Abstract
Congenital central hypoventilation syndrome (CCHS) is a rare genetic disorder characterized by hypoventilation due to impaired breathing control by the central nervous system and other symptoms of autonomic dysfunction. Mutations in paired-like homeobox 2 B (PHOX2B) are responsible for most cases of CCHS. Patients with CCHS have various phenotypes and severities, making the diagnosis difficult. This study aimed to present a comprehensive single-center experience of patients with CCHS, including key clinical features, treatment strategies, and outcomes. A retrospective chart review was performed for patients diagnosed with CCHS between January 2001 and July 2023 at Seoul National University Children’s Hospital. Finally, we selected 24 patients and collected their demographic data, genotypes, ventilation methods, and clinical features related to autonomic dysfunction. The relationship between the clinical manifestations and genotypes was also examined. All patients used home ventilators, and tracheostomy was performed in 87.5% of patients. Fifteen (62.5%) patients had constipation and nine (37.5%) were diagnosed with Hirschsprung disease. Arrhythmia, endocrine dysfunction, and subclinical hypothyroidism were present in nine (37.5%), six patients (25.0%), and two patients (16.7%), respectively. A significant number of patients exhibited neurodevelopmental delays (19 patients, 79.2%). There was a correlation between the phenotype and genotype of PHOX2B in patients with CCHS. (r = 0.71, p < 0.001).
Conclusion: There was a positive correlation between paired-like homeobox 2 B mutations (especially the number of GCN repeats in the polyalanine repeat mutations sequence) and clinical manifestations. This study also demonstrated how initial treatment for hypoventilation affects neurodevelopmental outcomes in patients with CCHS.
What is Known: • Congenital central hypoventilation syndrome is a rare genetic disorder characterized by hypoventilation and dysfunction of autonomic nervous system. • The disease-defining gene of CCHS is PHOX2B gene – most of the cases have heterozygous PARMs and the number of GCN triplets varies among the patients(20/24 – 20/33). | |
What is New: • We have noted in the Korean patients with CCHS that there is a correlation between genotype (number of GCN repeats) and severity of phenotype. • National support for rare diseases allowed for a prompter diagnosis of patients with CCHS in Korean population. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital central hypoventilation syndrome (CCHS) is a rare genetic disorder characterized by hypoventilation, particularly during sleep, due to impaired central control of breathing and autonomic dysfunction. While the incidence of CCHS has been reported to be 1 case per 148,000 live births in Japan and 1 case per 200,000 live births in France [1, 2] recent incidence of CCHS in Korea is estimated to be 1/52,000–1/90,000 live births [3]. Clinical hallmarks of CCHS include central hypoventilation and sleep apnea due to reduced or absent ventilatory responses to hypercapnia and hypoxia and associated autonomic nervous system dysfunction (ANSD) manifestations, such as Hirschsprung disease (HD), cardiac arrhythmia, and neural crest-derived tumors [4]. Most cases present with clinical symptoms in the neonatal period due to hypoventilation; however, later-onset presentations are increasingly recognized during childhood and adulthood [4].
Paired-like homeobox 2B (PHOX2B) is a disease-defining gene in patients with CCHS. Associated PHOX2B mutations are mostly related to the expansion of GCN triplets in the 20 polyalanine coding regions in exon 3, defined as polyalanine repeat mutations (PARMs). Most cases had heterozygous PARMs for alanine residues 24–33, with genotypes expressed as 20/24–20/33. A minority of patients with CCHS have a non-PARM (NPARM) mutation, in which the gene is mutated outside the PARM frame, including frameshift, nonsense, and missense mutations of PHOX2B. A genotype–phenotype correlation of symptom severity has been described according to the number of polyalanine repeats of PARMs, and NPARMs are generally associated with the most severe symptoms [5, 6].
The increase in CCHS awareness over the last decade has resulted in earlier screening and interventions for patients with CCHS [7]. Therefore, recent studies have focused not only on patient survival but also on neurodevelopment and cognitive skills [8]. In 2017, the Korean Ministry of Health and Welfare designated CCHS as a rare disease, which means that medical care is covered by the national insurance copayment system, and awareness of CCHS has increased. The clinical features, treatment strategies, and outcomes of Korean patients with CCHS have not been previously reported.
We aimed to present a comprehensive single-center experience of patients with CCHS, including key clinical features, treatment strategies, and outcomes. To date, this is the first and largest cohort of patients with CCHS in South Korea.
Materials and methods
Study design
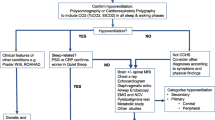
A retrospective chart review was performed on patients diagnosed with CCHS between January 2001 and July 2023 at Seoul National University Hospital (SNUH). First, we screened patients with CCHS diagnostic codes in the in-hospital clinical data warehouse (CDW) SUPREME. Patients who underwent PHOX2B genetic analysis were included in this study. Patients with missing variant information and those with benign, likely benign, or variants of uncertain significance (VUS) were excluded (Fig. 1). After collecting demographic data, genotypes, ventilation methods, and clinical features related to autonomic dysfunction, clinical manifestations, and management according to genotype were reviewed. Patients were also categorized into those born before and after CCHS was designated as a rare disease in Korea in June 2017. The clinical characteristics and management were compared between the two groups. Institutional Review Board (IRB) approval (IRB no. 2307–027-1474) was obtained from SNUH for a retrospective observational study with a waiver of informed consent.
Genetic study
Peripheral blood samples were collected from patients clinically suspected of having CCHS. The 5'UTR coding region and its flanking region of exons 1–3 of the PHOX2B (OMIM:603851) gene were analyzed by polymerase chain reaction and direct sequencing, and the deletion/duplication of each exon was examined by MLPA kit P318-A1 (Lot# 1009, MRC Holland, Amsterdam, Netherlands). The reference sequences were NC_000004.11, NM_003924.3, and the basic mutation data were obtained from the Human Gene Mutation Database (http://www.hgmd.cf.ac.uk/ac/). For nucleotide numbering, ATG (initiation codon NM_003924.3) was designated as the first codon in the sequence. The clinical manifestations of each base mutation were determined in accordance with the 2015 recommendations of the American College of Medical Genetics and Genomics [9, 10].
Genotypes of PARM mutations are expressed as ‘20/24 ~ 20/33’, where the first number represents the wild type of 20 polyalanine repeats, and the second number specifies the mutation of 24 to 33 polyalanine repeats.
Phenotype data
To collect phenotypic data, pertinent data from medical records, including birth weight, gestational age, height, weight, vital signs, ventilator setting records, laboratory data, echocardiography, electrocardiogram, electroencephalogram, radiologic evaluation of the abdomen and brain, surgical records, and medication prescriptions, were thoroughly reviewed. Symptoms related to ANSD were also recorded. The neurodevelopmental outcomes were evaluated by pediatric neurologists and rehabilitation specialists.
Statistical analysis
Data are presented as number (percentage) or median (interquartile range). The correlation between the genotype and phenotype was analyzed using the Spearman rank correlation test. To compare the clinical features and management of patients born before and after the CCHS rare disease designation, non-parametric testing was performed. Fisher’s exact test was used to compare proportions, and Wilcoxon rank sum test was used to compare medians. Height, weight, and body mass index (BMI) z-scores were calculated according to the 2017 Korean National Growth Charts [11]. The growth parameter z-scores for each age group were compared to 0 using the one-way Wilcoxon rank-sum test. Statistical significance was set at P < 0.05. All statistical analyses were performed using R version 4.3.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Demographic characteristics of selected subjects
The CDW search for patients with CCHS yielded 52 patients, and after review of PHOX2B genetic studies, 20 patients were excluded due to missing gene studies and six patients were excluded due to benign/likely benign variants, VUS, or missing variant information. Twenty-four patients were included in this study (Fig. 1). The study participants’ age ranged from 2 months to 26 years, and the median age at the time of the study was 8 years. Ten patients (41.7%) were male and 17 (70.8%) were born at term, with a median birth weight of 2.873 kg (Table 1). Most patients with CCHS (22 patients, 91.7%) presented with apnea or hypopnea during the neonatal period (within 1 month) and were admitted to the NICU due to respiratory distress, except for two patients who presented symptoms at a later onset (each of them had symptoms at 2 and 36 months after birth). The median age of patients who underwent PHOX2B analysis was 2 months. Four patients had a family history of CCHS and were identified as two couples of monozygotic twins (Table 1).
PHOX2B genotypes
The PHOX2B genetic study revealed that 22 patients (91.7%) had PARMs and two patients (8.3%) had NPARMs. The most common PARM genotype was 20/27 (11 patients, 45.8%), followed by 20/26 (8 patients, 33.3%). There was one patient each with genotypes 20/25, 20/28, and 20/31.
Assisted ventilation
All patients used home ventilators, and tracheostomy was performed in 87.5% (21 out of 24) of patients at 1–5 months of age (Table 1). Among the patients who underwent tracheostomy, seven were successfully decannulated at school-age and switched from the T-cannula interface to the nasal or oronasal mask. None of the patients with a high number of GCN repeats (≥ 28) or NPARM underwent decannulation (Table 2).
All patients started on 24-h ventilator use during the neonatal period; currently, 21 patients (87.5%) use ventilators only during sleep. The three patients who were on full-time ventilation included one infant who was currently 6 months old and two patients who had undergone severe hypoxic ischemic brain damage. Various ventilator modes were used; pressure-support ventilatory (PSV) mode with back up rate for 8 patients (66.7%, 8 out of 24), pressure-controlled synchronized intermittent mandatory ventilation (SIMV) mode for 5 patients (20.8%, 5 out of 24), spontaneous-timed mode for 2 patients (8.3%, 2 out of 24), pressure-controlled (assist control) mode for 4 patients (16.7%, 4 out of 24), and continuous positive airway pressure (CPAP) for one patient.
Symptoms related to ANSD
Fifteen patients (62.5%) had some degree of constipation requiring treatment. Hirschsprung disease (HD) was diagnosed in twelve patients (50.0%) who underwent a Soave procedure for aganglionosis. All patients with NPARM and genotypes 20/28 and 20/31 had gastrointestinal symptoms, while 72.7%, 37.5%, and 0% had symptoms associated with genotypes 20/27, 20/26, and 20/25, respectively (Fig. 2).
Arrhythmia was present in nine patients (37.5%); one patient had sinus tachycardia and eight patients had sinus bradycardia, of which two patients experienced sinus arrest and were implanted with a loop recorder for electrocardiography monitoring. Half of patients with the PARM genotypes 20/28 and 20/31 had arrhythmias. In total, 57.5% and 12.5% of the patients with genotypes 20/27 and 20/26, respectively, had arrhythmia (Fig. 2).
Endocrine dysfunctions, such as abnormal thyroid function and impaired glycemic control, were also present. Six patients (25.0%) experienced impaired glycemic control with either hyperglycemia or hypoglycemia. One patient was diagnosed with diabetes mellitus and treated with insulin and metformin. Two (16.7%) patients were diagnosed with subclinical hypothyroidism (Fig. 2).
Ophthalmic disorders, including pupillary abnormalities, astigmatism, and strabismus, were also found in seven patients (29.2%). Neuroblastoma was present in one patient with NPARM (4.2%), who underwent excisional biopsy.
Neurologic features
A wide spectrum of neurological symptoms were prevalent in our cohort. Twenty patients (83.3%) had some degree of developmental delay, including in speech and language development. One patient had ADHD and two had moderate to severe autism spectrum disorder. Nine patients (54.2%) presented with documented seizures and epileptiform discharges on electroencephalography (Fig. 2).
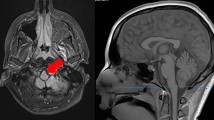
Of the 14 patients with available brain imaging (including MRI and ultrasonography), 57.1% (8 out of 14) had abnormal brain imaging; 62.5% of the patients with abnormal imaging (5 out of 8) had a mild to severe degree of diffuse brain atrophy, four patients (50%) had hypoxic ischemic encephalopathy, and two had intracranial hemorrhage due to hypoxia.
Genotype–phenotype relationship of PHOX2B gene in CCHS
When the number of symptoms, including gastrointestinal symptoms, arrhythmia, endocrine dysfunction, ophthalmologic symptoms, neural crest tumors, and neurocognitive symptoms, were plotted across genotypes, the number of phenotypes ranged from 0 to 5 (Fig. 3). Patients with NPARMs have several clinical manifestations. Patients with fewer GCN repeats tended to exhibit fewer phenotypes. There was a positive correlation between the genotypes in our study, treated as ordinal values, and the number of phenotypes (p < 0.001).
Growth parameters
The height and weight of 22 patients were recorded. Eighteen patients had a median height z-score below 0, and four patients (18.2%) had a median height z-score below -2. Twelve patients had a median weight z-score below 0, and two patients (9.1%) had a median weight z-score below -2. Six patients had a median BMI z-score below 0 and no patients had a BMI z-score below -2. Median z-scores for each age group in years were calculated for ages 0–12 years, as we only had three patients who were currently older than 12 years (Fig. 4). The median height z-score was significantly smaller than 0 for patients aged 0–4 years. The median weight z-score was significantly lower than 0 for those aged 0 years. The median BMI z-score did not differ from 0 for any age group.
Impact of rare disease designation on patients with CCHS
Sixteen patients were born before and eight patients were born after CCHS was designated as a Rare Disease in Korea. There was no difference in age at clinical manifestation, but the age at genetic diagnosis was significantly earlier in patients born after the Rare Disease designation than in those born before. However, the age at tracheostomy and proportion of patients with each phenotype did not differ between groups (Table 3).
Discussion
To our knowledge, this is the first study describing the clinical characteristics and management of patients with CCHS in South Korea. Most patients presented with apnea or hypopnea during the neonatal period, and all were on home ventilators via a T-cannula or mask. Patients had various degrees of ANSD, including gastrointestinal, cardiac, and endocrine dysfunctions, with genotype–phenotype correlations. The height of patients was smaller than that of the normal population for some age groups, whereas weight did not significantly differ. Notably, this is the first study to assess the growth parameters of patients with CCHS. Additionally, with the designation of rare diseases, the genetic diagnosis of these patients has accelerated, emphasizing the need for national support.
Adequate ventilatory support is crucial throughout the lifetime of patients with CCHS [4]. Modes of ventilatory support include positive-pressure ventilation (PPV) via a tracheostomy or mask, phrenic nerve pacing, or negative-pressure ventilation. However, in Korea, phrenic nerve pacing and negative pressure are not commercially available, and all patients are on PPV. Home ventilators are supported by the National Health Insurance System; when physicians prescribe home ventilators, they are rented by home respiratory care companies for approximately $535.00 per month, and 90% to 100% depending on diagnosis and economic status is reimbursed by the government, allowing for affordable mechanical ventilation at home for all patients [12].
Regarding the ventilation interface, tracheostomy is recommended during infancy. For patients with late-onset CCHS who only require nighttime ventilation, mask ventilation is also possible [4, 13]. In our cohort, all but three patients underwent tracheostomy during infancy. In one pair of identical twins, one underwent tracheostomy, but the parents refused tracheostomy for the other twin, even after a diligent explanation of the possible outcomes by the medical staff. In one of the twins receiving mask ventilation, parents had trouble with ventilator compliance during sleep due to child resistance, resulting in frequent desaturation at sleep onset. Currently, a child on a mask ventilator is diagnosed with ASD, while the other twin with a tracheostomy has a mild language developmental delay. It cannot be inferred whether the ventilation interface was the cause of the different neurological outcomes in this pair of twins; however, inadequate ventilation has been associated with adverse neurocognitive outcomes [14]. Decannulation in school-aged children has been reported to be successful, and an algorithm for decannulation has been suggested [15, 16].
Since PHOX2B is a transcription factor responsible for neural development during early embryogenesis, alterations in the PHOX2B gene result in various ANSDs [5]. When the differentiation of enteric neurons is affected, gastrointestinal manifestations, ranging from constipation to HD, may occur. While the HD rate in CCHS is reported to be approximately 20–31%, [17, 18] 50% of patients were diagnosed with HD in our cohort. Cardiovascular manifestations of CCHS, including transient asystole, sinus bradycardia, and blood pressure abnormalities, can present as frequent syncope and life-threatening sinus pauses, which can lead to many fatal events that eventually require cardiac pacemaker placement [19, 20]. Guidelines recommend yearly screening for arrhythmia with 48 to 72-h Holter monitoring in patients with CCHS [4, 13]. In patients with syncope without sinus pause from Holter monitoring, an implantable loop recorder may be inserted [21]. In our cohort, arrhythmia was present in 37.5% of patients, and 8.3% had sinus pauses. Patients did not have a cardiac pacemaker inserted, but data on the frequency of sinus pauses were collected using implantable loop recorders.
Other manifestations include ocular disorders and neural crest-derived tumors. The most common diseases related to ocular disorders are pupillary abnormalities, convergence insufficiency, strabismus, or ptosis [4]. The prevalence of ocular disorders (29.2%) was lower than reported (46–92%), [22, 23] which may be due to missed ophthalmological screening. Neural crest-derived tumors may occur in 3–5% of patients [4]. Neuroblastomas, ganglioblastomas, and ganglioneuromas are mostly found in PARMs with higher numbers of GCN repeats and NPARMs [24].
Owing to the potential for repeated hypoxic brain damage, neurocognitive functioning is often impaired. Comprehensive neuropsychological assessment is recommended for patients with CCHS to improve their quality of life [8]. In our cohort, almost all patients had some form of developmental delay. However, many patients who were born before 2017, when the diagnosis of CCHS was classified as a rare disease in Korea, did not undergo neurocognitive tests before school age, and most of the older patients' neurocognitive development evaluation had been recently conducted or they were already undergoing treatment after being diagnosed with developmental delay. Younger patients with tracheostomy cannulas inevitably have expressive language delays, which can be resolved once they learn to speak with the tracheostomy. Further testing is needed when children born after the rare disease designation reach school age. Whether neurocognitive impairment or delay is a result of CCHS neuronal development itself or inadequate ventilation is controversial [7, 25]. Ventilation and neurocognitive screening should be provided to minimize potential hypoxic damage.
In the study group, most patients were within the normal range of birth weight; however, at preschool age, their height was below the average height of their peer group. The relationship between mutations in the PHOX2B gene and growth impairment is still unknown. However, some studies have reported that growth retardation may be related to ventilator-assisted respiratory failure or hypoxic brain damage. One study found that intermittent hypoxia in rats could impair GH/IGF-1 signaling during the first few weeks of life and might contribute to long-term organ and body growth impairments [26]. We can hypothesize that early hypoxic damage in patients may affect the endocrine system related to growth hormone signaling, resulting in growth retardation.
Since CCHS was classified as a rare disease in Korea in June 2017, patients have been able to receive medical expense and other social welfare benefits. Therefore, patients born after the rare disease designation underwent multidisciplinary follow-up as recommended, but those born before were not able to undergo all recommended screenings. Although genetic diagnosis was accelerated in those born after this classification, there was no significant difference in the prevalence of most phenotypes. We speculate that younger children with milder symptoms were more thoroughly screened after the rare disease designation. However, further studies comparing the two groups are needed when patients born after the classification reach school age.
This study has some limitations. First, this was a single-center study, so not all Korean patients with CCHS were included, but as we are the largest national children’s hospital, this is as close as possible to a nationwide cohort. Second, due to the wide age range and rare disease designation of CCHS, multidisciplinary management for related ANSDs has not been performed thoroughly for older patients. This emphasizes the need for a solid social welfare system for patients with multidisciplinary disorders.
In conclusion, CCHS is a rare disorder with an autosomal dominant mutation in PHOX2B, which is characterized by central hypoventilation and accompanied by other diseases related to ANSD. The patients exhibited a spectrum of clinical features, including respiratory, cardiac, endocrine, and other autonomic nervous system-innervated systems. Since all clinical characteristics of CCHS are often not present at birth or upon initial diagnosis and appear in various phenotypes, the management of patients with CCHS requires multidisciplinary care and regular follow-up to ensure optimal outcomes.
Data availability
The datasets generated and/or analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ANSD:
-
Autonomic nervous system dysregulation
- ASD:
-
Autism spectrum disorder
- BMI:
-
Body mass index
- CCHS:
-
Congenital central hypoventilation syndrome
- HD:
-
Hirschsprung disease
- NPARM:
-
Non-polyalanine repeat mutations
- PARM:
-
Polyalanine repeat mutation
- PHOX2B:
-
Paired-like homeobox 2B
- VUS:
-
Variants of uncertain significance
References
Trang H, Girard A, Laude D, Elghozi JL (2005) Short-term blood pressure and heart rate variability in congenital central hypoventilation syndrome (Ondine’s curse). Clin Sci (Lond) 108(3):225–230. https://doi.org/10.1042/CS20040282
Shimokaze T, Sasaki A, Meguro T, Hasegawa H, Hiraku Y, Yoshikawa T et al (2015) Genotype-phenotype relationship in Japanese patients with congenital central hypoventilation syndrome. J Hum Genet 60(9):473–477. https://doi.org/10.1038/jhg.2015.65. Epub 2015 Jun 11
Korea Disease Control and Prevention Agency (KDCA). Annual report on the rare disease patients in Korea 2019–2021. https://helpline.kdca.go.kr/cdchelp/ph/ptlcontents/selectPtlConSent.do?schSno=145&menu=C0400. Accessed 30 Nov 2023. In Korean
Trang H, Samuels M, Ceccherini I, Frerick M, Garcia-Teresa MA, Peters J et al (2020) Guidelines for diagnosis and management of congenital central hypoventilation syndrome. Orphanet J Rare Dis 15(1):252. https://doi.org/10.1186/s13023-020-01460-2
Bachetti T, Ceccherini I (2020) Causative and common PHOX2B variants define a broad phenotypic spectrum. Clin Genet 97(1):103–113. https://doi.org/10.1111/cge.13633. Epub 2019 Aug 30
Di Lascio S, Benfante R, Di Zanni E, Cardani S, Adamo A, Fornasari D et al (2018) Structural and functional differences in PHOX2B frameshift mutations underlie isolated or syndromic congenital central hypoventilation syndrome. Hum Mutat 39(2):219–236. https://doi.org/10.1002/humu.23365. Epub 2017 Nov 21
Ogata T, Muramatsu K, Miyana K, Ozawa H, Iwasaki M, Arakawa H (2020) Neurodevelopmental outcome and respiratory management of congenital central hypoventilation syndrome: a retrospective study. BMC Pediatr 20(1):342. https://doi.org/10.1186/s12887-020-02239-x
Macdonald KT, Mosquera RA, Yadav A, Caldas-Vasquez MC, Emanuel H, Rennie K (2020) Neurocognitive functioning in individuals with congenital central hypoventilation syndrome. BMC Pediatr 20(1):194. https://doi.org/10.1186/s12887-020-2006-5
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30. Epub 2015 Mar 5
Korea Disease Control and Prevention Agency (KDCA). Korean Reference Genome DB: PHOX2B. http://coda.nih.go.kr/coda/KRGDB/index. Accessed 8 Nov 2020
Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ et al (2018) The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr 61(5):135–149. https://doi.org/10.3345/kjp.2018.61.5.135. Epub 2018 May 28
Kim HI, Cho JH, Park SY, Lee YS, Chang Y, Choi WI et al (2019) Home mechanical ventilation use in south korea based on national health insurance service data. Respir Care 64(5):528–535. https://doi.org/10.4187/respcare.06310. Epub 2018 Dec 24
Weese-Mayer DE, Berry-Kravis EM, Ceccherini I, Keen TG, Loghmanee DA, Trang H (2010) An official ATS clinical policy statement: congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am J Respir Crit Care Med 181(6):626–644. https://doi.org/10.1164/rccm.200807-1069ST
Watson RS, Beers SR, Asaro LA, Burns C, Koh MJ, Perry MA et al (2022) Association of Acute Respiratory Failure in Early Childhood With Long-term Neurocognitive Outcomes. JAMA 327(9):836–845. https://doi.org/10.1001/jama.2022.1480
Canning J, Mills N, Mahadevan M (2020) Pediatric tracheostomy decannulation: When can decannulation be performed safely outside of the intensive care setting? A 10 year review from a single tertiary otolaryngology service. Int J Pediatr Otorhinolaryngol 133:109986. https://doi.org/10.1016/j.ijporl.2020.109986. Epub 2020 Mar 8
Paglietti MG, Porcaro F, Sovtic A, Cherchi C, Verrillo E, Pavone M et al (2019) Decannulation in children affected by congenital central hypoventilation syndrome: A proposal of an algorithm from two European centers. Pediatr Pulmonol 54(11):1663–1669. https://doi.org/10.1002/ppul.24448. Epub 2019 Jul 16
Balakrishnan K, Perez IA, Keens TG, Sicolo A, Punati J, Danialifar T (2021) Hirschsprung disease and other gastrointestinal motility disorders in patients with CCHS. Eur J Pediatr 180(2):469–473. https://doi.org/10.1007/s00431-020-03848-5. Epub 2020 Oct 28
Berry-Kravis EM, Zhou L, Rand CM, Weese-Mayer DE (2006) Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am J Respir Crit Care Med 174(10):1139–1144. https://doi.org/10.1164/rccm.200602-305OC. Epub 2006 Aug 3
Dudoignon B, Denjoy I, Patout M, Matrot B, Gallego J, Bokov P et al (2023) Heart rate variability in congenital central hypoventilation syndrome : relationships with hypertension and sinus pauses. Pediatr Res 93(4):1003–1009. https://doi.org/10.1038/s41390-022-02215-4. Epub 2022 Jul 26
Laifman E, Keens TG, Bar-Cohen Y, Perez IA (2020) Life-threatening cardiac arrhythmias in congenital central hypoventilation syndrome. Eur J Pediatr 179(5):821–825. https://doi.org/10.1007/s00431-019-03568-5. Epub 2020 Jan 16
Mitacchione G, Bontempi L, Curnis A (2019) Clinical approach to cardiac pauses in congenital central hypoventilation syndrome. Pediatr Pulmonol 54(2):E4–E6. https://doi.org/10.1002/ppul.24189. Epub 2018 Nov 20
Patwari PP, Stewart TM, Rand CM, Rand CM, Carroll MS, Kuntz NL et al (2012) Pupillometry in congenital central hypoventilation syndrome (CCHS): quantitative evidence of autonomic nervous system dysregulation. Pediatr Res 71(3):280–285. https://doi.org/10.1038/pr.2011.38. Epub 2012 Jan 25
Goldberg DS, Ludwig IH (1996) Congenital central hypoventilation syndrome: ocular findings in 37 children. J Pediatr Ophthalmol Strabismus 33(3):175–80. https://doi.org/10.3928/0191-3913-19960501-11
Heide S, Masliah-Planchon J, Isidor B, Guimier A, Bodet D, Coze C et al (2016) Oncologic phenotype of peripheral Neuroblastic tumors associated with PHOX2B non-Polyalanine repeat expansion mutations. Pediatr Blood Cancer 63:71–77. https://doi.org/10.1002/pbc.25723. Epub 2015 Sep 16
Trang H, Bourgeois P, Cheliout-Heraut F (2020) Neurocognition in Congenital Central Hypoventilation Syndrome: influence of genotype and ventilation method. Orphanet J Rare Dis 15:322. https://doi.org/10.1186/s13023-020-01601-7
Cai C, Ahmad T, Valencia GB, Aranda JV, Xu J, Beharry KD (2018) Intermittent hypoxia suppression of growth hormone and insulin-like growth factor-I in the neonatal rat liver. Growth Horm IGF Res 41:54–63. https://doi.org/10.1016/j.ghir.2018.03.001. Epub 2018 Mar 8
Acknowledgements
We would like to thank the parents of CCHS patients in SNUCH for cooperations and Lee Kun-hee Child Cancer & Rare Disease Project in Republic of Korea for their financial support.
Funding
Open Access funding enabled and organized by Seoul National University Hospital. This study was supported and funded by the SNUH Lee Kun-hee Child Cancer & Rare Disease Project, Republic of Korea (Grant number 22C-015-0000).
Author information
Authors and Affiliations
Contributions
Min Jeong Lee performed the validation, investigation, formal analysis, and the writing of the original manuscript. Ji Soo Park contributed to the conceptualization, methodology, investigation, validation, and revision of the manuscript. Dong In Seo drafted the article and critically revised it for important intellectual content. Kyunghoon Kim, Jung Min Ko, and June Dong Park contributed to data curation and manuscript review. All authors have approved the final manuscript as submitted and agreed to be accountable for all aspects of this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, M.J., Park, J.S., Kim, K. et al. Congenital central hypoventilation syndrome in korea: 20 years of clinical observation and evaluation of the ventilation strategy in a single center. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05611-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00431-024-05611-6