Abstract
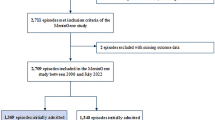
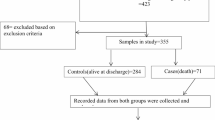
Brain abscess is a rare but life-threatening complication of meningitis. The purpose of this study was to identify clinical features and potentially relevant factors of brain abscess in neonates with meningitis. This study was a propensity score–matched case–control study of neonates with brain abscess and meningitis in a tertiary pediatric hospital between January 2010 and December 2020. A total of 16 neonates with brain abscess were matched to 64 patients with meningitis. Demography, clinical characteristics, laboratory results, and pathogens were collected. Conditional logistic regression analyses were performed to identify the independent risk factors associated with brain abscess. The most common pathogen we found in the brain abscess group was Escherichia coli. Risk factors of brain abscess were identified: multidrug-resistant bacterial infection (OR, 11.204; 95% CI, 2.315–54.234; p = 0.003), C-reactive protein (CRP) > 50 mg/L (OR, 11.652; 95% CI, 1.799–75.470; p = 0.010).
Conclusion: The risk factors of brain abscess are multidrug-resistant bacterial infection and CRP > 50 mg/L. Monitoring the level of CRP is essential. Bacteriological culture and rational use of antibiotics are necessary for the prevention of MDR bacterial infection as well as the occurrence of brain abscess.
What is Known: • Morbidity and mortality of neonatal meningitis have declined, but brain abscess associated with neonatal meningitis is still life-threatening. | |
What is New: • This study investigated relevant factors related to brain abscess. • It is important for neonatologists to perform prevention, early identification, and appropriate interventions for neonates with meningitis. |

Similar content being viewed by others
Data availability
The data is available on demand.
Code availability
Not applicable.
Abbreviations
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- CRP:
-
C-reactive protein
- CLSI:
-
Clinical and Laboratory Standards Institute
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MDR:
-
Multi-drug resistant
- NEC:
-
Necrotizing enterocolitis of newborn
- ORs:
-
Odds ratios
- PICC:
-
Peripherally inserted central catheter
- PCT:
-
Procalcitonin
- PROM:
-
Premature rupture of membranes
- sPDA:
-
Symptomatic patent ductus arteriosus
- TPN:
-
Total parenteral nutrition
- WBC:
-
White blood cell
- VLBW:
-
Very low birth weight
References
Ouchenir L, Renaud C, Khan S et al (2017) The epidemiology, management, and outcomes of bacterial meningitis in infants. Pediatrics 140:e20170476. https://doi.org/10.1542/peds.2017-0476.
Pareek P, Gupta B, Chetan C et al (2020) Burkholderia cepacia brain abscess in a term neonate. Indian J Pediatr 87:478–479. https://doi.org/10.1007/s12098-019-03156-3
Sahbudak Bal Z, Eraslan C, Bolat E et al (2018) Brain abscess in children: a rare but serious infection. Clin Pediatr (Phila) 57:574–579. https://doi.org/10.1177/0009922817733301
Giovane RA, Lavender PD (2018) Central nervous system infections. Prim Care 45:505–518. https://doi.org/10.1016/j.pop.2018.05.007
Gilard V, Beccaria K, Hartley JC et al (2020) Brain abscess in children, a two-center audit: outcomes and controversies. Arch Dis Child 105:288–291. https://doi.org/10.1136/archdischild-2018-316730
Ming K, Rosenbaum PR (2000) Substantial gains in bias reduction from matching with a variable number of controls. Biometrics 56(1):118–124. https://doi.org/10.1111/j.0006-341x.2000.00118.x
Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD (2014) Early-onset neonatal sepsis. Clin Microbiol Rev 27(1):21–47
Felsenstein S, Williams B, Shingadia D, Coxon L, Riordan A, Demetriades AK, Chandler CL, Bassi S, Koutoumanou E, Stapleton S, Sharland M, Bryant PA (2013) Clinical and microbiologic features guiding treatment recommendations for brain abscesses in children. Pediatr Infect Dis J 32(2):129–135. https://doi.org/10.1097/INF.0b013e3182748d6e
Özsürekci Y, Kara A, Cengiz AB, Çelik M, ÖzkayaParlakay A, Karadağ-Öncel E, Ceyhan M (2012) Brain abscess in childhood: a 28-year experience. Turk J Pediatr 54(2):144–149
Raffaldi I, Garazzino S, Castelli GG, Lipreri R, Lancella L, Esposito S, Giannini AM, Montagnani C, Marseglia GL, Pignata C, Bernardi F, Tovo PA (2017) Sitip Brain Abscesses Registry. Brain abscesses in children: an Italian multicentre study. Epidemiol Infect 145(13):2848–2855. https://doi.org/10.1017/S0950268817001583
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Magiorakos AP, Srinivasan A, Carey RB et al (2012). Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. J Clin Microbiol Infect 18:268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Masand R, Ali A, Purohit A (2015) Neonatal brain abscess: an typical presentation. J Pediatr Neurosci 10:282–284. https://doi.org/10.4103/1817-1745.165722
Angus DC, van der Poll T (2013) Severe sepsis and septic shock. N Engl 369:840–51. https://doi.org/10.1056/NEJMra1208623
Emami CN, Petrosyan M, Giuliani S (2009) Role of the host defense system and intestinal microbial flora in the pathogenesis of necrotizing enterocolitis. Surg Infect (Larchmt) 10:407–417. https://doi.org/10.1089/sur.2009.054
Brunengraber LN, Robinson AV, Chwals WJ (2009) Relationship of serum C-reactive protein and blood glucose levels with injury severity and patient morbidity in a pediatric trauma population. J Pediatr Surg 44:992–996. https://doi.org/10.1016/j.jpedsurg.2009.01.043
Al-Baradie RS, Pu S, Liu D, Zeinolabediny Y et al (2021) Monomeric C-reactive protein localized in the cerebral tissue of damaged vascular brain regions is associated with neuro-inflammation and neurodegeneration-an immunohistochemical study. Front Immunol 12:644213. https://doi.org/10.3389/fimmu.2021.644213
Neidert MC, Karlin K, Actor B et al (2015) Preoperative C-reactive protein predicts the need for repeated intracerebral brain abscess drainage. Clin Neurol Neurosurg 131:26–30. https://doi.org/10.1016/j.clineuro.2015.01.015
Brouwer MC, Coutinho JM, van de Beek D (2014) Clinical characteristics and outcome of brain abscess. Systematic review and meta-analysis. Neurology 82:806–813. https://doi.org/10.1212/WNL.0000000000000172
Shachor-Meyouhas Y, Bar-Joseph G, Guilburd JN, Lorber A, Hadash A, Kassis I (2010) Brain abscess in children-epidemiology, predisposing factors and management in the modern medicine era. Acta Paediatr 99(8):1163–1167. https://doi.org/10.1111/j.1651-2227.2010.01780.x
Lee CG, Kang SH, Kim YJ, Shin HJ, Choi HS, Lee JH, Lee MH (2010) Brain abscess in Korean children: a 15-year single center study. Korean J Pediatr 53(5):648–652. https://doi.org/10.3345/kjp.2010.53.5.648
Dubos F, De La Rocque F, Levy C et al (2008) Sensitivity of the bacterial meningitis score in 889 children with bacterial meningitis. J Pediatr 152:378–82
Renier D, Flandin C, Hirsch E et al (1988) Brain abscess in neonates: a study of 30 cases. J Neurosurg 69:877–82. https://doi.org/10.3171/jns.1988.69.6.0877
Kline MW (1988) Citrobacter meningitis and brain abscess in infancy: epidemiology, pathogenesis, and treatment. J Pediatr 113:430–4. https://doi.org/10.1016/s0022-3476(88)80623-1
Makhoul IR, Epelman M, Kassis I et al (2002) Escherichia coli brain abscess in a very low birth weight premature infant. Isr Med Assoc J 4:727–728
Ku LC, Boggess KA, Cohen-Wolkowiez M et al (2015) Bacterial meningitis in infants. Clin Perinatol 42:29–45, vii-viii. https://doi.org/10.1016/j.clp.2014.10.004
Issa E, Salloum T, Tokajian S (2020) From normal flora to brain abscesses: a review of Streptococcus intermedius. Front Microbiol 11:826. https://doi.org/10.3389/fmicb.2020.00826
Otto M (2012) MRSA virulence and spread. Cell Microbiol 14(10):1513–21. https://doi.org/10.1111/j.1462-5822.2012.01832.x
Tompkins K, van Duin D (2021) Treatment for carbapenem-resistant Enterobacterales infections: recent advances and future directions. Eur J Clin Microbiol Infect Dis 40(10):2053–2068. https://doi.org/10.1007/s10096-021-04296-1
Tompkins K, Duin DV (2021) Treatment for carbapenem‑resistant Enterobacterales infections: recent advances and future directions. Eur J Clin Microbiol Infect Dis. 40(10):2053–2068. https://doi.org/10.1007/s10096-021-04296-1
Kielian T (2004) Immunopathogenesis of brain abscess. J Neuroinflammation 1:16. https://doi.org/10.1186/1742-2094-1-16
Grumann D, Nübel U, Bröker BM (2014) Staphylococcus aureus toxins—their functions and genetics. Infect Genet Evol 21:583–92. https://doi.org/10.1016/j.meegid.2013.03.013
Author information
Authors and Affiliations
Contributions
Nan Peng collected the data, analyzed the data, and drafted the original manuscript. Lizhen Fu and Qi Lu conceived the study idea and critically reviewed the manuscript. Xiaohua Liang helped in study conception and data analysis and critically reviewed the data. All authors take full responsibility for the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Review Board, Children’s Hospital of Chongqing Medical University. Standards of STROBE initiative were followed by our study.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peng, N., Fu, L., Liang, X. et al. Risk factors of brain abscess in neonatal meningitis: a propensity score–matched study. Eur J Pediatr 182, 2215–2223 (2023). https://doi.org/10.1007/s00431-023-04860-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04860-1