Abstract
Potential medium- and long-term neurodevelopmental sequelae of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection during pregnancy have not been ruled out. We aimed to systematically review and summarize the evidence regarding the effects of intrauterine exposure to SARS-CoV-2 on infant development and behavior. Scopus, PubMed, Web of Science, CINAHL, and PsycNet databases were searched for studies published up to February 6, 2023, investigating the effects of gestational SARS-CoV-2 on infant development and behavior. We performed narrative synthesis according to updated protocols. Studies using comparison groups and with the Ages and Stages Questionnaires-Third Edition (ASQ-3) scores available were included in a meta-analysis performed according to Cochrane protocols. We used the Newcastle–Ottawa Quality Assessment Scale to analyze the risk of bias. Heterogeneity was calculated using the I2 statistic. The search identified 2,782 studies. After removing duplicates and applying the eligibility criteria, we performed a narrative synthesis of 10 included studies and a meta-analysis of three. There was no evidence of higher developmental delay rates in infants exposed to SARS-CoV-2 during pregnancy compared to non-exposed infants. However, the exposed infants scored lower than either the non-exposed children or pre-pandemic cohorts in some domains. Pooled results from the random-effects model indicated that SARS-CoV-2-exposed infants had lower scores on fine motor (mean difference [MD] = -4.70, 95% confidence interval [CI]: -8.76; -0.63), and problem-solving (MD = -3.05, 95% CI: -5.88; -0.22) domains than non-exposed infants (heterogeneity: I2 = 69% and 88%, respectively). There was no difference between the exposed and non-exposed infants in the communication, gross motor, and personal-social ASQ-3 domains.
Conclusion: We did not find evidence confirming the association between SARS-CoV-2 gestational exposure and neurodevelopmental delays. However, the meta-analysis indicated that gestational exposure negatively affected fine motor and problem-solving skills. Robust evidence on this topic is still incipient, and the available studies present methodological inconsistencies that limit the drawing of clear-cut conclusions.
PROSPERO registration: #CRD42022308002; March 14, 2022.
What is Known: • COVID-19 is associated with adverse pregnancy outcomes potentially linked to neurodevelopmental delays. • SARS-CoV-2 vertical transmission is rare; however, infections during pregnancy can be deleterious to the fetus, possibly mediated by maternal immune activation and other inflammatory mechanisms. | |
What is New: • No evidence of increased developmental delay rates among SARS-CoV-2 gestational-exposed infants was found. However, a meta-analysis of three studies showed lower scores in fine motor and personal social ASQ-3 domains among exposed infants. • SARS-CoV-2 gestational exposure and the pandemic can affect child development via many mechanisms. Potential neurodevelopmental sequelae of SARS-CoV-2 exposure during gestation have not been ruled out. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Since the beginning of the coronavirus disease 2019 (COVID-19) pandemic, more than 58 million women of reproductive age (15–40 years) have been infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. The prevalence of COVID-19 in pregnant women varies from 6 to 8%, based on universal screening surveys [2,3,4]. A serologic survey that analyzed 1,900 asymptomatic dyads in the first week after childbirth, between April and August 2021, found that 13% of puerperal women were seropositive for SARS-CoV-2 anti-N IgG as were 15% of their neonates [5].
Growing evidence has shown that SARS-CoV-2 vertical transmission is rare [6,7,8,9,10]. However, even in the absence of vertical transmission and a direct effect of the virus on the fetus, gestational infections can still be deleterious to the offspring, possibly mediated by maternal immune activation (MIA) and other inflammatory mechanisms [10,11,12,13,14]. It has been well documented that COVID-19 is associated with adverse pregnancy outcomes potentially linked to neurodevelopmental delays, such as preeclampsia, preterm birth, fetal distress requiring cesarean delivery, and neonatal intensive care admission [2, 4, 15,16,17,18].
Moreover, gestational infections induce inflammatory and immunological responses, which may disrupt the placental function, altering hormonal release, increasing cytokine production, and immune cell infiltration [19]. Placental malfunctioning is also related to fetal distress, lower cord pH, fetal hypoxia, and NICU admission [18]. Secondary neuroinflammation and modified embryogenesis may potentially interfere with central nervous system development [19]. Although neonatal COVID-19's most common manifestation is a sepsis-like syndrome, neurologic symptoms and neurologic inflammation secondary to SARS-CoV-2 vertical transmission have been demonstrated [9]. Neurological manifestations are relatively common in neonatal COVID-19 and may be due to the direct viral cytopathic effect, but also due to prematurity induced by maternal COVID-19 [8, 9, 13, 14].
Regardless of the biological plausibility of the adverse outcomes of SARS-CoV-2 gestational exposure, it is important to consider the effect of COVID-19 pandemic–related psychological stress on gestational and neonatal outcomes [20,21,22,23]. Pre- and postnatal maternal depression may compromise the quality of parenting practices and mother–child interactions, such as low responsiveness to the child’s needs and harsh parenting [24, 25]. Feelings of uncertainty and fear, death of loved ones, social isolation, loss of income, and domestic violence are some factors that can contribute to maternal anxiety and depression, and increasing, though, the risk of negative outcomes related to child development [24, 26,27,28]. A recent Brazilian study explored the association between COVID-19 and women’s mental health. Almost half of the 1,041 pregnant women included in the study were suspected of suffering from common mental disorders, and the negative feelings brought about by the pandemic, such as fear and anxiety, were strongly associated with these symptoms [29].
Current literature has generally explored the short-term neonatal outcomes of children born to infected mothers [4, 8, 16, 17, 30, 31]. Nevertheless, such exposure may have long-term effects, even without direct neonatal infection [10,11,12, 20,21,22,23]. Given the large number of pregnant women infected by the SARS-CoV-2, even a modest increase in the risk for adverse neurodevelopmental outcomes would still have a massive public health impact [12].
Despite a notable increase in the knowledge around gestational exposure to SARS-CoV-2, studies analyzing the mid and long-term effects of this exposure are still incipient [12, 21], and the potential neurodevelopmental sequelae have not been ruled out [12, 21]. Therefore, the present study aimed to systematically review and summarize the evidence concerning the effects of intrauterine exposure to SARS-CoV-2 on infant development.
Methods
We conducted a rapid systematic review of primary studies according to the JBI Manual for Evidence Synthesis [32], Meta-Analyses of Observational Studies in Epidemiology (MOOSE) [33], Synthesis Without Meta-Analysis (SWiM) [34], and Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [35] guidelines. The review protocol was registered with PROSPERO on March 14, 2022 (#CRD42022308002). The review question was: What are the effects of being exposed to SARS-CoV-2 during gestation on infants’ development?
Outcomes
The primary outcome, developmental and behavioral disorders, refers to physical and/or mental impairments that limit the child from progressively developing and achieving the skills expected at each age [36].
Eligibility criteria
The following inclusion criteria were used to select studies that investigated: (a) the impact of SARS-CoV-2 infection during pregnancy on the development and behavior of children aged from 1 to 23 months; (b) SARS-CoV-2 infection during pregnancy confirmed by viral tests, or presumed by serological or antigen tests, or documented in medical records or official reporting databases; (c) SARS-CoV-2 infection that occurred at any gestational period with any clinical presentation, including asymptomatic cases; (d) standardized assessment of child development and behavior using validated tests, based on direct observation or parental reports; and (e) observational studies (cohort, case–control, cross-sectional).
We excluded studies regarding (a) maternal exposure to other infectious diseases during pregnancy (e.g., SARS-CoV-1, MERS-CoV); (b) infants with congenital malformations, sensory deficits, chromosomal disorders, and other conditions that can affect neurodevelopment; (c) isolated assessments of neurosensory functions without a link to child development and behavior; (d) letters, editorials, commentaries, book chapters, and qualitative, psychometrics studies, reviews, meta-analyses, case reports, protocols, and pilot studies; and (f) papers not written in English, Spanish, or Portuguese.
Search strategy
The research team developed, tested, and revised the search strategy based on the eligibility criteria after the pilot test. Eligible studies were searched for in five electronic databases: Scopus, PubMed, Web of Science, CINAHL, and PsycNet. The databases were accessed on February 6, 2023. Descriptors were identified in the Medical Subject Headings (MeSH). The search strategy was adapted based on the descriptors in each database and is presented in Table S1 (see Additional File 1).
Selection process
All identified studies were included and managed during the screening phase at the Rayyan web app for systematic reviews [37]. Screening and removal of duplicate papers, initial screening based on the title and abstract, and full reading of the screened papers were performed by two independent researchers according to the eligibility criteria (G.S.M.A.P. and R.C.S.). Studies that met all the eligibility criteria were included in the present rapid review. Discordance was resolved by consensus with other authors.
Data extraction and synthesis
Data, including author, year of publication, study location, objective, instruments, data collection procedure, study design, and main findings, were extracted using a predefined form. The data extraction process was performed by two authors based on the SWiM protocol [34] and was validated by the research team. Data were organized in tables and presented as follows: author and year, study design, country, follow-up period, sample characteristics, instruments, and main results. Additionally, we evaluated whether the studies had sufficient data to conduct a meta-analysis. Studies that included a control group and presented the child scores by Ages and Stages Questionnaires-Third Edition (ASQ-3) domains met the criteria for meta-analysis [38,39,40]. ASQ-3 scores by domain were the main outcome of the meta-analysis.
Risk of bias
The Newcastle–Ottawa Quality Assessment Scale (NOS) [41] assesses three quality parameters (selection, comparability, and outcome) and is widely used to analyze the risk of bias in observational studies. The highest score (nine stars) indicates a high-quality study, while studies with less than five stars indicate a high risk of bias. The risk of bias of the 10 studies included in the rapid review was independently assessed by two researchers and is presented in Table S2 (see Additional File 1).
Statistical analysis
No statistical method other than the description of proportions and frequencies of the main findings was used to perform the narrative synthesis.
Meta-analysis were performed using Cochrane RevMan Manager 5.4.1 software [42]. Treatment effects were expressed as mean differences (MDs) and calculated using a random-effects model. Considering the small number of studies included in the meta-analysis, the Mantel–Haenszel method was used to estimate the effect size. Forest plots were used to visualize treatment effects. The effects of statistical heterogeneity between the studies were assessed using the Cochran Q test. The I2 statistic was used to assess the extent of heterogeneity between studies. Heterogeneity was considered low for I2 < 30%, moderate for I2 ≥ 30 and ≤ 75%, and high for I2 > 75% [43]. Prediction intervals and subgroup analyses were not performed because of the small number of included studies. The risk of publication bias was examined using the asymmetry of the funnel plot and Egger’s test.
Results
Study selection
The search identified 2,782 studies. After removing duplicates (n = 1,389), titles and abstracts of the remaining 1,393 studies were screened. Initial screening identified 15 studies that met the eligibility criteria. During the full-reading phase, five more studies were excluded. The remaining 10 studies were included in the narrative synthesis, and three of them were included in the meta-analysis. Figure 1 shows the PRISMA flow diagram.
PRISMA 2020 flow diagram [35]
Studies overview
The overview of the studies is detailed in Table 1. For most of the 10 studies included in the present review, data collection was carried out in 2020 (n = 9) [38,39,40, 44,45,46,47,48,49,50]. These studies were conducted in China (n = 3) [38, 39, 46], Italy (n = 1) [48], the United States (n = 3) [40, 45, 49], United States and Brazil (n = 1) [50], India (n = 1) [47], and Kuwait (n = 1) [44].
Most studies used a prospective design (n = 9) [38, 40, 44,45,46,47,48,49,50], and six used a comparison group [39, 40, 47,48,49,50].
Gestational exposure to SARS-CoV-2 was defined based on nasal-swab polymerase chain reaction (PCR) results in the majority of studies (n = 8) [38, 40, 44, 45, 47,48,49,50]. Serology results (n = 1) [35] and information extracted from medical records or official databases (n = 6) [38, 39, 44, 46, 49, 50] were also accepted to define gestational exposure. Except for the study by Shuffrey et al. [40], all other studies included women who were predominantly infected in the third trimester of gestation [38, 39, 44,45,46,47,48,49,50]. Maternal disease presentation was described in nine of the 10 studies, and most of the women had mild or asymptomatic COVID-19 [38,39,40, 44,45,46, 48,49,50]
Methodological aspects
Tables 2 and 3 summarize the studies’ assessment approaches and main findings. Regarding the characteristics of the study samples, Wu et al. and Cheng et al. compared exposed infants to non-exposed ones [38, 39]. Shuffrey et al. initially compared exposed and non-exposed infants; afterward, children born during the pandemic period were grouped to explore the differences between pandemic and pre-pandemic cohorts [40]. Martinez et al. also compared exposed infants to neurotypical pre-pandemic controls [50]. Munian et al. grouped the neonates of infected mothers according to their infection status; thus, positively exposed neonates were compared to negatively exposed ones [47]. Mulkey et al. compared exposed infants born to symptomatic and asymptomatic mothers and perinatally infected neonates [49]. Wang et al., Schuh et al., Buonsenso et al., and Ayed et al. did not group the participants [44,45,46, 48].
Child neurodevelopment was assessed using standardized questionnaires in eight studies [38,39,40, 44,45,46,47, 49], and neurological examination was reported in four studies [47,48,49,50] (Table 2). Additionally, three studies explored neurosensory functions based on audiological [40, 42, 43] and ophthalmological tests [48] (Table 3).
The ASQ-3 was the most commonly used tool (n = 7) to assess children’s development, considering the communication, fine motor, gross motor, problem-solving, and personal-social domains [38,39,40, 44,45,46, 49]. In two studies, the ASQ: Social-Emotional, Second Edition (ASQ: SE-2) was also used [39, 46]. The Developmental Profile 3 (DP3) was used in one study to assess adaptative behavior, social-emotional, cognitive, and communication skills [47]. Developmental assessments were performed when the children were 3 to 17 months old.
Standardized neurological examination using the Amiel-Tison method at six months old [47], gross motor skills based on postural milestones in children from zero to nine months old [48], General Movement Assessment (GMA) videos between 3 and 5 months [50], and the CDC´s developmental milestones between 6 and 8 months of age [50] were also used to assess child development.
All three studies that assessed neurosensory outcomes examined the infant Auditory Brainstem Response (ABR) [45, 47, 48] (Table 3). Buonsenso et al. [48] completed the audiological evaluation using the Transient Evoked Otoacoustic Emissions (TEOAE) test. In addition, they reported that infants’ ophthalmological examinations included retinal ultra-widefield fluorescein angiography (FFA), retinal spectral domain optical coherence tomography (SD-OCT), and behavioral assessment of visual function (ability to fix, track, saccade movements, visual acuity, attention at distance, binocular visual fields, and contrast sensitivity) [48].
Main findings of individual studies
The main findings of individual studies were described according to the tools used to assess children’s developmental and neurosensory outcomes, as presented in Tables 2 and 3.
Child development and behavior
Regarding the three single-arm cohorts based on the ASQ-3, Schuh et al. reported that all 15 exposed infants were classified as normal at six months old [45]. Conversely, Wang et al. reported that the proportion of children at risk of developmental delay at three months of age varied between 13.5% and 23.1% in the ASQ-3 subdomains but reached 86.4% in the socio-emotional domain [46]. According to Ayed et al., 10% of 10–12 month-old children scored below the cut-off in at least one subdomain, with fine motor, personal social, and gross motor being the most frequently affected [44]. Ayed et al. also explored the association between the moment at which maternal infection occurred and the risk of developmental delay and showed that infections in the first and second trimesters were associated with a higher risk of developmental delay than those in the third trimester [44].
Among the studies with comparison groups, Wu et al. described an overall developmental delay in 13.5% of the exposed and 8.1% of the non-exposed infants (p = 0.35); and also a higher proportion of delay in fine motor and personal social skills in the exposed infants at three months of age, although the difference was not statistically significant [39]. Mulkey et al. showed that the proportion of children at risk for developmental delays was higher when they were born to symptomatic mothers compared to asymptomatic mothers or when they were infected after birth in all ASQ domains [49]. Moreover, the authors found an association between maternal symptoms and the risk for global developmental delay (p = 0.04), fine motor delay (p = 0.01), and personal social delay (p = 0.02). Munian et al. did not find differences in overall or specific domain delays when comparing positive and negative exposed neonates using the DP3 questionnaire [47]. Martinez et al. compared the movement patterns of children exposed to SARS-CoV-2 during pregnancy with neurotypical children born before the pandemic using the Motor Optimality Score- Revised (MOS-R) [50]. The authors observed abnormal movement and postural patterns and movement characters more frequently in the exposed children than in the control group (p < 0.001).
Considering the ASQ-3 subdomain scores, Wu et al. found that exposed infants scored significantly lower on gross motor, fine motor, problem-solving, and personal social skills at three months of age [39]. Cheng et al. reported that exposed infants also had lower scores on communication, gross motor, fine motor, problem-solving, and personal-social skills than non-exposed infants between 8 and 10 months of age; however, the difference was not significant [38]. Shuffrey et al. did not find differences in any of the five ASQ-3 subdomain scores when comparing exposed and non-exposed infants [40].
Chinese authors have also performed other analyses considering the association between mother-infant separation duration after birth and ASQ subdomain scores [39, 46]. Communication, gross motor, and personal social domain scores were inversely associated with the duration of mother-infant separation, but no statistical difference was noted in the socio-emotional domain [39, 46].
Shuffrey et al. compared pandemics (exposed and non-exposed) to historical cohorts [40]. Children born during the pandemic had significantly lower scores on gross motor, fine motor, and personal-social skills and a higher proportion of gross motor delay than the historical cohort. Furthermore, infants born to mothers in the first trimester of pregnancy during the first-wave pandemic peak scored lower in gross motor, fine motor, and personal social domains than others.
Neurological exam
All the children assessed by Buonsenso et al. and Munian et al. had normal neurological examination results. Buonsenso et al. assessed postural milestones in infants from 1 to 9 months of age, while Munian et al. assessed passive and active tone and primary reflexes (Amiel-Tison method) at six months of corrected age [47, 48]. Nevertheless, Martinez et al. performed a neurological examination and developmental milestones assessment (CDC tool) in 109 exposed infants between 6 and 8 months of age and found that 12% of them presented developmental delay. In addition, the prevalence of developmental delay among infants exposed to SARS-CoV-2 in the first trimester of gestation was higher than that in other trimesters, although the difference was not statistically significant (p = 0.42) [50].
Audiological assessment
The number of exposed neonates with abnormal audiological evaluation referred to retest and with confirmed abnormal audiological function was comparable to that of non-exposed infants of the same age [45, 47, 48].
Ophthalmological assessment
Regarding structural assessment, all exposed infants presented with age-appropriate retinal development, and no other abnormalities were identified on SD-OCT examination; 15% of them had retinal vascular abnormalities. Behavioral assessment of visual function was normal in 85% of children. Notably, six children (30%) had reduced attention at a distance, while three (15%) had reduced contrast sensitivity [48].
Results of meta-analysis
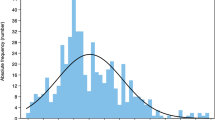
Figure 2 shows the meta-analysis results of the three studies with data on ASQ-3 domains (communication, gross motor, fine motor, problem-solving, and personal social) in comparison groups [38,39,40].
Pooled results from the random-effects model indicated that exposed infants had lower scores on fine motor [MD = -4.70, 95% CI: -8.76; -0.63] and problem-solving [MD = -3.05, 95% CI: -5.88; -0.22] domains than non-exposed infants. There was no difference between the exposed and unexposed infants regarding communication [MD = -3.40, 95% CI: -10.42; 3.63], gross motor skills [MD = -3.16, 95% CI: -6.41; 0.08], and personal-social skills [MD = -1.98, 95% CI: -4.61; 0.66]. The heterogeneity between the studies was moderate for gross motor (I2 = 73%) and problem-solving (I2 = 69%) skills, but high for communication (I2 = 96%), fine motor (I2 = 88%), and personal social (I2 = 80%) skills (Fig. 2).
Discussion
The present rapid review analyzed 10 papers published between 2020 and 2023, selected from more than 2,700 studies identified in the five databases. Although it seems few, it is important to consider that the COVID-19 pandemic was officially recognized in March 2020 [51]. Furthermore, the main outcome analyzed—the development and behavior of infants exposed to SARS-CoV-2 during gestation—is time-consuming, considering the pregnancy duration and the time needed for developmental and behavioral disorders to emerge. It is noteworthy that only one study collected data from low- and middle-income countries (LMIC). The others were predominantly from China, which may not reflect the worldwide phenomenon.
The longest follow-up was 17 months, which may be a very short period, considering that most developmental delays emerge only when children are older [52]. Only four studies compared the exposed infants to a non-exposed control group. The lack of a comparison group made it difficult to determine the effect of gestational exposure from other possible contextual and cultural risk factors. Moreover, children’s development has mostly been assessed using parent-informed screening questionnaires. Only one study has performed a direct observational assessment of the general movements of very young infants. This implies that more information is necessary to confirm the causal relationship between gestational exposure to SARS-CoV-2 and developmental and behavioral disorders. Notably, only two studies included behavioral assessments, and only one had a comparison group.
Buonsenso et al. performed a neurodevelopmental assessment based on postural milestones and auditory and visual function evaluation [48]. The other two studies included an audiological assessment of exposed infants [45, 47]. Sensory integration is primordial to optimal development [53], and the experience with the TORCH infections (toxoplasmosis, “other” infections, rubella, cytomegalovirus, and herpes simplex virus) reinforces the importance of neurosensorial approaches for children exposed to gestational infections [54]. Although the studies analyzed did not demonstrate an association between SARS-CoV-2 gestational infection and neurosensorial outcomes, Martinez et al. observed suboptimal motor development using GMA in infants exposed to SARS-CoV-2 during gestation. GMA is a predictor of motor, cognitive, and neurodevelopmental outcomes, mainly cerebral palsy and neuropsychiatric disorders [50]. Abnormal movements are related to gestational conditions, including infections and maternal stress; however, the authors could not discard the associations between these factors and child motor development [50]. Despite its relevance, these findings should be cautiously interpreted because the comparison group was a selected sample of pre-pandemic neurotypical infants. Furthermore, elevated stress triggered by maternal infection and pandemic circumstances may be involved in GMA results.
None of the three papers that included a non-exposed comparison group demonstrated an association between SARS-CoV-2 gestational exposure and developmental or socio-emotional delays based on ASQ-3 and ASQ:SE [38,39,40]. Of note, two studies investigated the same sample [39, 46]. The 57 exposed infants described by Wang et al. [46] were compared with non-exposed infants in a study by Wu et al. [39]. Wang et al. [46] found a considerable proportion of children at risk for delay, especially in the socio-emotional domain (86.4%). Nevertheless, when compared to the non-exposed sample, there were no differences in the proportion of children with delay between the groups in any of the domains. Mulkley et al. also found a high proportion of children at risk for developmental delays among infants born to symptomatic mothers; however, when compared to those in utero exposed children born to asymptomatic mothers and those infected perinatally, differences were not significant [49]. Thus, these results do not enable us to conclude about the association between SARS-CoV-2 gestational exposure and developmental delay.
Considering the screening test cutoffs, no differences between the exposed and non-exposed children were demonstrated regarding the risk of developmental delays. Nevertheless, the meta-analysis showed that the exposed infants had lower fine motor and problem-solving scores than the non-exposed infants. Individually, the papers reported divergent results. Wu et al. [39] found that 3-month-old exposed infants had lower scores in gross motor, fine motor, problem-solving, and personal social skills than non-exposed infants. Shuffrey et al. [40] assessed infants at six months of age and did not find the same tendency. Cheng et al. [38] assessed infants between eight and ten months old, and at this age, exposed infants had lower scores than non-exposed infants only in the fine motor subdomain. Although the studies included in the meta-analysis [38,39,40] used the same instrument and design, the heterogeneity was moderate to high. This could be related to differences in the sample size and age range at the time of assessment [43]. Populational studies demonstrate that the prevalence of developmental delay increases with children’s age [55]; thus, these initial results highlight the need for long-term follow-up studies to clarify the present research question.
The timing of infection is an important factor that may be associated with the offspring outcomes in gestational infections [15]. Most mothers in the included studies were infected during the third gestational trimester. The timing of maternal SARS-CoV-2 infection was associated with developmental outcomes reported by Shuffrey et al. [40]. However, Ayed et al. and Martinez et al. found a higher proportion of children at risk for developmental delay when they were exposed early in pregnancy, although only Ayed et al. demonstrated a significant association [39, 50]. A recent study examining fresh tissues of human fetuses aged 9–21 post-conception weeks reported SARS-CoV-2 infection in the fetal brain associated with hemorrhage, disrupted endothelial integrity, and infiltration of immune cells in the developing cortex [13]. Nevertheless, the authors highlighted that it is still unclear whether these findings are due to a direct effect of SARS-CoV-2 infection or a consequence of MIA. Most fetuses with cerebral hemorrhages were between 12 and 14 weeks of gestation, a critical window of human fetal brain development when endothelial tight junctions increase to form the blood–brain barrier [13]. Conversely, Bard et al. concluded that the risk of adverse obstetric and neonatal outcomes, many of which are somewhat related to brain development, is higher when SARS-CoV-2 infects mothers during the late second and third trimesters of gestation [15]. Immunological and inflammatory events related to SARS-CoV-2 infection during pregnancy are complex and not completely understood [8, 18].
Many other factors, such as placenta maturity, the developmental stage of the fetus’s central nervous system at the moment of maternal infection, the viral load and variants, and the COVID-19 clinical presentation, would theoretically modify developmental outcomes [10, 15, 56,57,58,59,60]. Regarding the severity of maternal disease, most mothers in the analyzed studies were asymptomatic or had mild COVID-19 symptoms. Shuffrey et al. found no association between the severity of maternal disease and child developmental outcomes [40]. However, Mulkey et al., analyzing a very small sample of neonates exposed to SARS-CoV-2 in utero and after birth, demonstrated a higher proportion of infants at risk for developmental delay among symptomatic mothers [49]. Nevertheless, the authors highlighted that 31 of the 34 neonates were admitted to the NICU, which may be a confounder because it indicates other clinical events possibly associated with adverse developmental outcomes. Unfortunately, most of the studies included in the present review did not explore many of these aspects, limiting their conclusions.
Beyond SARS-CoV-2’s direct effect on mothers and infants, it is crucial to recognize the potential impact of the pandemic on the children’s development and behavior [22, 25, 27]. Shuffrey et al.’s primary analysis showed no association between SARS-CoV-2 infection, timing, or disease severity and ASQ-3 scores [40]. Nevertheless, when the pooled healthy infants born during the pandemic cohort were compared to a historical cohort, the authors observed significant differences between the groups in the gross motor, fine motor, and personal social domains. These findings agree with Huang et al. results, which used the ASQ-3 to compare children born during the pandemic to a historical cohort [61]. In this paper, 12-month-old children from the pandemic cohort had lower scores in the fine motor and communication domains than those from the historical cohort, implying that the “pandemic context” cannot be neglected. Thus, special attention to mother–child mental health and socioeconomic disparities must be universally assured through integral and nurturing care, aiming to mitigate the long-term effects of the pandemic on humanity.
Finally, Chinese studies have analyzed the impact of mother-newborn separation on child outcomes [39, 46]. It is noteworthy that early in the pandemic, international protocols recommended that SARS-CoV-2-infected mothers be kept apart from their newborns immediately after birth [7]. At that time, a meta-analysis of 176 published cases of neonatal SARS-CoV-2 infections concluded that mother-neonate rooming-in increased the incidence of neonatal infection fourfold in the first three days after birth [8]. Wang et al. and Wu et al. demonstrated that the negative developmental outcomes of children exposed to SARS-Cov-2 during pregnancy were moderated by the duration of mother–child separation, confirming that this protocol was more deleterious than helpful for many child outcomes [39, 46].
Concerning sensorial assessments, studies have shown that referral and confirmed auditory disorder rates among exposed infants were similar to the overall global incidence [45, 47, 48, 62]. This tendency was similar to that reported by Ghiselli et al., although previous studies documented a high rate of infants exposed to SARS-CoV-2 during gestation who were referred for a retest [63, 64]. The retinal vascular problems identified by Buonsenso et al. [48] in a small sample of children exposed to SARS-CoV-2 during gestation were also described by Kiappe et al. [65]. Despite being incipient, these preliminary results highlight the need for neurosensory assessments and multidisciplinary follow-up of prenatally exposed infants.
To the best of our knowledge, this is the first study to review the potential impact of gestational exposure to SARS-CoV-2 on child development and behavior. Although we followed the recommended and updated protocols to conduct the present review and performed a meta-analysis, some limitations should be considered. We aimed to perform a rapid review; thus, we searched a limited number of databases and did not include preprint papers.Therefore, there is a chance that some studies were missed. The meta-analysis results of the communication and personal-social domains should be interpreted cautiously, as the overall effect test was higher than the recommended cutoffs.
Future research should investigate the impact of gestational exposure in other contexts, mainly in low- and middle-income countries, where the pandemic has deepened social inequalities and raised many environmental stressors. Furthermore, the use of observational techniques to assess child development with longer follow-up periods, as well as considering the clinical features of maternal infection, would provide more evidence of the impact of SARS-CoV-2 gestational exposure.
Although some clues have been raised, the present systematic review did not find sufficient evidence to confirm the association between SARS-CoV-2 gestational exposure and neurodevelopmental delays. However, the meta-analysis indicated that gestational exposure negatively affected fine motor and problem-solving skills. Robust evidence on this topic is still incipient, and the available studies present methodological inconsistencies that limit the drawing of clear-cut conclusions.
Availability of data and materials
The datasets generated and/or analyzed are available from the corresponding author upon reasonable request.
Abbreviations
- ABR:
-
Auditory Brainstem Response
- ASQ-3:
-
Ages and Stages Questionnaires, Third Edition
- ASQ: SE-2:
-
Ages and Stages Questionnaires: Social-Emotional, Second Edition
- CDC-DM:
-
Centers on Disease Control -Developmental Milestones
- CM:
-
Communication
- DD:
-
Developmental Delay
- DP3:
-
Developmental Profile 3
- FFA:
-
Retinal ultra-widefield fluorescein angiography
- FM:
-
Fine motor
- GM:
-
Gross motor
- GMA:
-
General Movement Assessment
- LMIC:
-
Low- and middle-income countries
- MeSH:
-
Medical Subject Headings
- MIA:
-
Maternal immune activation
- MOOSE:
-
Meta-Analyses of Observational Studies in Epidemiology
- MOS-R:
-
Motor Optimality Score – Revised
- NOS:
-
Newcastle-Ottawa Quality Assessment Scale
- PBS:
-
Problem-solving
- PCR:
-
Polymerase chain reaction
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- PS:
-
Personal-social
- SD-OCT:
-
Spectral Domain Optical Coherence Tomography
- SE:
-
Socio-emotional
- SWiM:
-
Synthesis Without Meta-Analysis
- TEOAE:
-
Transient Evoked Otoacoustic Emissions
- TORCH:
-
Toxoplasmosis, “other” infections, rubella, cytomegalovirus, and herpes simplex virus
References
WHO (2022) COVID cases and deaths with age and sex reported. https://app.powerbi.com/view?r=eyJrIjoiYWRiZWVkNWUtNmM0Ni00MDAwLTljYWMtN2EwNTM3YjQzYmRmIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9
Overton EE, Goffman D, Friedman AM (2021) The Epidemiology of COVID-19 in Pregnancy. Clin Obstet Gynecol 65:110–122
Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Tong VT et al (2020) Update: Characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status — United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep 69:1641–1647
Allotey J, Chatterjee S, Kew T, Gaetano A, Stallings E, Fernández-García S et al (2022) SARS-CoV-2 positivity in offspring and timing of mother-to-child transmission: Living systematic review and meta-analysis on behalf of the PregCOV-19 Living Systematic Review Consortium. BMJ 1–11
Pinheiro GSMA, Azevedo VMGO, Bentes AA, Januário GC, Januário JN, Cintra ML et al (2022) Serological survey for IgG antibodies against SARS-CoV-2 from newborns and their mothers. Cad Saude Publica 38:e00021022
Kotlyar AM, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, Tal O et al (2021) Vertical transmission of coronavirus disease 2019. Am J Obstet Gynecol 224:35–53
WHO (2021) Definition and categorization of the timing of mother-to-child transmission of SARS-CoV-2
Raschetti R, Vivanti AJ, Vauloup-Fellous C, Loi B, Benachi A, de Luca D (2020) Synthesis and systematic review of reported neonatal SARS-CoV-2 infections. Nat Commun 11:1
Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, do Cao J et al (2020) Transplacental transmission of SARS-CoV-2 infection. Nat Commun 11:1
Garcia-Flores V, Romero R, Xu Y, Theis KR, Arenas-Hernandez M, Miller D et al (2022) Maternal-fetal immune responses in pregnant women infected with SARS-CoV-2. Nat Commun 13:320
Lu-Culligan A, Chavan AR, Vijayakumar P, Irshaid L, Courchaine EM, Milano KM et al (2021) Maternal respiratory SARS-CoV-2 infection in pregnancy is associated with a robust inflammatory response at the maternal-fetal interface. Med (N Y) 2:591-610.e10
Shook LL, Sullivan EL, Lo JO, Perlis RH, Edlow AG (2022) COVID-19 in pregnancy: Implications for fetal brain development. Trends Mol Med 28:319–330
Massimo M, Barelli C, Moreno C, Collesi C, Holloway RK, Crespo B et al (2023) Haemorrhage of human foetal cortex associated with SARS-CoV-2 infection. Brain awac372
Han VX, Patel S, Jones HF, Dale RC (2021) Maternal immune activation and neuroinflammation in human neurodevelopmental disorders. Nat Rev Neurol 17:564–579
Badr DA, Picone O, Bevilacqua E, Carlin A, Meli F, Sibiude J et al (2021) Severe acute respiratory syndrome coronavirus 2 and pregnancy outcomes according to gestational age at time of infection. Emerg Infect Dis 27:2535–2543
Marchand G, Patil AS, Masoud AT, Ware K, King A, Ruther S et al (2022) Systematic review and meta-analysis of COVID-19 maternal and neonatal clinical features and pregnancy outcomes up to June 3, 2021. AJOG Glob Rep 2:100049
Woodworth KR, Olsen EO, Neelam V, Lewis EL, Galang RR, Oduyebo T et al (2020) Birth and infant outcomes following laboratory-confirmed SARS-CoV-2 infection in pregnancy — SET-NET, 16 jurisdictions, March 29–October 14, 2020. MMWR Morb Mortal Wkly Rep 69:1635–1640
Vivanti AJ, Vauloup-Fellous C, Escourrou G, Rosenblatt J, Jouannic JM, Laurent-Bellue A, De Luca D (2022) Factors associated with SARS-CoV-2 transplacental transmission. Am J Obstet Gynecol 227:541–543
Jash S, Sharma S (2022) Pathogenic infections during pregnancy and the consequences for fetal brain development. Pathogens 11:193
Provenzi L, Grumi S (2022) The need to study developmental outcomes of children born during the COVID-19 pandemic. JAMA Pediatr 176:103
McCarthy J, Liu D, Kaskel F (2021) The need for life-course study of children born to Mothers With Prior COVID-19 infection. JAMA Pediatr 175:1097–1098
Brien ME, Bouron-Dal Soglio D, Dal Soglio S, Couture C, Boucoiran I, Nasr Y et al (2021) Pandemic stress and SARS-CoV-2 infection are associated with pathological changes at the maternal-fetal interface. Placenta 115:37–44
Venta A, Bick J, Bechelli J (2021) COVID-19 threatens maternal mental health and infant development: Possible paths from stress and isolation to adverse outcomes and a call for research and practice. Child Psychiatry Hum Dev 52:200–204
Premji S (2014) Perinatal distress in women in low- and middle-income countries: Allostatic load as a framework to examine the effect of perinatal distress on preterm birth and infant health. Matern Child Health J 18:2393–2407
Firestein MR, Dumitriu D, Marsh R, Monk C (2022) Maternal mental health and infant development during the COVID-19 pandemic. JAMA Psychiat 79:1040–1045
Monk C, Lugo-Candelas C, Trumpff C (2019) Prenatal developmental origins of future psychopathology: Mechanisms and pathways. Annu Rev Clin Psychol 15:317–344
Kolker S, Biringer A, Bytautas J, Blumenfeld H, Kukan S, Carroll JC (2021) Pregnant during the COVID-19 pandemic: An exploration of patients’ lived experiences. BMC Pregnancy Childbirth 21:851
Duguay G, Garon-Bissonnette J, Lemieux R, Dubois-Comtois K, Mayrand K, Berthelot N (2022) Socioemotional development in infants of pregnant women during the COVID-19 pandemic: The role of prenatal and postnatal maternal distress. Child Adolesc Psychiatry Ment Health 16:28
Machado MMT, Rocha HAL, Castro MC, Sampaio EGM, Oliveira FA, da Silva JPFD et al (2021) COVID-19 and mental health of pregnant women in Ceará. Brazil Rev Saude Publica 55:37
Zeng LK, Zhu HP, Xiao TT, Peng SC, Yuan WH, Shao JB et al (2021) Short-term developmental outcomes in neonates born to mothers with COVID-19 from Wuhan. China World J Pediatr 17:253–262
Ryan L, Plötz FB, van den Hoogen A, Latour JM, Degtyareva M, Keuning M et al (2022) Neonates and COVID-19: State of the art Neonatal Sepsis series. Pediatr Res 91:432–439
Aromataris E, Munn Z, editor (2020) JBI manual for evidence synthesis. JBI
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–12
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S et al (2020) Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 368:l6890
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA et al (2020) statement: An updated guideline for reporting systematic reviews. Syst Rev 2021:10
Lipkin PH, Macias MM (2020) Promoting Optimal Development: Identifying Infants and young children with developmental disorders through developmental surveillance and screening. Pediatrics 145
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:210
Cheng Y, Teng H, Xiao Y, Yao M, Yin J, Sun G (2021) Impact of SARS-CoV-2 infection during pregnancy on infant neurobehavioral development: A case-control study. Front Pediatr 9:762684
Wu T, Chen L, Wang Y, Shi H, Niu J, Yin X et al (2021) Effects of SARS-CoV-2 infection during late pregnancy on early childhood development: A prospective cohort study. Front Pediatr 9:750012
Shuffrey LC, Firestein MR, Kyle MH, Fields A, Alcántara C, Amso D et al (2022) Association of birth during the COVID-19 pandemic with neurodevelopmental status at 6 months in infants with and without in utero exposure to maternal SARS-CoV-2 infection. JAMA Pediatr 176:e215563
SB GW, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The newcastle-ottawa score for non-randomized studies. http://www.ohri.ca
Review Manager (RevMan) [Computer program] (2020) Version 5.4, The Cochrane Collaboration. https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman. Accessed 13 Nov 2022
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al (2022) Cochrane Handbook for Systematic Reviews of Interventions version 6.3. Cochrane. p. 2022; updated February 2022. www.training.cochrane.org/handbook. Accessed 13 Nov 2022
Ayed M, Embaireeg A, Kartam M, More K, Alqallaf M, Alnafisi A et al (2022) Neurodevelopmental outcomes of infants born to mothers with SARS-CoV-2 infections during pregnancy: A national prospective study in Kuwait. BMC Pediatr 22:319
Schuh TL, Mithal LB, Naureckas S, Miller ES, Garfield CF, Shah MD (2022) Outcomes from birth to 6 months of publicly insured infants born to mothers with severe acute respiratory syndrome coronavirus 2 infection in the United States. J Perinat Med 50:334–342
Wang Y, Chen L, Wu T, Shi H, Li Q, Jiang H et al (2020) Impact of Covid-19 in pregnancy on mother’s psychological status and infant’s neurobehavioral development: A longitudinal cohort study in China. BMC Med 18:1–10
Munian D, Das R, Hazra A, Ray S (2021) Outcome of neonates born to COVID-positive women at 6 months of age. Indian Pediatr 58:853–856
Buonsenso D, Costa S, Giordano L, Priolo F, Colonna AT, Morini S et al (2022) Short- and mid-term multidisciplinary outcomes of newborns exposed to SARS-CoV-2 in utero or during the perinatal period: Preliminary findings. Eur J Pediatr 181:1507–1520
Mulkey SB, Williams ME, Jadeed N, Zhang A, Israel S, DeBiasi RL (2022) Neurodevelopment in infants with antenatal or early neonatal exposure to SARS-CoV-2. Early Human Dev 175:105694
Martinez FV, Zhang D, Paiola S, Mok T, Cambou MC, Kerin T et al (2023) Neuromotor repertoires in infants exposed to maternal COVID-19 during pregnancy: a cohort study. BMJ Open 13:e069194
WHO, director (2020) General’s opening remarks at the media briefing on COVID-19. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 13 Nov 2022
Iverson JM (2021) Developmental variability and developmental cascades: Lessons from motor and language development in infancy. Curr Dir Psychol Sci 30:228–235
Section On Complementary And Integrative Medicine, Council on Children with Disabilities, American Academy of Pediatrics, Zimmer M, Desch L (2012) Sensory integration therapies for children with developmental and behavioral disorders. Pediatrics 129:1186–9
Muldoon KM, Fowler KB, Pesch MH, Schleiss MR (2020) SARS-CoV-2: Is it the newest spark in the TORCH? J Clin Virol 127:104372
Correia LL, Rocha HAL, Sudfeld CR, Rocha SGMO, Leite ÁJM, Campos JS et al (2019) Prevalence and socioeconomic determinants of development delay among children in Ceará, Brazil: A population-based study. PLoS ONE 14:e0215343
Smith LH, Dollinger CY, Vanderweele TJ, Wyszynski DF, Hernández-Díaz S (2022) Timing and severity of COVID-19 during pregnancy and risk of preterm birth in the International Registry of coronavirus Exposure in Pregnancy. BMC Pregnancy Childbirth 22:775
Ostrander B, Bale JF (2019) Congenital and perinatal infections. In: Handb Clin Neurol. Elsevier B.V 162:133–53
Racicot K, Mor G (2017) Risks associated with viral infections during pregnancy. J Clin Invest 127:1591–1599
Choi H, Lee EJ, Ahn YS, Yoo YM (2022) Effects of the Omicron variant on perinatal outcomes in full-term neonates. BMC Pediatr 22:625
Strid P, Zapata LB, Tong VT, Zambrano LD, Woodworth KR, Riser AP, Galang RR, Gilboa SM, Ellington SR (2022) Coronavirus Disease 2019 (COVID-19) Severity Among Women of Reproductive Age With Symptomatic Laboratory-Confirmed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection by Pregnancy Status-United States, 1 January 2020-25 December 2021. Clin Infect Dis 75(Suppl 2):S317
Huang P, Zhou F, Guo Y, Yuan S, Lin S, Lu J et al (2021) Association between the COVID-19 pandemic and infant neurodevelopment: A comparison before and during COVID-19. Front Pediatr 9:662165
The Joint Committee on Infant Hearing (2019) position statement: principles and guidelines for early hearing detection and intervention programs. 2019
Alan MA, Alan C (2021) Hearing screening outcomes in neonates of SARS-CoV-2 positive pregnant women. Int J Pediatr Otorhinolaryngol 146:110754
Celik T, Simsek A, Koca CF, Aydin S, Yasar S (2021) Evaluation of cochlear functions in infants exposed to SARS-CoV-2 intrauterine. Am J Otolaryngol 42:102982
Kiappe OP, Santos da Cruz NF, Rosa PAC, Arrais L, Bueno de Moraes NS (2021) Ocular Assessments of a Series of Newborns Gestationally Exposed to Maternal COVID-19 Infection. JAMA Ophthalmol 139(7):777–780
Acknowledgements
We acknowledge the National Council for Scientific and Technological Development (CNPq), Coordination for the Improvement of Higher Education Personnel (CAPES) and the Research Support Foundation of the State of Minas Gerais (FAPEMIG) for funding the present project. We would like to thank Editage (www.editage.com) for the English language editing.
Funding
This study was supported by grants from the National Council for Scientific and Technological Development (CNPq), Coordination for the Improvement of Higher Education Personnel (CAPES) and the Research Support Foundation of the State of Minas Gerais (FAPEMIG).
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. GSMAP and RCS screened the retrieved studies. GSMAP, RCS, and NSG analyzed the data, and VMGOA, SMAL, and CRLA took the lead in writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pinheiro, G.S.M.A., de Souza, R.C., de Oliveira Azevedo, V.M.G. et al. Effects of intrauterine exposure to SARS-CoV-2 on infants’ development: a rapid review and meta-analysis. Eur J Pediatr 182, 2041–2055 (2023). https://doi.org/10.1007/s00431-023-04910-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04910-8