Abstract
This study aims to determine the association of small for gestational age (SGA) and large for gestational age (LGA) at birth with hospital readmission after postpartum discharge for up to 28 days of delivery. This is a population-based, data-linkage study using the French National Uniform Hospital Discharge Database. “Healthy” singleton term infants born between January 1st, 2017, and November 30th, 2018, in the French South region were included. SGA and LGA were defined as birth weight < 10th and > 90th percentiles, respectively, according to sex and gestational age. A multivariable regression analysis was performed. Among 67,359 included infants, 2441 (3.6%) were readmitted, and 61% of them were hospitalized within 14 days postpartum. Hospitalized infants were more likely to be LGA at birth (10.3% vs. 8.6% in non-hospitalized infants, p < 0.01); the proportion of SGA infants did not differ between both groups. Compared to appropriate birth weight for GA (AGA) infants, LGA infants were more often hospitalized for infectious diseases (57.7% vs. 51.3%, p = 0.05). After regression analysis, LGA infants had a 20% higher odds of being hospitalized than those born AGA (aOR (95%CI) = 1.21 (1.06–1.39)), while aOR (95%CI) for SGA was 1.11 (0.96–1.28).
Conclusion: In contrast to SGA, LGA was associated with hospital readmission during the first month of life. Follow-up protocols that include LGA should be evaluated.
What is Known: • Newborns are at high risk of hospital readmission during the postpartum period. • However, the influence of appropriateness for gestational age at birth, i.e. being born small for gestational age (SGA) or large for gestational age (LGA), has been little evaluated. | |
What is New: • In contrast to SGA born infants, we found that infants born LGA were at high risk of hospital admission and the main cause was infectious diseases. • This population should be considered at risk of early adverse outcomes and should require attentive medical follow-up after postpartum discharge. |


Similar content being viewed by others
Data availability
The French National Uniform Hospital Discharge Database data can only be accessed through a secure server after obtaining requisite ethical and data protection authorizations. The data are available upon request from the authors.
References
Ellberg L, Högberg U, Lundman B et al (2008) Maternity care options influence readmission of newborns. Acta Paediatr 97:579–583
Shakib J, Buchi K, Smith E et al (2015) Timing of initial well-child visit and readmissions of newborns. Pediatrics 135:469–474
Boubred F, Herlenius E, Andres V et al (2016) Hospital readmission after postpartum discharge of term newborns in two maternity wards in Stockholm and Marseille. Arch Pediatr 23:234–240
Jones E, Stewart F, Taylor B et al (2021) Early postnatal discharge from hospital for healthy mothers and term infants. Cochr Data Syst Rev 6:CD002958
Srinivasjois R, Slimings C, Einarsdottir K et al (2015) Association of gestational age at birth with reasons for subsequent hospitalisation: 18 years of follow-up in a Western Australian population study. PLoS One 10
Lain SJ, Nassar N, Bowen J et al (2013) Risk factors and costs of hospital admissions in first year of life: a population-based study. J Pediatr 163:1014–1019
Batu ED, Yeni S, Teksam O (2015) The factors affecting neonatal presentations to the pediatric emergency department. J Emerg Med 48:542–547
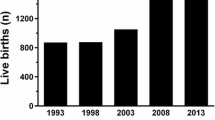
Surkan PJ, Hsieh CC, Johansson A et al (2004) Reasons for increasing trends in large for gestational age births. Obstet Gynecol 104:720–726
Henriksen T (2008) The macrosomic fetus: a challenge in current obstetrics. Acta Obstetricia Gynecologica Scandinavica 87:134–145
Chiavaroli V, Castorani V, Guidone P et al (2016) Incidence of infants born small- and large-for-gestational-age in an Italian cohort over a 20-year period and associated risk factors. Ital J Pediatr 42:42
Ehrenberg HM, Mercer BM, Catalano PM (2004) The influence of obesity and diabetes on the prevalence of macrosomia. Am J Obstet Gynecol 191:964–968
Bao C, Zhou Y, Jiang L et al (2011) Reasons for the increasing incidence of macrosomia in Harbin, China: increasing incidence of macrosomia in China. BJOG 118:93–98
Goldstein RF, Abell SK, Ranasinha S et al (2017) Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA 317:2207–2225
Kramer MS, Morin I, Yang H et al (2002) Why are babies getting bigger? Temporal trends in fetal growth and its determinants. J Pediatr 141:538–542
Boubred F, Pauly V, Romain F et al (2020) The role of neighbourhood socioeconomic status in large for gestational age. PLoS ONE 15:e0233416
Weissmann-Brenner A, Simchen MJ, Zilberberg E et al (2012) Maternal and neonatal outcomes of large for gestational age pregnancies. Acta Obstetricia and Gynecologica Scandinavica 91:844–849
Chauhan SP, Rice MM, Grobman WA et al (2017) Neonatal morbidity of small- and large-for-gestational-age neonates born at term in uncomplicated pregnancies. Obstet Gynecol 130:511–519
Ludvigsson JF, Lu D, Hammarström L et al (2018) Small for gestational age and risk of childhood mortality: a Swedish population study. PLoS Med 15:e1002717
Paranjothy S, Dunstan F, Watkins WJ et al (2013) Gestational age, birthweight, and risk of respiratory hospital admission in childhood. Pediatrics 132:e1562–9
Serrano-Lomelin J, Hicks A, Kumar M et al (2021) Patterns of respiratory health services utilization from birth to 5 years of children who experienced adverse birth outcomes. PLoS ONE 16:e0247527
Boudemaghe T, Belhadj I (2017) Data resource profile: the French national uniform hospital discharge data set database (PMSI). Intern J Epidemiol 46:392-d
Hascoët JM, Petitprez K (2014) Maternal discharge: conditions and organization for mothers and newborns returning home. The French National Authority for Health recommendations update. Arch Pediatr 21:1053–1059
Laugier O, Garcia P, Boucékine M et al (2017) Influence of socioeconomic context on the rehospitalization rates of infants born preterm. J Pediatr 190:174-179.e1
Dietz PM, Rizzo JH, England LJ et al (2013) Health care utilization in the first year of life among small- and large- for-gestational age term Infants. Matern Child Health J 17:1016–1024
Khambalia AZ, Algert CS, Bowen JR et al (2017) Long-term outcomes for large for gestational age infants born at term. J Paediatr Child Health 53:876–881
Bedell S, Hutson J, de Vrijer B et al (2021) Effects of maternal obesity and gestational diabetes mellitus on the placenta: current knowledge and targets for therapeutic interventions. Curr Vasc Pharmacol 19:176–192
Parisi F, Milazzo R, Savasi VM et al (2021) Maternal low-grade chronic inflammation and intrauterine programming of health and disease. Int J Mol Sci 22:1732
Vieira MC, McCowan LME, North RA et al (2018) Antenatal risk factors associated with neonatal morbidity in large-for-gestational-age infants: an international prospective cohort study. Acta Obstet Gynecol Scand 97:1015–1024
Perez M, Robbins ME, Revhaug C et al (2019) Oxygen radical disease in the newborn, revisited: oxidative stress and disease in the newborn period. Free Radical Biol Med 142:61–72
Author information
Authors and Affiliations
Contributions
Nimal Marion and Camille Ravel designed the data collection, analysed the data, drafted the initial manuscript, and reviewed and revised the manuscript. Steve Nauleau and David Lapidus designed the data collection instruments, collected data, and carried out the initial analyses. Clotilde Des Robert and Sophie Tardieu conceptualized and designed the study, and Farid Boubred conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is an observational study using the data from the French National Uniform Hospital Discharge Database (Programme de Médicalisation du Système d’Information (PMSI)). All data are fully anonymized; informed written patient consent and ethical committee approval are not required in accordance of the French law after a deliberation of the French Commission for Data Protection and Liberties (CNIL) with the methodological reference MR005. All French regulations have been respected.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nimal, M., Ravel, C., Nauleau, S. et al. Relationship between large and small for gestational age and hospital readmission after postpartum discharge: a population-based, data-linkage study. Eur J Pediatr 182, 2245–2252 (2023). https://doi.org/10.1007/s00431-023-04908-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04908-2