanied by functional and morphological vascular changes. Arterioscler Thromb Vasc Biol 26(11):2541–6. Available from: https://pubmed.ncbi.nlm.nih.gov/16973973/
Skinner AC, Perrin EM, Moss LA, Skelton JA (2015) Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med 373(14):1307–17. Available from: https://pubmed.ncbi.nlm.nih.gov/26422721/
Propst M, Colvin C, Griffin RL, Sunil B, Harmon CM, Yannam G et al (2015) Diabetes and prediabetes are significantly higher in morbidly obese children compared with obese children. Endocr Pract 21(9):1046–53. Available from: http://www.endocrinepractice.org/article/S1530891X20357220/fulltext
Li L, Pérez A, Wu LT, Ranjit N, Brown HS, Kelder SH (2016) Cardiometabolic risk factors among severely obese children and adolescents in the United States, 1999–2012. Child Obes 12(1):12–9. Available from: https://pubmed.ncbi.nlm.nih.gov/26785314/
Cho WK, Han K, Ahn MB, Park YM, Jung MH, Suh BK et al (2018) Metabolic risk factors in Korean adolescents with severe obesity: results from the Korea National Health and Nutrition Examination Surveys (K-NHANES) 2007–2014. Diabetes Res Clin Pract 138:169. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6221804/pdf/nihms-946992.pdf
Marcus MD, Foster GD, El Ghormli L (2014) Stability of relative weight category and cardiometabolic risk factors among moderately and severely obese middle school youth. Obesity (Silver Spring) 22(4):1118. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968217/pdf/nihms551090.pdf
Dündar I, Akıncı sehan (2022) Frequency of dyslipidemia and associated risk factors among obese children and adolescents in Turkey. 32(3)
Deeb A, Attia S, Mahmoud S, Elhaj G, Elfatih A (2018) Dyslipidemia and fatty liver disease in overweight and obese children. J Obes 2018:8626818. Available from: https://pubmed.ncbi.nlm.nih.gov/30009050/
Brzeziński M, Metelska P, Myśliwiec M, Szlagatys-Sidorkiewicz A (2020) Lipid disorders in children living with overweight and obesity- large cohort study from Poland. Lipids Health Dis 19(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7076982/pdf/12944_2020_Article_1218.pdf
Nielsen TRH, Lausten-Thomsen U, Fonvig CE, Bøjsøe C, Pedersen L, Bratholm PS et al (2017) Dyslipidemia and reference values for fasting plasma lipid concentrations in Danish/North-European White children and adolescents. BMC Pediatr 17(1):116. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5410076/pdf/12887_2017_Article_868.pdf
Hillier TA, Pedula KL (2001) Characteristics of an adult population with newly diagnosed type 2 diabetes The relation of obesity and age of onset. Diabetes Care 24(9):1522–7. Available from: https://doi.org/10.2337/diacare.24.9.1522
Ek AE, Rössner SM, Hagman E, Marcus C (2015) High prevalence of prediabetes in a Swedish cohort of severely obese children. Pediatr Diabetes 16(2):117–28. Available from: https://pubmed.ncbi.nlm.nih.gov/24635861/
Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K et al (2002) Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 346(11):802–810
Funding
This research was funded in whole by National Science Center, Poland (2021/41/B/NZ5/01676).
Author information
Authors and Affiliations
Contributions
E.S. and A.S. collected data and wrote the main manuscript. M.B.M. performed laboratory analysis, collected data, and wrote the main manuscript. S.B.H. analyzed data and wrote the main manuscript. B.F. wrote the main manuscript and supervised study. E.M.T. wrote the main manuscript and supervised study. A.M. and E.P. collected data, wrote the main manuscript, and supervised the study. M.B.R. and M.W. wrote the main manuscript and supervised the study. A.Z. created the study, acquired funding, collected data, wrote the main manuscript, and supervised the study. M.W. collected and analyzed data, created figures, wrote the main manuscript, and supervised the study. The authors contributed equally.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Open access
For the purpose of Open Access, the authors have applied a CC-BY public copyright license to any Author Accepted Manuscript (AAM) version arising from this submission.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szczudlik, E., Stępniewska, A., Bik-Multanowski, M. et al. The age of the obesity onset is a very important factor for the development of metabolic complications and cardiovascular risk in children and adolescents with severe obesity. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05636-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00431-024-05636-x