Abstract
To quantify the tracking of apolipoprotein B (apoB) levels from childhood and adolescence and compare the tracking of apoB with low-density lipoprotein (LDL) cholesterol, a systematic search of MEDLINE, Embase, Web of Science, and Google Scholar was performed in October 2023 (PROSPERO protocol: CRD42022298663). Cohort studies that measured tracking of apoB from childhood/adolescence (< 19 years) with a minimum follow-up of 1 year, using tracking estimates such as correlation coefficients or tracking coefficients, were eligible. Pooled correlations were estimated using random-effects meta-analysis. Risk of bias was assessed with a review-specific tool. Ten studies of eight unique cohorts involving 4677 participants met the inclusion criteria. Tracking of apoB was observed (pooled r = 0.63; 95% confidence interval [CI] = 0.53–0.71; I2 = 96%) with no significant sources of heterogeneity identified. Data from five cohorts with tracking data for both lipids showed the degree of tracking was similar for apoB (pooled r = 0.59; 95% CI = 0.55–0.63) and LDL cholesterol (pooled r = 0.58; 95% CI = 0.47–0.68). Study risk of bias was moderate, mostly due to attrition and insufficient reporting.
Conclusion: ApoB levels track strongly from childhood, but do not surpass LDL cholesterol in this regard. While there is strong evidence that apoB is more effective at predicting ASCVD risk than LDL cholesterol in adults, there is currently insufficient evidence to support its increased utility in pediatric settings. This also applies to tracking data, where more comprehensive data are required.
What is known: • Apolipoprotein B is a known cause of atherosclerotic cardiovascular disease. • Apolipoprotein B levels are not typically measured in pediatric settings, where low-density lipoprotein cholesterol remains the primary lipid screening measure. | |
What is new: • This meta-analysis of 10 studies showed apolipoprotein B levels tracked strongly from childhood but did not exceed low-density lipoprotein cholesterol in this regard. • More comprehensive tracking data are needed to provide sufficient evidence for increased utility of apolipoprotein B in pediatric settings. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concentration of cholesterol contained in lipids such as low-density lipoprotein (LDL) and non-high-density lipoprotein (non-HDL) cholesterols, in addition to the concentration of triglycerides, has a long history of association with atherosclerotic cardiovascular disease (ASCVD). As such, these lipids tend to form a cornerstone of screening and treatment for the reduction of ASCVD in adult settings [1,2,3]. Although the concentration of cholesterol and triglycerides in each of these conventional lipids and their subtypes can differ substantially, each of these circulating atherogenic lipoproteins contains a molecule of apolipoprotein B-100 (apoB) [4]. This hepatically produced protein is a key component of very-low-density lipoprotein, LDL, intermediate-density lipoprotein particles and is present in lipoprotein(a) [5]. Most evidence from large and rigorously performed studies shows that the total number of apoB-containing lipoprotein particles, not cholesterol or triglyceride concentration, is the key lipid determinant of ASCVD [6,7,8,9], shorter lifespan, and type 2 diabetes [10]. Hence, it is proposed that apoB combines information from conventional lipids into a singular index quantifying ASCVD risk [4, 11,12,13].
In the USA, population-wide screening for conventional lipid levels targeting pediatric ASCVD risk reduction is recommended at ages 9–11 years and again at 17–21 years [14]. While pediatric screening for lipid levels is controversial [15, 16], the persistence of these lipid levels (tracking) into later life partly informs the case for screening recommendations [14, 17,18,19]. Given the emerging role of apoB as the key lipid determinant in ASCVD, we performed a systematic review and meta-analysis to examine the degree to which apoB levels track from childhood and adolescence into later life and how this compares to LDL cholesterol.
Methods
The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42022298663). It was designed, conducted, and reported in alignment with systematic review best practices, including the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Statement 2020 (Online Resource Table 1), Cochrane Handbook, Embase Guide, and university library guides [20,21,22,23,24].
Eligibility criteria
Eligible studies were cohort studies that measured the degree of tracking of apoB levels from childhood or adolescence (age < 19 years) into later life (follow-up period ≥ 1 year) with a correlation coefficient or a tracking coefficient (which is comparable but not equivalent to a correlation [25]). A minimum follow-up period of 1 year was chosen because it typically coincides with recommendations for routine (yearly) clinical assessment of ASCVD risk factors such as body mass index and blood pressure in the pediatric setting [26, 27]. The full eligibility criteria are described in Table 1.
Information sources
We identified studies by searching electronic databases, reference lists, topical reviews, and authors’ personal databases. MEDLINE (via Ovid, 1946 to 13 October 2023) Embase (via Ovid, 1974 to 13 October 2023), Web of Science (Core Collection, 1945 to 16 October 2023), and Google Scholar (first 200 results on 14 January 2022 and 16 October 2023) were searched by one researcher (OS). We applied Bramer et al.’s recommended optimal combination of electronic databases [28] and designed the search strategy in consultation with University of Tasmania library staff experienced in electronic literature searching.
Search strategy
The search strategy aimed to capture cohort studies that mentioned apolipoproteins, childhood or adolescence, and tracking. Subject headings, keywords, titles, and abstracts (full text for Google Scholar) were searched. The full search strategy (terms and parameters) for each database is described in Online Resource Table 2.
Study selection
Studies from our search were imported to Covidence online software (Veritas Health Innovation, Melbourne, VIC, Australia) and de-duplicated. Two researchers (OS, ZZ) independently screened the titles and abstracts against the eligibility criteria and then the full texts for those that passed title/abstract screening, with conflicts resolved via an adjudicating vote from a third researcher (CGM). Two researchers (RF, TK) assisted with screening full texts in languages other than English (four Spanish, one Japanese).
Data extraction
Relevant data were extracted (including supplemental material if necessary) by one researcher (OS or RF). Information that was not reported (missing data) was sought in other published material about the studies. A second researcher (ZZ or OS) verified the data extracted from each study. Discrepancies were reviewed by three researchers (OS, ZZ, CGM) and corrections were made if necessary. Extracted data were recorded and stored in Covidence.
Data items and effect measures
The following information was extracted about each study: study name, study design, and country where data were collected. The following information was extracted about each eligible tracking estimate: type of apolipoprotein/lipid, effect estimate, tracking effect measure, variables used for adjustment, sample size, sex, ethnicity, age at baseline, length of follow-up, fasting status at baseline and follow-up as defined by the authors, number of serum measurements used to derive levels at baseline and follow-up, and measurement methods.
Risk of bias assessment
A modified version of the Newcastle–Ottawa Scale for assessing the quality of cohort studies was used to assess the risk of bias of the studies (Online Resource Methods 1) [29]. Two researchers (OS, ZZ) independently assessed the risk of bias of the studies, with another researcher (RF) assisting with the assessments of materials in languages other than English. Discrepancies were reviewed and resolved by three researchers (OS, ZZ, CGM).
Synthesis methods
Descriptive statistics were used to summarize and compare the characteristics of the included studies and cohorts. Discrete variables were summarized as counts (percentages) and continuous variables as mean (standard deviation [SD], range). We used the DerSimonian-Laird random-effects meta-analysis to estimate the tracking of apoB from childhood and adolescence, quantified as pooled correlation or tracking coefficients, weighted by the standard error of the effect estimate. Stratified random-effects meta-analysis compared the tracking of apoB and LDL cholesterol levels among studies with data available on both. Estimates were Z-transformed for meta-analysis and back-transformed for interpretation. Each cohort contributed up to one observation per meta-analysis; if an overall effect estimate for the cohort was not reported, the weighted mean among the applicable subgroup estimates was used. Forest plots visualized cohort-level and pooled effect estimates and their 95% confidence intervals (CIs). Statistical (between-cohort) heterogeneity was quantified by the I2 statistic and interpreted according to the Cochrane Handbook [30]. Potential sources of heterogeneity (sex, length of follow-up, age at baseline, sex, and age at baseline strata) were examined by exploratory stratified random-effects meta-analysis. Analyses were performed with Stata version 17 (StataCorp, College Station, TX, USA). Statistical significance level was set at p < 0.05.
Reporting bias assessment
Publication bias was visually examined by funnel plots, and the pooled coefficient including potentially missing studies was estimated with nonparametric restricted maximum likelihood trim-and-fill analysis.
Certainty of evidence assessment
We used the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach, a widely endorsed method for grading the quality of evidence and the strength of recommendations, to assess the certainty of the evidence [31, 32].
Results
Study selection
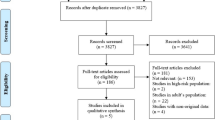
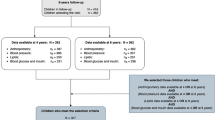
The flow of studies through each phase of selection and screening is shown in Fig. 1. After removal of 1489 duplicates, 2757 unique studies were screened for eligibility, 2723 of these were excluded during title and abstract screening, and the full texts of the remaining 34 studies were assessed. Another 24 studies were ineligible during full-text screening; the most frequent reasons for exclusion were did not use required effect measures (n = 8) and did not measure serum/plasma apoB levels (n = 7). Ten studies were included [33,34,35,36,37,38,39,40,41,42].
Phases of study selection. Databases searched: 16 October 2023; figure adapted from the PRISMA statement [20]; apoB: apolipoprotein B
Study characteristics
This review extracted apoB and LDL cholesterol tracking estimates from 10 studies of eight unique cohorts of 40 to 1758 participants (totaling 4677 unique participants). The studies and cohorts are summarized in Table 2 and extracted estimates are described in Online Resource Table 3. Data was collected in Europe and the USA between 1974 and 2020. Most studies reported multiple eligible tracking estimates because analyses were often stratified by subgroups (e.g., sex, age at baseline, length of follow-up, timepoint pairs). The results of six cohorts were stratified by sex [33, 34, 36, 38,39,40]. Age at baseline ranged from 0.0 to 16.0 years and length of follow-up ranged from 1.0 to 7.4 years, and tracking to adulthood (age ≥ 19 years at follow-up) was assessed in two cohorts [33, 39]. One study reported estimates adjusted for age, height, and ponderal index [33]. The adjusted estimates were pooled with unadjusted estimates because the authors reported they were essentially the same as the unreported unadjusted estimates and excluding the adjusted estimates did not change the meta-analysis results. The number of measurements per person varied across the included studies, but no studies derived baseline levels or follow-up levels from multiple blood draws that were averaged.
Risk of bias
Risk of bias scores are summarized in Table 2. On average, the studies were assessed as having a moderate risk of bias, with a high risk of bias due to attrition, measurement, and potential conflicts of interest, and a moderate risk of bias due to sample selection and confounding. Insufficient reporting contributed to the risk of bias, with studies providing insufficient detail for 39% of the risk of bias items (60% for representativeness of sample, 55% for adequacy of follow-up, 55% for lipid measurement protocols, 30% for number of measurements at timepoints, 10% for fasting status, 18% for confounding, 70% for conflicts of interest).
Results of syntheses
Collectively, there was a positive correlation for tracking of apoB levels (r = 0.63, 95% CI = 0.53, 0.71; Fig. 2). An estimated 40% (r2) of variation in later-life apoB levels was explained by variation in childhood/adolescence apoB levels. There was considerable heterogeneity between cohorts (Fig. 2). In exploratory subgroup analyses (not tabulated), neither sex, length of follow-up, age at baseline, nor sex and age at baseline stratification (pre-pubertal males, pre-pubertal females, peri-pubertal males, peri-pubertal females) explained the observed heterogeneity.
Random-effects meta-analysis of tracking of apoB from childhood/adolescence to at least 1 year later in life. Effect estimates (r) pooled across cohorts using DerSimonian-Laird random-effects model; I2 = 96% (95% CI = 62%, 99%); weight (%) indicated above effect estimates; 95% confidence interval (CI) represented by capped lines; apoB: apolipoprotein B
Meta-analysis of tracking of apoB to adulthood was not possible due to an insufficient number of cohorts (n = 2). Correlation coefficients ranged from 0.20 to 0.69 (cohort mean r = 0.45 and 0.69 for the cohorts) for tracking from late adolescence (14–18 years) to early adulthood (19–22 years) [33, 39].
No difference in the degree of tracking of apoB and LDL cholesterol was found across the five cohorts that reported the tracking of both lipids (Fig. 3).
Stratified random-effects meta-analysis of tracking of apoB and LDL cholesterol from childhood/adolescence to at least 1 year later in life. Effect estimates (r) pooled across cohorts using DerSimonian-Laird random-effects model; apoB subgroup I2 = 38%; LDL cholesterol subgroup I2 = 92%; weight (%) indicated above effect estimate; 95% confidence interval (CI) represented by capped lines; apoB: apolipoprotein B; LDL: low-density lipoprotein
Reporting biases
Despite insufficient cohorts (n < 10) to statistically quantify the presence of publication bias in the reporting of apoB tracking, there was some visual evidence of asymmetry in the funnel plot, with a deficit of small studies reporting a large effect size (Fig. 4). Imputation of two potentially missing studies increased the estimated degree of apoB tracking by 5% (pooled r = 0.66; 95% CI = 0.59, 0.72).
Funnel plot of the effect estimate (r) and standard error (ser) of tracking of apoB from childhood/adolescence to at least 1 year later in life. The circles represent the cohort-specific coefficients, the vertical line represents the pooled coefficient, and the dashed triangular region represents the boundary within which 95% of studies are expected to fall in the absence of both biases and heterogeneity; apoB: apolipoprotein B
Discussion
This meta-analysis found a single measure of apoB from childhood or adolescence tracks strongly into later life. A subanalysis showed apoB and LDL cholesterol tracked similarly. Applying the GRADE approach to the primary research question [31, 32], we are moderately confident in the effect estimates. The true tracking of apoB is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different due to risk of bias, heterogeneity, inconsistent use of cut-offs for risk classification, and absence of data on tracking to adulthood.
The included studies had moderate risk of bias, with insufficient detail on lipid measurement protocols, sample selection, and conflicts of interest, but no visual evidence of publication biases was detected. The main meta-analysis showed considerable variation between studies which was not explained by differences in the length of follow-up or the sex or age of the samples at baseline. Attrition was a common source of risk of bias, with little consideration of potential differential loss to follow-up or use of statistical approaches to account for it.
This review considered tracking of continuous lipid levels via correlation, describing how relative rankings based on a lipid level at one timepoint can predict those at a later timepoint [38, 43, 44]. It did not cover the tracking of categorical risk factor levels which examines the degree to which risk classification remains stable over time—information that is much more clinically useful [45]. The focus on tracking of continuous levels was necessary to allow meta-analysis because cut-offs used to denote high risk wary widely among studies (studies either defined high risk arbitrarily as the upper quartile or quintile of the sample distribution or used different pre-specified thresholds [33,34,35, 37,38,39,40]) which might reflect a lack of consensus cut-offs for apoB, particularly prior to the 2011 guidelines [14]. Another gap in the literature is the absence of data on the tracking of apoB from childhood to middle and late adulthood, when clinical ASCVD typically presents [46, 47]. Also, while screening guidelines recommend calculating levels from two lipid profile measurements to limit measurement error due to within-person variability [17, 48,49,50], no studies adhered to this practice. Thus, the true degree of tracking may be higher in practice where current guidelines recommend multiple measurements than estimated in this meta-analysis. There is also limited tracking data that considers sex and age, or reliable assessment of sexual maturation status, at baseline, which is needed to consider any potential influence of changes in lipid levels that occur with puberty on tracking [51, 52].
The heterogeneity analyses, risk of bias assessment, and absence of data for risk classification stability and tracking to adulthood suggest more data are needed to fully assess the case for screening based on tracking. The availability of standardized apoB methodology [53], valid estimation of apoB into adulthood from standard lipid measurements (total cholesterol, HDL cholesterol, triglycerides) [54], standardized pediatric cut-offs to denote high risk [14, 17,18,19], and the likely reduction in risk of bias that could be attained by simple reporting of key details and consideration of differential loss to follow-up mean that the more data are needed should be readily obtainable from pre-existing cohort studies.
The screening, treatment, and clinical management of pediatric lipid levels to reduce ASCVD risk have predominantly revolved around LDL cholesterol, estimated from standard lipid panel assays of total cholesterol, HDL cholesterol, and triglycerides [14, 16, 55, 56]. The extensive use of LDL cholesterol as the primary outcome in clinical trials, combined with its long-standing familiarity among physicians, grants it significant inertia in clinical practice. For any emerging marker, whether it be apoB or non-HDL cholesterol, to gain widespread clinical acceptance, it would likely need to outperform LDL cholesterol in terms of clinical benefits or have considerable practical advantages. A growing body of evidence, primarily stemming from adult populations, suggests that apoB and non-HDL cholesterol may offer superior risk prediction capabilities compared to or alongside other lipids and lipoproteins and can be measured without the need to fast [6,7,8,9, 55, 57,58,59,60,61,62]. While childhood data regarding apoB’s and non-HDL cholesterol’s utility remains limited, preliminary findings hint at their potential to bolster current and future ASCVD risk prediction [63,64,65,66,67,68], especially among those with obesity-associated dyslipidemia characterized by hypertriglyceridemia and low HDL cholesterol [69]. However, the adoption of apoB faces challenges. Notably, the adherence of pediatricians to existing guidelines in the USA where universal lipid screening in children is endorsed is disappointingly low [70, 71]. Introducing a new or additional measure with yet-to-be-defined reference values and concerns over added costs and standardization—though these have largely been addressed [72, 73]—might exacerbate the reluctance and difficulties in implementation among physicians [71, 73, 74]. These concerns may be less pertinent for non-HDL cholesterol, which can be accurately calculated from a standard lipid panel and is increasingly favored for ASCVD health and risk reduction [6,7,8,9, 14, 75, 76]. Decisive factors in the uptake of any lipid measurement(s) in pediatric care will hinge on its predictive utility and the subsequent physician education around it [71]. Although current evidence is preliminary, direct evidence with clinical outcomes might soon emerge from the International Childhood Cardiovascular Cohort (i3C) Consortium [77].
Strengths and limitations
This systematic review adheres to best practices and was developed in consultation with leading experts [20,21,22,23]. It presents the most comprehensive synthesis and only meta-analysis of apoB tracking data to date. However, cohorts contributing data to this review were from high-income countries of Estonia, Finland, Sweden, Spain, and the USA and therefore may not be generalizable to low- or middle-income countries or regions outside of Europe and North America [78].
Conclusions
ApoB levels exhibit strong tracking from childhood, though they do not surpass LDL cholesterol in this regard. Although there is a strong evidence base in adults for apoB’s enhanced ASCVD risk prediction capabilities independent of, or in addition to, LDL cholesterol, evidence for increased utility of apoB in pediatric settings is currently too few. This also applies to tracking data, where more comprehensive data are needed.
Data availability
The datasets generated and analyzed during the current study are available in the University of Tasmania Research Data Portal and Research Data Australia repository (Stanesby O, Magnussen C (2023) Data from: Dataset - Tracking of apolipoprotein B levels measured in childhood and adolescence: systematic review and meta-analysis. https://doi.org/10.25959/vrta-vt46).
Change history
31 January 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00431-024-05445-2
References
National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (2002) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Goff DC, Jr., Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Sr., Gibbons R et al (2014) 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63(25 Pt B):2935–2959
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH et al (2014) 2013 ACCAHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol63(25 Pt B):2889–2934
Sniderman AD, Thanassoulis G, Glavinovic T, Navar AM, Pencina M, Catapano A et al (2019) Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol 4(12):1287–1295
Behbodikhah J, Ahmed S, Elyasi A, Kasselman L, De Leon J, Glass A et al (2021) Apolipoprotein B and cardiovascular disease: biomarker and potential therapeutic target. Metabolites 11(10)
Sniderman AD, Williams K, Contois JH, Monroe HM, McQueen MJ, de Graaf J et al (2011) A meta-analysis of low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B as markers of cardiovascular risk. Circ Cardiovasc Qual Outcomes 4(3):337–345
Ference BA, Bhatt DL, Catapano AL, Packard CJ, Graham I, Kaptoge S et al (2019) Association of genetic variants related to combined exposure to lower low-density lipoproteins and lower systolic blood pressure with lifetime risk of cardiovascular disease. JAMA 322(14):1381–1391
Richardson TG, Sanderson E, Palmer TM, Ala-Korpela M, Ference BA, Davey Smith G et al (2020) Evaluating the relationship between circulating lipoprotein lipids and apolipoproteins with risk of coronary heart disease: a multivariable Mendelian randomisation analysis. PLoS Med 17(3):e1003062
Zuber V, Gill D, Ala-Korpela M, Langenberg C, Butterworth A, Bottolo L et al (2021) High-throughput multivariable Mendelian randomization analysis prioritizes apolipoprotein B as key lipid risk factor for coronary artery disease. Int J Epidemiol 50(3):893–901
Richardson T, Wang Q, Sanderson E, Mahajan A, McCarthy M, Frayling T et al (2021) Effects of apolipoprotein B on lifespan and risks of major diseases including type 2 diabetes: a Mendelian randomisation analysis using outcomes in first-degree relatives. Lancet Healthy Longev 2(6):e317–e326
Glavinovic T, Sniderman AD (2021) Apolipoprotein B: the Rosetta Stone of lipidology. Curr Opin Endocrinol Diabetes Obes 28(2):90–96
Visseren F, Mach F, Smulders Y, Carballo D, Koskinas K, Bäck M et al (2021) 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: developed by the task force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur Heart J 42(34):3227–3337
Sniderman A, Navar A, Thanassoulis G (2022) Apolipoprotein B vs low-density lipoprotein cholesterol and non–high-density lipoprotein cholesterol as the primary measure of apolipoprotein B lipoprotein-related risk: the debate is over. JAMA Cardiol 7(3):257–258
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart Lung and Blood Institute (2011) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. J Pediatr 128(Suppl 5):S213–S256
US Preventive Services Task Force (2007) Screening for lipid disorders in children: US Preventive Services Task Force recommendation statement. Pediatrics 120(1):e215–e219
Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, García FA et al (2016) Screening for lipid disorders in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 316(6):625–633
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart Lung and Blood Institute (2012) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: full report. U.S. Department of Health and Human Services, National Institutes of Health, and National Heart, Lung and Blood Institute, NIH Publication No. 12–7486, Bethesda, MD, United States
Hagan J, Shaw J, Duncan P (2017) Bright futures: guidelines for health supervision of infants, children, and adolescents. American Academy of Pediatrics, 4th ed. Elk Grove Village, IL, United States
Bright Futures/American Academy of Pediatrics (2021) Recommendations for preventive pediatric health care - periodicity schedule. American Academy of Pediatrics, Elk Grove Village, IL, United States
Moher D, Liberati A, Tetzlaff J, Altman D, Prisma Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Ovid Technologies (2020) Embase: excerpta medica database guide. Elsevier B.V. (Corporate Office), Amsterdam, Netherlands. Available from: https://ospguides.ovid.com/OSPguides/embase.htm. Accessed 17 May 2022
Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M et al (2021) Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Available from www.training.cochrane.org/handbook. Accessed 17 May 2022
University of Tasmania Library (2020) Systematic reviews for health subject guide. University of Tasmania, Hobart, Australia. Available from: https://utas.libguides.com/SystematicReviews. Accessed 17 May 2022
Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Twisk J, Kemper H, Mellenbergh D, van Mechelen W (1996) Factors influencing tracking of cholesterol and high-density lipoprotein: the Amsterdam Growth and Health Study. Prev Med 25(3):355–364
Flynn J, Kaelber D, Baker-Smith C, Blowey D, Carroll A, Daniels S et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140(3)
Committee on Practice Ambulatory Medicine and Bright Futures Periodicity Schedule Workgroup, Simon G, Baker C, Barden G, Brown O, Hackell J et al (2016) 2016 recommendations for preventive pediatric health care. Pediatrics 137(1)
Bramer W, Rethlefsen M, Kleijnen J, Franco O (2017) Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 6(1):1–12
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al (2000) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, Canada: Ottawa Hospital Research Institute
Deeks J, Higgins J, Altman D, on behalf of the Cochrane Statistical Methods Group (2022) Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 63 (2022). Cochrane. Available from www.training.cochrane.org/handbook. Accessed 17 May 2022
Schünemann H, Brożek J, Guyatt G, Oxman A (2013) GRADE Handbook: Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. Grading of Recommendations, Assessment, Development and Evaluation (GRADE) Working Group. Available from https://gdt.gradepro.org/app/handbook/handbook.html. Accessed 25 Jan 2023
NHMRC (2019) Guidelines for guidelines: assessing certainty of evidence. Last published 6 September 2019: National Health and Medical Research Council (NHMRC). https://nhmrc.gov.au/guidelinesforguidelines/develop/assessing-certainty-evidence
Bao W, Srinivasan S, Berenson G (1993) Tracking of serum apolipoproteins A-I and B in children and young adults: The Bogalusa Heart Study. J Clin Epidemiol 46(7):609–616
del Villar-Rubín S, Escorihuela R, Ortega-Senovilla H, de Oya M, Garcés C (2013) High tracking of apolipoprotein B levels from the prepubertal age to adolescence in Spanish children. Acta Paediatr 102(8):e374–e377
Kurvinen E, Aasvee K, Zordania R, Jauhiainen M, Sundvall J (2005) Serum lipid and apolipoprotein profiles in newborns and six-year-old children: the Tallinn Young Family Study. Scand J Clin Lab Invest 65(7):541–550
Öhlund I, Hernell O, Hörnell A, Lind T (2011) Serum lipid and apolipoprotein levels in 4-year-old children are associated with parental levels and track over time. Eur J Clin Nutr 65(4):463–469
Peláez Gómez de Salazar M, Sánchez Bayle M, González-Requejo A, Ruiz-Jarabo Quemada C, Asensio Antón J, Otero de Becerrea J (2000) Perfil lipídico en niños de Rivas-Vaciamadrid. Seguimiento de 2 años. An Esp Pediatr 52(5):443–446
Porkka K, Viikari J, Taimela S, Dahl M, Åkerblom H (1994) Tracking and predictiveness of serum lipid and lipoprotein measurements in childhood: a 12-year follow-up. The Cardiovascular Risk in Young Finns Study. Am J Epidemiol 140(12):1096–1110
Sánchez-Bayle M, Gonzalez-Requejo A, Ruiz-Jarabo C, Asensio J, Baeza J, Vila S et al (1996) Serum lipids and apolipoproteins in Spanish children and adolescents: a 5 year follow-up. Acta Paediatr 85(3):292–294
Sánchez-Bayle M, Sánchez Bernardo A, Asensio Antón J, Ruiz-Jarabo Quemada C, Baeza Mínguez J, Morales San José M (2005) Seguimiento de 5 años del perfil lipídico en los niños. Estudio Rivas-Vaciamadrid. An Esp Pediatr 63(1):34–38
Srinivasan S, Sharma C, Foster T, Berenson G (1982) Longitudinal changes of serum lipid and apoB levels in a newborn-infant cohort. Metabolism 31(2):167–171
Maidowski L, Kiess W, Baber R, Dathan-Stumpf A, Ceglarek U, Vogel M (2023) Tracking of serum lipids in healthy children on a year-to-year basis. BMC Cardiovasc Disord 23(1):386
Magnussen C, Thomson R, Cleland V, Ukoumunne O, Dwyer T, Venn A (2011) Factors affecting the stability of blood lipid and lipoprotein levels from youth to adulthood: evidence from the Childhood Determinants of Adult Health Study. Arch Pediatr Adolesc Med 165(1):68–76
Lee J, Kim H, Kang D, Suh I (2017) The 23-year tracking of blood lipids from adolescence to adulthood in Korea: the Kangwha study. Lipids Health Dis 16(1):221
Twisk J, Kemper H, Mellenbergh G, Van Mechelen W (1997) A new approach to tracking of subjects at risk for hypercholesteremia over a period of 15 years: the Amsterdam Growth and Health Study. Eur J Epidemiol 13(3):293–300
Strong J, McGill H Jr (1962) The natural history of coronary atherosclerosis. Am J Pathol 40(1):37
McGill H Jr, McMahan A, Gidding S (2008) Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study. Circulation 117(9):1216–1227
Nuotio J, Oikonen M, Magnussen C, Viikari J, Hutri-Kähönen N, Jula A et al (2015) Adult dyslipidemia prediction is improved by repeated measurements in childhood and young adulthood. The Cardiovascular Risk in Young Finns Study. Atherosclerosis 239(2):350–357
Bookstein L, Gidding S, Donovan M, Smith F (1990) Day-to-day variability of serum cholesterol, triglyceride, and high-density lipoprotein cholesterol levels. Arch Intern Med 150(8):1653–1657
Gillman M, Cupples A, Moore L, Ellison C (1992) Impact of within-person variability on identifying children with hypercholesterolemia: Framingham Children’s Study. J Pediatr 121(3):342–347
Jolliffe C, Janssen I (2006) Distribution of lipoproteins by age and gender in adolescents. Circulation 114(10):1056–1062
Eissa M, Mihalopoulos N, Holubkov R, Dai S, Labarthe D (2016) Changes in fasting lipids during puberty. J Pediatr 170:199–205
Carr S, Hooper A, Sullivan D, Burnett J (2019) Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment. Pathology 51(2):148–154
Raitakari O, Mäkinen V, McQueen M, Niemi J, Juonala M, Jauhiainen M et al (2013) Computationally estimated apolipoproteins B and A1 in predicting cardiovascular risk. Atherosclerosis 226(1):245–251
Grundy S, Stone N, Bailey A, Beam C, Birtcher K, Blumenthal R et al (2019) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139(25):e1082–e1143
Chew D, Scott I, Cullen L, French J, Briffa T, Tideman P et al (2016) National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Heart Lung Circ 25(9):895–951
Tremblay A, Morrissette H, Gagné J, Bergeron J, Gagné C, Couture P (2004) Validation of the Friedewald formula for the determination of low-density lipoprotein cholesterol compared with β-quantification in a large population. Clin Biochem 37(9):785–790
Raitakari O, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N et al (2003) Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns Study. JAMA 290(17):2277–2283
Wilkins J, Li R, Sniderman A, Chan C, Lloyd-Jones D (2016) Discordance between apolipoprotein B and LDL-cholesterol in young adults predicts coronary artery calcification: The CARDIA Study. JACC 67(2):193–201
Sniderman A, Langlois M, Cobbaert C (2021) Update on apolipoprotein B. Curr Opin Lipidol 32(4):226–230
Johannesen C, Mortensen M, Langsted A, Nordestgaard B (2021) Apolipoprotein B and non-HDL cholesterol better reflect residual risk than LDL cholesterol in statin-treated Patients. J Am Coll Cardiol 77(11):1439–1450
Su X, Cai X, Pan Y, Sun J, Jing J, Wang M et al (2022) Discordance of apolipoprotein B with low-density lipoprotein cholesterol or non-high-density lipoprotein cholesterol and coronary atherosclerosis. Eur J Prev Cardiol 29(18):2349–2358
Gidding S, Sniderman A (2014) Improving recognition of cardiovascular risk in children. J Pediatr 164(2):228–230
Perak AM, Ning H, Kit BK, de Ferranti SD, Van Horn LV, Wilkins JT et al (2019) Trends in levels of lipids and apolipoprotein B in US youths aged 6 to 19 years, 1999–2016. JAMA 321(19):1895–1905
Juonala M, Viikari J, Kähönen M, Solakivi T, Helenius H, Jula A et al (2008) Childhood levels of serum apolipoproteins B and A-I predict carotid intima-media thickness and brachial endothelial function in adulthood: the cardiovascular risk in young Finns study. J Am Coll Cardiol 52(4):293–299
Juonala M, Wu F, Sinaiko A, Woo J, Urbina E, Jacobs D et al (2020) Non-HDL cholesterol levels in childhood and carotid intima-media thickness in adulthood. Pediatrics 145(4)
Frontini M, Srinivasan S, Xu J, Tang R, Bond M, Berenson G (2008) Usefulness of childhood non-high density lipoprotein cholesterol levels versus other lipoprotein measures in predicting adult subclinical atherosclerosis: the Bogalusa Heart Study. Pediatrics 121(5):924–929
Armstrong M, Fraser B, Hartiala O, Buscot M, Juonala M, Wu F et al (2021) Association of non-high-density lipoprotein cholesterol measured in adolescence, young adulthood, and mid-adulthood with coronary artery calcification measured in mid-adulthood. JAMA Cardiol 6(6):661–668
Mietus-Snyder M, Drews K, Otvos J, Willi S, Foster G, Jago R et al (2013) Low-density lipoprotein cholesterol versus particle number in middle school children. J Pediatr 163(2):355–362
de Ferranti S, Rodday A, Parsons S, Cull W, O’Connor K, Daniels S et al (2017) Cholesterol screening and treatment practices and preferences: a survey of United States pediatricians. J Pediatr 185:99–105.e2
Pradhan S, Dodgen A, Snyder C (2021) Improving compliance with dyslipidemia screening guidelines in a single-center U.S. outpatient pediatric cardiology clinic. Pediatr Qual Saf 6(3):e401
Contois J, Langlois M, Cobbaert C, Sniderman A (2023) Standardization of apolipoprotein B, LDL-cholesterol, and non-HDL-cholesterol. J Am Heart Assoc 12(15):e030405
Garcia E, Bennett D, Connelly M, Jeyarajah E, Warf F, Shalaurova I et al (2020) The extended lipid panel assay: a clinically-deployed high-throughput nuclear magnetic resonance method for the simultaneous measurement of lipids and Apolipoprotein B. Lipids Health Dis 19(1):247
Wilson P, Jacobson T, Martin S, Jackson E, Le N, Davidson M et al (2021) Lipid measurements in the management of cardiovascular diseases: practical recommendations a scientific statement from the national lipid association writing group. J Clin Lipidol 15(5):629–648
Raja V, Aguiar C, Alsayed N, Chibber Y, ElBadawi H, Ezhov M et al (2023) Non-HDL-cholesterol in dyslipidemia: review of the state-of-the-art literature and outlook. Atherosclerosis 383:117312
Ramjee V, Sperling L, Jacobson T (2011) Non-high-density lipoprotein cholesterol versus apolipoprotein B in cardiovascular risk stratification: do the math. J Am Coll Cardiol 58(5):457–463
Jacobs D, Woo J, Sinaiko A, Daniels S, Ikonen J, Juonala M et al (2022) Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med 386(20):1877–1888
World Bank (2023) World Bank country and lending groups: country classification. The World Bank Group. Available from https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
Funding
Open Access funding provided by University of Turku (including Turku University Central Hospital). This work is supported by a National Health and Medical Research Council (NHMRC) Investigator Grant (grant number APP1176494 [to CGM]) for Dr. Costan Magnussen.
Author information
Authors and Affiliations
Contributions
OS had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: CGM, OS, PO, and GRT. Acquisition, analysis, or interpretation of data: OS, ZZ, RF, TK, CGM. Drafting of the manuscript: OS, CGM. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: OS, PO. Supervision: CGM.
Corresponding author
Ethics declarations
Ethics approval
This study is a review and meta-analysis of publicly available data. No ethical approval is required.
Competing interests
The authors declare no competing interests.
Disclaimer
The contents of the published material are solely the responsibility of the individual authors and do not reflect the views of the NHMRC.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The link for Dataset under Data Availability has been added.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stanesby, O., Zhou, Z., Fonseca, R. et al. Tracking of apolipoprotein B levels measured in childhood and adolescence: systematic review and meta-analysis. Eur J Pediatr 183, 569–580 (2024). https://doi.org/10.1007/s00431-023-05350-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05350-0