Abstract
The relationship between iron metabolism and cardiometabolic risk factors has been scarcely studied in children, and the results are controversial. The objective of this study was to evaluate the association between iron parameters and lipid, glycemic and blood pressure alterations in the pediatric population. This was a cross-sectional study of 1954 children between 9 and 10 years of age in Madrid (Spain), participants in a longitudinal study of childhood obesity. Iron metabolism parameters, i.e., serum iron (Is), ferritin (Fs), transferrin (Tf) and transferrin saturation (STf) and lipid, glycemic and blood pressure profiles were evaluated. Odds ratios (ORs) were estimated using logistic regression models adjusted for sociodemographic characteristics, diet, physical activity, C-reactive protein and body mass index. Compared with the participants in the low Is and STf tertiles, those in the upper tertiles had a lower risk of low HDL-Chol (OR: 0.34; 95%CI: 0.17; 0.67) and OR: 0.44 (95%CI: 0.23; 0.84), respectively, and children in the upper Fs tertile had an OR of 2.07 (95%CI: 1.16; 3.68) for low HDL-Chol. Children in the highest Is and STf tertiles had a lower risk of prediabetes [OR: 0.63 (95%CI: 0.41; 0.97) and OR: 0.53 (95%CI: 0.34; 0.82)] and insulin resistance (IR) (OR: 0.37; 95%CI: 0.22; 0.64), and those in the upper Tf tertile had a higher risk of IR (OR: 1.90; 95%CI: 1.16; 3.12). An increased risk of hypertension was found only in children in the upper Fs tertile (OR: 1.46; 95%CI: 1.01; 2.13).
Conclusions: Biomarkers of iron metabolism are associated with cardiometabolic alterations in the pediatric population, with a variable direction and magnitude depending on the indicators used.
What is Known: • Iron metabolism is related to important cardiometabolic alterations such as metabolic syndrome and its components. • Association between biomarkers of iron status and cardiometabolic risk have been less explored in children. | |
What is New: • Biomarkers of iron metabolism are associated with cardiometabolic alterations in the pediatric population. • Iron parameters in the pediatric population could be of great help to detect and prevent cardiometabolic abnormalities early. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Iron is a necessary mineral for the human body and plays an important role in essential biological processes such as DNA synthesis, haemoglobin formation, and oxygen transport [1]. Iron homeostasis is maintained through complex mechanisms involved in intake, transfer and storage. Ferritin is an iron storage protein; therefore, high concentrations of serum ferritin indicate a risk of iron overload. Furthermore, ferritin is an acute phase protein that can be affected by other infectious and metabolic processes [2]. Transferrin, or transporter protein, increases when iron requirements increase, and its saturation reflects the amount of iron it is capable of fixing. When transferrin is saturated, free iron remains, which is toxic to cells [3].
Inappropriate overloads or deficiencies of this mineral can contribute to metabolic disturbances that correlate with a wide range of cardiovascular diseases and type 2 diabetes [4,5,6,7]. Iron deficiency is common in patients with heart failure and pulmonary hypertension [5, 8], and iron overload is related to an increased risk of atherosclerosis as well as the appearance of metabolic syndrome (MetS) and its components, such as dyslipidemia, increased body mass index (BMI), high blood pressure, hyperglycemia and insulin resistance [9,10,11].
However, most of the scientific evidence comes from studies carried out in the adult population; therefore, it is not clear whether these associations occur in early life and what effects changes in iron levels and cardiometabolic risk have in early life. Studies that explore this relationship in children are limited, and their results are inconclusive [12,13,14].
Cardiometabolic risk factors (CMRFs) usually appear in an aggregate way, and the coexistence of 3 or more risk factors is defined as MS [15]. For the preschool and childhood stages, there is no accepted definition of MetS because in this period, there are intrinsic variations in age and growth; therefore, it is more appropriate to analyze the components of MetS and other CMRFs independently [16].
The objective of this study was to explore the association between four iron parameters, i.e., serum iron (Is), serum ferritin (Fs), serum transferrin (Tf) and transferrin saturation (STf), and CMRFs in the child population aged 9–10 years.
Methods
Study population
The data were obtained from the Longitudinal Study of Childhood Obesity (ELOIN study), a population-based prospective longitudinal study consisting of a representative baseline cohort of the 4-year-old population of the Community of Madrid (6.8 million inhabitants); the methodology has been previously published [17]. The study consisted of a physical examination of children at 4, 6, and 9 years of age and a telephone interview with the parents, as well as the collection of a blood sample at 9 years of age.
Inclusion and exclusion criteria: For this cross-sectional study, 1954 participants aged 9–10 years old (born in 2008–2009) and who had a physical examination a blood sample and parent interview were included. On the other hand, 1030 children who had physical examination but not blood sample data were excluded and 8 children who had blood sample but not physical examination data were also excluded.
Blood pressure and anthropometric measurements
Physical examinations were performed by pediatricians and nurses from the Sentinel Network of the 31 primary care centers participating in the study [18]. Standardized measurements of weight, height and blood pressure (BP) were collected.
BP was measured in pediatric offices using the auscultatory method with the right arm. The participants remained seated at rest for 5 min. Two measurements were taken at least 2 min apart on the same day, and a third measurement was repeated if there were differences over 4 mmHg. The average of the measurements was used. BP values were standardized by age, sex and height using the reference tables of the Fourth Report of Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents (NHBPEP) [19].
Weight was measured by means of a digital scale, and height was measured with a telescopic height rod. Two measurements were made, and the average was calculated. Using the weight and height, BMI was estimated in kg/m2.
Biochemical parameters were obtained from a blood sample taken at primary care centers by venipuncture using a Vacutainer©; the samples were obtained after the participant had fasted for 8 h. Venous blood was collected and separated into a tube with anticoagulant and a tube with whole blood, and the samples were stored at 4 °C immediately after extraction.
The following serum parameters of iron metabolism were analyzed: serum iron (Is) by ferrocin, serum ferritin (Fs), serum transferrin (Tf) and transferrin saturation (STf). STf values were calculated using the following formula: STf % = (Serum iron (µg/dl) × 70,645)/Transferrin (mg/dl) [20].
Total cholesterol (TC) and high-density lipoproteins (HDL-Chol) were quantified using enzymatic methods (cholesterol oxidase, esterase and peroxidase); low-density lipoproteins (LDL-Chol) were quantified using the Friedewald formula: LDL = (CT-HDL)—(TG/5); triglycerides (TG) were quantified using by the lipase/glycerol kinase colorimetric method; C-reactive protein (CRP) was quantified via immunoturbidimetry; and glucose was quantified using an enzymatic method (glucose hexokinase coupled to glucose 6-P dehydrogenase). All measurements were carried out on an ADVIA Chemistry XPT from Siemens Healthineers in the Clinical Biochemistry Laboratory of Puerta de Hierro University Hospital (Majadahonda, Madrid).
Insulin was measured via chemiluminescence, and HbA1c was measured via high-performance liquid chromatography (HPLC) on a TOSOH G8 analyzer. Insulin resistance (IR) was estimated using the homeostatic model assessment of insulin resistance (HOMA-IR), calculated as (fasting glucose (mg/dL) x fasting insulin (µU/mL))/405 [21].
Definition of metabolic abnormalities
The criteria of the National Heart, Lung and Blood Institute [22] and the European Guidelines on Cardiovascular Disease Prevention [23] were used to define altered lipid and glycemic profile values:
Lipid profile: high TC, TC ≥ 200 mg/dL; high TG, TG ≥ 130 mg/dL; low HDL-Chol, HDL-Chol < 40 mg/dL; and high LDL-Chol, LDL-Chol ≥ 130 mg/dL; and.
Glycemic profile: prediabetes, fasting blood glucose > 100 mg/dL or HbA1c ≥ 5.7%; hyperinsulinemia ≥ 15 µU/dL; and high IR, HOMA-IR ≥ 3.16 µU/dL.
High BP was defined using the 90th percentile of systolic and/or diastolic BP for age and sex following the recommendations of the European Society of Hypertension for children and adolescents [24].
Covariates
The sociodemographic variables included sex, age, and family purchasing power. Purchasing power was estimated with the Family Affluence Scale (FAS-II), which is a global indicator of a family's socioeconomic level [low (0–3 points), medium (4–5 points) or high (6–9 points)] [25].
Other covariates were mean daily iron intake; quality of the diet (Mediterranean Diet Quality Index (Med-DQI) [26] estimated on the basis of a semiquantitative food consumption frequency questionnaire used to record the frequency of consumption (daily, weekly, monthly or yearly) of 145 food items in the last year); and physical activity (Physical Activity Questionnaire—Children (PAQ-C), with a score ranging from 1 (little physical activity) to 5 (high physical activity)) [27].
This study complies with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Ramón y Cajal University Hospital in Madrid, Spain (CIHURC- 122/11). Written consent was obtained from the parents and/or guardians of the participants, and the data were anonymized to ensure confidentiality.
Statistical analysis
Is (< 68, 69–94 and > 94 μg/mL), Fs (< 33, 33–49 and > 49 ng/mL), Tf (< 256, 256–280 and > 280 mg/dl) and STf (< 17.8, 17.8–24.5 and > 24.5%) were categorized into tertiles.
To study the association between iron metabolism markers and cardiometabolic biochemical parameters, two sequential multiple linear regression models were developed, with progressive adjustment of the variables, using the lower tertile as the reference category: Model 1) adjusted for sex, age, family purchasing power, iron intake, quality of diet and physical activity; and Model 2) Model 1 plus BMI and CRP. Taking into account that some markers, mainly glycemic markers, did not follow a normal distribution, these linear regression models were repeated with logarithmic transformation of the cardiometabolic biochemical parameters (supplementary material).
Through logistic regression, associations between the tertiles of the markers of iron metabolism and the cardiometabolic alterations and adjusting for the possible confounding factors were estimated, calculating odds ratios (ORs) with the same sequential models described above.
The level of statistical significance was established at p < 0.05 (two-tailed) for all estimators.
The analyses were carried out in STATA 16.1 (StataCorp, College Station, Texas, USA).
Results
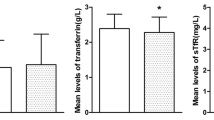
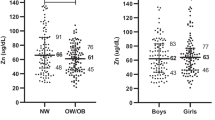
Table 1 provides the demographic and anthropometric characteristics and mean values for biomarkers of iron metabolism and the lipid and glycemic profiles of the study population (N = 1954). The mean age of the participants was 9.0 years, and 51.5% were female. A total of 14.0% lived in households with low purchasing power. The mean concentrations of Is, Fs, Tf, and STf were 83.0 μg/mL, 45.5 ng/mL, 269.5 mg/dL, and 22.0%, respectively.
Tables 2 and 3 show the results of the multiple linear regression models for Is, Fs, Tf and STf with the cardiometabolic parameters, adjusted for the main covariates. In Model 2, controlling for sociodemographic variables, diet quality, iron intake, physical activity, BMI and CRP, participants with high levels of Is (tertile 3), compared to those with low levels (tertile 1), had higher CT and HDL-Chol values, with estimated β coefficients of 3.17 (95% CI: 0.24; 6.11) and 1.47 (95% CI: 0.05; 2.88), respectively (Table 2). Regarding the glycemic profile, there was a negative association between Is levels and all glycemic parameters in Model 1; after including BMI and CRP (Model 2), the association was maintained for tertile 3 of fasting glycemia (β coef.: –1.81 (95% CI: –2.63; –0.98)) and HbA1c (β coef.: –0.06 (95% CI: –0.09; –0.03)) (Table 2).
Children with high levels of Fs (tertile 3) had, in the model of maximum adjustment, higher levels of TC and LDL-Chol (β coef.: 3.05 (95% CI: 0.18, 5.93) and 5.30 (95% CI: 2.84, 7.76), respectively) and lower levels of HDL-Chol (β coef.: –2.23 (95% CI: –3.61; –0.85)). There was a negative correlation between Fs and the glycemic parameters; when adjusted for BMI and CRP, the correlation was maintained only for HbA1c (β coef.: –0.05 (95% CI: –0.08; –0.02)) (Table 2).
Regarding Tf (Table 3), there was a positive association between high levels of Tf (tertile 3) and the concentration of CT [β coef.: 9.12 (95% CI: 6.26; 11.97)], HDL-Chol [β coef.: 2.95 (95% CI: 1.57; 4.33)], LDL-Chol [β coef.: 4.06 (95% CI: 1.59; 6.53)], and TG [β coef.: 10.34 (95% CI: 7.09; 13.60)]. Additionally, high Tf tertiles were associated with a higher fasting glucose concentration [β coef.: 1.31 (95% CI: 0.50; 2.13)] and HbA1c [β coef.: 0.04 (95% CI: 0.01; 0.06)].
Finally, there was a negative relationship between high levels of STf and all glycemic profile parameters (Table 3), with lower concentrations of glucose (p < 0.001), HbA1c (p < 0.001), and insulin (p < 0.05) and lower HOMA-IR values (p < 0.05).
The associations of the cardiometabolic parameters and the Is, Fs, Tf and STf tertiles, with logarithmic transformation of the CMRFs (Tables S1 and S2 of the supplementary material), were similar.
Table S3 (supplementary material) shows the prevalence of cardiometabolic risk factors in children aged 9–10 years.
Tables 4 and 5 show associations, in terms of adjusted OR, between the tertiles of the iron parameters and the prevalence of CMRFs. For Is, in Model 2, for the high tertile, the OR of having high LDL-Chol was 1.82 (95% CI: 1.03; 3.22), and the OR for low HDL-Chol values was 0.34 (95% CI: 0.17; 0.67). The risks (OR) of prediabetes, high insulin and high HOMA-IR were lower for the upper Is tertiles than for the lowest tertile (Table 4).
The association between Fs and having low HDL-Chol and high BP increased positively in tertile 3 compared to tertile 1, with ORs of 2.07 (95% CI: 1.16, 3.68) and 1.46 (OR 95% CI: 1.01, 2.13), respectively.
Compared with the participants in the lowest Tf tertile, the participants in the upper tertiles had a higher risk of high TC (OR: 1.55; 95% CI: 1.04; 2.32); high TG (OR: 2.32; 95% CI: 1.56; 3.45); high insulin (OR: 1.68; 95% CI: 1.03; 2.75) and high HOMA-IR values (OR: 1.90; 95% CI: 1.16; 3.12).
Participants in the upper STf tertiles had low HDL-Chol (OR: 0.44; 95% CI: 0.23; 0.84) compared with that of participants in the lower tertile. Additionally, the ORs for prediabetes, high insulin and high HOMA-IR were significantly lower for the participants in higher STf, tertiles, with ORs of 0.53 (95% CI: 0.34; 0.82), 0.48 (CI 95: 0.28; 0.82) and 0.37 (95% CI: 0.22; 0.64), respectively.
Discussion
This study examined the relationship between different parameters of iron metabolism and CMRFs in a representative sample of children aged 9–10 years in Madrid (Spain). The direction and magnitude of the associations was variable depending on the biomarker analyzed. A worse lipid profile was observed with high Fs and Tf values, and Is was associated with an increase in both LDL-Chol and HDL-Chol. The glycemic profile was better in children who had high concentrations of Is and STf and was more unfavorable in children with high values of Tf. Finally, the only biomarker associated with an increased risk of hypertension was Fs.
Studies that have evaluated the relationship between iron parameters and CMRFs in the pediatric population are scarce [12,13,14, 28,29,30,31], and most have been carried out in Asian countries [12,13,14, 28, 29, 31]. The most widely used indicator of iron metabolism in these studies has been Fs, generally observing a worse lipid profile with higher concentrations of this biomarker. There are few disputes about the association between Fs and HDL-Chol levels, where there is a decrease in this cholesterol fraction when Fs levels are high [12, 13, 28, 30]; however, one study found a positive relationship, i.e., an increase in HDL-Chol [14]. The two studies that have examined the relationship between Fs and TC observed, as in this study, a positive association [12, 13]. There are more discrepancies in the association between Fs and TG; although a large number of studies found no association [12, 14, 30], two other studies observed contradictory associations, with one reporting a positive correlations [28] and the other reporting a negative correlation [13]. Few authors have incorporated other indicators of iron metabolism apart from Fs. Lee et al. studied Is and ST [12], and Zhang et al. studied Is [14], observing, as in our study, an increase in HDL-Chol with an increase in the levels of these biomarkers.
The evidence of associations between iron indicators and glycemic metabolism is also highly variable depending on the biomarkers used for evaluation. Three studies [12, 14, 30] report no association between Fs and fasting blood glucose, similar to the results of our study; however, in another work, higher concentrations of Fs were related to decreases in glucose levels [28]. Likewise, a majority of studies did not find an association between Fs and the HOMA-IR index [12, 13, 29]; however, one study reported a positive relationship [30]. Associations with other indicators of iron metabolism were similar between those observed in our study and those estimated by Lee et al., i.e., a decrease in blood glucose, insulin and HOMA-IR index with an increase in Is and STf [12], and a positive relationship between these glycemic indicators and Tf [29].
Regarding blood pressure, the increased risk of elevated blood pressure in children with high concentrations of Fs is consistent with the results reported by Yi et al. in a study of a male child population [28]; another study found no associations with Fs but rather with Is [14].
The mechanisms to explain the correlation between iron metabolism and lipid and glycemic metabolism are very complex and are related to the activation of oxidative stress factors, the response to inflammatory hypoxia and cell proliferation [32]. Excessive iron is sequestered by macrophages and deposited in muscles and adipose tissue, accelerating lipolysis, which affects the oxidation of lipoproteins, glucose and IR [33, 34]. This tissue damage also includes blood vessels, resulting in hypertension and vascular damage. In addition, high levels of iron generate high oxidative activity in the pancreas that can damage β cells, thus affecting insulin production [35]. Our results support these mechanisms, i.e., high levels of iron storage markers alter the lipid profile. In contrast, high levels of Is, Tf and STf activate the production of HDL-Chol, which can serve as a protective factor against oxidative stress in tissues and glucose metabolism [34]. The mechanisms underlying the negative association between Is and STf and glycemic metabolism and IR remain to be determined. High levels of ferritin and transferrin could antagonize the effect of insulin and contribute to IR [34]. Low levels of Is and STf, indicators of functional iron deficiency [36], can cause hepcidin dysregulation, resulting in iron being retained in reticulocytes, altering glucose metabolism and causing IR [37].
The levels of iron parameters fluctuate with age and can be altered through inflammatory processes, with certain chronic diseases and states of obesity causing chronic inflammation [2]. In this study, when introducing BMI and CRP differently from other covariates, the magnitude of the association was generally attenuated, potentially indicating a mediation effect; however, an independent effect remains.
Strengths and limitations
To ensure the correct interpretation of the results of this study, some limitations and strengths should be considered. First, given the cross-sectional nature of the study design, the underlying causal sequence of the relationships between iron metabolism and CMRFs cannot be identified. Second, the data used to define high blood pressure were based on 1 measurement and not on 3 measurements taken on different days, as recommended by the European Society of Hypertension [24]. Third, although our models include the main covariates adjustment, some residual confounders cannot be ruled out.
Regarding strengths, various indicators of iron metabolism were available. In addition, each CMRF was analyzed independently to better understand its relationship with iron parameters. Second, this is one of the few studies conducted with a representative sample of the child population. Third, the main confounding variables were taken into account, including diet, with the quantification of iron intake, and physical activity. Finally, to control the independent effect of inflammatory mechanisms related to excess weight, BMI was included, as was CRP, in the regression models sequentially.
Conclusions
The results of this study show that indicators of iron metabolism are associated with cardiometabolic alterations, with a direction and magnitude that vary depending on the biomarker analyzed. High concentrations of Fs and Tf are associated with a worse lipid profile, and Is is associated with an increase in both LDL-Chol and HDL-Chol. The glycemic profile is better in children who have high concentrations of Is and STf and is more unfavorable in children with high concentrations of Tf. The only biomarker positively associated with an increased risk of hypertension was Fs. Iron parameters in the pediatric population could be of great help to detect cardiometabolic alterations early.
Data availability
According to private and confidential clauses stated in the informed consent, the dataset generated and analyzed during the current study is restricted and not publicly available for ethical reasons. Data will be available from the corresponding author (Dr. Honorato Ortiz-Marrón; E-mail: honorato.ortiz@salud.madrid.org) on reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- BP:
-
Blood Pressure
- CMRFs:
-
Cardiometabolic risk factors
- CI:
-
Confidence Interval
- ELOIN:
-
Longitudinal Childhood Obesity Study
- Fs:
-
Serum ferritin
- HbA1c:
-
Glycated haemoglobin
- HDL-Chol:
-
High-Density Lipoprotein Cholesterol
- HOMA-IR:
-
Homeostatic Model Assessment—Insulin Resistance
- Is:
-
Serum iron
- LDL-Chol:
-
Low-Density Lipoprotein Cholesterol
- MetS:
-
Metabolic Syndrome
- OR:
-
Odds Ratio
- SD:
-
Standard Deviation
- STf:
-
Transferrin saturation
- TC:
-
Total Cholesterol
- Tf:
-
Transferrin
- TG:
-
Triglycerides
References
Milto IV, Suhodolo IV, Prokopieva VD, Klimenteva TK (2016) Molecular and Cellular Bases of Iron Metabolism in Humans. Biochem Biokhimiia 81(6):549–564. https://doi.org/10.1134/S0006297916060018
Cappellini MD, Scaramellini N, Motta I (2023) Iron status in chronic inflammatory disease: therapeutic implications. Pol Arch Intern Med 133(2):16430. https://doi.org/10.20452/pamw.16430
Vogt ACS, Arsiwala T, Mohsen M, Vogel M, Manolova V, Bachmann MF (2021) On Iron Metabolism and Its Regulation. Int J Mol Sci 22(9):4591. https://doi.org/10.3390/ijms22094591
Camaschella C, Nai A, Silvestri L (2020) Iron metabolism and iron disorders revisited in the hepcidin era. Haematologica 105(2):260–272. https://doi.org/10.3324/haematol.2019.232124
Naito Y, Masuyama T, Ishihara M (2021) Iron and cardiovascular diseases. J Cardiol 77(2):160–165. https://doi.org/10.1016/j.jjcc.2020.07.009
Kunutsor SK, Apekey TA, Walley J, Kain K (2013) Ferritin levels and risk of type 2 diabetes mellitus: an updated systematic review and meta-analysis of prospective evidence. Diabetes Metab Res Rev 29(4):308–318. https://doi.org/10.1002/dmrr.2394
Orban E, Schwab S, Thorand B, Huth C (2014) Association of iron indices and type 2 diabetes: a meta-analysis of observational studies. Diabetes Metab Res Rev 30(5):372–394. https://doi.org/10.1002/dmrr.2506
Li S, Zhang X (2021) Iron in Cardiovascular Disease: Challenges and Potentials. Front Cardiovasc Med 8:707138. https://doi.org/10.3389/fcvm.2021.707138
Zhang WCB, Xing Y, Shao B (2021) Serum Ferritin and the Risk of Metabolic Syndrome: A Systematic Review and Dose-Response Meta-Analysis of Cross-sectional Studies. Biomed Environ Sci BES 34(8):623–631. https://doi.org/10.3967/bes2021.086
Suárez-Ortegón MF, Ensaldo-Carrasco E, Shi T, McLachlan S, Fernández-Real JM, Wild SH (2018) Ferritin, metabolic syndrome and its components: A systematic review and meta-analysis. Atherosclerosis 275:97–106. https://doi.org/10.1016/j.atherosclerosis.2018.05.043
Abril-Ulloa V, Flores-Mateo G, Solà-Alberich R, Manuel-y-Keenoy B, Arija V (2014) Ferritin levels and risk of metabolic syndrome: meta-analysis of observational studies. BMC Public Health 14:483. https://doi.org/10.1186/1471-2458-14-483
Lee HJ, Jang HB, Park JE et al (2014) Relationship between Serum Levels of Body Iron Parameters and Insulin Resistance and Metabolic Syndrome in Korean Children. Osong Public Health Res Perspect 5(4):204–210. https://doi.org/10.1016/j.phrp.2014.06.005
Kim YE, Kim DH, Roh YK et al (2016) Relationship between Serum Ferritin Levels and Dyslipidemia in Korean Adolescents. PLoS ONE 11(4):e0153167. https://doi.org/10.1371/journal.pone.0153167
Zhang H, Wang L, Li S et al (2020) Association of Iron Storage Markers with Metabolic Syndrome and Its Components in Chinese Rural 6–12 Years Old Children: The 2010–2012 China National Nutrition and Health Survey. Nutrients 12(5):1486. https://doi.org/10.3390/nu12051486
Weiss R, Dziura J, Burgert TS et al (2004) Obesity and the metabolic syndrome in children and adolescents. N Engl J Med 350(23):2362–2374. https://doi.org/10.1056/NEJMoa031049
Magge SN, Goodman E, Armstrong SC (2017) CommitteE On Nutrition, Section on Endocrinology, Section on Obesity. The Metabolic Syndrome in Children and Adolescents: Shifting the Focus to Cardiometabolic Risk Factor Clustering. Pediatrics 140(2):e20171603. https://doi.org/10.1542/peds.2017-1603
Ortiz-Marron H, Cuadrado-Gamarra JI, Esteban-Vasallo M, Cortes-Rico O, Sanchez-Diaz J, Galan-Labaca I (2016) The Longitudinal Childhood Obesity Study (ELOIN): Design, Participation and Characteristics of the Baseline Sample. Rev Espanola Cardiol Engl Ed 69(5):521–523. https://doi.org/10.1016/j.rec.2016.01.017
Pérez-Farinós N, Galán I, Ordobás M, Zorrilla B, Cantero JL, Ramírez R (2009) A sampling design for a sentinel general practitioner network. Gac Sanit SESPAS 23(3):186–191. https://doi.org/10.1016/j.gaceta.2008.05.010
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2 Suppl 4th Report):555–576
Thomas DW, Hinchliffe RF, Briggs C et al (2013) Guideline for the laboratory diagnosis of functional iron deficiency. Br J Haematol 161(5):639–648. https://doi.org/10.1111/bjh.12311
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419. https://doi.org/10.1007/BF00280883
Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute (2011) Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 128 Suppl 5:S213–256. https://doi.org/10.1542/peds.2009-2107C
2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association | Stroke. Accessed March 30, 2023. https://www.ahajournals.org/doi/10.1161/STR.0000000000000375c
Lurbe E, Agabiti-Rosei E, Cruickshank JK et al (2016) 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens 34(10):1887–1920. https://doi.org/10.1097/HJH.0000000000001039
Torsheim T, Cavallo F, Levin KA et al (2016) Psychometric Validation of the Revised Family Affluence Scale: a Latent Variable Approach. Child Indic Res 9:771–784. https://doi.org/10.1007/s12187-015-9339-x
Gerber M (2006) Qualitative methods to evaluate Mediterranean diet in adults. Public Health Nutr 9(1A):147–151. https://doi.org/10.1079/phn2005937
Manchola-González J, Bagur-Calafat C, Girabent-Farrés M (2017) Fiabilidad de la versión española del Cuestionario de actividad física PAQ-C / Reliability of the Spanish Version of Questionnaire of Physical Activity PAQ-C. Rev Int Med Cienc Act Física Deporte (65). https://doi.org/10.15366/rimcafd2017.65.010
Yi KH, Hwang JS, Lim SW, Lee JA, Kim DH, Lim JS (2016) Ferritin level is associated with metabolic syndrome and elevated alanine aminotransferase in children and adolescents. J Pediatr Endocrinol Metab JPEM 29(12):1337–1344. https://doi.org/10.1515/jpem-2016-0045
Wei J, Luo X, Zhou S et al (2019) Associations between iron status and insulin resistance in Chinese children and adolescents: findings from the China Health and Nutrition Survey. Asia Pac J Clin Nutr 28(4):819–825. https://doi.org/10.6133/apjcn.201912_28(4).0019
Suárez-Ortegón MF, Blanco E, McLachlan S et al (2019) Ferritin levels throughout childhood and metabolic syndrome in adolescent stage. Nutr Metab Cardiovasc Dis NMCD 29(3):268–278. https://doi.org/10.1016/j.numecd.2018.11.008
Zhu Y, He B, Xiao Y, Chen Y (2019) Iron metabolism and its association with dyslipidemia risk in children and adolescents: a cross-sectional study. Lipids Health Dis 18(1):50. https://doi.org/10.1186/s12944-019-0985-8
Galaris D, Barbouti A, Pantopoulos K (2019) Iron homeostasis and oxidative stress: An intimate relationship. Biochim Biophys Acta Mol Cell Res 1866(12):118535. https://doi.org/10.1016/j.bbamcr.2019.118535
Green A, Basile R, Rumberger JM (2006) Transferrin and iron induce insulin resistance of glucose transport in adipocytes. Metabolism 55(8):1042–1045. https://doi.org/10.1016/j.metabol.2006.03.015
Fernández-Real JM, McClain D, Manco M (2015) Mechanisms Linking Glucose Homeostasis and Iron Metabolism Toward the Onset and Progression of Type 2 Diabetes. Diabetes Care 38(11):2169–2176. https://doi.org/10.2337/dc14-3082
Harrison AV, Lorenzo FR, McClain DA (2023) Iron and the Pathophysiology of Diabetes. Annu Rev Physiol 85:339–362. https://doi.org/10.1146/annurev-physiol-022522-102832
Sierpinski R, Josiak K, Suchocki T et al (2021) High soluble transferrin receptor in patients with heart failure: a measure of iron deficiency and a strong predictor of mortality. Eur J Heart Fail 23(6):919–932. https://doi.org/10.1002/ejhf.2036
Ambachew S, Biadgo B (2017) Hepcidin in Iron Homeostasis: Diagnostic and Therapeutic Implications in Type 2 Diabetes Mellitus Patients. Acta Haematol 138(4):183–193. https://doi.org/10.1159/000481391
Acknowledgements
We thank all of the health care professionals for their support with the study and all the families who participated. We are grateful to Demométrica, Sondaxe and Sigmados, which conducted the telephone interviews. This project received a grant for the translation and publication of this paper from the Foundation for Biosanitary Research and Innovation in Primary Care (FIIBAP).
Funding
The ELOIN study was funded by the General Directorate of Public Health of the Ministry of Health of the Community of Madrid. The authors have not received financial support for the research, authorship or publication of this article. This project received a grant for the translation and publication of this paper from the Foundation for Biosanitary Research and Innovation in Primary Care (FIIBAP).
Author information
Authors and Affiliations
Contributions
Honorato Ortiz-Marrón and Iñaki Galán conceptualized and designed the study, wrote the initial draft of the manuscript, created tables and figures and checked and revised the final manuscript. Gloria Cabañas Pujadas prepared figures and tables and conducted the initial analysis. Encarnación Donoso Navarro, Mar Burreros García, María Isabel Herreros Álvaro, Alma María Mejía Fernández de Velasco and Ana Cornejo Gutiérrez critically reviewed the manuscript for intellectual content and edited the manuscript. All authors commented on previous versions of the manuscript and read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
The Ethics Committee of Hospital Ramon y Cajal in Madrid approved the study (CIHURC- 122/11). This study was conducted in accordance with the Declaration of Helsinki, and all methods were performed in accordance with the relevant guidelines and regulations.
Informed consent
Written informed consent was obtained from the parents/caregivers of all participating children.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ortiz-Marrón, H., Cabañas Pujadas, G., Donoso Navarro, E. et al. Association between biomarkers of iron status and cardiometabolic risk in Spanish children aged 9–10 years. The ELOIN study. Eur J Pediatr 182, 5649–5659 (2023). https://doi.org/10.1007/s00431-023-05244-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05244-1