Abstract
Improved prediction of physical child abuse could aid in developing preventive measures. Parental physical disease has been tested previously as a predictor of documented physical child abuse but in broad categories and with differing results. No prior studies have tested clinically recognizable categories of parental disease in a high-powered dataset. Using Danish registries, data on children and their parents from the years 1997–2018 were used to explore several parental physical disease categories’ associations with documented physical child abuse. For each disease category, survival analysis using pseudovalues was applied. When a parent of a child was diagnosed or received medication that qualified for a category, this family and five comparison families not in this disease category were included, creating separate cohorts for each category of disease. Multiple analyses used samples drawn from 2,705,770 children. Estimates were produced for 32 categories of physical diseases. Using Bonferroni-corrected confidence intervals (CIc), ischemic heart disease showed a relative risk (RR) of 1.44 (CIc 1.13–1.84); peripheral artery occlusive disease, RR 1.39 (CIc 1.01–1.90); stroke, RR 1.19 (1.01–1.41); chronic pulmonary disease, RR 1.33 (CIc 1.18–1.51); ulcer/chronic gastritis, RR 1.27 (CIc 1.08–1.49); painful condition, 1.17 (CIc 1.00–1.37); epilepsy, RR 1.24 (CIc 1.00–1.52); and unspecific somatic symptoms, RR 1.37 (CIc 1.21–1.55). Unspecific somatic symptoms were present in 71.87% of families at some point during the study period.
Conclusion: Most parental physical disease categories did not show statistically significant associations, but some showed predictive ability. Further research is needed to explore preventive potential.
What is Known: • Few and broad categories of parental physical disease have been examined as risk factors for severe physical child abuse; no prior study has used several categories as predictors. | |
What is New: • Unspecific symptoms, ischemic heart disease, peripheral artery occlusive disease, stroke, chronic pulmonary disease, stomach ulcer/chronic gastritis, painful condition, and epilepsy all showed to be potential predictors, with unspecific symptoms being the most prevalent. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Child physical abuse has detrimental consequences across the life span and is recognized by the World Health Organization as an important target for preventive efforts [1]. A prevailing etiologic explanation of physical child abuse is family stressors overcoming supportive factors [2]. In family stress theory [3], family stress has been connected with chronic illness, both among adults and children [4]. Adult disease has been linked with perceived stress [5], and parental chronic illness has been associated with deficiencies in family cohesion and functioning and increased levels of conflict [6]. Additionally, a dose–response relationship between symptom severity and negative impact on family functioning has been indicated [6]. Parental mental health problems have been found to predict lethal child abuse [7, 8], but parental physical health has shown differing results [9,10,11]. In the only study investigating parental physical health severity, using the parental Charlson Comorbidity Index and published concurrently in this journal, our group found no association with documented physical child abuse [12]. Possibly, this result was due to few high index scores among parents, with only 1.7% scoring ≥ 2, and because heterogeneous categories of diseases were covered. Extending beyond the severe categories in the Charlson index, adult disease has been categorized, based on previous studies [5]. Despite high prevalence [13, 14], diagnoses not attributable to well-defined physical diseases were not included [5]. These diagnoses, comprising functional somatic syndromes [15], known to be associated with stress [16] and adverse life effects [17, 18], and diagnoses defined by their symptoms and not pathology, together represent unspecific somatic symptoms.
In this study, we use categories for physical disease, with the addition of unspecific somatic symptoms [19, 20], to explore the association between parental physical health problems and documented physical child abuse. As parental physical health severity did not show a causal association with the outcome, the current study is exploratory.
Methods
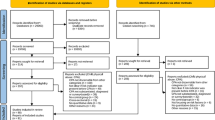
A prospective, observational cohort study was carried out. The data source used is also used in our article [12], published concurrently in this journal. All children living in Denmark between the 1st of January 1997 and the 31st of December 2018 and their legally registered parents were included, choosing this study period because among others the Fertility Database and the Medical Birth Register were available from this date. A parent was defined here as an adult registered as the current legal parent of a child, including unrelated adults in a legal parenting role. Any children without legally registered parents were excluded. Any children who emigrated and re-entered Denmark were censored at time of emigration to avoid immortality bias. Background data were drawn from other registries (see Table 1).
Exposure
See Table 2 for an overview. Parental disease was categorized mainly according to Prior et al. [5]. To ensure optimal coverage in the dataset, diagnoses not categorized by Prior et al. were added to existing categories (see below). The sorting algorithm was inspired by other studies [19, 20]. The full algorithm, and the code for data analysis, is described in the pre-registration for this study [42].
In short, all ICD 10 diagnoses were extracted from the National Patient Register; accidents, infections, and procedures were left out, and all remaining diagnoses, except psychiatric diagnoses (F-diagnoses), were sorted into conventionally defined diagnoses and unspecific symptoms. The conventionally defined diagnoses were then filtered according to Prior et al. [5] but excluding the category HIV/AIDS as our focus did not include infections. Finally, a category of “Other diagnoses” was added, comprising all diagnoses that did not fit within the well-defined disease categories or the category of unspecific symptoms, were not F-diagnoses, and were not excluded as described above. This resulted in 384 diagnosis sorting rules in addition to Prior et al., made by the first author, who is a trained medical doctor. To ease the reproducibility of this study, the final classification of 11,866 diagnostic codes is available in the Online Resource 1. For some categories, additional information on redeemed prescriptions was used, inspired by Prior et al. [5]. This captured a number of diseases treated in the primary sector. Information on redeemed prescriptions was obtained from the Register of Medicinal Products Statistics. For all disease categories, a 3-year burn-in period before the study was established. Health information for parents were read in from the first of January 1994 and onward, and, for example, parents with a code for hypertension during the period 1994–1997 were already classified in this category at study entry. All categories were updated throughout the study period on a monthly basis. To ensure precise categorization, some prescriptions used in the original categorization by Prior et al. were left out. For example, Anatomical Therapeutic Chemical (ATC) code C02, which was used by Prior et al. to categorize hypertension, is also registered for use in attention-deficit hyperactivity disorder and prostate hyperplasia. Prior et al. included this code because of its most prevalent use (A. Prior, personal communications, 2020), but we have excluded it for greater specificity.
Outcome
The outcome was documented physical child abuse. All hospital and police codes that indicated violence against a child, including lethal violence, were combined into a dichotomous variable indicating the first incidence of abuse. Details are available in our description of the coding algorithm [42].
Covariates
Covariates were chosen based on the literature (see Table 1 for references and data sources). Parental psychiatric diseases were extended from Prior’s categories to also include personality disorder [7, 50].
Statistical methods
We used pseudoobservations [51] to estimate relative risks (RR) adjusted for covariates, with 95% confidence intervals (CI) and Bonferroni-corrected 95% confidence intervals (CIc) [52, 53]. A child with at least one parent in a specific disease category was identified as exposed and the index date set at parental time of diagnosis or birth date of the child, whichever came last. Then, for each child exposed, five children who were not exposed at the index date were drawn from the underlying source population, matching on date of inclusion (a child is identified as exposed and within 3 months of calendar time, five other children not exposed are drawn), reconstituted family (living with biological parents, living with one or more unrelated adults, adopted or in foster care), child ages/birth year (matched within 1 year), number of children in the family (either one child, two children, three to five children, or six or more children), and mean parental age (within 5 years). Thus, individual cohorts were created for all disease categories studied. Each family was followed until end of study period, first incident of documented physical child abuse, emigration, the child being without registered parents, dying or reaching their 18th birthday, whichever came first, allowing for at least 1 month and at most < 18 years between exposure and outcome. Children experiencing the outcome before the exposure were excluded. Each child could participate in more than one cohort, but not twice in the same cohort, and not after first incident of documented physical child abuse. A full model, containing pre-specified variables, and a parsimonious model, reduced to avoid collinearity and small cells, were produced for all analyses. To avoid computational overload, a maximum of 100,000 exposed children were allowed in each analysis, drawn randomly among those available. Only rows with information on all variables were included. The parental disease categories were not adjusted among each other. Pseudoobservations assume that censoring in the dataset is marginally independent. As this was not the case for the calendar time groups, the dataset was stratified on this variable and pseudovalues generated within these strata. The same child could be included both as exposed and un-exposed; Eicker-Huber-White standard errors were used to compensate for this. Siblings could be included, and therefore clustering was adjusted for on a family level. In all models, death not related to abuse was treated as a competing risk. Analyses were presented with and without Bonferroni corrections, correcting for tests of 33 categories.
Results
Samples, demographics, and events
Exposed and unexposed children were drawn from 2,705,770 children available in the dataset. First-time documented physical child abuse was experienced by 70,892 children during the study period, and lethal child abuse was experienced by 111 children. Table 3 describes the full population’s distribution across covariates; this table is derived from the table included in our article [12], published concurrently in this journal. Table 4 describes the risk time, events, number of children studied, and number and percentage of children exposed in the full cohort. Most disease categories had less than 10% exposed during the study period, except unspecific symptoms (72%), allergy (23%), painful condition (11%), and other diagnoses (69%) (Table 4).
Estimates of relative risk
Table 5 describes the results for each disease category, including a specification of covariates used for each model. After Bonferroni-adjustment, we found the following disease categories to be statistically significantly associated with documented physical child abuse: ischemic heart disease, RR 1.44 (CIc 1.13–1.84); peripheral artery occlusive disease, RR 1.39 (CIc 1.01–1.90); stroke, RR 1.19 (1.01–1.41); chronic pulmonary disease, RR 1.33 (CIc 1.18–1.51); ulcer/chronic gastritis, RR 1.23 (CIc 1.00–1.51); painful condition, 1.17 (CIc 1.00–1.37); epilepsy, RR 1.27 (CIc 1.03–1.56); unspecific symptoms within the last 2 years and ever, RR 1.31 (CIc 1.14–1.50) and RR 1.33 (CIc 1.17–1.52), respectively; and other diagnoses, RR 1.23 (CIc 1.09–1.39). Diabetes mellitus and chronic liver disease showed increased risks, but these were not statistically significant after Bonferroni correction.
Discussion
In models adjusted for known risk factors for physical child abuse, the majority of disease categories explored were found to have no statistically significant association to documented physical child abuse. Ischemic heart disease, peripheral artery occlusive disease, stroke, chronic pulmonary disease, ulcer/chronic gastritis, painful condition, epilepsy, unspecific symptoms, and the broad category of “other diagnoses” showed varying degrees of associations. Diabetes mellitus and chronic liver disease showed increased risks, but results were not statistically significant after Bonferroni correction. Some findings of no association were expected based on our study on parental physical disease severity using the same dataset [12], published concurrently in this journal.
Motivating this study, we assumed that parental physical health influence family stress levels. As referenced earlier, this is indicated among parental unspecific symptoms [6] and functional somatic syndromes [16,17,18]. For many categories of disease, the specific impact on family stress levels is unknown, although there are studies on family functioning and its components. A previous study found no association between hypertension and family cohesion [54]. In diabetes, the association is influenced by treatment outcome. Among adults with non-insulin–dependent diabetes mellitus, good glycemic control was associated with lower family cohesion compared to those with lower quality glycemic regulation, while this relationship was reversed among adults with insulin-dependent diabetes mellitus [55]. Among chronic obstructive pulmonary disease patients, family functioning was found to be comparatively better among patients treated with oxygen in their home than hospitalized patients [56]. Lower family cohesion was found among individuals diagnosed with epilepsy compared to controls [57]. In a study of cancer, no differences were found in family functioning between patients and controls [58]. Headache symptom severity has been shown to adversely influence family cohesion [59]. Only cautious interpretations should be derived from single studies in each category. Nonetheless, it seems likely that disease categories’ influence on family functioning is not uniform, sometimes counterintuitive, and mediated by other factors, including treatment. Through this lens, the differing associations across categories in our results could be an expression of differences in how disease categories influence family stress.
The disease categories found to be associated with documented physical child abuse are all either chronic conditions or with considerable chronic subgroups. Consequently, part of the associations found could be an expression of the underlying chronicity of these categories. Nonetheless, a number of other disease categories representing chronic conditions show no association, possibly underlining the varying influences by different categories discussed above.
Residual confounding may also have influenced our findings. For example, adjusting for only two levels of education could result in strata with quite heterogeneous populations, and there may therefore be residual bias in the models. In addition, the model does not adjust for all possible risk factors. For example, the association with ischemic heart disease, peripheral artery occlusive disease, stroke, and chronic pulmonary disease may be affected by smoking. Smoking is a risk factor for all these conditions and has been associated with both childhood maltreatment among smokers [60] and as a risk factor for physical child abuse [29]. This is supported by the association before Bonferroni correction of diabetes mellitus, which is also associated with smoking. Thus, diseases resulting from smoking could be proxies for residual confounding from parental childhood maltreatment. Similarly, stomach ulcer/chronic gastritis is associated with substance abuse, which is also both a risk factor for [8] and a possible result of child maltreatment [61]. This is supported by the association of chronic liver disease without Bonferroni correction, also associated with substance abuse.
Epilepsy has been associated with depression and difficulties in emotional regulation [62], which may contribute to its influence on family cohesion. Affective disorders in parents have been linked to lethal physical child abuse [7, 8]. Another possible link could be that the risk of epilepsy is increased after trauma [63]. Thus, for a subgroup of parents with posttraumatic epilepsy, parental experiences of childhood maltreatment, which is a risk factor for maltreatment of offspring, could be proxied by adult epilepsy.
Chronic pain and childhood maltreatment have been previously studied, but Marin et al. in 2021 in a systematic review considered current evidence inconclusive [64]. The painful condition category in our study is based on the use of prescription analgesics at least four times within the last year. This category stands out by being defined by analgesics alone and thus possibly overlaps with other disease categories. Importantly, some diagnoses in the category unspecific symptoms describe manifestations of pain, and there might be a substantial overlap between the painful condition and unspecific symptoms categories.
Among unspecific symptoms, functional somatic syndromes have been shown to increase with childhood maltreatment [65]. This has also been shown for unspecific somatic complaints and childhood physical abuse, again invoking the possibility of residual confounding [66].
Unspecific symptoms stand out if their prevalence is taken into account. A better understanding of the individuals in the unspecific symptoms category, which encompassed 72% of the entire dataset, could potentially provide targets for preventive measures both to target populations and to inspire components for blended interventions. The current results do not warrant targeted interventions in their own right, but may inspire to future interventions such as integrating parental physical symptom checklists into existing home visiting programs or parenting programs or introducing tools to support parents in coping with their symptoms. However, further research is needed to study the associations found here and further specify their causal and/or predictive nature.
The association with the category “Other diagnoses,” diagnoses that do not fit with the remaining categories, is intriguing, but difficult to interpret due to their heterogeneous nature. Splitting this category into subcategories such as rare endocrine disorders, hereditary disorders, or similar may provide further insights.
Each disease category was not adjusted for other categories. This was inspired by our findings [12] as discussed above. Adjusting for other disease categories might consequently introduce more complexity to our models without a clear theoretical justification. Nonetheless, it is possible that some combinations, perhaps combinations of the categories found to be associated with documented physical child abuse, could have an additive or even multiplicative effect on the risk of abuse. This remains to be studied. Also, some diseases have common causes and may also be in each others’ causal pathways, for example, diabetes and heart disease [67]. This could explain the relatedness in our study of, for example, ischemic heart disease and stroke, and assumptions on the relations between categories should be remembered when designing future studies to elaborate on our results.
Strengths and weaknesses
To the best of our knowledge, this is the first study to describe a diverse set of disease categories in parents and their link to child risk of documented physical child abuse. The longitudinal nature of the data and size of the sample enable discovery of relevant candidates for further scrutiny in predictive and causal models. The categories applied have been utilized previously, and additional categorization was done based on clinical insight. The models were adjusted for a number of known risk factors, showing the relevance of the associations even after taking current knowledge into account. There are also some potential weaknesses. The categories used were not validated, although a number of diagnoses in the registries used have been validated [48]. Although the assignment of ICD 10 codes in the Danish healthcare system is done by trained health professionals, the rate of irregularities for many diagnoses is not known. Such misclassification would be expected to be independent of the outcome and hence would bias toward no association. As mentioned above, the model may contain residual bias, from unobserved or insufficiently observed variables. This is because it is based on registry data; for example, substance abuse is based on hospital diagnoses only. Thus, as argued above, the associations seen could be hypothesized to be based on residual confounding. On the contrary, this is useful in its own right for predictions. If, for example, stomach ulcer/chronic gastritis captures a part of substance abuse that is not otherwise visible through either registries or clinical observation, this category is useful for predictive modeling. Additional categorizations of diagnoses were only done by the first author. Although the categorizations were checked rigorously and backed up by clinical experience, a lack of validation might lead to unexpected associations. As noted for Table 5, the category hearing problems has an unexplained behavior in the time trend of number of diagnoses. Consequently, results from this category should be interpreted with special caution. Number of missing entries at entry in source population on neighborhood resources and reconstituted family were 20% and 23%, respectively. All cohorts were drawn using only complete cases, and there is a risk of bias if the risk of missing data is associated with differences in the underlying population, possibly affecting generalizability of the results. We used data sets drawn from all children living in Denmark up until 2018 in this study, and in some categories, we used all available children exposed to a parental disease category (for details, see Table 4). Nonetheless, a population correction factor was not used to correct the confidence intervals presented. This was because we regarded our population as a sub-population of all children living in settings with universal healthcare and because no analyses used data on all available non-exposed children. Also, some disease categories may represent a subset of families with parents in these categories, both because a maximum of 100,000 exposed families were allowed in each analysis and because some disease categories, for example, hypertension, may be underdiagnosed in patient registries not including the primary sector. Consequently, our analyses never represented the full population of interest. If the population of interest was limited to Danish children only and the variation in remaining non-exposed children assumed to be negligible, categories expected to be fully diagnosed within the registries available to us could be presented with more precise confidence intervals. However, as we find the estimated strength of associations presented as insignificant in our analyses to be moderate or less (see relative risks in Table 5), the usefulness of such categories for preventive and predictive purposes would be expected to be limited. Finally, as mentioned above, this study took place in a high-income country [68] with universal healthcare coverage. Results are likely to generalize to similar populations but would require replication elsewhere, in particular in low-income countries and healthcare systems that are organized differently. Additionally, most self-reported cases of maltreatment are not known to the sources used for the outcome [69]. Consequently, results may not generalize to the cases of physical child abuse unknown to healthcare or law enforcement.
Conclusion
A number of diverse disease categories were exploratively tested for an association with documented physical child abuse. A notable candidate for future studies was unspecific symptoms, presenting both a significant prevalence and an association with the outcome. Further candidates were ischemic heart disease, peripheral artery occlusive disease, stroke, chronic pulmonary disease, stomach ulcer/chronic gastritis, painful condition, and epilepsy. Further research into these is warranted and may inspire additions to preventive interventions.
Data availability
Access to data was granted by Statistics Denmark, and this study was exempt from ethics approval according to Danish law, as it only used administrative data. Data could not be made available due to legal requirements by Statistics Denmark. All code used, and additional resources, is available at https://osf.io/fh2sr.
Abbreviations
- ATC:
-
Anatomical Therapeutic Chemical
- CI:
-
95% Confidence interval
- CIc:
-
Bonferroni-corrected 95% confidence interval
- ICD 8:
-
International Classification of Diseases, 8th edition
- ICD 10:
-
International Classification of Diseases, 10th edition
- ISCED:
-
International Standard Classification of Education
- N:
-
Number of units
- RR:
-
Relative risk
- SD:
-
Standard deviation
References
Sethi D, Yon Y, Parekh N et al (2018) European status report on preventing child maltreatment. World Health Organization, Regional Office for Europe
Belsky J (1993) Etiology of child maltreatment: a developmental-ecological analysis. Psychol Bull 114:413–434. https://doi.org/10.1037/0033-2909.114.3.413
Hill R (1958) 1. Generic features of families under stress. Soc Casework 39:139–150. https://doi.org/10.1177/1044389458039002-318
Patterson JM, Garwick AW (1994) Levels of meaning in family stress theory. Fam Process 33:287–304. https://doi.org/10.1111/j.1545-5300.1994.00287.x
Prior A, Fenger-Grøn M, Larsen KK et al (2016) The association between perceived stress and mortality among people with multimorbidity: a prospective population-based cohort study. Am J Epidemiol 184:199–210. https://doi.org/10.1093/aje/kwv324
Pedersen S, Revenson TA (2005) Parental illness, family functioning, and adolescent well-being: a family ecology framework to guide research. J Fam Psychol 19:404–419. https://doi.org/10.1037/0893-3200.19.3.404
Lysell H, Runeson B, Lichtenstein P, Långström N (2014) Risk factors for filicide and homicide: 36-year national matched cohort study. J Clin Psychiatry 75:127–132. https://doi.org/10.4088/JCP.13m08372
Laursen TM, Munk-Olsen T, Mortensen PB et al (2011) Filicide in offspring of parents with severe psychiatric disorders: a population-based cohort study of child homicide. J Clin Psychiatry 72:698–703
Chang C-C, Hsieh M-H, Chiou J-Y et al (2021) Multiple factors associated with child abuse perpetration: a nationwide population-based retrospective study. J Interpers Violence 36:5360–5382. https://doi.org/10.1177/0886260518805100
Brown J, Cohen P, Johnson JG, Salzinger S (1998) A longitudinal analysis of risk factors for child maltreatment: findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse Negl 22:1065–1078. https://doi.org/10.1016/S0145-2134(98)00087-8
Meinck F, Cluver LD, Boyes ME (2015) Household illness, poverty and physical and emotional child abuse victimisation: findings from South Africa’s first prospective cohort study. BMC Public Health 15:444. https://doi.org/10.1186/s12889-015-1792-4
Græsholt-Knudsen T, Rask CU, Lucas S et al (2023) Parental physical disease severity and severe documented physical child abuse. Eur J Pediatr. https://doi.org/10.1007/s00431-023-05291-8
Petersen MW, Schröder A, Jørgensen T et al (2020) Irritable bowel, chronic widespread pain, chronic fatigue and related syndromes are prevalent and highly overlapping in the general population: DanFunD. Sci Rep 10:3273. https://doi.org/10.1038/s41598-020-60318-6
Haller H, Cramer H, Lauche R, Dobos G (2015) Somatoform disorders and medically unexplained symptoms in primary care. Dtsch Arztebl Int. https://doi.org/10.3238/arztebl.2015.0279
Burton C, Fink P, Henningsen P et al (2020) Functional somatic disorders: discussion paper for a new common classification for research and clinical use. BMC Med 18:34. https://doi.org/10.1186/s12916-020-1505-4
Fischer S, Lemmer G, Gollwitzer M, Nater UM (2014) Stress and resilience in functional somatic syndromes – a structural equation modeling approach. PLoS ONE 9:e111214. https://doi.org/10.1371/journal.pone.0111214
Goodoory VC, Ng CE, Black CJ, Ford AC (2022) Impact of Rome IV irritable bowel syndrome on work and activities of daily living. Aliment Pharmacol Ther 56:844–856. https://doi.org/10.1111/apt.17132
Věchetová G, Slovák M, Kemlink D et al (2018) The impact of non-motor symptoms on the health-related quality of life in patients with functional movement disorders. J Psychosom Res 115:32–37. https://doi.org/10.1016/j.jpsychores.2018.10.001
Petersen MW, Skovenborg EL, Rask CU et al (2018) Physical comorbidity in patients with multiple functional somatic syndromes. A register-based case-control study. J Psychosom Res 104:22–28. https://doi.org/10.1016/j.jpsychores.2017.11.005
Skovenborg EL, Schröder A (2014) Is physical disease missed in patients with medically unexplained symptoms? A long-term follow-up of 120 patients diagnosed with bodily distress syndrome. Gen Hosp Psychiatry 36:38–45. https://doi.org/10.1016/j.genhosppsych.2013.09.006
Tølbøll Blenstrup L, Knudsen LB (2011) Danish registers on aspects of reproduction. Scand J Public Health 39:79–82. https://doi.org/10.1177/1403494811399957
Bliddal M, Broe A, Pottegård A et al (2018) The Danish Medical Birth Register. Eur J Epidemiol 33:27–36. https://doi.org/10.1007/s10654-018-0356-1
Baadsgaard M, Quitzau J (2011) Danish registers on personal income and transfer payments. Scand J Public Health 39:103–105. https://doi.org/10.1177/1403494811405098
Cheung C-k, Leung K-k (2011) Neighborhood homogeneity and cohesion in sustainable community development. Habitat Int 35:564–572. https://doi.org/10.1016/j.habitatint.2011.03.004
Pedersen CB, Antonsen S, Timmermann A et al (2022) Urban-rural differences in schizophrenia risk: multilevel survival analyses of individual- and neighborhood-level indicators, urbanicity and population density in a Danish National Cohort Study. Schizophr Bull Open 3:sgab056. https://doi.org/10.1093/schizbullopen/sgab056
Statistics Denmark. SDG Indikator: 1.2.1 - Fattigdomsindikatorer. https://www.dst.dk/da/Statistik/Sdg/01-afskaf-fattigdom/delmaal-02/indikator-1. Accessed 11 Apr 2020
Greenland S, Pearce N (2015) Statistical foundations for model-based adjustments. Annu Rev Public Health 36:89–108. https://doi.org/10.1146/annurev-publhealth-031914-122559
Keenan HT (2003) A population-based study of inflicted traumatic brain injury in young children. JAMA 290:621. https://doi.org/10.1001/jama.290.5.621
Gessner BD, Moore M, Hamilton B, Muth PT (2004) The incidence of infant physical abuse in Alaska. Child Abuse Negl 28:9–23. https://doi.org/10.1016/j.chiabu.2003.03.002
Zuravin SJ (1988) Fertility patterns: their relationship to child physical abuse and child neglect. J Marriage Fam 50:983–993. https://doi.org/10.2307/352109
Helweg-Larsen K, Larsen HB (2005) A critical review of available data on sexual abuse of children in Denmark. Child Abuse Negl 29:715–724. https://doi.org/10.1016/j.chiabu.2004.11.005
Widom CS, Czaja SJ, DuMont KA (2015) Intergenerational transmission of child abuse and neglect: real or detection bias? Science 347:1480–1485. https://doi.org/10.1126/science.1259917
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39:22–25. https://doi.org/10.1177/1403494810387965
Norredam M, Kastrup M, Helweg-Larsen K (2011) Register-based studies on migration, ethnicity, and health. Scand J Public Health 39:201–205. https://doi.org/10.1177/1403494810396561
Mersky JP, Berger LM, Reynolds AJ, Gromoske AN (2009) Risk factors for child and adolescent maltreatment: a longitudinal investigation of a cohort of inner-city youth. Child Maltreat 14:73–88. https://doi.org/10.1177/1077559508318399
Brenner RA, Overpeck MD, DrPh, et al (1999) Deaths attributable to injuries in infants, United States, 1983–1991. Pediatrics 103:968–974. https://doi.org/10.1542/peds.103.5.968
Freisthler B, Maguire-Jack K (2015) Understanding the interplay between neighborhood structural factors, social processes, and alcohol outlets on child physical abuse. Child Maltreat 20:268–277. https://doi.org/10.1177/1077559515598000
Schnitzer PG, Ewigman BG (2005) Child deaths resulting from inflicted injuries: household risk factors and perpetrator characteristics. Pediatrics 116(5):e687–e693
Jensen VM, Rasmussen AW (2011) Danish education registers. Scand J Public Health 39:91–94. https://doi.org/10.1177/1403494810394715
Paxson C, Waldfogel J (2002) Work, welfare, and child maltreatment. J Labor Econ 20:435–474. https://doi.org/10.1086/339609
McGuigan WM, Pratt CC (2001) The predictive impact of domestic violence on three types of child maltreatment. Child Abuse Negl 25:869–883. https://doi.org/10.1016/S0145-2134(01)00244-7
Græsholt-Knudsen T, Obel C, Rask C, Lucas S (2021) Is parental illness a risk indicator of future physical child abuse? https://doi.org/10.17605/OSF.IO/FH2SR
Jobe-Shields L, Moreland AD, Hanson RF et al (2018) Co-occurrence of witnessed parental violence and child physical abuse from a national sample of adolescents. J Child Adolesc Trauma 11:129–139. https://doi.org/10.1007/s40653-015-0057-9
Chaffin M, Kelleher K, Hollenberg J (1996) Onset of physical abuse and neglect: psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse Negl 20:191–203. https://doi.org/10.1016/S0145-2134(95)00144-1
Doidge JC, Higgins DJ, Delfabbro P, Segal L (2017) Risk factors for child maltreatment in an Australian population-based birth cohort. Child Abuse Negl 64:47–60. https://doi.org/10.1016/j.chiabu.2016.12.002
Wasserman DR, Leventhal JM (1993) Maltreatment of children born to cocaine-dependent mothers. Am J Dis Child 147:1324–1328. https://doi.org/10.1001/archpedi.1993.02160360066021
Ahacic K, Kennison RF, Kåreholt I (2014) Alcohol abstinence, non-hazardous use and hazardous use a decade after alcohol-related hospitalization: registry data linked to population-based representative postal surveys. BMC Public Health 14. https://doi.org/10.1186/1471-2458-14-874
Schmidt M, Schmidt SAJ, Sandegaard JL et al (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 449. https://doi.org/10.2147/CLEP.S91125
Helweg-Larsen K (2011) The Danish Register of Causes of Death. Scand J Public Health 39:26–29. https://doi.org/10.1177/1403494811399958
Nager A, Sundquist K, Ramírez-León V, Johansson LM (2008) Obstetric complications and postpartum psychosis: a follow-up study of 1.1 million first-time mothers between 1975 and 2003 in Sweden. Acta Psychiatr Scand 117:12–19. https://doi.org/10.1111/j.1600-0447.2007.01096.x
Andersen PK, Pohar Perme M (2010) Pseudo-observations in survival analysis. Stat Methods Med Res 19:71–99. https://doi.org/10.1177/0962280209105020
Halekoh U, Højsgaard S, Yan J (2006) The R Package geepack for generalized estimating equations. J Stat Soft 15. https://doi.org/10.18637/jss.v015.i02
Team RC (2022) R: A language and environment for statistical computing
Brittain K, Taylor JY, Wu CY (2010) Family adaptability among urban African-American women with hypertension. J Nurse Pract 6:786–793. https://doi.org/10.1016/j.nurpra.2010.02.005
Konen JC, Summerson JH, Dignan MB (1993) Family function, stress, and locus of control. Relationships to glycemia in adults with diabetes mellitus. Arch Fam Med 2:393–402. https://doi.org/10.1001/archfami.2.4.393
Kanervisto M, Paavilainen E, Åstedt-Kurki P (2003) Impact of chronic obstructive pulmonary disease on family functioning. Heart Lung 32:360–367. https://doi.org/10.1016/j.hrtlng.2003.07.003
Wang Y-h, Haslam M, Yu M et al (2015) Family functioning, marital quality and social support in Chinese patients with epilepsy. Health Qual Life Outcomes 13:10. https://doi.org/10.1186/s12955-015-0208-6
Schmitt F, Santalahti P, Saarelainen S et al (2008) Cancer families with children: factors associated with family functioning—a comparative study in Finland. Psychooncology 17:363–372. https://doi.org/10.1002/pon.1241
Mikail SF, von Baeyer CL (1990) Pain, somatic focus, and emotional adjustment in children of chronic headache sufferers and controls. Soc Sci Med 31:51–59. https://doi.org/10.1016/0277-9536(90)90009-H
Spratt EG, Back SE, Yeatts SD et al (2009) Relationship between child abuse and adult smoking. Int J Psychiatry Med 39:417–426. https://doi.org/10.2190/PM.39.4.f
Scott KM, Smith DR, Ellis PM (2010) Prospectively ascertained child maltreatment and its association with DSM-IV mental disorders in young adults. Arch Gen Psychiatry 67:712–719. https://doi.org/10.1001/archgenpsychiatry.2010.71
Tombini M, Assenza G, Quintiliani L et al (2020) Depressive symptoms and difficulties in emotion regulation in adult patients with epilepsy: association with quality of life and stigma. Epilepsy Behav 107:107073. https://doi.org/10.1016/j.yebeh.2020.107073
Tubi MA, Lutkenhoff E, Blanco MB et al (2019) Early seizures and temporal lobe trauma predict post-traumatic epilepsy: a longitudinal study. Neurobiol Dis 123:115–121. https://doi.org/10.1016/j.nbd.2018.05.014
Marin TJ, Lewinson RE, Hayden JA et al (2021) A systematic review of the prospective relationship between child maltreatment and chronic pain. Children (Basel) 8:806. https://doi.org/10.3390/children8090806
Duncan R, Mulder R, Wilkinson SH, Horwood J (2019) Medically unexplained symptoms and antecedent sexual abuse: an observational study of a birth cohort. Psychosom Med 81:622–628. https://doi.org/10.1097/PSY.0000000000000726
Sansone RA, Wiederman MW, Tahir NA, Buckner VR (2009) A re-examination of childhood trauma and somatic preoccupation. Int J Psychiatry Clin Pract 13:233–237. https://doi.org/10.1080/13651500802621551
Haffner SM (2000) Coronary heart disease in patients with diabetes. N Engl J Med 342:1040–1042
The World Bank. High income | Data. https://data.worldbank.org/income-level/high-income?view=chart. Accessed 29 Jul 2022
Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LRA, van IJzendoorn MH, (2015) The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev 24:37–50. https://doi.org/10.1002/car.2353
Acknowledgements
Professor Carsten Obel in memoriam, in fond memory of his enthusiasm for this and related projects, his contribution of the necessary data infrastructure, and his many contributions and encouragements during the conceptualization of this study.
Funding
Open access funding provided by Royal Danish Library, Aarhus University Library This work was supported by a Fellowship grant by the PhD School of Health, Aarhus University, and a grant by Dagmar Marshalls Fund.
Author information
Authors and Affiliations
Contributions
Troels Græsholt-Knudsen, Charlotte Ulrikka Rask and Steven Lucas contributed to the study conception, and all authors contributed to the design. Data preparation and analysis were performed by Troels Græsholt-Knudsen, and revisions of the analysis was performed by all authors. The first draft of the manuscript was written by Troels Græsholt-Knudsen and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Græsholt-Knudsen, T., Rask, C.U., Lucas, S. et al. Exploratory assessment of parental physical disease categories as predictors of documented physical child abuse. Eur J Pediatr 183, 663–675 (2024). https://doi.org/10.1007/s00431-023-05317-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05317-1