Abstract
This study aims to assess the impact of time of onset and features of early foetal growth restriction (FGR) with absent end-diastolic flow (AEDF) on pregnancy outcomes and on preterm infants’ clinical and neurodevelopmental outcomes up to 2 years corrected age. This is a retrospective, cohort study led at a level IV Obstetric and Neonatal Unit in Bologna, Italy. Pregnant women were eligible if having singleton pregnancies, with no major foetal anomaly detected, and diagnosed with early FGR + AEDF (defined as FGR + AEDF detected before 32 weeks gestation). Early FGR + AEDF was further classified according to time of onset and specific features into very early and persistent (VEP, FGR + AEDF first detected at 20–24 weeks gestation and persistent at the following scans), very early but transient (VET, FGR + AEDF detected at 20–24 weeks gestation and progressively improving at the following scans) and later (LA, FGR + AEDF detected between 25 and 32 weeks gestation). Pregnancy and neonatal outcomes and infant follow-up data were collected and compared among groups. Neurodevelopment was assessed using the revised Griffiths Mental Developmental Scales (GMDS-R) 0–2 years. A regression analysis was performed to identify early predictors of preterm infants’ neurodevelopmental impairment. Fifty-two pregnant women with an antenatal diagnosis of early FGR + AEDF were included in the study (16 VEP, 14 VET, 22 LA). Four intrauterine foetal deaths occurred, all in the VEP group (p = 0.010). Compared to LA infants, VEP infants were born with lower gestational age and lower birth weight, had lower arterial cord blood pH and were at higher risk for intraventricular haemorrhage and periventricular leukomalacia (p < 0.05 for all comparisons). At 12 months, VEP infants had worse GMDS-R scores, both in the general quotient (mean [SD] 91.8 [12.4] vs 104.6 [8.7] in LA) and in the performance domain (mean [SD] 93.3 [15.4] vs 108.8 [8.8] in LA). This latter difference persisted at 24 months (mean [SD] 68.3 [17.0] vs 92.9 [17.7] in LA). In multivariate analysis, at 12 months corrected age, PVL was found to be an independent predictor of impaired general quotient, while the features and timing of antenatal Doppler alterations predicted worse scores in the performance domain.
Conclusion: Timing of onset and features of early FGR + AEDF might impact differently on neonatal clinical and neurodevelopmental outcomes. Shared awareness of the importance of FGR + AEDF features between obstetricians and neonatologists may offer valuable tools for antenatal counselling and for tailoring pregnancy management and neonatal follow-up in light of specific antenatal and neonatal risk factors.
What is Known: • Foetal growth restriction (FGR), together with antenatal umbilical Doppler abnormalities, is known to affect maternal and neonatal outcomes. • Infants born preterm and growth-restricted face the highest risk for neurodevelopmental impairment, especially when FGR occurs early during pregnancy (early FGR, before 32 weeks gestation). | |
What is New: • The timing of onset and features of FGR and antenatal umbilical Doppler abnormalities impact differently on maternal and neonatal outcomes; when FGR and Doppler abnormalities occur very early, at the limit of neonatal viability, and persist until delivery, infants face the highest risk for neurodevelopmental impairment. • Shared knowledge between obstetricians and neonatologists about timing of onset and features of FGR would provide a valuable tool for informed antenatal counselling in high-risk pregnancies. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Several definitions of foetal growth restriction (FGR) have been proposed over time, but none is really comprehensive of all the different causes leading to FGR [1]. Uteroplacental insufficiency accounts for 25–30% of FGR cases and represents the single most frequent risk factor for FGR [2]. Since its earlier definition, a large number of studies have explored the features and outcomes of FGR, but only few of them have focused specifically on early FGR (FGR occurring before 32 weeks gestation [3]) and examined whether the time of onset and features of early FGR would have a differential impact on pregnancy and neonatal outcomes. It is known that uteroplacental insufficiency with absence of end-diastolic flow (AEDF) in the umbilical arteries detected prior to neonatal viability is associated with a high rate of perinatal deaths and neonatal complications [4]. As there is no feasible in-utero approach to reverse AEDF, the detection of uteroplacental insufficiency at the limit of neonatal viability issues significant challenges for antenatal counselling: in this specific case, antenatal counselling should encompass not only the pros and cons for maternal health but also the consequences, in the short and long term, of the birth of a preterm and growth-restricted infant. Actually, the effects of FGR expand beyond the neonatal period, as postulated in the “thrifty phenotype” hypothesis [5], and likely include a direct influence on neurodevelopment, leading to cognitive, motor, psychological or behavioural impairment [6,7,8,9,10], as well as an increase in the susceptibility to cardiovascular, metabolic, renal and hepatic diseases [11]. The detrimental effects of FGR on later outcomes are further worsened by prematurity, which is an independent predictor of neurological impairment [10], and by the concomitant evidence of severely impaired flow in the umbilical arteries [12].
At present, it has not been described whether early FGR along with AEDF occurring in the middle of the second trimester, around the limit of neonatal viability, would impact differently on pregnancy and neonatal outcomes compared to early FGR + AEDF occurring few weeks later [1]: thus, the aim of the present study was to specifically assess the impact of the timing of onset and features of early FGR + AEDF on pregnancy outcomes and on preterm infants’ clinical and neurodevelopmental outcomes up to 2 years corrected age (CA).
Materials and methods
Ethical approval
The study protocol was approved by the Independent Ethical Committee CE-AVEC, Bologna, Italy (study ID 112/2021/Oss/AOUBo). The study was conducted in conformity with the principles of the Helsinki Declaration. Eligible pregnant women provided written consent to participate to the study for themselves and for their children. Follow-up data for preterm infants were collected within a specific research protocol which had been approved by the same Ethical Committee (study ID EM 193-2018_76/2013/U/Sper/AOUBo).
Study inclusion criteria: maternal data
A retrospective, cohort study was conducted at a level IV [13, 14] Obstetric and Neonatal Unit in Bologna, Italy. FGR was defined as an absolute foetal size measurement below the 10th centile, in the absence of any congenital anomaly [1]. Pregnant women, having singleton pregnancies, with no major foetal anomaly detected prenatally and estimated foetal weight below 10th centile plus AEDF in the umbilical arteries were included in the study if FGR + AEDF was detected before 32 weeks gestation (early FGR).
As per internal clinical protocol, women diagnosed with early FGR were scheduled for fortnightly antenatal scans, with additional weekly scans in the presence of Doppler abnormalities.
Antenatal evaluations included amniotic fluid volume, foetal biometry and Doppler evaluation of the uterine arteries, umbilical artery, middle cerebral artery and ductus venosus. Amniocentesis was offered to all women diagnosed with FGR, regardless of the gestational week at first detection. When women required hospitalization, a cardiotocographic analysis was also performed. Major criteria for hospitalization were abnormal flow in the ductus venous after 25 weeks gestation, absent amniotic fluid, maternal uncontrolled blood pressure and/or preeclampsia. For each pregnancy, gestational age (GA) was calculated based on the first-trimester crown-rump length.
Ultrasonographic assessment was performed using a Voluson GE Healthcare System machine with a 3.5–5-MHz convex probe. Both umbilical arteries were sampled close to placental insertion, using an insonation angle lower than 30°, including within the sample volume the entire vessel [15].
For the study purpose, early FGR + AEDF was further defined according to GA at first detection: FGR + AEDF detected between 20 and 24 weeks gestation was defined as very early FGR + AEDF and classified according to persistence of the blood flow anomaly over time into persistent (VEP, AEDF first detected between 20 and 24 weeks gestation and persistent in later scans until delivery) and transient (VET, AEDF detected between 20 and 24 weeks gestation and progressively improving in the following scans until delivery). FGR + AEDF detected between 25 and 32 weeks gestation (later FGR, LA) served as control group.
Study inclusion criteria: infant data
Infants were included in the study if born very preterm (GA < 32 weeks) and/or having a birth weight (BW) below 1500 g. As per internal clinical protocol, all preterm infants with these characteristics born at the study centre were admitted to the study Neonatal Intensive Care Unit (NICU) and, following discharge from the NICU, enrolled in a developmental follow-up including periodic assessment of clinical conditions, growth and neurodevelopment up to 24 months CA.
Infants clinical and follow-up data were collected and compared among groups. Since birth, growth was measured using the Intergrowth 21st growth charts [16], which are the most updated standards for measuring postnatal growth in preterm infants from birth to 6 months CA. Since 6 month CA, growth was measured using the World Health Organization (WHO) Child Growth Standards for term newborns, as they overlap with the Intergrowth 21stst charts without the need for any adjustment [17]. Neurodevelopmental assessment was performed at 12 and 24 months CA using the revised Griffiths Mental Developmental Scales (GMDS-R) 0–2 years [18]. The scale evaluates five developmental domains: locomotor (LOC), personal–social (PS), hearing–language (H–L), eye and hand coordination (EH) and performance (PERF), yielding standardized subscale quotients and a general developmental quotient (GQ). GQ was calculated using the tables of standardized scores for the English infants’ population (mean 100.5, standard deviation—SD 11.8), because standardized data for the Italian population are not available. As in previous studies [19] and according to the normative data [18], children’s psychomotor development was defined as normal (GQ score ≥ 88.7), or mildly (GQ score 76.9–88.6), moderately (GQ score 66–76.8) and severely (GQ score ≤ 65) impaired.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics 28.0 (IBM Corp., Armonk, NY, USA). Data distribution was evaluated through the Kolmogorov–Smirnov test. Since all the follow-up data were distributed normally, parametric tests were used. Differences among the three groups were evaluated using one-way analysis of variance (ANOVA) for continuous data and chi-squared test or Fisher’s exact test—when appropriate—for categorical data. Post hoc comparisons were performed with Student’s t-test for continuous variables and Fisher’s exact test for categorical variables, using Bonferroni correction to control the family-wise error rate. Follow-up variables that proved to be significantly different among groups were used to build a set of linear regression models on neurodevelopmental outcomes in which the type of Doppler alteration was included as the independent variable and the neonatal variables which differed among groups as additional covariates. Potential collinearity between independent variables included in the regression models was checked using the Pearson correlation coefficient or the point-biserial correlation coefficient as appropriate. Correlation was defined as “strong” when correlation coefficients were above 0.6. A p value < 0.05 was considered statistically significant.
Results
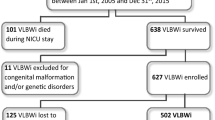
During the study period (January 2011 to December 2019), all eligible women (pregnant women with FGR + AEDF detected before 32 weeks gestation) were screened. Fifty-five patients fulfilled inclusion criteria: three were excluded from the study as one foetus was also diagnosed with Down syndrome, while two women were lost at follow-up.
Fifty-two pregnant women with a prenatal diagnosis of early FGR + AEDF, diagnosed as previously described, were included in the study (14 in the VET, 16 in the VEP and 22 in the LA group).
Maternal characteristics are reported in Table 1: most pregnant women were Caucasian, 3 were from Africa, and 6 were from Southeast Asia. More than half were primiparae; mean pre-pregnancy BMI was within normal ranges in all groups. No significant difference in maternal variables was detected among groups. As for antenatal scan data (Table 2), in the LA group, both GA and estimated foetal weight at diagnosis were significantly higher compared to both the VEP and the VET group. No significant difference in the examined antenatal scan parameters was detected apart from the ductus venosus α-wave before delivery, which was positive in a significantly larger proportion of infants in the LA group compared to the VEP group. Indications for delivery were significantly different among study groups, with preeclampsia being the most frequent reason for delivery in the LA group, and abnormal umbilical artery flow in the VEP group (Table 2). Amniocentesis was performed upon maternal consent in 27 cases. All obtained karyotypes were euploid.
Four intrauterine foetal deaths occurred (three at 27 weeks and one at 29 weeks gestation), all in the VEP group. In all cases, pregnant women were informed about potential benefits and risks of each treatment option and decided not to undergo an iatrogenic delivery, which had been proposed due to the worsening of foetal clinical conditions.
All the 48 infants born to the remaining pregnancies fulfilled the predefined inclusion criteria (GA < 32 weeks and/or BW < 1500 g) and were admitted to the study NICU. None of the infants had any major anomaly detected postnatally. Most infants were born small for gestational age (SGA, birth weight below 10° centile), with no significant differences among groups. Mean (standard deviation [SD]) BW was 789 (285) g and mean (SD) GA was 28.9 (2.1) weeks; infants in the VEP group had significantly lower BW (mean [SD] 636 [191] vs. 884 [273] g, respectively; p < 0.05) and GA (mean [SD] 27.6 [1.4] vs. 29.4 [1.9] g; p < 0.05) compared to infants in the LA group. Most mothers received a full course of antenatal steroidal prophylaxis (100% in the VET, 83.8% in the VEP and 90.9% in the LA group), with no significant difference among groups (p > 0.05). Magnesium sulphate prophylaxis was most likely in the LA group (52.3%, vs. 21.4% in the VET and 25% in the VEP group), but the difference with the other two groups was not significant (p > 0.05).
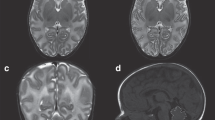
Arterial cord blood pH was significantly lower in infants belonging to the VEP group compared to those in the LA group (mean [SD] 7.16 [0.16] vs. 7.29 [0.09]; p < 0.05). A higher incidence of intraventricular haemorrhage (IVH) was detected in the VEP and VET groups compared with the LA group (29% and 25% vs. 0%), although comparisons failed to achieve statistical significance at post hoc evaluation. Similarly, periventricular leukomalacia (PVL) was higher in the VEP group (35%) as compared with both the VET and the LA group (no PVL cases in both groups), but post hoc evaluation did not reach statistical significance, probably due to small numbers. No difference in other clinical morbidities, length of hospital stay or growth parameters at hospital discharge was detected among groups (Table 3).
As for follow-up data (Table 4), at 12 months CA, infants in the VEP group had significantly lower weight centile (mean [SD] 3.6 [3.7]) compared to infants in the LA group (mean [SD] 25.6 [21.3]; overall comparison: p = 0.018; VEP vs. LA: p < 0.05). This difference did not persist at 24 months CA, and no difference in any other growth parameter was detected. Neurodevelopmental assessment through the GMDS-R showed that infants in the VEP group had a significantly lower GQ at 12 months CA compared to those in the LA group (mean [SD] 91.8 [12.4] vs. 104.6 [8.7]; overall comparison: p = 0.019; VEP vs. LA: p < 0.05); the evaluation of the five developmental domains which build up the GQ revealed that the most compromised domains in the VEP group, compared to the others, were the eye and hand coordination domain (mean [SD]: VEP 93.0 [22.7], VET 91.2 [13.6], LA 109.7 [12.9]; overall comparison: p = 0.025, between-group comparison: non-significant) and the performance domain (mean [SD]: VEP 93.3 [15.4], VET 94.3 [13.9], LA 108.8 [8.6]; overall comparison: p = 0.008, VEP vs. LA: p < 0.05). At 24 months CA, the difference in the performance domain between the two groups persisted (mean [SD]: VEP 68.3 [17.0], VET 78.7 [21.2], LA 92.9 [17.76]; overall comparison: p = 0.024, VEP vs. LA: p < 0.05), despite no difference in GQ.
Different linear regression models were built up to evaluate the effect of prenatal and neonatal characteristics on each neurodevelopmental outcome which was significantly different among groups (GQ at 12 months CA and performance at both 12 and 24 months CA, Table 5). Collinearity assessment revealed that the only two variables showing a strong correlation were GA and BW (r = 0.788, p = 0.000); thus, BW was not included, leaving GA, together with arterial cord blood pH, IVH and PVL as the type of Doppler alteration, as covariates to be included into each model.
As shown in Table 5, having PVL was significantly associated with a lower GQ at 12 months PMA (p = 0.039). In addition, Doppler features proved to be an independent predictor of the performance domain at 12 months CA (p = 0.011). None of the examined variables proved to be independently associated with the performance domain at 24 months CA in the multivariate analysis.
Discussion
According to the results of the present study, the timing of onset and course of Doppler alteration, together with relevant neurological morbidities such as PVL, might impact significantly on neonatal outcomes, both during NICU stay and follow-up, in early FGR associated with AEDF. Specifically, infants born to mothers with a diagnosis of early FGR + AEDF detected between 20- and 24 weeks gestation and persistent up to delivery face the highest risk of prematurity-related complications, as they are delivered at lower GAs and with lower BWs compared to infants with early FGR + AEDF detected between 25 and 32 weeks gestation. Furthermore, they are usually born in poorer condition, as documented by the lower arterial cord blood pH, experience more serious neurological complications, including IVH and PVL, in the neonatal period, and have a higher risk for poor growth and impaired neurodevelopment during the first 2 years of life. To note, also infants born to mothers with very early, but transient, AEDF seem to experience a higher risk of neurodevelopmental impairment, even if limited to the performance domain.
Several studies have documented a link between both FGR and SGA status and increased foetal and neonatal mortality and morbidity [20, 21]. In addition, recent systematic reviews and meta-analyses [8,9,10] have emphasized the high risk of neurodevelopmental impairment in infants with FGR or SGA. In most cases, foetuses with severe FGR are delivered preterm, and this further worsens the risk for adverse outcome. According to the results of the present study, infants with very early and persistent FGR + AEDF face the highest risk of growth and neurodevelopmental impairment and thus should be monitored carefully during both the neonatal period and early childhood. The performance domain, which examines cognitive functions for planning and completing intentional actions and representing objects mentally, appears to be specifically affected, suggesting that close attention should be paid to these functions during infants’ follow-up.
Differences in neurodevelopmental outcomes according to the timing of onset of early FGR + AEDF might be related to a different impact of FGR on the foetus according to the gestational stage in which it occurs; it has been described in animal models that FGR influences brain growth and brain structure, including altered neuronal arborization and reduced number of pre-oligodendrocytes [22]. Furthermore, following FGR, a redistribution of the foetal circulation can occur, in order to maintain an adequate cerebral perfusion (a phenomenon known as “brain sparing”) [23]. Some studies have described a link between brain sparing and adverse perinatal and postnatal outcomes, including neurodevelopment [24, 25], with a direct relationship with the severity of the alteration in the cerebroplacental ratio [26]. Brain sparing is thought to occur regionally rather than globally throughout the brain [23], and this might partly explain the selective impact of FGR associated with AEDF on neurodevelopmental domains. In the present study, no difference in terms of indices of brain sparing was detected among groups, but this result might be linked to the relatively small sample size and deserves further evaluation. Shared information about prenatal indices of brain sparing between obstetricians and neonatologists would add valuable information for antenatal counselling and might improve early neonatal clinical management.
The major point for shared antenatal counselling between obstetricians and neonatologists, when called to counsel couples with early FGR + AEDF detected around the limit of neonatal viability, is that the information provided may trigger a very important decision for the family, leading to different attitudes towards pregnancy continuation or termination. During an antenatal counselling following a diagnosis of very early FGR + AEDF, sharing with the couple evidence-based information about potential maternal and neonatal complications according to timing of onset and features of FGR + AEDF empowers clinicians’ explanation with details that can make the difference in the decision process.
Furthermore, the finding that preeclampsia is the most frequent complication that brings to deliver foetuses in the LA group is important for obstetricians who, in this way, are aware about which patients should be followed carefully with strict laboratory protocols [27].
At present, there is still a lack of potential therapeutic options to prevent neurological impairment following FGR [28]. The knowledge that, among early FGR + AEDF infants, those with FGR + AEDF occurring very early and persisting until delivery face the highest risk for adverse outcomes should prompt further research aimed at discovering biomarkers for identification of uteroplacental insufficiency at its onset; this may deepen our understanding of the complex pathogenetic landscape of FGR, to target potentially reversible or treatable mechanisms of disease (i.e., neuroinflammation). In addition, neonatal research should focus on improving the diagnostic ability of continuous neuromonitoring in the NICU, especially when an infant with early and severe FGR is born extremely preterm.
The strength of the present study relies on the highly selected population, which includes only infants facing the highest risk for severe neonatal and childhood complications (preterm infants who experienced, as foetuses, FGR with AEDF occurring before 32 weeks gestation). The classification according to the timing of onset and features of FGR + AEDF might constitute an additional strength, as it allows to identify these two factors as critical for the following clinical outcome.
As for study limitations, the relatively small sample size and the loss of significance of the AEDF features in the multivariate analysis investigating predictors of GQ at 12 months CA do not allow a thorough generalization of the study results but prompt further research in the same selected population to confirm the actual findings.
Conclusions
According to the results of the present study, pregnant women with FGR + AEDF detected very early and persisting through pregnancy face the highest risk for intrauterine foetal death. Preterm infants born to these mothers are born at lower GAs and with lower BWs and have higher risk for neurological complications during early life, including IVH and PVL. Furthermore, during the first 2 years of life, these infants might experience worse neurodevelopmental outcomes and poorer growth. The present study provides specific data about growth and neurodevelopment in preterm infants born following early FGR + AEDF during the first 2 years of life, thus offering valuable information for counselling pregnant women who experience this condition.
Data availability
The data that support the findings of this study are available on request from the corresponding author, AA.
Abbreviations
- AEDF:
-
Absence of end-diastolic flow
- BW:
-
Birth weight
- CA:
-
Corrected age
- EH:
-
Eye–hand coordination (developmental domain)
- FGR:
-
Foetal growth restriction
- GA:
-
Gestational age
- GMDS-R:
-
Griffiths Mental Developmental Scales
- GQ:
-
General developmental quotient
- H–L:
-
Hearing–language (developmental domain)
- IVH:
-
Intraventricular haemorrhage
- LA:
-
Later AEDF + FGR
- LOC:
-
Locomotor (developmental domain)
- PERF:
-
Performance (developmental domain)
- PS:
-
Personal–social (developmental domain)
- PVL:
-
Periventricular leukomalacia
- SD:
-
Standard deviation
- SGA:
-
Small for gestational age (foetus or infant)
- VEP:
-
Very early and persistent AEDF + FGR
- VET:
-
Very early but transient AEDF + FGR
References
Gordijn SJ, Beune IM, Thilaganathan B et al (2016) Consensus definition of fetal growth restriction: a Delphi procedure. Ultrasound Obstet Gynecol 48:333–339. https://doi.org/10.1002/uog.15884
Martins JG, Biggio JR, Abuhamad A (2020) Society for Maternal-Fetal Medicine Consult Series #52: diagnosis and management of fetal growth restriction: (Replaces Clinical Guideline Number 3, April 2012). Am J Obstet Gynecol 223:B2–B17. https://doi.org/10.1016/j.ajog.2020.05.010
Baschat AA, Cosmi E, Bilardo CM et al (2007) Predictors of neonatal outcome in early-onset placental dysfunction. Obstet Gynecol 109:253–261
Simonazzi G, Curti A, Cattani L et al (2013) Outcome of severe placental insufficiency with abnormal umbilical artery Doppler prior to fetal viability. BJOG An Int J Obstet Gynaecol 120:754–757. https://doi.org/10.1111/1471-0528.12133
Bar J, Weiner E, Levy M, Gilboa Y (2021) The thrifty phenotype hypothesis: the association between ultrasound and Doppler studies in fetal growth restriction and the development of adult disease. Am J Obstet Gynecol MFM 3:100473. https://doi.org/10.1016/j.ajogmf.2021.100473
Korzeniewski SJ, Allred EN, Joseph RM et al (2017) Neurodevelopment at age 10 years of children born <28 weeks with fetal growth restriction. Pediatrics 140:e20170697. https://doi.org/10.1542/peds.2017-0697
Delorme P, Kayem G, Lorthe E et al (2020) Neurodevelopment at 2 years and umbilical artery Doppler in cases of very preterm birth after prenatal hypertensive disorder or suspected fetal growth restriction: EPIPAGE-2 prospective population-based cohort study. Ultrasound Obstet Gynecol 56:557–565. https://doi.org/10.1002/uog.22025
Sacchi C, Marino C, Nosarti C et al (2020) Association of intrauterine growth restriction and small for gestational age status with childhood cognitive outcomes: a systematic review and meta-analysis. JAMA Pediatr 174:772–781. https://doi.org/10.1001/jamapediatrics.2020.1097
Levine TA, Grunau RE, McAuliffe FM et al (2015) Early childhood neurodevelopment after intrauterine growth restriction: a systematic review. Pediatrics 135:126–141. https://doi.org/10.1542/peds.2014-1143
Murray E, Fernandes M, Fazel M et al (2015) Differential effect of intrauterine growth restriction on childhood neurodevelopment: a systematic review. BJOG An Int J Obstet Gynaecol 122:1062–1072. https://doi.org/10.1111/1471-0528.13435
Armengaud JB, Yzydorczyk C, Siddeek B et al (2021) Intrauterine growth restriction: clinical consequences on health and disease at adulthood. Reprod Toxicol 99:168–176. https://doi.org/10.1016/j.reprotox.2020.10.005
Unterscheider J, Daly S, Geary MP et al (2013) Optimizing the definition of intrauterine growth restriction: the multicenter prospective PORTO study. Am J Obstet Gynecol 208:290.e1-290.e6. https://doi.org/10.1016/j.ajog.2013.02.007
The American College of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine (2019) Obstetric Care Consensus. Levels of maternal care
Stark AR, Pursley DM, Papille L-A et al (2023) Standards for levels of neonatal care: II, III, and IV. Pediatrics 151:e2023061957
Bhide A, Acharya G, Baschat A et al (2021) ISUOG Practice Guidelines (updated): use of Doppler velocimetry in obstetrics. Ultrasound Obstet Gynecol 58:331–339. https://doi.org/10.1002/uog.23698
The Global Health Network INTERGROWTH 21st - Standards and Tools
Villar J, Giuliani F, Barros F et al (2018) Monitoring the postnatal growth of preterm infants: a paradigm change. Pediatrics 141:e20172467. https://doi.org/10.1542/peds.2017-2467
Griffiths R (1996) The Griffiths Mental Development Scales from Birth to Two Years, Manual; Association for Research in Infant and Child Development
Gibertoni D, Corvaglia L, Vandini S et al (2015) Positive effect of human milk feeding during NICU hospitalization on 24 month neurodevelopment of very low birth weight infants: an Italian cohort study. PLoS One 10:e0116552. https://doi.org/10.1371/journal.pone.0116552
Lees C, Marlow N, Arabin B et al (2013) Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet Gynecol 42:400–408. https://doi.org/10.1002/uog.13190
Unterscheider J, O’Donoghue K, Daly S et al (2014) Fetal growth restriction and the risk of perinatal mortality-case studies from the multicentre PORTO study. BMC Pregnancy Childbirth 14:2–7. https://doi.org/10.1186/1471-2393-14-63
Pla L, Illa M, Loreiro C et al (2020) Structural brain changes during the neonatal period in a rabbit model of intrauterine growth restriction. Dev Neurosci 42:217–229
Cohen E, Baerts W, Van Bel F (2015) Brain-sparing in intrauterine growth restriction: considerations for the neonatologist. Neonatology 108:269–276. https://doi.org/10.1159/000438451
Flood K, Unterscheider J, Daly S et al (2014) The role of brain sparing in the prediction of adverse outcomes in intrauterine growth restriction: results of the multicenter PORTO Study. Am J Obstet Gynecol 211:288.e1-288.e5. https://doi.org/10.1016/j.ajog.2014.05.008
Monteith C, Flood K, Pinnamaneni R et al (2019) An abnormal cerebroplacental ratio (CPR) is predictive of early childhood delayed neurodevelopment in the setting of fetal growth restriction. Am J Obstet Gynecol 221:273.e1-273.e9. https://doi.org/10.1016/j.ajog.2019.06.026
Stampalija T, Arabin B, Wolf H et al (2017) Is middle cerebral artery Doppler related to neonatal and 2-year infant outcome in early fetal growth restriction? Am J Obstet Gynecol 216:521.e1-521.e13. https://doi.org/10.1016/j.ajog.2017.01.001
ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia (2019) Obstet Gynecol 133(1):1. https://doi.org/10.1097/AOG.0000000000003018
Fleiss B, Wong F, Brownfoot F et al (2019) Knowledge gaps and emerging research areas in intrauterine growth restriction-associated brain injury. Front Endocrinol (Lausanne) 10:1–24. https://doi.org/10.3389/fendo.2019.00188
Acknowledgements
The authors would like to gratefully thank Dr Silvia Savini, who performed preterm infants’ neurodevelopmental assessments.
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
A.A., A.N.D.G. and G.S. conceptualized the study; S.F.S., S.M., M.Z., A.Se. and C.D. performed data collection; A.A., A.N.D.G., S.M. and J.L. analysed data; L.C., A.Sa. and G.P. supervised data collection, analysis and interpretation. A.A., A.N.D.G. and G.S. wrote the first draft of the paper, which was critically revised by all the authors.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in conformity with the principles of the Helsinki Declaration. The study was approved by the Independent Ethical Committee CE-AVEC, Bologna, Italy (study ID 112/2021/Oss/AOUBo and EM 193-2018_76/2013/U/Sper/AOUBo).
Consent to participate
Eligible pregnant women provided written consent to participate to the study for themselves and for their child.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Della Gatta, A.N., Aceti, A., Spinedi, S.F. et al. Neurodevelopmental outcomes of very preterm infants born following early foetal growth restriction with absent end-diastolic umbilical flow. Eur J Pediatr 182, 4467–4476 (2023). https://doi.org/10.1007/s00431-023-05104-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05104-y