Abstract
This study aims to provide practical recommendations on prophylaxis for infection in pediatric patients with immune-mediated rheumatic diseases receiving/scheduled to receive immunosuppressive therapy. A qualitative approach was applied. A narrative literature review was performed via Medline. Primary searches were conducted using MeSH terms and free text to identify articles that analyzed data on infections and vaccinations in pediatric patients with immune-mediated rheumatic diseases receiving immunosuppressive therapy. The results were presented and discussed in a nominal group meeting comprising a committee of 12 pediatric rheumatologists from the Prevention and Treatment of Infections Working Group of the Spanish Society of Pediatric Rheumatology. Several recommendations were generated. A consensus procedure was implemented via a Delphi process that was extended to members of the Spanish Society of Pediatric Rheumatology and the Vaccine Advisory Committee of the Spanish Association of Pediatrics. Participants produced a score ranging from 0 (completely disagree) to 10 (completely agree). Agreement was considered to have been reached if at least 70% of participants voted ≥ 7. The literature review included more than 400 articles. Overall, 63 recommendations were generated (23 on infection prophylaxis) and voted by 59 pediatric rheumatologists and other pediatric specialists, all of whom achieved the pre-established level of agreement. The recommendations on prophylaxis of infection cover vaccination and prophylaxis against varicella zoster virus, tuberculosis, Pneumocystis jiroveccii, and invasive fungal infections in pediatric patients with immune-mediated rheumatic diseases receiving/scheduled to receive immunosuppressive therapy.
Conclusion: Based on current evidence and a Delphi process, we provided consensus and updated recommendations on prophylaxis and treatment of infections to guide those caring for pediatric rheumatology patients.
What is Known: |
•Data largely derived from adults find that infectious diseases and related complications are a major cause of morbidity and mortality in patients with immune-mediated rheumatic diseases. |
•It is crucial to be aware of the preventive measures that should be implemented to prevent these infections in children, although most guidelines are often extrapolated from adult cases. |
What is New: |
•In the absence of evidence, a literature review and a Delphi survey were conducted to establish a series of expert recommendations that could prove useful in clinical practice, providing a practical and simple day-to-day approach to be used by pediatric rheumatologists. |
•The recommendations focus on tuberculosis, herpes zoster virus, fungal infections, and Pneumocystis jirovecii. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious diseases and related complications are a major cause of morbidity and mortality in adult patients with immune-mediated rheumatic diseases. The increased risk of infection in this population may be related to several factors, including the immune effects of the disease itself, use of immunosuppressive drugs, comorbidities, medical/surgical procedures, as well as frequent visits to the clinic [1].
Like adults, pediatric patients with immune-mediated rheumatic diseases could be at a higher risk of infection than healthy children because of their underlying condition [2]. With current intensive treatment strategies incorporating the early use of immunosuppressive therapies such as biological drugs, high-dose glucocorticoids, and Janus kinase inhibitors, susceptibility to infections, including opportunistic infections, increases [3]. In addition, the fact that children receive many vaccinations during the first years of life could reduce the immunogenicity of vaccinations because of the patients’ immunosuppressed status, thereby further increasing the risk of infection [2]. Consequently, prophylaxis for infection in patients with immune-mediated rheumatic diseases, especially with immunosuppressive treatment, is essential.
The lack of published trials in the immunocompromised pediatric population means that pediatricians do not have comprehensive, up-to-date guidelines. Therefore, we designed this project to generate practical recommendations on screening, prophylaxis, and vaccination against infection in pediatric patients with immune-mediated rheumatic diseases receiving/scheduled to receive immunosuppressive therapy. The recommendations on screening were recently published (4). This article describes the current evidence and relevant recommendations generated on prophylaxis of infection (vaccination, herpes zoster virus, tuberculosis, fungal infections, and Pneumocystis jirovecii) in this population. We are confident this guide will help physicians resolve questions that may arise in day-to-day practice, thereby improving pediatric care and outcomes.
Methods
This qualitative study was based on a comprehensive narrative literature review, the experience of an expert committee, and the consensus achieved by pediatric rheumatologists. The project was carried out following the ethical principles of the Declaration of Helsinki for medical research involving human subjects and in accordance with the stipulations of Good Clinical Practice.
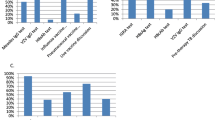
A narrative literature review was performed via Medline. Primary searches were conducted using MeSH terms and free text to identify articles that analyzed data on infections and vaccinations in pediatric patients with immune-mediated rheumatic diseases receiving immunosuppressive therapy. The results were presented and discussed in a nominal group meeting comprising a committee of 12 pediatric rheumatologists from the Prevention and Treatment of Infections Working Group of the Spanish Society of Pediatric Rheumatology. Several recommendations were generated. A consensus procedure was implemented via a Delphi process that was extended to members of the Spanish Society of Pediatric Rheumatology and the Vaccine Advisory Committee of the Spanish Association of Pediatrics. Participants produced a score ranging from 0 (completely disagree) to 10 (completely agree). Agreement was considered to have been reached if at least 70% of participants voted ≥ 7. With the assistance of a methodologist, each recommendation was assigned a level of evidence (LE) and grade of recommendation (GR) according to the recommendations of the Oxford Center for Evidence-Based Medicine [5].
A more detailed description of the process can be found [4]. In this article, the results refer to 23 recommendations that cover vaccination and prophylaxis against varicella zoster virus, tuberculosis, Pneumocystis jiroveccii, and invasive fungal infections in pediatric patients with immune-mediated rheumatic diseases receiving/scheduled to receive immunosuppressive therapy.
Results
Vaccination
The recommendations generated in this consensus document, as well as the Delphi process results, are depicted in Table 1. A total of 59 experts participated in the Delphi process (response rate, 64%), 45 from SERPE and 14 from SEIP.
Recommendation 1
Triple viral vaccination (measles, mumps, rubella (MMR)) is recommended, whenever possible, at least 2–4 weeks before starting immunosuppressive treatment (LE IIIb; GR D; LA 98%).
Children with rheumatic diseases, especially those receiving immunosuppressive treatment, are more susceptible to infections; therefore, it is important to update the vaccination schedule according to national vaccination guidelines. Because immunogenicity may be reduced by immunosuppressive treatments, usual practice and current consensus-based guidelines recommend waiting at least 2–4 weeks before starting these treatments after vaccination with live attenuated vaccines [2].
Booster vaccination against MMR is currently administered in patients receiving methotrexate < 15 mg/m2/week or low-dose corticosteroids. However, live attenuated vaccine is not recommended during disease flares or in patients taking high-dose corticosteroids (≥ 2 mg/kg or ≥ 20 mg/day for 2 weeks) or high doses of csDMARDs or bDMARDs. Nevertheless, recent data showed that booster MMR vaccine in patients with juvenile idiopathic arthritis receiving bDMARDs (anti-TNFα, anti-IL-1, or anti-IL-6) is safe and immunogenic, with no patients developing a disease flare [6, 7]. Therefore, vaccination can be considered on a case-to-case basis, weighing the risk of infections against the risk of inducing infection [8].
Recommendation 2
If serology testing for varicella zoster virus is negative, varicella vaccination is recommended, whenever possible, 2–4 weeks before starting immunosuppressive treatment (LE IIIb; GR D; LA 100%).
It is recommended to record varicella zoster virus (VZV) infection and vaccination history in children with rheumatic diseases, especially in those patients anticipating high-dose csDMARDS or bDMARDs. In cases of a negative history of infection or vaccination and a negative serology result during screening, VZV vaccine should be administered, at least 2–4 weeks before initiation of immunosuppressive therapy [2].
As VZV vaccine is a live attenuated vaccine, like MMR, the recommendations are similar to those described in the previous section. Increasing evidence from small case series shows that not only booster, but also primary VZV vaccination can be safe in children receiving treatments such as methotrexate, corticosteroids, and even bDMARDS (anti-TNF, anti-IL6) [9, 10].
Recommendation 3
Children 6 months or older with rheumatic diseases should be vaccinated against influenza during the flu season, especially if they are receiving immunosuppressive treatment. Vaccination of the entire family is recommended (LE IIIb; GR D; LA 98%).
Influenza vaccination combined with non-pharmacological measures continues to be the fundamental approach for preventing influenza today. The Vaccine Advisory Committee of the Spanish Association of Pediatrics recommends annual influenza vaccination in all chronically ill or immunosuppressed patients and their cohabiting family members provided they are over 6 months of age. Two doses separated by 4 weeks are administered in children under 9 years old who are being vaccinated for the first time the first year, and 1 dose if they are older than this age. In the following years, only 1 dose is needed each season.
The preparations currently marketed and approved for children are inactivated vaccines for intramuscular or subcutaneous administration (0.5 ml). At present, the most widely used preparations are the inactivated trivalent vaccines. However, the trend is towards the use of tetravalent preparations to optimize the effectiveness of influenza vaccination in the most vulnerable population [11]. An attenuated vaccine is currently marketed for intranasal administration (0.2 ml), although is contraindicated in immunocompromised patients.
Influenza vaccination in people receiving immunosuppressants may be less effective depending on the treatment administered [12,13,14,15]. Although the quality of the evidence is low, prophylaxis with oseltamivir for 10 days may be considered in immunosuppressed children at high risk of the complications of influenza, especially if unvaccinated, after close contact with a person infected by influenza virus [16].
Varicella zoster
Recommendation 4
Prophylactic treatment for chickenpox is recommended after contact with a person with varicella zoster infection in children with rheumatic diseases receiving medium- and high-risk immunosuppressive treatments who do not have a previous history of chickenpox or herpes zoster, vaccination, or evidence of immunity confirmed by serology testing (LE IIIb; GR D; LA 91%).
Regarding VZV infection, the risk of immunosuppressive drugs can be classified as low, intermediate (individuals who should be able to develop and maintain adequate antibodies from a previous infection or vaccination), and high (if they have not been able to develop or maintain immunity, since these may have been lost through immunosuppressive treatment) (Table 2) [17].
An algorithm for the management of reported contact with VZV in an immunosuppressed patient is presented in Fig. 1. In low-risk patients, no action should be taken after contact with a patient with chickenpox, because the risk of serious disease caused by the medication is assumed to be low.
Algorithm for managing an immunosuppressed patient after contact with varicella zoster virus. aFace to face or > 15 min in same room with any patient with chickenpox or exposed lesions (e.g., herpes zoster ophthalmicus) or contact with an immunosuppressed patient with covered zoster; bSee Table 2; cIf checking serology, do not delay treatment beyond 7 days post contact; It should be noted that serology might be unreliable dHistory of chickenpox or shingles or varicella/shingles vaccination or prior serological evidence of immunity; eVZV immunoglobulin is not frequently available (adapted from Cates M, Rheumatology 2018).f If VZIG and IVIG are unavailable, contraindicated or a patient prefers not to receive a blood-derived product, acyclovir or vancyclovir could be used
In intermediate-risk patients with a history of varicella or herpes zoster, prior VZV vaccination, or evidence of immunity by prior serology, no action should be taken. If this is not the case, serology testing should be performed. If this is negative, start treatment for exposure to chickenpox. Serology results should be available as early as possible, preferably before 7 days after exposure.
In all patients in the high-risk group, serology testing should be performed regardless of prior immunization status, vaccination, or positive serology after contact with chickenpox. This is because patients receiving immunosuppressive treatments in this group can reduce VZV-specific antibody titers to non-protective levels. This recommendation is based on expert opinion since the impact of specific immunosuppressants on VZV-specific humoral and cellular immunity is unknown [18, 19].
Recommendation 5
Prophylaxis with varicella zoster immunoglobulin or intravenous nons-pecific immunoglobulin within 10 days (preferably within 7 days) after exposure is recommended in patients considered at high risk of severe opportunistic disease (LE IIIb; GR D; LA 93%).
Administration of VZV immunoglobulin (VZIG) or intravenous non-specific immunoglobulin (IVIG) is recommended as soon as possible within 10 days (preferably within 7 days) after exposure to VZV in patients considered to be at high risk of severe disease (Fig. 1). VZIG is administered intramuscularly at 125 units/10 kg (maximum of 625 units) or according to the following dosage: 0–5 years, 250 mg; 6–10 years, 500 mg; 11–14 years, 750 mg; > 15 years, 1000 mg [17]. However, there are countries where this option is not available. Non-specific immunoglobulin is administered intravenously at 200 mg/kg.
For those seronegative contacts for whom VZIG is not indicated and/or those for whom prophylaxis with a non-blood product is preferred, oral acyclovir at 10 mg/kg 4 times a day (maximum dose of 3200 mg) or valacyclovir at 20 mg/kg 3 times a day (maximum dose 3000 mg) from days 7 to 14 after exposure can be considered. It should be noted that there is a risk of nephrotoxicity if cyclosporine is co-administered with acyclovir or valacyclovir. Acyclovir is excreted by the same tubular system as mycophenolate, although its co-administration does not produce a clinically significant change in levels in patients with normal renal function [20]. One small study has suggested an added benefit of acyclovir with VZIG compared with VZIG alone in children with renal disease taking steroids, however, in severely immunocompromised patients could be considered [19].
Tuberculosis
Recommendation 6
In the event of close contact with a person with active tuberculosis, the tuberculin skin test (TST) and interferon-gamma release assay (IGRA) should be performed, as should a chest X-ray (LE IIIb; GR D; LA 100%).
A risk contact for tuberculosis is considered one that has occurred during the previous 3 months, with close contact (> 4 h daily in the same room) with confirmed smear-positive tuberculosis (pulmonary, laryngeal, tracheal, or endobronchial). In these cases, a TST and IGRA should be performed to detect latent tuberculosis infection (LTBI) or tuberculosis [21].
Both the TST and the IGRA depend on cell-mediated immunity and provide immunologic evidence of host sensitization to antigens of Mycobacterium tuberculosis. Neither method can distinguish between latent tuberculosis infection and tuberculosis, and both methods display suboptimal performance in immunocompromised patients, who are at greatest risk for progression of LTBI to TB [22]. Long-term treatment with corticosteroids (more than 7.5 mg prednisone equivalent) and other immunosuppressive drugs can significantly affect the performance of the IGRA, including sensitivity and indeterminate results, probably due to corticosteroid-induced lymphopenia or the impaired function of T cells and antigen-presenting cells [23].
Performing both the TST and the IGRA maximizes the sensitivity of the results in children of any age with suspected tuberculosis, although it is mandatory in children under biological therapy (especially TNF-α antagonists) when the initial and repeat IGRA results are indeterminate or invalid, when the initial test results (TST or IGRA) are negative but there is a high clinical suspicion of TB, and when an initial TST result is positive in children previously vaccinated against BCG [22, 24].
It is necessary to rule out TB by asking about compatible clinical signs and symptoms and, if present, by performing a chest X-ray (anteroposterior and lateral) [21]. Importantly, tuberculosis is often asymptomatic, and the physical findings of childhood tuberculosis are usually few and non-specific in mild and moderate forms of the disease. Computed tomography (CT) is more sensitive than plain radiographs, but its routine use is not recommended. Nevertheless, it is useful in children with inconclusive radiographic findings, symptomatic patients with normal radiographic features, and if the diagnosis is uncertain in at-risk groups [25].
Recommendation 7
We recommend interrupting contact between the exposed child and the patient with tuberculosis for at least 2 weeks or until the adult no longer harbours the bacterium (LE IIIb; GR D; LA 98%).
It is recommended that the patient with tuberculosis be kept in isolation in an independent room at home while starting treatment. Isolation should be maintained at least until it is verified that the adult with tuberculosis is not harboring the bacterium (usually estimated after at least 2 weeks of adequate treatment) [21].
Recommendation 8
If it is considered that there is a risk of exposure to tuberculosis and the TST and IGRA are negative, chemoprophylaxis for LTBI will be administered for 2 months (8–10 weeks) (LE IIIb; GR D; LA 91%).
Even with a negative TST and IGRA result after a risk contact for tuberculosis, especially in children with risk factors for false-negative/indeterminate TST/IGRA results, such as those younger than 5 years of age or those receiving immunosuppressive therapy, treatment should be started for possible LTBI (window or primary chemoprophylaxis). Primary chemoprophylaxis is usually administered with daily isoniazid (H) (Table 3) [21].
TST or IGRA should be repeated after 8 to 10 weeks. If the results are still negative, chemoprophylaxis can be discontinued. If the TST or IGRA result becomes positive, active disease will be ruled out again and the regimen for LTBI should be completed [22]. In immunocompromised children, full treatment of LTBI is recommended, owing to the possible absence of TST reactivity and indeterminate/invalid results of IGRA, even if repeated TST or IGRA at 8 weeks are negative [21].
Recommendation 9
In the event of a positive TST or IGRA result, a simple posterior-anterior and lateral chest X-ray should be performed (if not previously done) (LE IIIb; GR D; LA 100%).
TB must be ruled out in the event of a positive TST or IGRA result by a thorough physical examination and a posterior-anterior and lateral chest X-ray. In the presence of radiological or clinical findings, additional diagnostic procedures (induced sputum or gastric juice aspiration depending on age) should be performed to confirm pulmonary and/or extrapulmonary tuberculosis. When choosing the treatment regimen, the risk of developing drug-resistant tuberculosis while on monotherapy with isoniazid or rifampin should be considered [22].
Recommendation 10
If the IGRA and/or TST results are positive and tuberculosis is ruled out, latent tuberculosis infection (LTBI) should be suspected, and appropriate treatment administered (LE IIIb; GR D; LA 93%).
LTBI is suspected in asymptomatic patients with a normal chest X-ray and positive TST and/or IGRA findings and a known contact with a tuberculosis patient harboring the bacterium. However, in clinical practice, children with no known risk contact for tuberculosis but with a positive TST and/or IGRA result should also be considered as having LTBI, especially if they are under 5 years of age or immunosuppressed. In the absence of a known contact or risk factors and a history of BCG vaccination, a positive TST result with a negative IGRA result is interpreted as an effect of BCG. These cases are not considered LTBI [21].
All children and adolescents diagnosed with LTBI should receive treatment as soon as possible to prevent tuberculosis.
Recommendation 11
Latent tuberculosis infection should be treated with any of the following treatment regimens:
-
Isoniazid (H) for 6–9 months (6H or 9H).
-
Isoniazid and rifampicin (R) for 3 months (3HR) or in children older than 12 years, isoniazid and rifapentine once weekly for 3 months (3HP). Directly observed therapy may be offered in intermittent treatment for improving adherence.
-
Rifampicin for 4 months (4R) (LE IIIb; GR D; LA 89%).
The treatment regimens for LTBI are described in Table 3. It should be noted that these regimens have not been specifically tested in immunocompromised patients. Adherence to medication regimens for LTBI can be improved with directly observed therapy or administration of medications by a health care professional or trained third party who observes and reports that the patient takes each dose of medication.
Isoniazid monotherapy (6H or 9H) is the most widely recommended and used treatment for LTBI, with an efficacy of 98% against tuberculosis. However, the long duration of this therapy (usually up to 9 months in immunocompromised patients) results in poor adherence and low completion rates. Therefore, it is only recommended when a rifampicin-containing regimen cannot be used.
Treatment regimens that combine isoniazid and rifampicin (3HR) or rifapentine 3HP have comparable or better efficacy than isoniazid in monotherapy, although they are associated with higher completion rates. 3HP is associated with good tolerance and low toxicity and is especially recommended in adolescents or when poor adherence is suspected.
The 4-month regimen of daily rifampicin (4R) has similar efficacy to 9 months of isoniazid, although the shorter period is associated with a significantly higher rate of completion. It is indicated in patients with toxicity or contraindications to isoniazid, or when strains of Mycobacterium tuberculosis resistant to isoniazid (and sensitive to rifampicin) are present [22, 26].
Due to the low risk of hepatotoxicity in children, routine transaminase monitoring is not recommended during LTBI treatment, except in the case of hepatotoxicity, underlying liver disease, or concomitant hepatotoxic medication. In immigrants from countries endemic for viral hepatitis or HIV, both diseases should be ruled out before starting treatment [21]. It is not necessary to repeat chest X-ray after completion. TST/IGRA remain positive and should not be repeated either [22].
The recommended duration of LTBI treatment before starting immunosuppressive therapy is not well established, although most authors suggest that, whenever possible, patients should receive at least 1 month of treatment for tuberculosis before starting immunosuppressive therapy.
Recommendation 12
An infectious disease specialist should be consulted for the management of patients with rheumatic disease and tuberculosis (exposure/infection/disease) (LE IIIb; GR D; LA 98%).
A specialist in infectious diseases should be consulted when test results are difficult to interpret. When TST or IGRA is positive, the specialist should collaborate in the early reporting of cases to the public health authorities [22]. An infection caused by a strain of Mycobacterium tuberculosis that is resistant to isoniazid and rifampicin (or to other antituberculosis drugs) requires an individual approach based on the exact drug resistance pattern. These cases should also be managed in consultation with a specialist with expertise in managing pediatric tuberculosis [27].
Fungal infections
Recommendation 13
In non-endemic areas, it is not necessary to take specific preventive measures against fungi before starting immunosuppressive treatment (LE IIIb; GR D; LA 91%).
The risk of opportunistic and endemic invasive fungal diseases (IFD) appears to depend on the underlying condition, the concomitant administration of corticosteroids and immunosuppressants, and geographic exposure. The recommendation to perform serology testing for Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis prior to starting immunosuppressive treatment would only be indicated in patients from endemic areas (Sub-Saharan Africa, Latin America, Southeast Asia) [28, 29].
Recommendation 14
In the case of travel to areas that are endemic for Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis, avoid risk activities (cave exploration, bird’s nest cleaning) (LE IIIb; GR D; LA 91%).
To avoid possible IFD in children with immunosuppressive treatment, risk activities such as cave exploration or nest cleaning should be avoided if travelling to areas that are endemic for Histoplasma capsulatum, Blastomyces dermatitidis, and Coccidioides immitis (Sub-Saharan Africa, Latin America, Southeast Asia) [28, 29].
Recommendation 15
Primary antifungal prophylaxis with oral posaconazole could be considered in patients with severe neutropenia (< 500 cells/µL) for more than 1 week (LE IIIb; GR D; LA 80%).
In patients with hematologic malignancies, primary antifungal prophylaxis with oral posaconazole is used in patients with severe neutropenia (< 500 cells/µL) lasting more than 1 week. The dose used is 200 mg every 8 h in children over 13 years of age. The alternative to posaconazole would be voriconazole administered orally (9 mg/kg/12 h in < 50 kg, 4 mg/kg/12 h in > 50 kg) or intravenously (8 mg/kg/12 h in < 50 kg, 4 mg/kg/12 h in > 50 kg). In the case of contraindication or adverse effects with azoles, liposomal amphotericin B or intravenous micafungin could be considered [30].
Although IFD is very rare in rheumatic diseases, isolated cases have been described in adults with rheumatoid arthritis and systemic lupus erythematosus (SLE) [31,32,33]. In patients with prolonged neutropenia that may be caused by immunosuppressive treatment or by high disease activity, primary fungal prophylaxis could also be considered. However, this is one of the recommendations that achieved the lowest degree of agreement among the experts. In cases of suspected or documented IFD, a high index of clinical suspicion and prompt initiation of appropriate antifungal therapy are probably better tools for controlling morbidity and mortality from IFD in immunocompromised children.
Neutropenia secondary to tocilizumab has been reported, although it has not been associated with the development of bacterial or fungal infections [34].
Pneumocystis pneumonia
Recommendation 16
Consider prophylaxis against Pneumocystis jirovecii pneumonia (PJP) in the following cases: systemic vasculitis (granulomatosis with polyangiitis, polyarteritis nodosa), idiopathic inflammatory myopathies, and associated interstitial lung disease. It should also be considered in patients receiving sustained immunosuppressive treatment that combines high doses of corticosteroids and an immunosuppressant or 2 associated immunosuppressive drugs (LE IIIb; GR D; LA 87%).
Pneumocystis jirovecii is a ubiquitous fungus that can cause pneumonia (PJP) in immunocompromised individuals, such as children with human immunodeficiency virus (HIV) infection, children with cancer, organ transplant recipients, and children with underlying autoimmune rheumatic diseases [35]. The overall incidence of PCP in patients with autoimmune rheumatic diseases remains relatively low, and PCP is usually the result of the simultaneous combination of several risk factors, such as immunosuppressive treatment, lymphopenia, and interstitial lung disease. However, when PCP occurs, morbidity and mortality are usually high [36,37,38].
The rheumatic disease with the highest risk for PJP is granulomatosis with polyangiitis (GPA), although it has also been reported in polyarteritis nodosa, idiopathic inflammatory myopathies (dermatomyositis, polymyositis), and autoimmune disease with associated interstitial lung disease. PJP prophylaxis should also be considered in any patient with an autoimmune disease in whom treatment is expected to be long-term. This should take the form of high doses of prednisone combined with an immunosuppressive agent (mainly cyclophosphamide, methotrexate, TNF-α antagonists, and rituximab) or 2 immunosuppressive agents combined [39, 40].
In these cases, PJP prophylaxis has been reported to be effective and safe [37, 41]. A recent study has shown the variability of PJP prophylaxis in patients who have risk conditions or take high-risk immunosuppressants, with up to 25% not receiving prophylaxis. However, the rates of PJP reported are low (2.2%), and the probability of adverse effects of prophylaxis necessitates a more personalized risk assessment before prescribing PJP prophylaxis [42].
Recommendation 17
Consider prophylaxis against Pneumocystis jirovecii pneumonia (PJP) in patients receiving long-term high-dose corticosteroids (LE IIIb; GR D; LA 96%).
The main risk factor for the development of PJP is treatment with high-dose corticosteroids over long periods, such as prednisone > 0.4 mg/kg/day (or > 30 mg/day) for more than 4 weeks or > 0.2 mg/kg (or 15 mg/day) for more than 8 weeks [39, 43]. However, in a retrospective cohort that included 119,399 children who had received at least 2 prescriptions for a systemic corticosteroid within a 60-day period (cancer, transplant, and HIV were excluded), it was observed that the incidence of PJP was low (0.61 and 0.53/10,000 patient-years between children exposed and not exposed to PJP prophylaxis, respectively). Although favorable in adults with rheumatic diseases [37], the risk–benefit ratio of TMP/SMX prophylaxis in children treated with corticosteroids has been debated, given the possible incidence of adverse effects (e.g., skin reactions and myelosuppression) reported with this compound and the low incidence of PJP [36, 44].
PJP prophylaxis should be discontinued when prednisone doses reach < 15 mg/day, provided that no other associated risk factors remain (immunosuppressive agents combined, low total and CD4 + lymphocyte counts) [39, 43].
Recommendation 18
Prophylaxis for PJP is recommended in patients receiving cyclophosphamide to induce remission of ANCA-associated vasculitis (LE IIIa; GR C; LA 91%).
Although it can appear years after initiation of treatment, PJP has been more frequently reported in patients with GPA during therapy to induce remission [45, 46]. However, it has not been routinely indicated in randomized trials but rather was optional or suggested, depending on the decision of the researcher. Some authors recommend prophylaxis when the CD4 count is below 250/mm3 or 300/mm3. In other studies, prophylaxis was prescribed to all participants [47, 48]. To standardize management, EULAR guidelines routinely encourage the prescription of PJP prophylaxis in the early phase of induction therapy with cyclophosphamide in ANCA-associated vasculitis [49].
Recommendation 19
Pneumocystis jirovecii prophylaxis in patients treated with rituximab might be considered in those receiving concomitant immunosuppressive therapy, including prednisone > 20 mg/day or equivalent dose for at least 4 weeks (LE IIIb; GR C; LA 91%).
Rituximab is associated with the development of PJP in patients with autoimmune diseases, such as rheumatoid arthritis [50], GPA [51], and systemic lupus erythematosus [52], although it is much less frequent than in patients with lymphoproliferative diseases. PCP usually occurs within 3–6 months of the last rituximab infusion, although it could also occur up to 32 months after the last treatment, both in monotherapy and in combination with other immunosuppressive drugs [39, 53].
The indication for prophylaxis in patients with autoimmune diseases treated with rituximab must be individualized and should be considered, especially if patients receive corticosteroids at > 20 mg/day [54] or if other risk factors for PJP are present (old age, kidney or lung involvement, previous infections due to T cell–mediated immune dysfunction, lymphocytopenia, and low CD4 cell counts) [51, 53]. PJP prophylaxis could be limited to 6 months after rituximab infusion if no other immunosuppressive drugs are prescribed [54].
Recommendation 20
Prophylaxis for Pneumocystis jirovecii pneumonia in patients treated with TNF-α antagonists might be considered in the presence of 2 or more of the following risk factors: high-dose corticosteroids, concomitant chronic lung disease, persistent lymphopenia, hypoalbuminemia, and hypogammaglobulinemia (LE IIIa; GR D; LA 85%).
Although PCP has been reported in adult patients treated with TNF-α antagonists, its incidence is usually low, ranging from < 0.01/1000 person-years in the USA to 8.8/1000 person-years in Japan, and routine PJP prophylaxis may not be beneficial [55]. In reported cases, in addition to older age, 2 or more of the following risk factors were present: high-dose corticosteroids, persistent lymphopenia, concomitant lung disease, hypoalbuminemia, and hypogammaglobulinemia [56,57,58]. Although the evidence is only available from studies in adult population, the presence of several of these risk factors could be considered to individualize the need for prophylaxis.
Recommendation 21
The total lymphocyte count (< 500 cells/mm3) will be taken into consideration before initiation of prophylaxis for Pneumocystis jirovecii pneumonia (LE IIIb; GR D; LA 70%).
Lymphopenia and a low CD4 + cell count have been consistently reported as risk factors for PCP, and several studies have addressed the recommendation of PJP prophylaxis in non-HIV-infected patients based on total lymphocyte and/or CD4 + lymphocyte count. The limits usually considered for PJP prophylaxis are a lymphocyte count of < 500/mm3 and CD4 cell count of < 200/mm3 [31, 59, 60], although PCP may also occur at higher counts. In fact, the value of lymphocyte and CD4 counts in establishing the need for prophylaxis in patients with autoimmune diseases has been questioned, and more than 600 lymphocytes/mm3 and more than 300 CD4/mm3 [61]. These limits may be more useful in other types of non-HIV-infected patients, such as those with lymphoproliferative diseases or transplant recipients, than in those with autoimmune disease.
Nevertheless, in a survey of rheumatologists’ practice for prescribing PJP prophylaxis, only 15% of respondents considered peripheral lymphocyte counts and 7.5% monitored CD4 cell counts [62].
Recommendation 22
The drug of choice for prophylaxis if Pneumocystis jirovecii pneumonia is trimethoprim-sulfamethoxazole at 5 mg/kg/day of trimethoprim, 3 days a week (on consecutive or alternate days) (LE IIb; GR B; LA 100%).
Trimethoprim-sulfamethoxazole is the preferred agent for PJP prophylaxis (Table 4). Although several dosing regimens are used, administration 3 times a week is the most common since it is as effective as daily administration [63, 64]. In addition to its activity against Pneumocystis jirovecii, trimethoprim-sulfamethoxazole also confers protection against many bacterial infections and toxoplasmosis. The most common adverse reaction is rash, which may be severe (e.g., Stevens-Johnson syndrome and toxic epidermal necrolysis). In these cases, TMP-SMX should be permanently discontinued [35].
Recommendation 23
For patients unable to tolerate trimethoprim-sulfamethoxazole, other prophylactic strategies include dapsone, atovaquone, and aerosolized pentamidine (LE IIIb; GR D; LA 100%).
In the case of adverse effects or intolerance to trimethoprim-sulfamethoxazole, the drug of choice for prophylaxis would be atovaquone [65]. Other options include nebulized pentamidine, provided that it can be administered under biosafety conditions, and dapsone, depending on the adverse effect profile (Table 4) [35]. It is advisable to reconsider the need for prophylaxis before starting it.
Discussion
Based on the best available evidence and consensus of experts, we present a series of recommendations concerning common and rare scenarios in the prophylaxis of infection for patients with immune-mediated rheumatic diseases receiving immunosuppressive treatment.
Our review showed that the level of evidence is very low for most scenarios. Therefore, several recommendations were based on expert opinion.
The recommendations are intended to assist specialists involved in the care of these patients in their routine clinical practice. The availability of explicit recommendations related to common situations with immunosuppressive treatments could prove helpful in daily practice.
We would like to mention here some specific recommendations that were not included in the Delphi.
-
Pneumococcal vaccination with PCV10 or PCV13 is recommended in all non-vaccinated pediatric patients with autoimmune/inflammatory rheumatic diseases. The immunogenicity and safety of PCVs have also been shown in these patients. The question remains whether should additionally receive a booster vaccination with the PPSV-23 in addition to the PCV10/13 vaccination. The EULAR Task Force decided after an intense discussion, that a 5-yearly PPSV-23 is not recommended as standard of care but can be considered in immunosuppressed patients and SLE patients. The taskforce recommends avoiding the PPSV-23 in cryopyrin-associated periodic syndrome due to safety reasons [ 66].
-
Meningococcal vaccination: Meningococcal C (MenC) conjugate vaccination was shown to be immunogenic and safe in patients with rheumatic diseases. The MenACWY conjugate vaccine was immunogenic in most inflammatory disease patients, but seroprotection was lower in patients using anti-TNF agents. Therefore, an extra booster MenACWY vaccination should be considered [ 67].
-
SARS-CoV2 vaccination: no patients had a significant increase in disease activity after vaccination, and the commonest side effects (localized pain and fatigue) were mild with no serious adverse events, with similar frequency in patients and controls. Most patients become seropositive after two doses of the vaccine; however, antibody titres are significantly lower than healthy controls; hence, the recommendation that patients on immunosuppression receive an additional dose of vaccine as part of the primary course. Current studies provide support for the current clinical practice of offering the BNT162b2 vaccine to children or adolescents with rheumatic diseases without stopping their immunosuppression [ 68].
References
Furer V, Rondaan C, Heijstek M, Van Assen S, Bijl M, Agmon-Levin N et al (2019) Incidence and prevalence of vaccine preventable infections in adult patients with autoimmune inflammatory rheumatic diseases (AIIRD): a systemic literature review informing the 2019 update of the EULAR recommendations for vaccination in adult patients with AIIRD. RMD Open 5(2)
Heijstek MW, Ott De Bruin LM, Bijl M, Borrow R, Van Der Klis F, Koné-Paut I et al (2011) EULAR recommendations for vaccination in paediatric patients with rheumatic diseases. Ann Rheum Dis 70(10):1704–12
Thiele F, Klein A, Windschall D, Hospach A, Foeldvari I, Minden K et al (2021) Comparative risk of infections among real-world users of biologics for juvenile idiopathic arthritis: data from the German BIKER registry. Rheumatol Int 41(4):751–762
Cuadros E, Calzada-Hernández J, Clemente D, Martín S, Silveira L, Lirola-Cruz M et al (2022) Position statement of the Spanish Society of Pediatric Rheumatology on infection screening, prophylaxis, and vaccination of pediatric patients with rheumatic diseases and immunosuppressive therapies: Part 1 (screening). Eur J Pediatr 181(6):2343–2354
CEBM Medicine (2011) CfEB: CEBM levels of evidence 2011. http://www.cebm.net/index.aspx?o=1025. Accessed 11 Apr 2013
Uziel Y, Moshe V, Onozo B, Kulcsár A, Tróbert-Sipos D, Akikusa JD et al (2020) Live attenuated MMR/V booster vaccines in children with rheumatic diseases on immunosuppressive therapy are safe: multicenter, retrospective data collection. Vaccine 38(9):2198–2201
Tse HN, Borrow R, Arkwright PD (2020) Immune response and safety of viral vaccines in children with autoimmune diseases on immune modulatory drug therapy. Expert Rev Vaccines 19:1115–27. Taylor and Francis Ltd
Blanchard-Rohner G (2021) Vaccination in children with autoimmune disorders and treated with various immunosuppressive regimens: a comprehensive review and practical guide. Front Immunol 12(711637)
Pileggi GS, De Souza CBS, Ferriani VPL (2010) Safety and immunogenicity of varicella vaccine in patients with juvenile rheumatic diseases receiving methotrexate and corticosteroids. Arthritis Care Res (Hoboken) 62(7):1034–1039
Groot N, Pileggi G, Sandoval CB, Grein I, Berbers G, Ferriani VPL et al (2017) Varicella vaccination elicits a humoral and cellular response in children with rheumatic diseases using immune suppressive treatment. Vaccine 35(21):2818–2822
José Álvarez García F, José M, Ortega C, Aldeán JÁ, Garcés-Sánchez M, Llanos EG et al (2022) Immunization schedule of the Pediatric Spanish Association: 2022 recommendations. An Pediatr (Engl Ed) 96:1–59
França ILA, Ribeiro ACM, Aikawa NE, Saad CGS, Moraes JCB, Goldstein-schainberg C et al (2012) TNF blockers show distinct patterns of immune response to the pandemic influenza a H1N1 vaccine in inflammatory arthritis patients. Rheumatology (Oxford) 51(11):2091–2098
Gelinck LBS, Van Der Bijl AE, Beyer WEP, Visser LG, Huizinga TWJ, Van Hogezand RA et al (2008) The effect of anti-tumour necrosis factor α treatment on the antibody response to influenza vaccination. Ann Rheum Dis 67(5):713–716
Eisenberg RA, Jawad AF, Boyer J, Maurer K, McDonald K, Prak ETL et al (2013) Rituximab-treated patients have a poor response to influenza vaccination. J Clin Immunol 33(2):388–396
Tsuru T, Terao K, Murakami M, Matsutani T, Suzaki M, Amamoto T et al (2014) Immune response to influenza vaccine and pneumococcal polysaccharide vaccine under IL-6 signal inhibition therapy with tocilizumab. Mod Rheumatol 24(3):511–516
Tagarro A, Cruz-Cañete M, Otheo E, Launes C, Couceiro JA, Pérez C et al (2019) Oseltamivir for the treatment of influenza in children and adolescents. An Pediatr (Engl Ed) 90(5):317.e1-317.e8
Public Health England. Guidance for issuing varicella-zoster immunoglobulin (VZIG).https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/811544/VZIG_issuing_guidance.pdf.
Cates M, Donati M, Gillet S, Ustianowski A, Galloway J (2018) Comment on: managing varicella zoster virus contact and infection in patients on anti-rheumatic therapy. Rheumatology (Oxford) 57(4):768
Cates M, Donati M, Gillet S, Ustianowski A, Galloway J (2018) Managing varicella zoster virus contact and infection in patients on anti-rheumatic therapy. Rheumatology (Oxford) 57(4):596–605
Gimenez F, Foeillet E, Bourdon O, Weller S, Garret C, Bidault R et al (2004) Evaluation of pharmacokinetic interactions after oral administration of mycophenolate mofetil and valaciclovir or aciclovir to healthy subjects. Clin Pharmacokinet 43(10):685–692
Baquero-Artigao F, del Rosal T, Falcón-Neyra L, Ferreras-Antolín L, Gómez-Pastrana D, Hernanz-Lobo A et al (2023) Update on the diagnosis and treatment of tuberculosis. Anales de Pediatría (English Edition) 98(6):460–9. Available from https://linkinghub.elsevier.com/retrieve/pii/S2341287923001084
Nolt D, Starke JR (2021) Tuberculosis infection in children and adolescents: testing and treatment. Pediatrics 148(6)
Yang Y, Wang HJ, Hu WL, Bai GN, Hua CZ (2022) Diagnostic value of interferon-gamma release assays for tuberculosis in the immunocompromised population. Diagnostics (Basel) 12(2)
Lewinsohn DM, Leonard MK, Lobue PA, Cohn DL, Daley CL, Desmond E et al (2017) Official American thoracic society/Infectious diseases society of America/Centers for disease control and prevention clinical practice guidelines: diagnosis of tuberculosis in adults and children. Clin Infect Dis 64(2):111–115
Moreno-Pérez D, Andrés Martín A, Altet Gómez N, Baquero-Artigao F, Escribano Montaner A, Gómez-Paístrana Durán D et al (2010) Diagnosis of tuberculosis in paediatrics. An Pediatr (Engl Ed) 72:283.e1–283.e14
Júnior JCL, Ramos RTT, Robazzi TCMV (2017) Treatment of latent tuberculosis in patients with juvenile rheumatic diseases: a systematic review. Rev Bras Reumatol Engl Ed 57(3):245–253
Nahid P, Mase SR, Migliori GB, Sotgiu G, Bothamley GH, Brozek JL et al (2019) Treatment of drug-resistant tuberculosis an official ATS/CDC/ERS/IDSA clinical practice guideline. Am J Respir Crit Care Med 200(10):E93-142
Tragiannidis A, Kyriakidis I, Zündorf I, Groll AH (2017) Invasive fungal infections in pediatric patients treated with tumor necrosis alpha (TNF-α) inhibitors. Mycoses 60(4):222–229
Kyriakidis I, Tragiannidis A, Zündorf I, Groll AH (2017) Invasive fungal infections in paediatric patients treated with macromolecular immunomodulators other than tumour necrosis alpha inhibitors. Mycoses 60(8):493–507
Mellinghoff SC, Panse J, Alakel N, Behre G, Buchheidt D, Christopeit M et al (2018) Primary prophylaxis of invasive fungal infections in patients with haematological malignancies: 2017 update of the recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society for Haematology and Medical Oncology (DGHO). Ann Hematol 97(2):197–207
Galli M, Antinori S, Atzeni F, Meroni L, Riva A, Scirè C et al (2017) Recommendations for the management of pulmonary fungal infections in patients with rheumatoid arthritis. Clin Exp Rhumatol 35(6):1018–1028
Vinicki JP, Pellet SC, Pappalardo C, Cruzat VC, Spinetto MA, Dubinsky D et al (2013) Invasive fungal infections in Argentine patients with systemic lupus erythematosus. Lupus 22(9):892–898
Kim HJ, Park YJ, Kim WU, Park SH, Cho CS (2009) Invasive fungal infections in patients with systemic lupus erythematosus: experience from affiliated hospitals of Catholic University of Korea. Lupus 18(7):661–666
Pardeo M, Wang J, Ruperto N, Alexeeva E, Chasnyk V, Schneider R et al (2019) Neutropenia during tocilizumab treatment is not associated with infection risk in systemic or polyarticular-course juvenile idiopathic arthritis. J Rheumatol 46(9):1117–1126
Pyrgos V, Shoham S, Roilides E, Walsh TJ (2009) Pneumocystis pneumonia in children. Paediatr Respir Rev 10(4):192–198
Basiaga ML, Ross ME, Gerber JS, Ogdie A (2018) Incidence of Pneumocystis jirovecii and adverse events associated with pneumocystis prophylaxis in children receiving glucocorticoids. J Pediatric Infect Dis Soc 7(4):283–289
Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB (2018) Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis 77(5):644–649
Martín Pedraz L, Carazo Gallego B, Moreno PD (2021) Clinical-epidemiological characteristics of Pneumocystis jirovecii pneumonia in a tertiary hospital in Spain. An Pediatr (Engl Ed) 95:4–10
Braga BP, Prieto-González S, Hernández-Rodríguez J (2019) Pneumocystis jirovecii pneumonia prophylaxis in immunocompromised patients with systemic autoimmune diseases. Med Clin (Barc) 152(12):502–507
Hsu HC, Chang YS, Hou TY, Chen LF, Hu LF, Lin TM et al (2021) Pneumocystis jirovecii pneumonia in autoimmune rheumatic diseases: a nationwide population-based study. Clin Rheumatol 40:3755–3763
Dunbar A, Schauwvlieghe A, Algoe S, van Hellemond JJ, Reynders M, Vandecasteele S et al (2020) Epidemiology of Pneumocystis jirovecii pneumonia and (non-)use of prophylaxis. Front Cell Infect Microbiol 15:10
Schmajuk G, Jafri K, Evans M, Shiboski S, Gianfrancesco M, Izadi Z et al (2019) Pneumocystis jirovecii pneumonia (PJP)prophylaxis patterns among patients with rheumatic diseases receiving high-risk immunosuppressant drugs. Semin Arthritis Rheum 48(6):1087–1092
Winthrop KL, Baddley JW (2018) Pneumocystis and glucocorticoid use: to prophylax or not to prophylax (and when?); That is the question. Ann Rheum Dis 77(5):631–633
Claytor B, Li Y (2022) Opinions on Pneumocystis jirovecii prophylaxis in autoimmune neuromuscular disorders. Muscle Nerve 65(3):278–283
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, De Groot K, Gross W et al (2009) EULAR recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis 68(3):310–317
Moosig F, Holle JU, Gross WL (2009) Value of anti-infective chemoprophylaxis in primary systemic vasculitis: what is the evidence? Arthritis ResTher 11(5)
Kronbichler A, Jayne DRW, Mayer G (2015) Frequency, risk factors and prophylaxis of infection in ANCA-associated vasculitis. Eur J Clin Invest 45(3):346–368
Guillevin L (2013) Infections in vasculitis. Best Pract Res Clin Rheumatol 27(1):19–31
Yates M, Watts RA, Bajema IM, Cid MC, Crestani B, Hauser T et al (2016) EULAR/ERA-EDTA recommendations for the management of ANCA-associated vasculitis. Ann Rheum Dis 75(9):1583–1594
Teichmann LL, Woenckhaus M, Vogel C, Salzberger B, Schölmerich J, Fleck M (2008) Fatal Pneumocystis pneumonia following rituximab administration for rheumatoid arthritis. Rheumatology (Oxford) 47(8):1256–1257
Besada E, Nossent JC (2013) Should Pneumocystis jiroveci prophylaxis be recommended with Rituximab treatment in ANCA-associated vasculitis? Clin Rheumatol 32(11):1677–1681
Bonilla-Abadía F, Betancurt JF, Pineda JC, Vélez JD, Tobón GJ, Cañas CA (2014) Pneumocystis jirovecii pneumonia in two patients with systemic lupus erythematosus after rituximab therapy. Clin Rheumatol 33(3):415–418
Zalmanovich A, Ben-Ami R, Rahav G, Alon D, Moses A, Olshtain-Pops K et al (2020) Rituximab identified as an independent risk factor for severe PJP: a case-control study. PLoS One 15(9 September)
Alexandre K, Ingen-Housz-Oro S, Versini M, Sailler L, Benhamou Y (2018) Pneumocystis jirovecii pneumonia in patients treated with rituximab for systemic diseases: report of 11 cases and review of the literature. Eur J Int Med 1(50):e23–e24
Grubbs JA, Baddley JW (2014) Pneumocystis jirovecii pneumonia in patients receiving tumor-necrosis-factor-inhibitor therapy: implications for chemoprophylaxis. Curr Rheumatol Rep 16(10):445–454
Komano Y, Harigai M, Koike R, Sugiyama H, Ogawa JUN, Saito K et al (2009) Pneumocystis jiroveci pneumonia in patients with rheumatoid arthritis treated with infliximab: a retrospective review and case-control study of 21 patients. Arthritis Care Res 61(3):305–312
Tanaka M, Sakai R, Koike R, Komano Y, Nanki T, Sakai F et al (2012) Pneumocystis jirovecii pneumonia associated with etanercept treatment in patients with rheumatoid arthritis: a retrospective review of 15 cases and analysis of risk factors. Mod Rheumatol 22(6):849–858
Watanabe K, Sakai R, Koike R, Sakai F, Sugiyama H, Tanaka M et al (2013) Clinical characteristics and risk factors for Pneumocystis jirovecii pneumonia in patients with rheumatoid arthritis receiving adalimumab: a retrospective review and case-control study of 17 patients. Mod Rheumatol 23(6):1085–1093
Zhang Y, Zheng Y (2014) Pneumocystis jirovecii pneumonia in mycophenolate mofetil-treated patients with connective tissue disease: analysis of 17 cases. Rheumatol Int 34(12):1765–1771
Messiaen PE, Cuyx S, Dejagere T, van der Hilst JC (2017) The role of CD4 cell count as discriminatory measure to guide chemoprophylaxis against Pneumocystis jirovecii pneumonia in human immunodeficiency virus-negative immunocompromised patients: a systematic review. Transpl Infect Dis 19(2)
Baulier G, Issa N, Gabriel F, Accoceberry I, Camou F, Duffau P (2018) Guidelines for prophylaxis of Pneumocystis pneumonia cannot rely solely on CD4-cell count in autoimmune and inflammatory diseases. Clin Exp Rheumatol 36(3):490–493
Cettomai D, Gelber AC, Christopher-Stine L (2010) A survey of rheumatologists’ practice for prescribing pneumocystis prophylaxis. J Rheumatol 37(4):792–799
Pereda CA, Nishishinya-Aquino MB, Brito-García N, Díaz del Campo Fontecha P, Rua-Figueroa I (2021) Is cotrimoxazole prophylaxis against Pneumocystis jirovecii pneumonia needed in patients with systemic autoimmune rheumatic diseases requiring immunosuppressive therapies? Rheumatol Int 41(8):1419–27
Boast A, Osowicki J, Cole T, Curtis N, Gwee A (2015) Question 1: Co-trimoxazole dosing dilemma: what is the right dose? Arch Dis Child 100(11):1089–1093
Ishikawa Y, Nakano K, Tokutsu K, Miyata H, Fujino Y, Matsuda S et al (2021) Estimation of treatment and prognostic factors of pneumocystis pneumonia in patients with connective tissue diseases. RMD Open 7(1)
Jansen MHA, Rondaan C, Legger GE, Minden K, Uziel Y, Toplak N et al (2023) EULAR/PRES recommendations for vaccination of paediatric patients with autoimmune inflammatory rheumatic diseases: update 2021. Ann Rheum Dis 82(1):35–47
Ohm M, van Straalen JW, Zijlstra M, de Joode-Smink G, Jasmijn Sellies A, Swart JF et al (2023) Meningococcal ACWY conjugate vaccine immunogenicity and safety in adolescents with juvenile idiopathic arthritis and inflammatory bowel disease: a prospective observational cohort study. Vaccine 41(25):3782–3789
Sen ES, Julandani D, Ramanan AV (2022) SARS-CoV-2 vaccinations in children and adolescents with rheumatic diseases. Rheumatology (Oxford) 61(11):4229–4231
Acknowledgements
The authors thank the Spanish Foundation of Rheumatology for providing medical writing/editorial assistance during the preparation of the manuscript. We would like to thank all those members of SERPE and SEIP who participated in the Delphi process: Agustín Remesal Camba, Walter Alberto Sifuentes Gigaldo, César Gavilán Martín, Tamara Rodríguez Araya, Almudena Román Pascual, María Isabel Garrote Llanos, Rocío Galindo Zavala, Alejandro Souto Vilas, Miguel Martí Masanet, Clara Udaondo, Jan Ramakers, Manoel Muñiz Fontan, Irene Rivero, Agustín López López, Begoña Carazo Gallego, Marta Salvatierra Arrondo, Manuel Oltra Benavent, Jesús Saavedra Lozano, Mª José Lirola Cruz, Sheila Miralbés Terraza, Andrea Martin, Manuel Oltra Benavent, Pilar Galán del Río, Eugenia Enríquez, Raquel Martin Domenech, Julio García Feitó, Cristina Zarallo Reales, Jenaro Graña Gil, Olaf Neth, María Muñoz San Jose, Antoni Noguera Julian, Laura Martín Pedraz, Andrea Zacarias Crovato, Isabel Pastora Granados Bautista, Vicenç Torrente Segarra, Clara Giménez Roca, Berta López, Jose Campos Esteban, Beatriz Bravo Mancheño, Marta Cano Cabrera, Carmen Vargas Lebrón, Marta Medrano San Ildefonso, Sara Pons Morales, Jorge Sotoca Fernandez, Berta Magallares López, Jordi Antón, Mari Pinedo, Mireia Lopez Corbeto, María López Sousa, Marta Valero Expósito, Judith Sánchez-Manubens, Juan Manuel Mosquera Angarita, Begoña Losada Pinedo.
Funding
Funding for open access publishing: Universidad Málaga/CBUA Open Access funding was provided thanks to the CRUE-CSIC agreement with Springer Nature. This project was partially funded by an unrestricted grant from Pfizer. Pfizer did not participate in the design or development of the project or in the drafting of the manuscript. SERPE also provided funds to the project. Funding for open access charge: Universidad de Málaga / CBUA.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the bibliographic search and revision of the manuscript. The wording of the various paragraphs is as follows: vaccination: Marisol Camacho Lovillo, M. José Lirola, and Laura Fernández Silveira; varicella zoster: Sara Guillén; tuberculosis: Joan Calzada and Cristina Calvo; Pneumocystis jirovecci: Esmeralda Núñez Cuadros and Daniel Clemente Garulo.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Clemente Garulo, D., Núñez-Cuadros, E., Camacho Lovillo, M. et al. Position statement on infection screening, prophylaxis, and vaccination in pediatric patients with rheumatic diseases and immunosuppressive therapies, part 2: infection prophylaxis. Eur J Pediatr 182, 4271–4284 (2023). https://doi.org/10.1007/s00431-023-05080-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05080-3