Abstract
To evaluate heart rate (HR), the presence of extrasystoles and other Holter findings among healthy newborns, and to collect data for new normal limits for Holter parameters in newborns. For this cross-sectional study, 70 healthy term newborns were recruited to undergo 24-h Holter monitoring. Linear regression analysis was used in HR analyses. The age-specific limits for HRs were calculated using linear regression analysis coefficients and residuals. The mean (SD) age of the infants was 6.4 (1.7) days during the recording. Each consecutive day of age raised the minimum and mean HR by 3.8 beats per minute (bpm) (95% CI: 2.4, 5.2; P < .001) and 4.0 bpm (95% CI: 2.8, 5.2; P < .001), respectively. Age did not correlate with maximum HR. The lowest calculated limit for minimum HR ranged from 56 bpm (aged 3 days) to 78 bpm (aged 9 days). A small number of atrial extrasystoles and ventricular extrasystoles were observed in 54 (77%) and 28 (40%) recordings, respectively. Short supraventricular or ventricular tachycardias were found in 6 newborns (9%).
Conclusion: The present study shows an increase of 20 bpm in both the minimum and mean HRs of healthy term newborns between the 3rd and 9th days of life. Daily reference values for HR could be adopted in the interpretation of HR monitoring results in newborns. A small number of extrasystoles are common in healthy newborns, and isolated short tachycardias may be normal in this age group.
What is Known: |
• The current definition of bradycardia in newborns is 80 beats per minute. |
• This definition does not fit into the modern clinical setting of continuously monitored newborns, where benign bradycardias are commonly observed. |
What is New: |
• A linear and clinically significant increase in heart rate was observed in infants between the ages of 3 and 9 days. |
• It appears as though lower normal limits for heart rate could be applied to the youngest newborns. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the neonatal period, major changes—such as a decrease in pulmonary vascular resistance, closure of fetal shunts, and a decline in hemoglobin levels—occur in the cardiovascular system. In addition, a progressive maturation of cardiac autonomic nervous control occurs during early postnatal life [1]. The above-mentioned changes affect the heart rate (HR) of newborns.
The lower limit for normal HR in newborns is commonly considered to be 80 beats per minute (bpm) [2]. Recently, Bohnhorst et al. challenged this definition by reporting that 30% of healthy newborns have bradycardias below 80 bpm [3].
Continuous HR monitoring is becoming increasingly common among newborns admitted to neonatal units. Large studies have recently presented new reference values for electrocardiogram (ECG) parameters [4, 5]. However, standard ECGs depict only a brief period of the HR, and a true resting state ECG can be difficult to obtain, especially in infants. There is a need for new HR reference values based on long-term HR monitoring.
During the neonatal period, extrasystoles are primarily a benign, self-resolving phenomenon [6]. The number of healthy newborns with extrasystoles varies significantly between studies, and the abnormal amount of extrasystoles in newborns remains unknown. In addition, there are still gaps in the understanding of cardiac arrhythmias during infancy.
This study’s purpose was to utilize modern Holter analytics and evaluate HR and heart rhythm in healthy newborns during the first week of life. The aim was to collect data for new normal limits for Holter parameters in newborns.
Materials and methods
For this cross-sectional study, healthy term (≥ 37 + 0/7 weeks of gestation) newborns were recruited to undergo 24-h Holter monitoring (Fig. 1). The newborns were recruited after birth from the maternity wards of Tampere University Hospital, Tampere, Finland, between December 2018 and April 2021. The study complied with the Declaration of Helsinki, and the Regional Ethics Committee of Tampere University Hospital approved the study. Written informed consent was obtained from the parents.
The study’s exclusion criteria included maternal hypertension or gestational diabetes mellitus that was treated with medication, maternal smoking or substance abuse, regular maternal medication that potentially affected newborns’ HRs (e.g., betablockers, beta sympathomimetics, selective serotonin reuptake inhibitors, anticonvulsants, thyroid medication), or Apgar scores below 7, hypoglycemia (blood sugar levels below 2.6 mmol/l), heart disease, suspected or diagnosed infection of the newborn, or admission to the neonatal ward. Newborns with Holter recordings of less than 18 h were excluded.
All the newborns were clinically examined, and a 12-lead ECG was performed. Reference ranges by Davignon et al. were applied to the ECGs [7]. Echocardiography (echo) and additional Holter recordings were performed if clinically indicated. Demographic data were obtained from medical records. Birth size was evaluated according to Finnish growth curves [8].
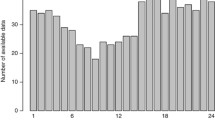
Twenty-four-hour Holter monitoring was initiated at the outpatient clinic after discharge from the hospital. A diary of the symptoms and activities was completed during the recording. A SEER Light or SEER Light Extend Holter recorder (GE Medical Systems Information Technologies, Milwaukee, WI, USA) with three-channel recordings was used for all subjects. Analysis of the recorded Holter data was performed with MARS V8 software (GE Medical Systems Information Technologies, Milwaukee, WI, USA). The software automatically analyzed the HR, maximum R-R interval, number of QRS complexes, and number and runs of atrial premature contractions (APCs) and ventricular premature contractions (VPCs). The software calculated HR in bpm from 10 R-R intervals. After automated analysis, Holter data were checked for any misinterpretation of the software and edited manually by trained nurses. The final Holter data were interpreted by two physicians specialized in clinical physiology (PL and AT).
Statistical analyses
In the sample size calculation, we assumed that the true minimum HR was 10 bpm lower than the current reference value of 94 bpm for 4–10-day-old newborns [9]. Using a standard deviation (SD) for HR of 13 bpm, as reported by Southall et al. [9], a sample size calculation showed that 28 observations were needed (force .80, P = .05). To ensure a large enough sample size, 70 newborns were planned to recruit.
Age was calculated in hours from birth and converted into days. Means and SDs were calculated for normally distributed variables, and medians and ranges were calculated for skew-distributed variables. Frequencies and percentages were used for categorical variables. Pearson correlation was used whenever appropriate. Linear regression analysis was used in univariate and multivariate HR analyses. The age-specific limits, with -2 and 2 SDs, for HRs were calculated using linear regression analysis coefficients and residuals. In case of missing data, complete case analysis was used. The statistical significance level was defined as P (two-sided) < .05, and 95% confidence intervals (CIs) were presented whenever appropriate. Statistical analyses were performed using IBM SPSS Statistics for Macintosh version 28.0 (IBM, Armonk, NY, USA).
Results
The study population consisted of 70 newborns (46% males) (Table 1). One infant had signs of ventricular hypertrophy on ECG. All other infants had normal ECG findings. Echo was performed on three infants due to a systolic murmur (n = 1), abnormal ECG (n = 1), and ventricular tachycardia (VT) in the Holter recording (n = 1), and they all had normal echo findings appropriate to their age.
The mean age at the start of the monitoring period was 6.4 days (range: 2.7–9.5 days) (Table 1). The means for the minimum and maximum HRs were 88 bpm and 208 bpm, respectively (Table 2). The minimum HR showed sinus rhythm in most cases (sinus rhythm, n = 68 [97%]; junctional rhythm, n = 2 [3%]). The minimum HR occurred during sleeping (n = 56 [80%]), eating (n = 4 [6%]), or unspecified activity (n = 10 [14%]). The maximum HR showed sinus rhythm in all cases. The maximum HR occurred during crying or agitation (n = 50 [71%]), eating (n = 6 [9%]), sleeping (n = 2 [3%]), hiccupping (n = 1 [1%]), or unspecified activity (n = 11 [16%]). No cardiac symptoms were reported during the recording.
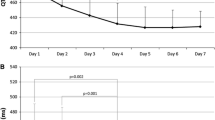
Positive correlations were observed between age and minimum HR (r = .55; P < .001) (Fig. 2) and age and mean HR (r = .64; P < .001) (Fig. 3). Age did not correlate with maximum HR (Fig. 4). According to the univariate linear regression analyses, each consecutive day of age raised the minimum and mean HRs by 3.8 bpm (95% CI: 2.4, 5.2; P < .001) and 4.0 bpm (95% CI: 2.8, 5.2; P < .001), respectively (Table 3). No statistically significant associations were found between sex and HR or gestational age (GA) at birth and HR in the univariate analyses.
Multivariate linear regression analyses for HR were performed with the independent variables of age, sex, and GA (Table 3). According to these analyses, age and male sex had a statistically significant correlation with minimum HR (age coefficient: 3.8 bpm [95% CI: 2.4, 5.2]; P < .001; sex coefficient: -4.7 bpm [95% CI: -9.3, -.05]; P < .05), and age and GA had a statistically significant correlation with mean HR (age coefficient: 4.1 bpm [95% CI: 3.0, 5.2]; P < .001; GA coefficient: -2.1 bpm [95% CI: -3.9, -.3]; P = .02). The association between age and HR was not significantly affected after adding variables (sex and GA) to the linear regression model (Table 3). None of the variables (age, sex and GA) showed a statistically significant correlation with maximum HR in the multivariate linear regression analysis.
The age-specific limits for minimum HR were calculated using the following formula based on regression analysis results: 63.6 bpm + 3.8 * Age (days); ± 2 * 9.7 (Table 4). A similar formula was used for mean HR: 115.1 bpm + 4.0 * Age (days); ± 2 * 8.0. The lowest calculated limit for HR was 56 bpm for 3-day-old newborns and 78 bpm for 9-day-old newborns.
One or more APCs and one or more VPCs were observed in 54 (77%) and 28 (40%) infants’ recordings, respectively (Table 2). The percentages for APCs and VPCs were ≤ 1% of total beats in all the recordings. Five neonates (7%) had one, two, or three 3-beat-long to 6-beat-long episodes of supraventricular tachycardia (SVT) with a median frequency of 193 bpm (range: 180–241 bpm). One infant (1%) had a 4-beat-long episode of VT with a frequency of 208 bpm. The total number of APCs or VPCs was low (range: 5–47 beats) in recordings with SVT or VT. All the infants with SVT or VT had normal results in the control recordings.
Discussion
The present study showed an increase of 20 bpm in the minimum and mean HRs of healthy term newborns between the 3rd and 9th days of life. In addition, the proportion of infants with extrasystoles was higher than previously reported, and short SVTs and VTs were observed in 9% of the recordings in healthy newborns.
Increasing HR during the neonatal period has been reported in previous studies [10,11,12,13,14]. In these studies, HR measurements were seldom based on Holter recordings or other long-term HR monitoring. In a large review by Fleming et al., the median HR increased from 127 bpm at birth to 145 bpm at 1 month [10]. While this review included studies with various HR measurements (e.g., ECG, blood pressure monitors, manual measurements, echo, pulse oximeters), only four studies in the review were Holter studies on newborns. Richards et al. studied 110 term infants with sequential Holter recordings during the first 6 months of their lives [11]. In this study, the mean HR increased from 116 to 141 bpm in the first 15 days. However, the researchers only reported HR during periods of regular breathing, with a total duration of 3 h (mean) in the first 15 days.
Previous findings on increasing HR during the neonatal period have been observations of mean or median heart rate measurements. To our knowledge, the present study is the first to report increases in both minimum and mean HR with postnatal age. Inaccuracies in the diaries held by parents during the recording prevented us from separately evaluating waking and sleeping HRs. However, HR has previously been observed to increase at similar rates during both waking and sleeping states during the first month of life [12, 15]. The maximum HR in our study population was not age-dependent. Since no stress test was performed, we do not know whether the recorded maximum HR was the true maximum HR of the evaluated newborns.
Due to the postnatal cardiovascular stabilization period, we did not perform Holter monitoring on our subjects during the first couple of days of life. However, according to previous studies, HR progression is not linear from birth. In HR variability studies, HR variability increases and HR declines during the first postnatal days [1]. Makarov et al. reported differences in the waking mean HR between days 1, 2, and 4—with day 2’s HR being the lowest [13]. In another study, the median HR (measured by a blood pressure monitor) declined progressively in the first 3 days and increased on the 4th day [14]. Both the early decline and subsequent increase of HR have been explained by the postnatal acceleration of autonomic nervous system maturation [1, 12].
Previous Holter studies support our result that the minimum HR for newborns is lower than 80 bpm (Table 5). The mean values for HRs were somewhat similar in these studies. The small differences in the values between the studies can be explained by the small sample sizes. However, none of these studies considered the possible effect of age on HR. Our findings highlight the importance of more age-specific HR thresholds. If the HR thresholds were equal in all neonates, the youngest newborns would likely be misclassified as sick, potentially leading to prolonged hospitalization. Furthermore, the use of the same reference values for all newborns may cause false-negative findings in older newborns.
Both male sex and GA had negative correlations with HR if age was included in the regression analysis. Previous studies’ findings on gender differences in the HRs of newborns are controversial [16,17,18]. In the present study, gender difference was observed only at the minimum heart rate. An inverse correlation between GA and HR has been reported [5, 19]. In these studies, the effect of GA on HR persisted after adjustment for confounding factors, such as birth weight, postnatal age and sex. The direct effect of GA on HR can be explained by the maturation of the autonomic nervous system. Premature newborns have a predominance of sympathetic tone, and cardiac parasympathetic activity increases progressively with GA [1, 20].
The frequency of extrasystoles has varied significantly between previous Holter studies [13, 21, 22]. This is likely due to the studies’ dissimilar equipment, small sample sizes, and diverse age ranges. The frequencies of APCs and VPCs in our previous Holter study [23] and the present study were higher than previously reported. For instance, Southall et al. found APCs in 19/134 (14%) newborns aged under 10 days, but they counted extrasystoles in randomly selected hours of recording [9]. In a Holter study of 25 healthy newborns with a population similar to present study’s (age range: 3–10 days; mean age: 6.5 days), 8% of the infants had APCs, and 28% had VPCs [24]. We conducted both automated and manual analyses of extrasystoles to ensure the reliability of the results. Most infants had < 100 APCs or VPCs during the 24-h recording. In support of previous studies’ findings, we can conclude that the presence of a small amount of extrasystoles is common in healthy newborns. Further research is warranted to evaluate the upper limit for normal amounts of extrasystoles in newborns.
The estimated prevalence of SVT in infancy is between 1/250 and 1/1000 [25]. SVT in the first year of life is considered an arrhythmia that requires prophylactic antiarrhythmic treatment until the tendency for SVT ceases spontaneously [26]. Isolated VT in infants without a structural heart disease is often an incidental finding in the course of evaluating an unrelated condition, and most of these infants may be managed with conservative observation alone [27, 28].
Interestingly, 9% of our healthy subjects had short episodes of SVT or VT that disappeared during follow-up and without treatment. In a retrospective study of an institution’s pediatric SVT, 74% of infants younger than 1 year presented no symptoms at diagnosis, and in 44% of infants, the diagnosis was made during routine investigations or monitoring [29]. Because infants may be asymptomatic during brief SVT episodes, the incidence of infantile SVT is likely underestimated. The incidental short tachycardias in our healthy newborn population could present as a subtype of SVT in infancy. Further studies are needed to evaluate whether the tendency for short tachycardias ceases at younger age than the tendency for longer or sustained SVT. Our findings suggest that some newborns with short SVTs could be managed with close follow-up and without prophylactic antiarrhythmic treatment.
The strengths of this study include its homogenous study population of healthy newborns, careful exclusion of neonatal and maternal conditions that could potentially affect HR, thorough Holter data analysis, and, compared to previous Holter studies, its sample size. However, the study is also limited by its sample size due to the small number of cases in each age group.
Conclusions
The present study showed clinically relevant age-dependent changes in minimum and mean HR by 9 days of age. Daily reference values for HR could be adopted in the interpretation of HR monitoring results in newborns. Larger and broader sample sizes could better verify the age-specific reference values and changes to these values with advancing age. A small number of extrasystoles are common in healthy newborns, and short isolated tachycardias may be normal in this age group.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- APC:
-
Atrial premature contraction
- Bpm:
-
Beats per minute
- CI:
-
Confidence interval
- ECG:
-
Electrocardiogram
- Echo:
-
Echocardiography
- GA:
-
Gestational age
- HR:
-
Heart rate
- SD:
-
Standard deviation
- SVT:
-
Supraventricular tachycardia
- VPC:
-
Ventricular premature contraction
- VT:
-
Ventricular tachycardia
References
Javorka K, Lehotska Z, Kozar M, Uhrikova Z, Kolarovszki B, Javorka M, Zibolen M (2017) Heart rate variability in newborns. Physiol Res 66(Suppl 2):S203–S214. https://doi.org/10.33549/physiolres.933676
Miller MS, Shannon KM, Wetzel GT (2000) Neonatal bradycardia. Prog Pediatr Cardiol 11:19–24. https://doi.org/10.1016/s1058-9813(00)00032-1
Bohnhorst B, Seidel K, Böhne C, Peter C, Pirr S (2019) Heart rate, respiratory rate, apnoeas and peripheral arterial oxygen saturation in healthy term neonates during quiet sleep. Acta Paediatr 108:231–238. https://doi.org/10.1111/apa.14470
Bratincsák A, Kimata C, Limm-Chan BN, Vincent KP, Williams MR, Perry JC (2020) Electrocardiogram standards for children and young adults using z-scores. Circ Arrhythm Electrophysiol 13:e008253. https://doi.org/10.1161/CIRCEP.119.008253
Hartmann J, Pærregaard MM, Norsk J, Pietersen A, Iversen KK, Bundgaard H, Christensen AH (2021) Gestational age and neonatal electrocardiograms. Pediatrics 148:e2021050942. https://doi.org/10.1542/peds.2021-050942
Jaeggi E, Öhman A (2016) Fetal and neonatal arrhythmias. Clin Perinatol 43:99–112. https://doi.org/10.1016/j.clp.2015.11.007
Davignon A, Rautaharju P, Boisselle E (1980) Normal ECG standards for infants and children. Pediatr Cardiol 1:123–131. https://doi.org/10.1007/BF02083144
Sankilampi U, Hannila ML, Saari A, Gissler M, Dunkel L (2013) New population-based references for birth weight, length, and head circumference in singletons and twins from 23 to 43 gestation weeks. Ann Med 45:446–454. https://doi.org/10.3109/07853890.2013.803739
Southall DP, Richards J, Mitchell P, Brown DJ, Johnston PGB, Shinebourne EA (1980) Study of cardiac rhythm in healthy newborn infants. Br Heart J 43:14–20. https://doi.org/10.1136/hrt.43.1.14
Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, Tarassenko L, Mant D (2011) Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377:1011–1018. https://doi.org/10.1016/S0140-6736(10)62226-X
Richards JM, Alexander JR, Shinebourne EA, de Swiet M, Wilson AJ, Southall DP (1984) Sequential 22-hour profiles of breathing patterns and heart rate in 110 full-term infants during their first 6 months of life. Pediatrics 74:763–777. https://doi.org/10.1542/peds.74.5.763
Mrowka R, Patzak A, Schubert E, Persson PB (1996) Linear and non-linear properties of heart rate in postnatal maturation. Cardiovasc Res 31:447–454. https://doi.org/10.1016/S0008-6363(95)00207-3
Makarov L, Komoliatova V, Zevald S, Schmidt G, Muller A, Serebruany V (2010) QT dynamicity, microvolt T-wave alternans, and heart rate variability during 24-hour ambulatory electrocardiogram monitoring in the healthy newborn of first to fourth day of life. J Electrocardiol 43:8–14. https://doi.org/10.1016/j.jelectrocard.2009.11.001
Sadoh WE, Sadoh AE (2012) Normal oscillometric heart rate of term African infants in the early days of life. Paediatr Int Child Health 32:107–110. https://doi.org/10.1179/2046905511Y.0000000015
Harper RM, Hoppenbrouwers T, Sterman MB, McGinty DJ, Hodgman J (1976) Polygraphic studies of normal infants during the first six months of life. I. Heart rate and variability as a function of state. Pediatr Res 10:937–944. https://doi.org/10.1203/00006450-197611000-00008
Salameh A, Gebauer RA, Grollmuss O, Vít P, Reich O, Janoušek J (2008) Normal limits for heart rate as established using 24-hour ambulatory electrocardiography in children and adolescents. Cardiol Young 18:467–472. https://doi.org/10.1017/S1047951108002539
Krasemann T, Bente K, Burkhardtsmaier G (2010) The corrected QT interval in 24 h ECGs in neonates. Clin Res Cardiol 99:309–314. https://doi.org/10.1007/s00392-010-0120-3
Nagy E, Orvos H, Bardos G, Molnar P (2000) Gender-related heart rate differences in human neonates. Pediatr Res 47:778–780. https://doi.org/10.1203/00006450-200006000-00016
Burtchen N, Myers MM, Lucchini M, Ordonez Retamar M, Rodriguez D, Fifer WP (2019) Autonomic signatures of late preterm, early term, and full term neonates during early postnatal life. Early Hum Dev 137:104817. https://doi.org/10.1016/j.earlhumdev.2019.06
Cardoso S, Silva MJ, Guimarães H (2017) Autonomic nervous system in newborns: a review based on heart rate variability. Childs Nerv Syst 33:1053–1063. https://doi.org/10.1007/s00381-017-3436-8
Nagashima M, Matsushima M, Ogawa A, Ohsuga A, Kaneko T, Yazaki T, Okajima M (1987) Cardiac arrhythmias in healthy children revealed by 24-hour ambulatory ECG monitoring. Pediatr Cardiol 8:103–108. https://doi.org/10.1007/BF02079464
Massin MM, Bourguignont A, Gérard P (2005) Study of cardiac rate and rhythm patterns in ambulatory and hospitalized children. Cardiology 103:174–179. https://doi.org/10.1159/000084590
Uusitalo A, Tikkakoski A, Reinikainen M, Lehtinen P, Ylänen K, Korhonen P, Poutanen T (2022) Extrasystoles or short bradycardias of the newborn seldom require subsequent 24-hour electrocardiographic monitoring. Acta Paediatr 111:979–984. https://doi.org/10.1111/apa.16259
Alpay F, Celiker A, Lenk MK, Ozcan O, Tanindi S, Isik E (1993) Ambulatory electrocardiographic monitoring in healthy newborn infants. Turk J Pediatr 35:163–170
Richardson C, Silver ES (2017) Management of Supraventricular Tachycardia in Infants. Pediatr Drugs 19:539–551. https://doi.org/10.1007/s40272-017-0254-0
Brugada J, Blom N, Sarquella-Brugada G, Blomstrom-Lundqvist C, Deanfield J, Janousek J, Abrams D, Bauersfeld U, Brugada R, Drago F et al (2013) Pharmacological and non-pharmacological therapy for arrhythmias in the pediatric population: EHRA and AEPC-Arrhythmia Working Group joint consensus statement. Europace 15:1337–1382. https://doi.org/10.1093/europace/eut082
Crosson JE, Callans DJ, Bradley DJ, Dubin A, Epstein M, Etheridge S, Papez A, Phillips JR, Rhodes LA, Saul P et al (2014) PACES/HRS expert consensus statement on the evaluation and management of ventricular arrhythmias in the child with a structurally normal heart. Heart Rhythm 11:e55–e78. https://doi.org/10.1016/j.hrthm.2014.05.010
Levin MD, Stephens P, Tanel RE, Vetter VL, Rhodes LA (2010) Ventricular tachycardia in infants with structurally normal heart: a benign disorder. Cardiol Young 20:641–647. https://doi.org/10.1017/S1047951110000867
Vos P, Pulles-Heintzberger CFM, Delhaas T (2003) Supraventricular tachycardia: An incidental diagnosis in infants and difficult to prove in children. Acta Paediatr 92:1058–1061. https://doi.org/10.1111/j.1651-2227.2003.tb02577.x
Montague TJ, Taylor PG, Stockton R, Roy DL, Smith ER (1982) The Spectrum of Cardiac Rate and Rhythm in Normal Newborns. Pediatr Cardiol 2:33–38. https://doi.org/10.1007/BF02265614
Funding
Open access funding provided by Tampere University including Tampere University Hospital, Tampere University of Applied Sciences (TUNI). The study was supported by the Support Association for Tampere Children’s Clinic (to TP [grant number: MS593]), the Foundation for Pediatric Research (to PHK; and to AU [grant number: 190128]), the Instrumentarium Science Foundation (to AU [grant number: 200066]), and the Competitive State Research Financing of the Expert Responsibility Area of Tampere University Hospital (to AU).
Author information
Authors and Affiliations
Contributions
All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work. All authors contributed to the study conception and design. Tuija Poutanen and Päivi Korhonen supervised the execution of the study. Data collection was performed by Asta Uusitalo, Antti Tikkakoski, Pieta Lehtinen and Kaisa Ylänen. Material preparation and data analysis were performed by Asta Uusitalo and Antti Tikkakoski. The first draft of the manuscript was written by Asta Uusitalo, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was performed in line with the Declaration of Helsinki and was approved by the Regional Ethics Committee of Tampere University Hospital (No R18083).
Consent to participate
Written informed consent was obtained from the parents.
Consent to publish
All the patient data are anonymized, and parents consented to publication of the results of the project.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Uusitalo, A., Tikkakoski, A., Lehtinen, P. et al. Younger postnatal age is associated with a lower heart rate on Holter monitoring during the first week of life. Eur J Pediatr 182, 2359–2367 (2023). https://doi.org/10.1007/s00431-023-04914-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04914-4