Abstract
To analyze the optimal lumbar puncture position in infants. A systematic review and meta-analysis. Infants (age < 1 year). December 2022 in PubMed, Scopus, and Web of Science. Randomized controlled trials focusing on lumbar puncture positions were included. Other lumbar puncture position than standard lateral decubitus position. First puncture success and overall success rate. Secondary outcome was desaturation during puncture and procedure-related harms. Risk of bias 2.0 assessment was performed. Outcomes are reported as risk ratios (RR) with 95% confidence intervals (CI). We screened 225 abstracts, and six studies were included. Four studies compared sitting position, one study head elevated lateral position, and one study prone position to lateral position. Risk of bias was high in two studies. First puncture success rate in sitting position (RR 1.00, CI: 0.78–1.18; 2 studies) and overall success rate in sitting position were similar to lateral position (RR 0.97, CI: 0.87–1.17; 3 studies). First attempt success rate was higher in elevated lateral position (RR 1.48, CI: 1.14–1.92; 1 study) and in prone position (RR 1.09, CI: 1.00–1.17; 1 study).
Conclusion: Sitting position seems to be equally effective in terms of first attempt and overall success in lumbar puncture than standard lateral position. Elevated lateral position and prone positions had better first attempt success than standard lateral position, but these were assessed only in one study each and thus further studies in these positions are needed.
Trial registration: This review was registered in PROSPERO. ID: CRD42022382953.
What is Known: • Success rate in lumbar puncture has been poor and first attempt success rate has varied between 50 to 80% in literature. • Optimal lumbar puncture positions for infants have been debated between sitting and lateral decubitus position mostly. | |
What is New: • This is the first meta-analysis focused on lumbar puncture positions in infants, and it found that sitting position was equal to standard lateral position. • Prone position and head elevated lateral positions had higher first puncture success rates, but these were assessed both only in one study, which creates uncertainty to the finding. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lumbar puncture is among the most common invasive procedures in children. Especially neonates and infants have high need for lumbar punctures due to the highest rates of bacterial meningitis, as for example the infant bacterial meningitis rate in the UK has been reported to be 0.4 per 1000 births [1, 2]. The first attempt success rate of lumbar puncture is low and has varied between 50 and 80% in previous studies [3,4,5]. The rates of traumatic lumbar puncture (classified as red blood cell count > 10,000/µl) are higher in neonates than in infants [6].
Optimal lumbar puncture position in infants and neonates has remained controversial. Few observational studies assessing the success rate between different positions have found that sitting position might have a higher success rate [7,8,9]. However, there are also reports with lower success rates in sitting position [10]. Other alternative positions have rarely been studied in infants. Furthermore, the optimal puncture position has been evaluated by ultrasound in terms of how the puncture space opens in sitting position compared to lateral position. In these studies, sitting position has seemed to offer the widest opening angle for lumbar puncture [11, 12]. However, the clinical first attempt success rate of ultrasound-marked puncture sites in randomized controlled trials has been relatively comparable to standard palpation method [3, 13, 14]. A recent large randomized controlled trial (RCT) found that sitting position was associated with better success rate than standard lateral position [15]. Thus, we wanted to update the current evidence on optimal lumbar puncture position in infants.
The aim of this systematic review with meta-analysis was to compare first attempt and overall puncture success rates between different lumbar puncture positions in infants.
Methods
Search process
We searched PubMed, Scopus, and Web of Science databases on December 4, 2022. The following search phrase was utilized: “lumbar puncture” AND position AND (infant OR neonate OR newborn OR child OR pediatric). Reference lists of the included studies were also hand searched, and relevant articles included, if found. Search results were then uploaded to Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia, 2022) for screening. Two authors independently screened the abstracts and the full texts. In cases of disagreement, a mutual consensus was searched by discussion.
Inclusion and exclusion criteria
We included randomized controlled studies that compared any other lumbar puncture position to standard lateral decubitus position. We classified infants as children aged 0 to 364 days. We excluded all observational studies. We excluded studies with older children if data were not presented separately for infants. Furthermore, non-English studies and studies that did not present any original data were excluded.
Outcome measures
Our main outcome measures were the rate of first attempt success and overall puncture success rate. In all analyses, alternative lumbar puncture positions were compared to standard lateral decubitus position. A lumbar puncture attempt is classified as needle perforating the skin. The definition for a successful puncture was that the fluid was clear and that red blood cell count was less than 10,000/µl. First attempt success rate is defined as obtaining successful cerebrospinal fluid sample with first puncture. Overall puncture success rate is defined as obtaining successful cerebrospinal fluid sample regardless of the number of attempts. Secondary outcomes were the rates of desaturation during the lumbar puncture and puncture-related adverse events.
Data extraction
The following data were extracted by one author and verified by the other author from each included study to a predesigned Excel worksheet: authors, journal, country, setting, main outcome(s), secondary outcome(s), number of participants in each group, number of successful punctures, number or first attempt successful punctures, overall number of punctures, and adverse events.
Risk of bias
Risk of bias was assessed according to Cochrane risk of bias 2.0 tool [16]. Risk of bias is presented for each individual study and as a summary plot per assessed domains. Figures were generated by robvis package [17].
Statistics
This review has been conducted according to the guidelines in the Cochrane handbook of systematic reviews [18]. Studies were pooled together in meta-analysis. Random-effects model was chosen due to expected heterogeneity between the studies. Risk ratios with 95% confidence intervals (CI) were calculated with Mantel–Haenszel test. Publication bias is analyzed for all analyses where at least five studies are included [19]. Review Manager version 5.4.1 was used in all statistical analyses.
Evidence quality for all outcomes was assessed by the Grading of Recommendations, Assessment, Development and Evaluations [20]. This study has been reported according to the preferred reporting items in systematic reviews and meta-analyses 2020 (PRISMA) guideline and the checklist is found in the supplementary materials [21].
Protocol registration
This protocol was registered to PROSPERO: ID CRD42022382953. It is available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022382953.
Results
Search
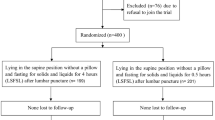
A total of 225 abstracts were screened. After further assessment of 22 full reports, 16 studies were excluded [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] and 6 studies included for systematic review and meta-analysis (Fig. 1) [15, 38,39,40,41,42]. All the six studies included were conducted in high-resource countries. Three studies were performed in neonatal intensive care units, two in operation rooms and one in an emergency department (Table 1). Interestingly, only one study reported the funding details and three studies had conflicts of interest statements (Table 1). In studies that reported the baseline characteristics, there were no substantial differences regarding age, weight, and gestational age of the infants (Table 2).
Risk of bias
Risk of bias was assessed to be high in two studies; one had some concerns and three studies had low risk of bias (Fig. 2). Most biases arise from the randomization process and bias due to outcome measurement (Fig. 2, Table 3).
First attempt success rate
Two studies [15, 38] with 1243 infants compared sitting position to lateral position (Fig. 3). The first attempt success rate was 62.3% in sitting position and 58.2% in lateral position (RR 1.00, CI 0.78–1.28, I2 70%). Evidence quality was ranked as moderate (Table 4). One study [40] with 116 infants compared elevated lateral position (table tilted up 45 degrees from the head side) to normal lateral position and the first attempt success rate was higher in elevated lateral position (50/58, 86.2%) than in standard lateral position (28/48, 58.3%), RR 1.48 (CI 1.14–1.92). Evidence quality was ranked as low (Table 4). One study [39] compared prone position to standard lateral position with 171 infants in neonatal intensive care unit. Prone position had higher first attempt success rate (70/82, 85.4%) than standard lateral position group success rate (57/89, 64.0%), RR 1.33 (1.11–1.60). Evidence quality was ranked as low.
Overall success rate
Three studies [38, 41, 42] with 223 infants compared the overall success rate between sitting and lateral position (Fig. 4). The overall success rate was 73.6% in sitting position and 78.8% in lateral position (RR 0.97, CI 0.87–1.09, I2 0%). Evidence quality was ranked as low. One study [39] with 171 infants compared prone position to lateral position. Overall success rate was 97.6% (80/82) in prone position and 89.9% (80/89) in lateral position, RR 1.09 (CI 1.00–1.17). Evidence quality was ranked as low.
Adverse events
Adverse events were reported heterogeneously between the studies (Table 3). One study reported that median lowest saturations were lower in the standard lateral position than in the sitting position [15] and another study reported longer durations of desaturation in lateral position [42]. Another study reported similar saturations in both groups [41]. Puncture-related adverse events were rare in all positions, as only one study reported a single case of puncture site hemorrhage (Table 3).
Discussion
We found in this systematic review low- and moderate-quality evidence that sitting position is equally effective as standard lateral position in terms of overall success and first attempt success in lumbar punctures performed to infants aged less than 12 months. In addition, we found low-quality evidence that elevated lateral position and prone position had higher first attempt success rates than standard lateral position, but these positions were analyzed only by one study each. All positions seemed to have low rates of adverse events and desaturation during the punctures.
We did not identify any previous meta-analysis on the positions during lumbar punctures in infants. Our search retrieved three non-randomized studies that were excluded from this meta-analysis. All of these three assessed sitting position in comparison to lateral position and found that the success rate in sitting position was higher than in the standard lateral position [7,8,9]. The systematic review by Hart et al. stated that the different positions seemed to be equally effective and better quality evidence is needed. However, the authors did not pool the results or conduct any critical appraisal [43].
The success rates in the included studies varied between 58.2 and 100%. This causes clear heterogeneity in the results. Three studies were conducted in neonatal intensive care units, and these had both the lowest and highest success rates [15, 39, 42]. The original studies did not control for the experience of the lumbar puncture performer in their analyses. Furthermore, operation room lumbar punctures were conducted by anesthesiologists, who typically use routinely lumbar punctures in their daily job while conducting neuraxial anesthesia [40, 41]. In the three studies that were carried out in the neonatal units, the puncture was performed by a pediatrician. One of the studies was conducted in the emergency department, where the setting is completely different from an operating room or neonatal intensive care unit, and the punctures were performed by pediatricians, family medicine doctors, or emergency medicine doctors [38].
One possible confounder to the results could have been the type of analgesia or procedural sedation used. Two of the included studies did not comment on the pain relief or sedation used [38, 42]. Two studies used non-nutritive sucking, topical analgesic cream/gel, and sucrose gel as analgesic [15, 39]. One study used topical analgesic cream/gel and midazolam [40], and one study used topical analgesia with nitric oxide inhalation [41]. Thus, all the included studies were conducted on awake patients, with typical non-medical and topical analgesic methods; this does not cause any notable issues to the pooling and synthesis of these studies.
Our main strength is that we did not have protocol deviations. Furthermore, we were able to perform a systematic synthesis of an important topic. Most limitations arise from the limited reporting of the original studies included in this review. Only three of the included studies were judged to have low risk of bias; thus, the reporting quality was limited. Due to the low number of included studies, we did not conduct sensitivity or publication bias analysis. Marshall et al. defined the success rate as first procedure and did not clearly specify the number of attempts, whereas Hanson et al. defined the first puncture success as first attempt success rate. Heterogeneity was a notable limiting factor as for example the study settings were differing (neonatal intensive care unit vs emergency department), and this likely increased the heterogeneity and decreases the validity of the results. Furthermore, the included studies had heterogenous reporting especially in adverse events. Therefore, we decided not to pool these together in meta-analysis. Due to these factors, the evidence quality remained either very low or low mostly.
Continuous research effort is needed to improve the success rates in lumbar punctures in infants. Further studies are needed to confirm the findings of all modified positions in relation to standard lateral positions before clear recommendations on the optimal position can be given. Ultrasound was believed to be a promising tool for help in lumbar punctures, but the success rates in randomized controlled trials have not been superior to standard methods in infants [44]. There are some reports on the use of bioimpedance needles that are able to detect the cerebrospinal fluid and could thus guide more precisely the optimal depth of the puncture. However, bioimpedance needles have yet not been assessed in randomized trials nor in infants [45].
Conclusion
We found low- to moderate-quality evidence that sitting position seems to be equally effective in terms of first attempt and overall success in lumbar puncture than standard lateral position. Elevated lateral position and prone positions had better first attempt success than standard lateral position, but these were assessed only in one study each and the evidence quality was low. Further studies on optimal lumbar puncture position are needed before concluding which should be the preferred position.
Data availability
All data generated during review process available upon request.
References
Dalai R, Dutta S, Pal A, Sundaram V, Jayashree M (2022) Is lumbar puncture avoidable in low-risk neonates with suspected sepsis? Am J Perinatol 39(1):99–105
Okike IO, Johnson AP, Henderson KL, Blackburn RM, Muller-Pebody B, Ladhani SN et al (2014) Incidence, etiology, and outcome of bacterial meningitis in infants aged <90 days in the United Kingdom and Republic of Ireland: prospective, enhanced, national population-based surveillance. Clin Infect Dis Off Publ Infect Dis Soc Am 59(10):e150-157
Grady M, Runyon M, Weekes A, Hogg M, Chaudoin L (2022) Comparison of ultrasound-marked versus standard lumbar puncture success in infants. Pediatr Emerg Care 38(1):e121–e125
Nigrovic LE, McQueen AA, Neuman MI (2007) Lumbar puncture success rate is not influenced by family-member presence. Pediatrics 120(4):e777-782
Nigrovic LE, Kuppermann N, Neuman MI (2007) Risk factors for traumatic or unsuccessful lumbar punctures in children. Ann Emerg Med 49(6):762–771
Sievänen H, Palmu S, Kari J, Soukka H, Lähteenmäki P, Eskola V (2022) Incidence of traumatic lumbar punctures in neonates and infants. Am J Perinatol
Bedetti L, Lugli L, Marrozzini L, Baraldi A, Leone F, Baroni L et al (2021) Safety and success of lumbar puncture in young infants: a prospective observational study. Front Pediatr 9:692652
Bhagat RP, Amlicke M, Steele F, Fishbein J, Kusulas M (2022) Retrospective study comparing success rates of lumbar puncture positions in infants. Am J Emerg Med 56:228–231
Hanson AL, Ros S, Soprano J (2014) Analysis of infant lumbar puncture success rates: sitting flexed versus lateral flexed positions. Pediatr Emerg Care 30(5):311–314
Glatstein MM, Zucker-Toledano M, Arik A, Scolnik D, Oren A, Reif S (2011) Incidence of traumatic lumbar puncture: experience of a large, tertiary care pediatric hospital. Clin Pediatr (Phila) 50(11):1005–1009
Abo A, Chen L, Johnston P, Santucci K (2010) Positioning for lumbar puncture in children evaluated by bedside ultrasound. Pediatrics 125(5):e1149-1153
Oulego-Erroz I, Mora-Matilla M, Alonso-Quintela P, Rodríguez-Blanco S, Mata-Zubillaga D, de Armentia SLL (2014) Ultrasound evaluation of lumbar spine anatomy in newborn infants: implications for optimal performance of lumbar puncture. J Pediatr 165(4):862-865.e1
Zummer J, Desjardins MP, Séguin J, Roy M, Gravel J (2021) Emergency physician performed ultrasound-assisted lumbar puncture in children: a randomized controlled trial. Am J Emerg Med 43:158–163
Kessler D, Pahalyants V, Kriger J, Behr G, Dayan P (2018) Preprocedural ultrasound for infant lumbar puncture: a randomized clinical trial. Acad Emerg Med Off J Soc Acad Emerg Med 25(9):1027–1034
Marshall ASJ, Scrivens A, Bell JL, Linsell L, Hardy P, Yong J et al (2022) Assessment of infant position and timing of stylet removal to improve lumbar puncture success in neonates (NeoCLEAR): an open-label, 2 × 2 factorial, randomised, controlled trial. Lancet Child Adolesc Health
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 28(366):l4898
McGuinness LA, Higgins JPT (2021) Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods 12(1):55–61
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page M et al (2022) Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, . [Internet]. Available from: Available from https://www.training.cochrane.org/handbook
Lin L, Chu H (2018) Quantifying publication bias in meta-analysis. Biometrics 74(3):785–794
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–94
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 29(372):n71
Baxter A, Welch J, Burke B (2004) Pain, position, and stylet styles: infant lumbar puncture practices of pediatric emergency attendings. Pediatr Res 55(4):123A-123A
Bedetti L, Lugli L, Marrozzini L, Baraldi A, Leone F, Baroni L et al (2021) Safety and success of lumbar puncture in young infants: a prospective observational study. Front Pediatr 9:692652
Bhagat RP, Amlicke M, Steele F, Fishbein J, Kusulas M (2022) Retrospective study comparing success rates of lumbar puncture positions in infants. Am J Emerg Med 56:228–231
Bouttefroy S, Savona M, Kebaili K, Goy F, Rivet C, Sautel-Debard B et al (2021) Use of a positioning inflatable cushion for children during lumbar puncture. Pediatr Blood Cancer 68:S329–S329
Duru C, Ederiane O, Allen-Ameri D, Ibrahim Z, Pondei K, Aliyu I (2017) Does hypoxemia occur before, during or after lumbar puncture procedure in ill newborns? Our experience in a tertiary health center. J Clin Neonatol 6(3):173–178
Ferdosian F, Fallah R, Dehghani Z (2020) Comparison of success rates in performing lumbar puncture and reduction of its anxiety and pain between standard sitting and lateral decubitus positions in 1 to 5-year-old children. Iran J Pediatr Hematol Oncol 10(3):173–178
Fiser DH, Gober GA, Smith CE, Jackson DC, Walker W (1993) Prevention of hypoxemia during lumbar puncture in infancy with preoxygenation. Pediatr Emerg Care 9(2):81–83
Glatstein MM, Zucker-Toledano M, Arik A, Scolnik D, Oren A, Reif S (2011) Incidence of traumatic lumbar puncture: experience of a large, tertiary care pediatric hospital. Clin Pediatr Phila 50(11):1005–1009
Hanson AL, Ros S, Soprano J (2014) Analysis of infant lumbar puncture success rates: sitting flexed versus lateral flexed positions. Pediatr Emerg Care 30(5):311–314
Hart C, Thompson A, Moriarty P (2016) Is the lateral decubitus position best for successful paediatric lumbar puncture? Arch Dis Child 101(8)
Marshall ASJ, Sadarangani M, Scrivens A, Williams R, Yong J, Bowler U et al (2020) Study protocol: NeoCLEAR: Neonatal Champagne Lumbar punctures Every time - An RCT: a multicentre, randomised controlled 2 × 2 factorial trial to investigate techniques to increase lumbar puncture success. BMC Pediatr 20(1):165
Matilla M, Quintela P, Blanco S, Erroz I, de Armentia S, Benavides M et al (2013) Performing a lumbar puncture in neonates: do we know the ideal position? Intensive Care Med 39:S89–S89
Molina A, Fons J (2006) Factors associated with lumbar puncture success [5]. Pediatrics 118(2):842–844
Naik V, Jin J, Tinsay A, Pricco N, Madhok M (2022) Medication use in the diagnostic pediatric lumbar puncture. Clin Pediatr Phila 99228221120687
Pinheiro JMB, Porter F, Miller JP, Cole FS, Marshall RE (1992) Position for lumbar punctures [1]. Pediatrics 89(5):976
Serrao KL, Serrao P, Marques R, Posada JC (1996) Optimal position during a lumbar puncture (LP): a randomized study in preterm newborns. J Invest Med [Internet] 44(1) Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-33749544554&partnerID=40&md5=f244a45f87178489714c9888724a96b1
Hanson AL, Schunk JE, Corneli HM, Soprano JV (2016) A randomized controlled trial of positioning for lumbar puncture in young infants. Pediatr Emerg Care 32(8):504–507
Guo W, Ma D, Qian M, Zhao X, Zhang J, Liu J et al (2022) Lumbar puncture in the prone position for low birth weight neonates. BMC Pediatr 22(1):2
Apiliogullari S, Duman A, Gok F, Ogun CO, Akillioglu I (2008) The effects of 45 degree head up tilt on the lumbar puncture success rate in children undergoing spinal anesthesia. Paediatr Anaesth 18(12):1178–1182
Vilà R, Lloret J, Munar F, Vinzo J (2002) Spinal anaesthesia for inguinal herniotomy in preterm infants sedated with nitrous oxide: a comparison of lumbar puncture in the lateral or sitting position. Anaesthesia 57(12):1164–1167
Weisman L, Merenstein G, Steenbarger J (1983) The effect of lumbar puncture position in sick neonates. Am J Dis Child 137(11):1077–1079
Hart C, Thompson A, Moriarty P (2016) QUESTION 2: Is the lateral decubitus position best for successful paediatric lumbar puncture? Arch Dis Child 101(8):774–777
Olowoyeye A, Fadahunsi O, Okudo J, Opaneye O, Okwundu C (2019) Ultrasound imaging versus palpation method for diagnostic lumbar puncture in neonates and infants: a systematic review and meta-analysis. BMJ Paediatr Open 3(1):e000412
Långström S, Huurre A, Kari J, Lohi O, Sievänen H, Palmu S (2022) Bioimpedance spinal needle provides high success and low complication rate in lumbar punctures of pediatric patients with acute lymphoblastic leukemia. Sci Rep 12(1):6799
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by IK and MR. The first draft of the manuscript was written by IK, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable to meta-analysis.
Consent to participate
Not applicable to meta-analysis.
Consent for publication
Not applicable to meta-analysis.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kuitunen, I., Renko, M. Lumbar puncture position in infants—a systematic review and meta-analysis. Eur J Pediatr 182, 4573–4581 (2023). https://doi.org/10.1007/s00431-023-05137-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05137-3