Abstract
The purpose of this study is to define the impact of early brain growth trajectory in very low birth weight infants (VLBWI) on neurological prognosis at 2 years, assessed using sequential ultrasound (US) scans. This is a prospective cohort study with consecutive inclusion of VLBWI ≤ 32 weeks gestational age and ≤ 1500 g at birth. Total brain volume (TBV) was assessed using sequential 3D-US from birth to discharge. Prognosis at 2 years (corrected age) was assessed using the Bayley Scales of Infant and Toddler Development Third Edition. TBV showed slower growth with postmenstrual age (PMA) in those VLBWI who had an adverse cognitive prognosis compared to those with good cognitive prognosis (mean difference in TBV between prognostic groups from 4.56 cm3 at 28 weeks to 42.58 cm3 at 43 weeks) as well as in those with adverse language prognosis (mean difference in TBV from 2.21 cm3 at 28 weeks to 26.98 cm3 at 43 weeks) although other variables showed more impact than TBV on language prognosis (gestational age at birth, brain injury at term, and socioeconomic status). No association was found between TBV and motor prognosis. Brain growth rate was also significantly higher in those VLBWI who presented good cognitive scores (18.78 + (0.33 × (PMA-33)) cm3/week) compared to those with adverse cognitive outcome (13.73 + (0.64 × (PMA-33)) cm3/week).
Conclusion: Early altered brain growth is associated with poor cognitive prognosis at 2 years of age. Using sequential US monitoring, we can detect early brain growth deviation in patients who will have adverse cognitive outcomes.
What is known: • The prediction of neurodevelopmental outcome of VLBWI is mostly based on the presence of brain injury in US and structural magnetic resonance imaging (MRI) at term. • Some studies have related brain volume measured on MRI at term with neurodevelopment outcome. | |
What is new: • VLBWI with adverse cognitive prognosis at two years of age present smaller brain volumes detectable by sequential US during NICU admission. • Brain volume can be estimated from 2D and 3D US and has prognostic value in VLBWI. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Very low birth weight infants (VLBWI) are a high-risk population exposed to high-morbidity rates and a wide spectrum of long-term neurodevelopmental abnormalities. Although advances in perinatal medicine have led to an increase in the survival rates at extreme gestational ages [1,2,3,4,5], the long-term neurologic outcome of these patients remains a matter of concern due to high rates of neurodevelopmental disorders including intellectual deficits, behavioral disorders, cerebral palsy, and epilepsy [3, 4, 6,7,8,9,10]. These sequelae of prematurity have a great impact on the child’s future health, with notable family and social impact.
Brain imaging using ultrasound (US) and magnetic resonance imaging (MRI) is a valuable tool during neonatal admission to diagnose brain injury, assisting the clinician to predict the long-term outcome of preterm infants. The increasing research interest in the developing brain together with the technological improvement of these tools has led to a better understanding of the impact of prematurity on the immature brain. MRI is considered the gold standard but cannot rival US for its role in sequential and incubator-based neurological assessment in the preterm infant. Aside from brain injury, US has the potential to estimate brain volumes as reliably as MRI [11] allowing the study of early brain growth patterns. Moreover, we have previously demonstrated that those preterm infants born at lower gestational age and exposed to an increasing number of comorbidities have a deviated pattern of brain growth [12]. However, our study was previously based on the results of term-equivalent MRI while our aim in this study is to identify the pattern of early brain growth in the preterm infants in relation to the 2-year neurodevelopmental outcome.
Materials and methods
Study population
This longitudinal study included VLBWI admitted to the Hospital Puerta del Mar, Cádiz, Spain, from May 2018 to January 2021. We consecutively enrolled those VLBWI with a birth weight equal or less than 1500 g and/or a gestational age at birth equal or less than 32 weeks. The exclusion criteria were defined as the presence of congenital or chromosomal anomalies, metabolic disorders, and central nervous system infections. We also excluded those preterm infants who presented posthemorrhagic ventricular dilatation or died. This study was approved by the Research and Ethics Committee, and all parents or guardians of the participants provided informed consent.
Perinatal and postnatal variables were prospectively collected (see Table S1 in Supplemental material for a detailed definition of the clinical variables).
2D and 3D brain US
Weekly 2D and 3D brains US were carried out while the included patients were admitted to the neonatal intensive care unit (NICU), with the infant lying supine and their head turned to the right. Volume acquisition was carried out using the 3D option of the 3D/4D Voluson S8 BT18 (General Electric Healthcare, Buckinghamshire, United Kingdom) as explained elsewhere [11].
TBV was measured by manual tracing the brain contour on 6 slices at 30 degrees rotation on the vertical axis using VOCAL (Virtual Organ Computer-Aided Analysis) feature of the 4D View software (version 17.0; GE Healthcare). This technique provides a reliable measure of TBV as previously published by our group [11].
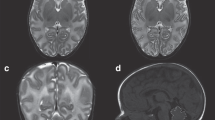
Brain MRI
At term-corrected age, all patients underwent a cranial MRI. MRI scans were performed using 1.5 T scanner Magneton Symphony (Siemens Health Care, Erlangen, Germany) located in the radiology unit. T1-weighted images were obtained using a three-dimensional spoiled gradient [repetition time 1660 (RT)/echo time 5.16(ET)] and transverse T2-weighted turbo spin-echo imaging (4180.00/98.00).
Term-MRI scans were evaluated using the scale published by Kidokoro et al. [13], which separately grades the development and injury of the cortical and deep gray matter, white matter and cerebellum. Those with a score of less than 8 points were considered to have normal/mild abnormalities at term-MRI, while those with a score equal or greater than 8 points were classified as having moderate/severe abnormalities at term-MRI.
Assessment at two years of age
All the included patients were reviewed after discharge as part of the neonatal neurology follow-up program. Assessments at two years of corrected age were performed using the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III). The scores obtained on the cognitive, motor, and language scales are standardized with a mean of 100 and a standard deviation of 15. We considered both the quantitative data and further dichotomized the scores considering a good neurodevelopmental outcome if the score was greater than or equal to 85 and adverse outcome if they scored under 85 for each scale.
Statistical analysis
Clinical characteristics and demographic variables were described as frequency and percentage if categorical, or mean and standard deviation (sd), or median and interquartile range [IQR] according to their distribution. Bivariate analysis was performed using Pearsonʼs chi-squared test or Fisherʼs exact test for categorical data and Studentʼs t-test or Mann–Whitney U test for continuous variables after testing for normality. Multilevel linear regression models were used to study the relationship between Bayley-III scores, TBV, and clinical variables accounting for repeated measurements and time. The included variables were selected based on the theoretical background, and a backward stepwise approach was performed to exclude the non-significant variables if not considered to be variables for which an adjustment was needed.
Statistical analysis was conducted using Stata 16.0 (Stata Statistical Software: Release 16. College Station, TX: StataCorp LP). A result was considered statistically significant at p < 0.05.
Results
Clinical characteristics of the studied population and 2-year neurodevelopmental outcomes
For this study, we included those VLBWI who were admitted to the NICU at Puerta del Mar Hospital from May 2018 to January 2021, including a total population of 163 patients. Nineteen (11.7%) of these patients died during the neonatal period. Six (3.7%) patients were excluded: one patient for congenital cytomegalovirus infection (CMV), a patient with Down syndrome, and four patients for developing posthemorrhagic ventricular dilatation (PHVD). Of the remaining 138 patients, our final sample size included 105 (76.1%) that completed the assessment at 2 years of corrected age. These patients had a combined total of 719 brain US during their stay in the NICU (see Fig. S1 in Supplemental material).
Our population had a mean gestational age at birth of 29.3 (± 2.3) weeks and mean birth weight of 1168.6 (± 363.1) grams. Seventeen patients (16.19%) were small for gestational age (SGA). A detailed description of the perinatal variables, socioeconomic status, and comorbidities related to the 2-year neurodevelopmental outcome is shown in Table S2 in Supplemental material.
Motor outcome
Those with an adverse motor outcome had a lower proportion of exposure to prenatal steroids compared to those with a good motor outcome (7/13 (53.85%) vs. 75/88 (85.23%); p = 0.015), a higher proportion of severe retinopathy of prematurity (ROP) (4/13 (30.77%) vs. 3/91 (3.3%); p = 0.004), moderate/severe bronchopulmonary dysplasia (BPD) (6/13 (46.15%) vs. 13/90 (14.44%); p = 0.014), intraventricular hemorrhage (IVH) grade 3 (3/13 (23.08%) vs. 3/92 (3.26%); p = 0.024), moderate/severe white matter injury (WMI) (2/13 (15.38%) vs. 0/92 (0%); p = 0.014), higher scores on the Kidokoro scale (2 [0–10] vs. 0 [0–2]; p = 0.03), and a greater number of comorbidities (1 [0–3] vs. 0 [0–1]; p = 0.006), respectively (see Table S2 in Supplemental material).
Cognitive outcome
The proportion of multiple births 7/9 (77.78%) was higher in those with an adverse cognitive outcome when compared to those with a good cognitive outcome (34/96 (35.42%); p = 0.026). No other differences were found in the baseline characteristics of the studied population related to cognitive outcome (see Table S2 in Supplemental material).
Language outcome
Sex was associated with language scores at 2 years with females having better outcomes: 47 females/83 (56.63%) had good vs. 6 females/22 (27.27%) with an adverse language outcome; p = 0.001. Adverse language outcome was related to severe ROP (4/22 (18.88%) vs. 3/82 (3.66%); p = 0.035) and moderate/severe WMI (2/22 (9.09%) vs. 0/83 (0%); p = 0.042) (see Table S2 in Supplemental material).
Total brain volume (TBV) during early postnatal life related to 2-year neurodevelopmental outcome
We studied the association of sequential measurements of TBV, gestational age (GA) at birth, and PMA at the time of US, with the 2-year neurodevelopmental outcome (see Table 1). TBV was related to cognitive and language outcome, while no association was found with motor outcome.
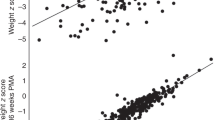
TBV showed a slower increased related to PMA in those VLBWI who had an adverse cognitive outcome, with mean TBV differences between both outcome groups being significant from 28 weeks PMA onwards and ranging from 4.56 cm3 at 28 weeks PMA to 42.58 cm3 at 43 weeks PMA (see Table 2 and Fig. 1).
Similarly, TBV showed a slower increase related to PMA in those VLBWI who had an adverse language outcome, with mean TBV differences between both outcome groups being significant from 28 weeks PMA onwards and ranging from 2.21 cm3 at 28 weeks PMA to 26.98 cm3 at 43 weeks PMA (see Table 3; Fig. 2).
Association of perinatal factors, maternal level of education, comorbidities, and brain injury with the prognostic scores
Motor outcome
Motor outcome at 2 years was related to GA at birth (β coef = 0.52; p = 0.008), sex (β coef (female) = 2.23; p = 0.025), being SGA (β coef = -4.4; p = 0.0001), and moderate/severe findings in term-equivalent MRI (β coef = −14.87; p = 0.0001). We did not find a statistically significant association of brain volumes during NICU admission and socioeconomic status (SES) on motor scores (see Table 4).
Cognitive outcome
Cognitive outcome was associated to GA at birth (β coef = 0.56; p = 0.005), sex (β coef (female) = 2.13; p = 0.033), SES (low SES group β coef = −5.7; p = 0.0001), being SGA (β coef = −2.67; p = 0.028), moderate/severe abnormalities on term-MRI (β coef = −12.87; p = 0.0001), and TBV (β coef = 0.02; p = 0.037) (see Table 4).
Language outcome
Language outcome at 2 years was associated with GA at birth (β coef = 0.86; p = 0.0001), SES (low SES group β coef = −11.85; p = 0.0001; medium SES group β coef = −10.51; p = 0.0001), moderate/severe abnormalities at term MRI (β coef = −14.26; p = 0.0001) while brain volume in early postnatal life was not related to language scores (see Table 4).
Brain growth rate related to cognitive outcome
As TBV was more consistently related to cognitive outcome, we explored brain growth rate related to the 2-year cognitive outcome. We calculated brain growth rate as the difference in TBV between two consecutive ultrasound scans divided by time (cm3/week). In those VLBWI with good cognitive outcome, brain growth rate was as follows: TBV growth rate (cm3/week) = 18.78 + (0.33 × (PMA-33)) while in those with an adverse cognitive outcome, it was adjusted to the following equation: TBV growth rate = 13.73 + (0.64 × (PMA-33)) (see Fig. 3 and Table S3 in Supplemental material).
TBV during early postnatal life in VLBWI with normal cognitive outcome related to PMA as a reference for clinical use
To facilitate establishing routine TBV monitoring during NICU admission of VLBWI, we estimated the TBV percentiles by PMA and sex in those patients with good cognitive outcomes (see Table 5 and Fig. 4). TBV can be accurately estimated using 2D US measurements of three orthogonal axes (biparietal diameter, vertical axis, and anteroposterior axis) as we have previously shown [11].
A detailed table of mean TBV by PMA and the population 95% confidence interval by PMA and sex is shown on Tables S4 in supplemental material.
Discussion
The study of TBV through serial US during NICU admission of VLBWI has allowed us to identify an early deviated pattern of brain growth related to 2-year neurodevelopmental outcome. While we have previously shown that TBV can be monitored accurately through 3D and 2D US [11] and we have shown that those preterm infants born at lower gestational ages and exposed to a greater number of comorbidities had smaller brain volumes related to moderate/severe findings in term-equivalent MRI, this study adds insights into the usefulness of early brain growth monitoring [12].
We found TBV was independently associated with the 2-year neurodevelopmental outcome, with those having good cognitive outcomes showing greater brain volume and brain growth during early postnatal life. In line with other studies, good cognitive outcome was also associated with GA at birth, being female, and the maternal level of education; being SGA, and having moderate to severe MRI findings had a negative impact on the 2-year cognitive outcome [14,15,16,17,18].
Similarly, TBV evolution during early postnatal life was associated with language scores in our preterm study population. Nevertheless, other variables were more importantly related to language outcome, with TBV losing significance when studied with such variables. Thus, language outcome showed a positive association with GA at birth and maternal level of education, while those children with moderate or severe brain injury had lower language scores at two years of age as shown elsewhere [19,20,21,22,23].
In turn, we found no association of TBV and brain growth during the first postnatal weeks and later motor scores at 2 years. We did find that motor outcome was affected by GA at birth, sex (with better motor scores in females), being SGA, and the presence of moderate to severe brain injury on term-MRI, as also supported by previous evidence in the literature [16, 24,25,26,27].
We have estimated the population mean of TBV per week of PMA and calculated TBV centiles in those preterm with good cognitive outcome to assist clinicians with normative reference values. This could help incorporating routine TBV monitoring during NICU admission.
The relationship between structural alterations on MRI at term corrected age and adverse long-term neurodevelopmental outcome has been extensively studied [28,29,30]. Some studies have related total and regional brain volumes measured on MRI at term to motor, cognitive, language, executive, and behavioral functioning in childhood [31,32,33,34,35]. Soria et al. [36] found reduced regional white and gray matter volumes and decreased intellectual functioning in their cohort of low-risk preterm newborns. Arhan et al. [37], similarly, studied regional brain volumes in low-risk preterm infants, identifying smaller volumes than their term controls, with these smaller regional volumes being associated with worse cognitive scores. Bolk et al. [38] found a positive association of volumes in specific brain areas, fine motor skills and visuomotor integration. Kelly et al. [39] found a relationship between white and gray matter volumes with cognitive and language outcomes, with no differences found in motor or behavioral scores.
Few studies have explored brain volumes earlier than term corrected age and through US, as we have seen, volume segmentations have been mostly performed at term equivalent MRI. In recent years, some authors have been interested in investigating early brain volume and their possible association with short- and long-term neurological prognosis. Graça et al. [40] studied a cohort of 128 infants (72 very preterm infants at term equivalent age and 56 term infants during their first postnatal week) in which they estimated brain volumes from intracranial diameters measured on brain US at term, finding that, even in the absence of structural brain damage or major cerebral lesions, preterm infants had smaller brain volumes than term infants. Similarly, they found that smaller brain volumes at term were associated with lower GA at birth, lower birth weight and being SGA. While they were one of the first research groups to study brain volume from ultrasound images, they did not perform early brain volume estimation, nor did they recruit a longitudinal cohort as these preterm infants were assessed after term corrected age. Moreover, in contrast to our previous report [11], their model was not validated in relation to manual segmentation or MRI based TBV estimation. Simsek et al. [41] developed a similar model of estimating brain volume from intracranial diameters measured on ultrasound images based on an ellipsoid, studying brain volume longitudinally in a cohort of 121 preterm infants from the first postnatal days until 34 weeks of corrected age. Subsequently, they related lower brain volumes to poorer neurodevelopment outcomes assessed at two years of age. This was one of the first studies to investigate the relationship between brain volumes measured by US and neurodevelopment in VLBW preterm infants, although it was also based on indirect measurements of brain volume. Furthermore, Cuzzilla et al. [42] evaluated brain growth using sequential cUS regional linear measures from birth to term-equivalent age in a cohort of 139 infants born at < 30 weeks and related it to cognitive, language, and motor outcome at two years of age. They found a positive relationship between the growth of the corpus callosum, cerebellum, and vermis with cognitive and language scores; in contrast, no relationship was demonstrated between tissue measurements and motor scores. This study, unlike the previous ones, did not estimate total brain volume, but instead assessed brain growth through a series of multiple linear measurements at different levels of brain tissue, directly studying the relationship of these isolated measurements with the prognosis at two years. Our study provides new insights into the study of brain growth, thanks to the use of 3D ultrasound, directly assessing total brain volume sequentially from the time of birth, and subsequently relating it to long-term neurological prognosis.
Our study suggests that we can identify an early deviation of the trajectory of brain growth in those preterm infants who will have worse cognitive scores in the long term. We have established reference values that would enable the clinician to identify preterm infants who, despite not necessarily showing brain injury, have an altered brain growth pattern and, therefore, are at a higher risk of presenting adverse neurodevelopmental outcomes.
This study has some limitations that should be acknowledged. Firstly, we had a small number of patients who had adverse neurological outcomes, which has limited us from more robust statistical analysis. Regional volumes may further explain the relationship between early brain growth and neurodevelopmental outcome. We measured TBV and not regional brain volume, which is warranted in future research.
Conclusions
Measurement of smaller TBV by serial ultrasound during the first weeks of life and up to term age is associated with poor cognitive prognosis at two years of age. Using a sequence of ultrasound scans, we can detect a deviation of brain growth in patients who will have worse cognitive outcomes. We propose normal values for TBV that can serve as a reference as part of the overall assessment in NICU incubators.
Data availability
The data from this study are available from the corresponding author upon reasonable request.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- CMV:
-
Cytomegalovirus
- GA:
-
Gestational age
- IVH:
-
Intraventricular hemorrhage
- MRI:
-
Magnetic resonance imaging
- NICU:
-
Neonatal intensive care unit
- PHVD:
-
Posthemorrhagic ventricular dilatation
- PMA:
-
Postmenstrual age
- ROP:
-
Retinopathy of prematurity
- SES:
-
Socioeconomic status
- SGA:
-
Small for gestational age
- TBV:
-
Total brain volume
- US:
-
Ultrasound
- VLBWI:
-
Very low birth weight infants
- VOCAL:
-
Virtual Organ Computer-Aided Analysis
- WMI:
-
White matter injury
References
Ream MA, Lehwald L (2018) Neurologic consequences of preterm birth. Curr Neurol Neurosci Rep 18:48
Patel RM (2016) Short- and long-term outcomes for extremely preterm infants. Am J Perinatol 33:318–328
Moore T, Hennessy EM, Myles J, Johnson SJ, Draper ES, Costeloe KL, Marlow N (2012) Neurological and developmental outcome in extremely preterm children born in England in 1995 and 2006: the EPICure studies. BMJ 345:e7961
Pierrat V, Marchand-Martin L, Arnaud C, Kaminski M, Resche-Rigon M, Lebeaux C, Bodeau-Livinec F, Morgan AS, Goffinet F, Marret S, Ancel PY, group E-w, (2017) Neurodevelopmental outcome at 2 years for preterm children born at 22 to 34 weeks’ gestation in France in 2011: EPIPAGE-2 cohort study. BMJ 358:j3448
Cao Y, Jiang S, Sun J, Hei M, Wang L, Zhang H, Ma X, Wu H, Li X, Sun H, Zhou W, Shi Y, Wang Y, Gu X, Yang T, Lu Y, Du L, Chen C, Lee SK, Zhou W, Chinese Neonatal N (2021) Assessment of neonatal intensive care unit practices, morbidity, and mortality among very preterm infants in China. JAMA Netw Open 4:e2118904
Serenius F, Källén K, Blennow M, Ewald U, Fellman V, Holmström G, Lindberg E, Lundqvist P, Maršál K, Norman M, Olhager E, Stigson L, Stjernqvist K, Vollmer B, Strömberg B, Group E (2013) Neurodevelopmental outcome in extremely preterm infants at 2.5 years after active perinatal care in Sweden. JAMA 309:1810–1820
Hirschberger RG, Kuban KCK, O’Shea TM, Joseph RM, Heeren T, Douglass LM, Stafstrom CE, Jara H, Frazier JA, Hirtz D, Rollins JV, Paneth N, Investigators ES (2018) Co-occurrence and severity of neurodevelopmental burden (cognitive impairment, cerebral palsy, autism spectrum disorder, and epilepsy) at age ten years in children born extremely preterm. Pediatr Neurol 79:45–52
García P, San Feliciano L, Benito F, García R, Guzmán J, Salas S, Fernández C, Prado Del N, Ciprián D, Figueras J (2013) SEN1500 hpa, 2013 Evolución a los 2 años de edad corregida de una cohorte de recién nacidos con peso inferior o igual a 1.500 g de los hospitales pertenecientes a la red neonatal SEN1500 [Outcome at two years corrected age of a cohort of very low birth weight infants from hospitals within the neonatal SEN1500 network] An Pediatr (Barc) 79:279–287
Duncan AF, Matthews MA (2018) Neurodevelopmental outcomes in early childhood. Clin Perinatol 45:377–392
Synnes A, Hicks M (2018) Neurodevelopmental outcomes of preterm children at school age and beyond. Clin Perinatol 45:393–408
Benavente-Fernández I, Ruiz-González E, Lubian-Gutiérrez M, Lubián-Fernández SP, Cabrales Fontela Y, Roca-Cornejo C, Olmo-Duran P, Lubián-López SP (2021) Ultrasonographic estimation of total brain volume: 3D reliability and 2D estimation. Enabling Routine Estimation During NICU Admission in the Preterm Infant. Front Pediatr 9:708396
Ruiz-Gonzalez E, Benavente-Fernandez I, Lubian-Gutierrez M, Segado-Arenas A, Zafra-Rodriguez P, Mendez-Abad P, Lubian-Lopez SP (2023) Ultrasonographic evaluation of the early brain growth pattern in very low birth weight infants. Pediatr Res
Kidokoro H, Neil JJ, Inder TE (2013) New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am J Neuroradiol 34:2208–2214
Linsell L, Malouf R, Morris J, Kurinczuk JJ, Marlow N (2015) Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight: a systematic review. JAMA Pediatr 169:1162–1172
Kidokoro H, Anderson PJ, Doyle LW, Woodward LJ, Neil JJ, Inder TE (2014) Brain injury and altered brain growth in preterm infants: predictors and prognosis. Pediatrics 134:e444-453
Li SJ, Tsao PN, Tu YK, Hsieh WS, Yao NJ, Wu YT, Jeng SF (2022) Cognitive and motor development in preterm children from 6 to 36 months of age: trajectories, risk factors and predictability. Early Hum Dev 172:105634
Eves R, Mendonca M, Baumann N, Ni Y, Darlow BA, Horwood J, Woodward LJ, Doyle LW, Cheong J, Anderson PJ, Bartmann P, Marlow N, Johnson S, Kajantie E, Hovi P, Nosarti C, Indredavik MS, Evensen KI, Raikkonen K, Heinonen K, Zeitlin J, Wolke D (2021) Association of very preterm birth or very low birth weight with intelligence in adulthood: an individual participant data meta-analysis. JAMA Pediatr 175:e211058
Eryigit Madzwamuse S, Baumann N, Jaekel J, Bartmann P, Wolke D (2015) Neuro-cognitive performance of very preterm or very low birth weight adults at 26 years. J Child Psychol Psychiatry 56:857–864
Taskila HL, Heikkinen M, Yliherva A, Valimaa T, Hallman M, Kaukola T, Kallankari H (2022) Antenatal and neonatal risk factors in very preterm children were associated with language difficulties at 9 years of age. Acta Paediatr 111:2100–2107
van Noort-van der Spek IL, Franken MC, Weisglas-Kuperus N, (2012) Language functions in preterm-born children: a systematic review and meta-analysis. Pediatrics 129:745–754
Kovachy VN, Adams JN, Tamaresis JS, Feldman HM (2015) Reading abilities in school-aged preterm children: a review and meta-analysis. Dev Med Child Neurol 57:410–419
Sentenac M, Johnson S, Charkaluk ML, Seppanen AV, Aden U, Cuttini M, Maier R, Mannamaa M, Zeitlin J, the Eg, (2020) Maternal education and language development at 2 years corrected age in children born very preterm: results from a European population-based cohort study. J Epidemiol Community Health 74:346–353
Ko G, Shah P, Lee SK, Asztalos E (2013) Impact of maternal education on cognitive and language scores at 18 to 24 months among extremely preterm neonates. Am J Perinatol 30:723–730
Linsell L, Malouf R, Morris J, Kurinczuk JJ, Marlow N (2016) Prognostic factors for cerebral palsy and motor impairment in children born very preterm or very low birthweight: a systematic review. Dev Med Child Neurol 58:554–569
Kato T, Mandai T, Iwatani S, Koda T, Nagasaka M, Fujita K, Kurokawa D, Yamana K, Nishida K, Taniguchi-Ikeda M, Tanimura K, Deguchi M, Yamada H, Iijima K, Morioka I (2016) Extremely preterm infants small for gestational age are at risk for motor impairment at 3 years corrected age. Brain Dev 38:188–195
El Rafei R, Jarreau PH, Norman M, Maier RF, Barros H, Van Reempts P, Pedersen P, Cuttini M, Costa R, Zemlin M, Draper ES, Zeitlin J, Group ER (2021) Association between postnatal growth and neurodevelopmental impairment by sex at 2 years of corrected age in a multi-national cohort of very preterm children. Clin Nutr 40:4948–4955
Arulkumaran S, Tusor N, Chew A, Falconer S, Kennea N, Nongena P, Hajnal JV, Counsell SJ, Rutherford MA, Edwards AD (2020) MRI findings at term-corrected age and neurodevelopmental outcomes in a large cohort of very preterm infants. AJNR Am J Neuroradiol 41:1509–1516
Brouwer MJ, Kersbergen KJ, van Kooij BJM, Benders M, van Haastert IC, Koopman-Esseboom C, Neil JJ, de Vries LS, Kidokoro H, Inder TE, Groenendaal F (2017) Preterm brain injury on term-equivalent age MRI in relation to perinatal factors and neurodevelopmental outcome at two years. PLoS ONE 12:e0177128
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE (2006) Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med 355:685–694
Van ’t Hooft J, van der Lee JH, Opmeer BC, Aarnoudse-Moens CS, Leenders AG, Mol BW, de Haan TR, (2015) Predicting developmental outcomes in premature infants by term equivalent MRI: systematic review and meta-analysis. Syst Rev 4:71
Cheong JL, Thompson DK, Spittle AJ, Potter CR, Walsh JM, Burnett AC, Lee KJ, Chen J, Beare R, Matthews LG, Hunt RW, Anderson PJ, Doyle LW (2016) Brain volumes at term-equivalent age are associated with 2-year neurodevelopment in moderate and late preterm children. J Pediatr 174(91–97):e91
Keunen K, Isgum I, van Kooij BJ, Anbeek P, van Haastert IC, Koopman-Esseboom C, Fieret-van Stam PC, Nievelstein RA, Viergever MA, de Vries LS, Groenendaal F, Benders MJ (2016) Brain volumes at term-equivalent age in preterm infants: imaging biomarkers for neurodevelopmental outcome through early school age. J Pediatr 172:88–95
Katusic A, Raguz M, Zunic Isasegi I (2020) Brain tissue volumes at term-equivalent age are associated with early motor behavior in very preterm infants. Int J Dev Neurosci
Lind A, Haataja L, Rautava L, Valiaho A, Lehtonen L, Lapinleimu H, Parkkola R, Korkman M, Group PS (2010) Relations between brain volumes, neuropsychological assessment and parental questionnaire in prematurely born children. Eur Child Adolesc Psychiatry 19:407–417
Liverani MC, Loukas S, Gui L, Pittet MP, Pereira M, Truttmann AC, Brunner P, Bickle-Graz M, Huppi PS, Meskaldji DE, Borradori-Tolsa C (2023) Behavioral outcome of very preterm children at 5 years of age: prognostic utility of brain tissue volumes at term-equivalent-age, perinatal, and environmental factors. Brain Behav 13:e2818
Soria-Pastor S, Padilla N, Zubiaurre-Elorza L, Ibarretxe-Bilbao N, Botet F, Costas-Moragas C, Falcon C, Bargallo N, Mercader JM, Junque C (2009) Decreased regional brain volume and cognitive impairment in preterm children at low risk. Pediatrics 124:e1161-1170
Arhan E, Gucuyener K, Soysal S, Salvarli S, Gurses MA, Serdaroglu A, Demir E, Ergenekon E, Turkyilmaz C, Onal E, Koc E, Atalay Y (2017) Regional brain volume reduction and cognitive outcomes in preterm children at low risk at 9 years of age. Childs Nerv Syst 33:1317–1326
Bolk J, Padilla N, Forsman L, Brostrom L, Hellgren K, Aden U (2018) Visual-motor integration and fine motor skills at 6½ years of age and associations with neonatal brain volumes in children born extremely preterm in Sweden: a population-based cohort study. BMJ Open 8:e020478
Kelly CE, Thompson DK, Spittle AJ, Chen J, Seal ML, Anderson PJ, Doyle LW, Cheong JL (2020) Regional brain volumes, microstructure and neurodevelopment in moderate-late preterm children. Arch Dis Child Fetal Neonatal Ed 105:593–599
Graca AM, Cardoso KR, da Costa JM, Cowan FM (2013) Cerebral volume at term age: comparison between preterm and term-born infants using cranial ultrasound. Early Hum Dev 89:643–648
Simsek GK, Canpolat FE, Buyuktiryaki M, Okman E, Keser M, Ustunyurt Z, Kutman HGK (2020) Developmental outcomes of very low birthweight infants with non-hemorrhagic ventricular dilatations and the relationships thereof with absolute brain volumes measured via two-dimensional ultrasonography. Childs Nerv Syst 36:1231–1237
Cuzzilla R, Cowan FM, Rogerson S, Anderson PJ, Doyle LW, Cheong JLY, Spittle A (2023) Relationships between early postnatal cranial ultrasonography linear measures and neurodevelopment at 2 years in infants born at <30 weeks’ gestational age without major brain injury. Arch Dis Child Fetal Neonatal Ed
Funding
Funding for open access publishing: Universidad de Cádiz/CBUA This study was funded by the Cadiz integrated territorial initiative for biomedical research European Regional Development Fund (ERDF) (2014–2020) and the Andalusian Ministry of Health and Families, Spain (PI-0052–2017 and ITI-0019–2019).
Author information
Authors and Affiliations
Contributions
Isabel Benavente Fernandez has played a fundamental role in the conception and design of the work, in the analysis and interpretation of the study data, in the editing of the manuscript, and in the approval of its final version. Simón P. Lubián López has played a fundamental role in the conception and design of the work, in the interpretation of the study data, and in the correction of the manuscript and approval of its final version. Manuel Lubián Gutiérrez has actively contributed to data acquisition and interpretation/measurement of images and has been involved in the approval of the final version of the manuscript. Antonio Segado Arenas, Pamela Zafra Rodríguez, and Paula Mendez Abad have actively contributed to data acquisition and medical assistance in the performance of MRI scans and have been involved in the approval of the final version of the document. Natalia Jiménez Luque and Yolanda Marín Almagro have actively contributed to the follow-up and psychological assessment of patients at two years of corrected age and to the updating of the database and registry of informed consents and have participated in the approval of the final version of the document.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Research and Ethics Committee of Puerta del Mar University Hospital.
Consent to participate
Informed consent was obtained from all participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ruiz-González, E., Lubián-López, S.P., Jiménez Luque, N. et al. Relationship of early brain growth pattern measured by ultrasound with neurological outcome at two years of age in very low birth weight infants. Eur J Pediatr 182, 5119–5129 (2023). https://doi.org/10.1007/s00431-023-05170-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05170-2