Abstract
Arterial hypertension during childhood or adolescence is rising, and smoking during pregnancy may constitute a modifiable risk factor. This study aims to evaluate the effect of maternal smoking during pregnancy on diastolic (DBP) and systolic blood pressure (SBP) in childhood and adolescence. A bibliographic search was conducted in PubMed, Embase, and CENTRAL databases in March 2022. Meta-analysis was performed with the difference in mean-adjusted SBP/DBP of children and adolescents aged 3–17 years, according to maternal smoking/non-smoking in pregnancy. A random effects model was applied; a leave-one-out analysis and meta-analysis by subgroups were performed. A modified Newcastle–Ottawa scale was used to assess the quality of the studies. Evidence levels were rated using the GRADE system. Fifteen studies were included in the meta-analysis; all of them evaluated the mean-adjusted SBP difference in children or adolescents (N = 73,448), and 6 also that of DBP (N = 31,459). Results showed that maternal smoking during pregnancy significantly increased SBP (β = 0.31 mmHg 95% CI 0.14–0.49). A greater increase in mean-adjusted SBP was observed in those studies that completed the recruitment before 1990, were conducted in non-European countries, used standard mercury or manual sphygmomanometry, adjusted for birth weight, and were in the lowest quality subgroup. No significant association was found for DBP. The GRADE level of evidence was low for SBP and very low for DBP.
Conclusion: Smoking in pregnancy might increase SBP in childhood and adolescence. Due to the low level of evidence, solid inferences cannot be drawn about the clinical relevance of these findings.
What is Known: • AHT is the leading cause of premature death among adults worldwide. • Deleterious effects derived from SHS exposure on children's health have been documented since early 1970. To date, there are contradictory results about the effects of prenatal SHS exposure on children’s BP. | |
What is New: • Smoking in pregnancy may increase SBP during childhood and adolescence. • Maternal smoking during pregnancy could have greater influence on their offspring's SBP than on DBP. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High blood pressure (BP) or arterial hypertension (AHT) in children, defined as systolic blood pressure (SBP) or diastolic blood pressure (DBP) equal to or higher than the 95th percentile, by sex, age, and height, up to age 16, or ≥ 130/85 mmHg for age 16 or older [1], is an increasingly frequent condition during childhood or adolescence [2]. It often tends to be asymptomatic, and is underdiagnosed by health professionals [3, 4]. The global prevalence of AHT in the general pediatric population (children aged 6 to 19 years) is estimated at around 4.0%, with 3.0% for systolic hypertension and 1.9% for diastolic hypertension [2]. Even so, the US National Health and Nutrition Examination Survey shows that 13.3% of American children have high BP [5].
Like many chronic diseases, the etiology of AHT is complex and is thought to develop as a consequence of an interaction between genetic predisposition and the environment, mediated in part by epigenetic factors. It has been shown that tobacco use during pregnancy can cause changes in the placenta, generating fetal alterations which are associated with health problems, both pre- and postnatal [6]. Tobacco increases the risk of ectopic pregnancy, rupture of membranes, fetal mortality, intrauterine growth restriction, premature birth, low birth weight, and sudden infant death syndrome [7, 8]. Similarly, it can affect the growth of pulmonary parenchyma and airways, increasing the risk of asthma and respiratory infections, as well as giving rise to other cerebral and cardiovascular alterations [9, 10]. Globally, 1.7% of women are estimated to smoke during pregnancy; however, prevalence stands at 8.1% in the European region or at 5.9% in the Region of the Americas [11].
Since Barker published a study on the influence of adverse intrauterine conditions on postnatal development of cardiovascular diseases [12], a great deal of research has been done on how exposure to maternal smoking in the fetal period might affect the development of AHT during childhood, taking into account the atherogenic effect of this teratogen [13]. AHT is the leading cause of premature death among adults worldwide [14], and current physiopathologic and epidemiologic evidence suggests that childhood AHT increases the risk of essential AHT, as well as cardiovascular events later in life [15].
The precise role played by smoking during pregnancy in development of AHT in childhood and adolescence has not yet been established, and controversy remains with mixed findings from studies [16, 17]. Two previous reviews with meta-analysis were identified, but most of the studies included were cross-sectional, and the cohort studies included had a short follow-up time [16, 18]. Furthermore, one of the reviews drew no distinction between maternal smoking during pregnancy and children’s exposure to environmental tobacco smoke (ETS) [16].
The aim of this study was to analyze current evidence by conducting a systematic review with meta-analysis of prospective cohort studies and to evaluate the association between maternal smoking in pregnancy and their offspring’s DBP and/or SBP during childhood or adolescence.
Material and methods
We carried out a systematic review with meta-analysis, following the standard PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines [19]. The systematic review protocol was registered in the PROSPERO database and updated in December 2022 (registration no. CRD42021247824). During the review process, we identified the need to modify the eligibility criteria relating to study design and participants’ target age range to improve the quality of the evidence. This justifies the updating of the initial protocol recorded in PROSPERO. Reassuringly, following the guidelines of the Cochrane Handbook, sensitivity analyses were further performed to identify if these particular decisions influenced our findings.
Search strategy
In March 2022, we conducted a bibliographic search of the MEDLINE (PubMed), EMBASE, and CENTRAL databases, applying a pre-designed search strategy (Supplementary Table 1) drawn up by 3 expert reviewers in the matter. The search terms included both MeSH and free terms: “tobacco smoke pollution,” “smoking,” “tobacco smoking,” “cigarette smoking,” “pregnancy,” “hypertension,” “blood pressure,” “passive smoking,” “secondhand smoke,” “environmental tobacco smoke,” “smok*,” “maternal smoking,” “paternal smoking,” “arterial pressure,” “hypertension,” “systolic pressure,” “diastolic pressure,” and “mean blood pressure.” A manual review of the bibliographic references from included studies was performed to ensure the inclusion of all possible studies. No restrictions were applied in terms of country, study period, study design, or language.
Eligibility criteria
The review covered studies that evaluated the association between maternal smoking in pregnancy and the BP of their offspring aged 3 through 17 years. We included all studies published in peer-reviewed journals that met the following PECOS question: “Among children or adolescents, what is the effect of maternal smoking during pregnancy on their mean-adjusted DBP and/or SBP, compared to those whose mothers did not smoke?”. The PECOS framework focuses on population, exposure, comparator, outcome and study design: Population: Pregnant mothers and their offspring aged 3 through 17 years; exposure: Tobacco use during pregnancy; comparator: Non-tobacco use during pregnancy; outcome: Difference in children’s or adolescents’ mean-adjusted DBP and/or SBP (in mmHg); Study design: Prospective cohort studies that provided the necessary data to calculate mean-adjusted differences and their 95% confidence intervals (95% CIs).
The studies with the following characteristics were excluded: studies that did not provide sufficient data to calculate mean-adjusted BP differences and their 95% CIs; studies including women who consumed exclusively e-cigarettes or other tobacco products; studies that reported combined results (women’s use of other tobacco products in addition to cigarettes); studies that evaluated exposure to ETS during pregnancy, not exclusively due to maternal smoking; studies that estimated mean DBP and/or SBP without adjustment for possible covariates; studies that included population under 3 years old or over 17 years old; studies that included exclusively female or male population since we intended to examine maternal smoking effects jointly in both sexes; and studies that included smoking children and/or adolescents. Furthermore, we excluded studies published in a language other than Spanish, English, or Portuguese, and communications to congresses, letters to the editor, opinion articles, narrative reviews, case–control studies, cross-sectional studies, case series, simulation studies, and studies which had been withdrawn. Although cross-sectional studies were identified, they were not included in the main meta-analysis to avoid misleading results.
Selection of papers and extraction of data
After eliminating duplicated papers, 3 researchers screened the titles and abstract of all the papers yielded by the search. Each researcher evaluated eligibility separately on the basis of the title and abstract. In the case of papers considered potentially relevant, the full text was read to ensure that they fulfilled the inclusion/exclusion criteria. Differences of opinion about the inclusion or exclusion of any given paper were settled by consensus of the 3 reviewers. Where different papers based on the same study were identified, we included those that had the largest sample size and with the most up-to-date data.
Where the outcome variable was adjusted for different confounding variables, we selected the model with the best fit. In the case of studies that exclusively provided mean-adjusted DBP and/or SBP of children and/or adolescents according to maternal smoking, we used the EPIDAT program to calculate the coefficient of the difference between means along with the 95% CI.
To extract the relevant information from each paper, a data extraction sheet was designed in Microsoft Excel. The data were manually extracted by 2 of the authors, and both sets of extractions were then reviewed by a third. Differences of opinion were discussed and settled by consensus. From each paper, data were extracted on [1] study design; [2] author and year of publication of the study; [3] period of recruitment of pregnant women; [4] country of study; [5] data source; [6] age of children in whom BP was evaluated; [7] sample size; [8] definition of maternal tobacco use in pregnancy; [9] number of BP measures; [10] BP measurement method, i.e., oscillometry or digital sphygmomanometry and standard mercury or manual sphygmomanometry; [11] difference in mean-adjusted SBP/DBP (in mmHg) according to maternal smoking in pregnancy, along with the 95% CI; and [12] adjustment for confounding variables.
Assessment of quality and level of evidence
The AMSTAR 2 tool was used to score the systematic review [20]. The quality of the studies included was evaluated using an adaptation of the Newcastle–Ottawa scale [21]. Two researchers screened each study separately by reference to the representativeness of the sample, sample size, ascertainment of the exposure to maternal smoking, number of BP measurements obtained, adjustment for covariates, and statistical test. Supplementary Table 2 shows detailed information on the criteria and the number of points assigned to the studies according to each item. Studies were scored from 0 to 10 by each researcher, with the final score being reached by agreement. In the event of any difference of opinion, a third researcher was consulted. Studies that obtained a score of < 5 points were rated as poor quality, those with a score of 5–6 points as moderate quality, and those with a score of ≥ 7 points as high quality. While no studies were excluded on the basis of the evaluation of risk of bias, a sensitivity analysis was nonetheless performed with the higher quality studies.
Evidence levels were rated using the GRADE (Grading of Recommendations, Assessment, Development and Evaluation) system. The GRADE system allows for classification of evidence into four grades of evidence (high quality, moderate, low, and very low) attending to the risk of bias, inconsistency, uncertainty, inaccuracy, publication bias, and other considerations [22].
Data analysis
To perform the meta-analysis, we calculated the difference in mean-adjusted SBP/DBP of children or adolescents, according to whether their mothers had or had not been smokers during pregnancy. A random effects model was applied, and differentiated analyses were performed for DBP and/or SBP, using the study’s covariate-adjusted results.
Inter-study heterogeneity was evaluated using the p-value of the Cochrane Q test and the I2 statistic. A p-value < 0.1 indicates the presence of heterogeneity, with such heterogeneity being considered substantial if I2 > 50% [23,24,25]. Presence of publication bias was analyzed using a funnel plot, Egger’s regression test for funnel plot asymmetry, and Begg’s test [26, 27]. In cases where the p-value is < 0.1, risk of publication bias was deemed to exist.
We performed both a leave-one-out analysis to ascertain the influence of each of the studies, sensitivity analysis including cross-sectional studies and one prospective cohort study with 18-year-old males, and the following meta-analyses by subgroups: (1) study quality (low vs. medium/high); (2) studies that adjusted for children’s birth weight (yes vs. no); (3) recruitment period (1958–1989; 1990–2000; 2001–2007); (4) continent (European or non-European); (5) BP measurement method (digital sphygmomanometry or oscillometry vs. standard mercury or manual sphygmomanometry); and (6) age group (3–6.5 years vs. 7–15 years). All analyses were performed using the STATA statistical analysis software program v17.
Results
Search results
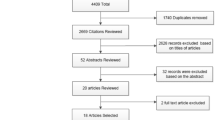
The search yielded a total of 12,035 papers; 21 studies fulfilled the inclusion criteria and 15 were included in the meta-analysis (Fig. 1). Supplementary Table 3 shows the characteristics of those potentially relevant studies excluded from the systematic review after reading the full text (n = 34), including cross-sectional studies [28,29,30,31] and a prospective cohort study with 18-year-old males [32].
Characteristics of the studies included
All of the 15 studies included in the meta-analysis evaluated the difference in the mean-adjusted SBP of children and/or adolescents, aged 3 to 15 years, according to maternal use/non-use of tobacco (N = 73,448), and 6 also evaluated the difference in the mean-adjusted DBP (N = 31,459) (Table 1).
Most studies recruited pregnant women before or during the 1990s (n = 12), were conducted in non-European continental areas (n = 12), and used oscillometry to measure BP (n = 12). With the exception of one study, all of them obtained at least 2 BP readings. Six studies were excluded from the meta-analysis because they did not adjust BP for covariates, and because the data came from the same study (Generation R) as another paper with a larger sample size (Table 1).
Maternal smoking during pregnancy was measured using self-reported questionnaires. One study evaluated use with determination of cotinine in maternal serum during pregnancy and in cord blood (Table 1).
Adjustment variables, related both to the mother, offspring, father/partner, and BP measurement, differed among the studies, yet most adjusted for sex, age, height, weight, and socioeconomic status and/or educational level (Table 2).
Regarding the sources of funding for the 15 studies included in the meta-analysis, most study authors indicated that studies received funding (n = 13), particularly, from universities, Medical Research Council and National Institutes of Health; of note, the authors from one study did not disclose information on financial support [33].
Study quality
The systematic review was rated as high quality using the AMSTAR 2 tool, considering that it provides an accurate and comprehensive summary of the results of available studies addressing the question of interest.
In terms of the quality scores, 5 studies were rated as being high quality, 5 as moderate, and 5 as low quality when using a modified Newcastle–Ottawa scale (Supplementary Table 4). Most of the studies displayed classification bias.
Results of the meta-analysis
Maternal smoking in pregnancy significantly increased SBP during childhood or adolescence (β = 0.31 mmHg; 95% CI: 0.14–0.49) (Fig. 2). The Cochrane Q test indicated that there might be inter-study heterogeneity (p-value < 0.1) but that such heterogeneity was not substantial (I2 = 0.00%). The leave-one-out analysis showed that none of the studies significantly modified the results (Supplementary Fig. 1). The funnel plot (Supplementary Fig. 2) and Egger’s test suggested that there might be publication bias (p-value < 0.1). No significant associations were found for DBP (β = −0.16 mmHg; 95% CI: −0.75–0.43) and inter-study heterogeneity was high (I2 = 73.10% and p-value of the Q test < 0.1) (Fig. 3). None of the studies contributed substantially to reducing this heterogeneity (Supplementary Fig. 3). Supplementary Fig. 4 shows the funnel plot.
Findings from the meta-analysis including cross-sectional studies show similar results and great heterogeneity for both SBP and DBP (β = 0.37 mmHg; 95% CI: 0.03–0.70 [I2: 79.33%] and β = −0.13 mmHg; 95% CI: −0.62–0.35 [I2: 59.76%], respectively] (Supplementary Figs. 5 and 6). Inter-study heterogeneity disappeared in the sensitivity analyses restricting to prospective cohort studies measuring SBP (Fig. 2). After including the prospective cohort study with 18-year-old males in the meta-analysis, similar results were found for both SBP and DBP (β = 0.26 mmHg; 95% CI: 0.13–0.38 [I2: 0.00%] and β = −0.04 mmHg; 95% CI: −0.54–0.47 [I2: 82.77%], respectively) (Supplementary Figs. 7 and 8).
Regarding the meta-analyses conducted by subgroups, a greater increase in mean-adjusted SBP was observed in the subgroup of studies that completed the recruitment before 1990, were conducted in non-European continental areas, used standard mercury or manual sphygmomanometry, adjusted for birth weight, and were in the lowest quality subgroup. However, inter-study heterogeneity was substantial for some subgroups (Table 3). Subgroup analyses were not deemed for studies measuring DBP due to the small number (n = 6) and marked inter-study heterogeneity.
The GRADE level of evidence was low for SBP and very low for DBP (Supplementary Table 5).
Discussion
These results show that smoking in pregnancy increases children’s and adolescent’s SBP, though the difference in adjusted-means is small (< 1 mmHg). With respect to DBP, no effect is in evidence, though the studies are very heterogeneous. Part of this heterogeneity could be due to some factors, including different adjustments for covariates and classification of maternal smoking, participants’ characteristics, or BP measurement method.
Importantly, the fact that maternal smoking during pregnancy was associated with SBP but not DBP could be due to effects on the arterial stiffness or pulse pressure, which mainly influences SBP, rather than effects on peripheral vascular resistance, which predominantly affects DBP [34]. Fetal growth retardation and arterial resistance adaptations resulting from exposure to maternal smoking could lead to altered elastin synthesis, which becomes more pronounced with age; gradual loss of elastin and replacement by collagen may result in reduced distensibility of the aorta and large arteries, leading to higher SBP [35].
The estimates are consistent with those of a previous one conducted in 2008 [17], which observed a higher increase in BP; however, it drew no distinction between SBP and DBP (0.62 mmHg 95% CI: 0.19–1.05) [17]. The results also coincide with those of another meta-analysis [16], which observed that passive exposure to tobacco (parental smoking or exposure to ETS from other smokers) significantly increased SBP (β = 0.26 mmHg 95% CI 0.12–0.39) but not DBP (β = 0.07 mmHg 95% CI −0.15–0.29). As with our analysis, the number of studies which evaluated DBP was limited to evaluate the possible causes of heterogeneity.
With the sole exception of one study [36], maternal smoking was measured with self-report, and most studies defined maternal smoking as “use during pregnancy: yes/no.” This definition is too broad and does not allow us to know the daily amount of tobacco cigarettes, the intensity, or the specific consumption according to the week of gestation. Although self-reported questionnaires have been widely used to evaluate prenatal exposure to ETS, and their validity is rated as high by some researchers [37], they could underestimate the prevalence of children’s exposure, due to pregnant women’s reticence to reveal their smoking status, social-desirability, or memory bias [38,39,40]. In this respect, whenever feasible, prenatal exposure should be measured with maternal biomarkers such as cotinine to provide a more accurate estimate.
Prior investigators found a dose-dependent association between maternal smoking during pregnancy and children’s or adolescents’ BP [16, 41]. Unfortunately, this could not be tested in this meta-analysis since just 2 studies recorded the daily cigarette consumption [33, 42].
Increased SBP was greater in the group of children and adolescents exposed to maternal tobacco smoke who participated in studies whose recruitment was conducted during 1959–1985 [33, 36, 42,43,44,45], compared to those with recruitment after 1985, and in that from non-European studies [36, 43,44,45,46,47,48], compared to European. These findings could be due to greater cigarette consumption by smoking mothers during pregnancy, as a consequence of lower awareness and social concern about the harmful effects for the fetus [49,50,51,52], worse diagnosis and treatment of gestational hypertension [35, 53], or lower prevalence and/or shorter duration of maternal breastfeeding [44, 54]. Alternatively, maternal socioeconomic status, parity and age at childbirth, and child’s BMI could also have influenced the results [28, 33, 41, 44, 54]; however, when examining the available data from the meta-analyzed studies, it was observed that the majority of the mothers were multiparous, were between 25 and 35 years old, and had average household income, and their children’s BMI ranged from 15 to 17 kg/m2.
The difference in mean-adjusted SBP was significant only in children and adolescents from studies in which BP was measured with standard mercury or manual sphygmomanometry [36, 42, 43, 45, 46]; however, it should be noted that these studies were mainly conducted before 1990 and in Non-European countries. Previous studies displayed discrepancies in terms of overestimation or underestimation of SBP according to the measurement method (oscillometry vs. standard mercury or manual sphygmomanometry) [55,56,57]. Accuracy of children’s BP reading could be influenced by the equipment (cuff size and calibration), subject (previous activity and activity during measurement, age, and height), setting and time of day of BP reading, and measurement technique (device, staff training, and experience) [3, 58].
We noted that the information provided in the studies included in the meta-analysis regarding staff training, cuff size, extremity used for the measurement, patient position, and environmental factors varied from one study to another. Of note, some studies did not follow a standard procedure and did not comply with the most recommended practices [59]; thus, one paper indicated that the BP measurement was obtained with the child in the supine position rather than seated [41]; two studies stated that the BP measurement was performed on the left arm rather than the right arm [33, 60], and some papers did not specify whether they used the appropriate cuff size for the child [36, 60].
The heterogeneity among the study participants could also affect BP estimates. Children’s age differed by studies [34, 41, 42, 44,45,46,47, 60,61,62,63]. After conducting the subgroup analysis by age group, we observed a higher increase in SBP among those studies including older children; however, statistical significance was not reached. Interestingly, 3 of the meta-analyzed studies [43, 62, 64] measured BP during puberty and observed that the association between mothers’ smoking in pregnancy and BP of their offspring did not vary according to whether measurements were obtained before or during initiation of puberty.
Some of the meta-analyzed studies excluded twins, children with congenital heart disease or kidney abnormalities, premature births, and newborns with low or high birth weight for gestational age, which could have underestimated the total effect of tobacco smoke exposure on child’s BP [33, 34, 36, 43, 57, 63]. The unique study that included exclusively premature children and children with low birth weight [45] reported no statistically significant increase in mean-adjusted SBP of children exposed to maternal tobacco smoke, compared to those unexposed. In the subgroup analysis, the difference in mean-adjusted SBP was greater in the group of studies that adjusted for birth weight with respect to those that did not. A previous study concluded that the direct effect of birth weight on children’s and adolescents’ BP could be overestimated, when taking into account the indirect effect of this variable on children’s height and BMI; in this case, all the studies which adjusted for birth weight, with the exception of 3 [34, 42, 44], also did so for children or adolescents’ height and BMI. Specifically, 8 studies adjusted BP for child’s height [41, 43,44,45,46,47, 62], and all but 5 studies [36, 41, 45, 48, 63], for child’s weight or BMI.
This meta-analysis has a series of strengths. First, we evaluated the differences in mean-adjusted BP (in mmHg) and not the probability of suffering from AHT, thereby reducing the risk of incorrect classification, in view of the different criteria for defining AHT in children and adolescents [3, 60]. Second, our inclusion criteria were strict and we focused on cohort studies with longitudinal measures of BP. Third, our results make it possible to examine the difference in SBP and DBP across almost 5 decades, considering adjustment for different covariates, for a total of 73,448 children and adolescents whose mothers smoked during pregnancy.
However, the overall quality of evidence was judged to be low for SBP and very low for DBP. The certainty in the evidence was downgraded due to the high risk of bias in the individual studies included for both outcomes. Several studies displayed bias related to the design and analysis such as selection, sample size, classification of prenatal exposure to maternal smoking, and confounding. Confounding bias was the most widely observed limitation in low- and moderate-quality studies due to failure to adjust for important variables which could have confounded the association, or due to adjustment for potential causal intermediates which could result in an underestimation of the total effect of maternal smoking during pregnancy on child’s BP, such as birth weight or gestational age. For example, we are aware that increase in child’s SBP could be influenced by current ETS exposure as some mothers could continue smoking but just one of the studies included in the meta-analysis adjusted BP for this covariate. Reassuringly, although no studies were excluded on the basis of the evaluation of risk of bias, a sensitivity analysis was performed considering the quality rating assigned to the individual studies according to the adapted Newcastle–Ottawa scale, and higher increase was observed in the subgroup of studies rated as being low quality but increase was just statistically significant for those moderate-high quality studies. We did not include gray literature, and therefore, this could have contributed to the risk of publication bias observed in the funnel plots, for both SBP and DBP.
With regard to DBP, certainty was further rated down for inconsistency and imprecision due to the large unexplained heterogeneity of results, and the wide variance in point estimates and CIs of included studies. While random effects model was applied and meta-analysis by subgroups was conducted for those studies measuring SBP, subgroup analysis could not be performed for DBP due to the small number of studies and their marked heterogeneity, but it should be borne in mind that AHT in children is mainly due to elevated SBP [41].
We are reasonably confident in not having missed any relevant studies, since we complemented the search with a manual review of the references of included studies. To the best of our knowledge, just two studies were excluded due to language (studies were written in Russian and Japanese) [65, 66]. Of note, papers assessing the effects of postnatal exposure on children’s or adolescents’ BP were not included due to the fact that they were all cross-sectional in nature [67,68,69,70,71,72].
Conclusions
This study supports the hypothesis that maternal smoking in pregnancy could increase SBP of offspring during childhood and adolescence. Due to the low level of evidence, solid inferences cannot be drawn about the clinical relevance of these findings. Future cohorts should examine the effect of maternal smoking or ETS exposure on child’s SBP and DBP, after adjusting for different covariates.
Availability of data and materials
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- AHT:
-
Arterial hypertension
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CIs:
-
Confidence intervals
- DBP:
-
Diastolic blood pressure
- ETS:
-
Environmental tobacco smoke
- GRADE:
-
Grading of recommendations, assessment, development, and evaluation
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analysis
- SBP:
-
Systolic blood pressure
References
de Simone G, Mancusi C, Hanssen H, Genovesi S, Lurbe E, Parati G et al (2022) Hypertension in children and adolescents. Eur Heart J 43(35):3290–3301. https://doi.org/10.1093/eurheartj/ehac328. (PubMed PMID: 35896123)
Song P, Zhang Y, Yu J, Zha M, Zhu Y, Rahimi K et al (2019) Global prevalence of hypertension in children: a systematic review and meta-analysis. JAMA Pediatr 173(12):1154–1163. https://doi.org/10.1001/jamapediatrics.2019.3310. (PubMed PMID: 31589252; PubMed Central PMCID: PMC 6784751)
Hansen ML, Gunn PW, Kaelber DC (2007) Underdiagnosis of hypertension in children and adolescents. JAMA 298(8):874–879. https://doi.org/10.1001/jama.298.8.874. (PubMed PMID: 17712071)
Sorof J, Daniels S (2002) Obesity hypertension in children: a problem of epidemic proportions. Hypertension 40(4):441–447. https://doi.org/10.1161/01.hyp.0000032940.33466.12. (PubMed PMID: 12364344)
Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW et al (2021) Heart Disease and Stroke Statistics-2021 update: a report from the American Heart Association. Circulation. 143(8):e254-e743. Epub 20210127. https://doi.org/10.1161/cir.0000000000000950. (PubMed PMID: 33501848)
Asmussen I (1979) Fetal cardiovascular system as influenced by maternal smoking. Clin Cardiol 2(4):246–256. https://doi.org/10.1002/clc.4960020403. (PubMed PMID: 262573)
Pineles BL, Park E, Samet JM (2014) Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol 179(7):807–23. Epub 20140210. https://doi.org/10.1093/aje/kwt334. (PubMed PMID: 24518810; PubMed Central PMCID: PMC3969532)
Avşar TS, McLeod H, Jackson L (2021) Health outcomes of smoking during pregnancy and the postpartum period: an umbrella review. BMC Pregnancy Childbirth 21(1):254. Epub 20210326. doi: https://doi.org/10.1186/s12884-021-03729-1. (PubMed PMID: 33771100; PubMed Central PMCID: PMC7995767)
Office on Smoking and H. Publications and reports of the surgeon general (2006) The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US)
Raghuveer G, White DA, Hayman LL, Woo JG, Villafane J, Celermajer D et al (2016) Cardiovascular consequences of childhood secondhand tobacco smoke exposure: prevailing evidence, burden, and racial and socioeconomic disparities: a scientific statement from the American Heart Association. Circulation 134(16):e336-e59. Epub 2016/10/19. https://doi.org/10.1161/cir.0000000000000443. (PubMed PMID: 27619923; PubMed Central PMCID: PMC5207215)
Lange S, Probst C, Rehm J, Popova S (2018) National, regional, and global prevalence of smoking during pregnancy in the general population: a systematic review and meta-analysis. Lancet Glob Health 6(7):e769-e76. Epub 20180531. https://doi.org/10.1016/s2214-109x(18)30223-7. (PubMed PMID: 29859815)
Wilson J (1999) The Barker hypothesis. An analysis. Aust N Z J Obstet Gynaecol 39(1):1–7. https://doi.org/10.1111/j.1479-828x.1999.tb03432.x. (PubMed PMID: 10099738)
Matturri L, Lavezzi AM, Ottaviani G, Rossi L (2003) Intimal preatherosclerotic thickening of the coronary arteries in human fetuses of smoker mothers. J Thromb Haemost 1(10):2234–2238. https://doi.org/10.1046/j.1538-7836.2003.00409.x. (PubMed PMID: 14521609)
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL et al (2003) The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. Jama 289(19):2560–72. Epub 20030514. https://doi.org/10.1001/jama.289.19.2560. (PubMed PMID: 12748199)
Osmond C, Barker DJ (2000) Fetal, infant, and childhood growth are predictors of coronary heart disease, diabetes, and hypertension in adult men and women. Environ Health Perspect 108 Suppl 3(Suppl 3):545–53. https://doi.org/10.1289/ehp.00108s3545. (PubMed PMID: 10852853; PubMed Central PMCID: PMC1637808)
Aryanpur M, Yousefifard M, Oraii A, Heydari G, Kazempour-Dizaji M, Sharifi H et al (2019) Effect of passive exposure to cigarette smoke on blood pressure in children and adolescents: a meta-analysis of epidemiologic studies. BMC Pediatr 19(1):161. Epub 20190521. https://doi.org/10.1186/s12887-019-1506-7. (PubMed PMID: 31113399; PubMed Central PMCID: PMC6528314)
Brion MJ, Leary SD, Lawlor DA, Smith GD, Ness AR (2008) Modifiable maternal exposures and offspring blood pressure: a review of epidemiological studies of maternal age, diet, and smoking. Pediatr Res 63(6):593–598. https://doi.org/10.1203/PDR.0b013e31816fdbd3. (PubMed PMID: 18317238)
Oken E, Levitan EB, Gillman MW (2008) Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. Int J Obes (Lond) 32(2):201–10. Epub 2008/02/19. doi: https://doi.org/10.1038/sj.ijo.0803760. (PubMed PMID: 18278059; PubMed Central PMCID: PMC2586944)
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev 10(1):89. Epub 20210329. https://doi.org/10.1186/s13643-021-01626-4. (PubMed PMID: 33781348; PubMed Central PMCID: PMC8008539)
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J et al (2017) AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj 358:j4008. Epub 20170921. https://doi.org/10.1136/bmj.j4008. PubMed PMID: 28935701; PubMed Central PMCID: PMC5833365
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–5. Epub 20100722. https://doi.org/10.1007/s10654-010-9491-z. (PubMed PMID: 20652370)
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64(4):383–94. Epub 20101231. https://doi.org/10.1016/j.jclinepi.2010.04.026. (PubMed PMID: 21195583)
Bowden J, Tierney JF, Copas AJ, Burdett S (2011) Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol 11:41. Epub 20110407. https://doi.org/10.1186/1471-2288-11-41. (PubMed PMID: 21473747; PubMed Central PMCID: PMC3102034)
Galbraith RF (1988) A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 7(8):889–894. https://doi.org/10.1002/sim.4780070807. (PubMed PMID: 3413368)
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557. (PubMed PMID: 12958120; PubMed Central PMCID: PMC 192859)
Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds.) (2021) Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane. Available from: www.training.cochrane.org/handbook
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629. (PubMed PMID: 9310563; PubMed Central PMCID:PMC 2127453)
Whincup PH, Cook DG, Papacosta O (1992) Do maternal and intrauterine factors influence blood pressure in childhood? Arch Dis Child 67(12):1423–1429. https://doi.org/10.1136/adc.67.12.1423. (PubMed PMID: 1489219; PubMed Central PMCID:PMC 1793969)
Li L, Peters H, Gama A, Carvalhal MI, Nogueira HG, Rosado-Marques V et al (2016) Maternal smoking in pregnancy association with childhood adiposity and blood pressure. Pediatr Obes 11(3):202–9. Epub 20150714. https://doi.org/10.1111/ijpo.12046. (PubMed PMID: 26178147; PubMed Central PMCID: PMC4949567)
Zhang H, Yu L, Wang Q, Tao Y, Li J, Sun T et al (2020) In utero and postnatal exposure to environmental tobacco smoke, blood pressure, and hypertension in children: the Seven Northeastern Cities study. Int J Environ Health Res 30(6):618–29. Epub 20190529. https://doi.org/10.1080/09603123.2019.1612043. (PubMed PMID: 31140839)
Simonetti GD, Schwertz R, Klett M, Hoffmann GF, Schaefer F, Wühl E (2011) Determinants of blood pressure in preschool children: the role of parental smoking. Circulation 123(3):292–8. Epub 20110110. https://doi.org/10.1161/circulationaha.110.958769. (PubMed PMID: 21220729)
Högberg L, Cnattingius S, Lundholm C, D’Onofrio BM, Långström N, Iliadou AN (2012) Effects of maternal smoking during pregnancy on offspring blood pressure in late adolescence. J Hypertens 30(4):693–699. https://doi.org/10.1097/HJH.0b013e32835168f4. (PubMed PMID: 22388229; PubMed Central PMCID:PMC3664185)
Law CM, Barker DJ, Bull AR, Osmond C (1991) Maternal and fetal influences on blood pressure. Arch Dis Child 66(11):1291–1295. https://doi.org/10.1136/adc.66.11.1291. (PubMed PMID: 1755640; PubMed Central PMCID: PMC1793274)
Taal HR, de Jonge LL, van Osch-Gevers L, Steegers EA, Hofman A, Helbing WA et al (2013) Parental smoking during pregnancy and cardiovascular structures and function in childhood: the Generation R Study. Int J Epidemiol 42(5):1371–1380. https://doi.org/10.1093/ije/dyt178. (PubMed PMID: 24159077)
Geelhoed JJ, Fraser A, Tilling K, Benfield L, Davey Smith G, Sattar N et al (2010) Preeclampsia and gestational hypertension are associated with childhood blood pressure independently of family adiposity measures: the Avon Longitudinal Study of Parents and Children. Circulation 122(12):1192–9. Epub 20100907. https://doi.org/10.1161/circulationaha.110.936674. (PubMed PMID: 20823385; PubMed Central PMCID: PMC5321267)
Wen X, Triche EW, Hogan JW, Shenassa ED, Buka SL (2011) Prenatal factors for childhood blood pressure mediated by intrauterine and/or childhood growth? Pediatrics 127(3):e713–21. Epub 20110207. https://doi.org/10.1542/peds.2010-2000. (PubMed PMID: 21300676; PubMed Central PMCID: PMC3065147)
George L, Granath F, Johansson AL, Cnattingius S (2006) Self-reported nicotine exposure and plasma levels of cotinine in early and late pregnancy. Acta Obstet Gynecol Scand 85(11):1331–1337. https://doi.org/10.1080/00016340600935433. (PubMed PMID: 17091413)
Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, Koren G (2009) Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology. Ther Drug Monit 31(1):14–30. Epub 2009/01/07. https://doi.org/10.1097/FTD.0b013e3181957a3b. (PubMed PMID: 19125149; PubMed Central PMCID: PMC3644554)
Aurrekoetxea JJ, Murcia M, Rebagliato M, Guxens M, Fernández-Somoano A, López MJ et al (2016) Second-hand smoke exposure in 4-year-old children in Spain: sources, associated factors and urinary cotinine. Environ Res 145:116–25. Epub 20151206. https://doi.org/10.1016/j.envres.2015.11.028. (PubMed PMID: 26656512)
Mourino N, Pérez-Ríos M, Santiago-Pérez MI, Lanphear B, Yolton K, Braun JM (2021) Secondhand tobacco smoke exposure among children under 5 years old: questionnaires versus cotinine biomarkers: a cohort study. BMJ Open 11(6):e044829. Epub 20210628. https://doi.org/10.1136/bmjopen-2020-044829. (PubMed PMID: 34183339; PubMed Central PMCID: PMC8240561)
van den Berg G, van Eijsden M, Galindo-Garre F, Vrijkotte TG, Gemke RJ (2013) Explaining socioeconomic inequalities in childhood blood pressure and prehypertension: the ABCD study. Hypertension 61(1):35–41. Epub 20121105. https://doi.org/10.1161/hypertensionaha.111.00106. (PubMed PMID: 23129697)
Morley R, Leeson Payne C, Lister G, Lucas A (1995) Maternal smoking and blood pressure in 7.5 to 8 year old offspring. Arch Dis Child 72(2):120–4. https://doi.org/10.1136/adc.72.2.120. (PubMed PMID: 7702372; PubMed Central PMCID: PMC1511033)
Williams S, Poulton R (1999) Twins and maternal smoking: ordeals for the fetal origins hypothesis? A cohort study Bmj 318(7188):897–900. https://doi.org/10.1136/bmj.318.7188.897. (PubMed PMID: 10102850; PubMed Central PMCID: PMC27807)
Lawlor DA, Najman JM, Sterne J, Williams GM, Ebrahim S, Davey Smith G (2004) Associations of parental, birth, and early life characteristics with systolic blood pressure at 5 years of age: findings from the Mater-University study of pregnancy and its outcomes. Circulation 110(16):2417–23. Epub 20041011. https://doi.org/10.1161/01.cir.0000145165.80130.b5. (PubMed PMID: 15477400)
Belfort MB, Gillman MW, McCormick MC (2012) Prenatal and perinatal predictors of blood pressure at school age in former preterm, low birth weight infants. J Perinatol 32(4):265–9. Epub 20110707. https://doi.org/10.1038/jp.2011.88. (PubMed PMID: 21738122; PubMed Central PMCID: PMC4638382)
Bergel E, Haelterman E, Belizán J, Villar J, Carroli G (2000) Perinatal factors associated with blood pressure during childhood. Am J Epidemiol 151(6):594–601. https://doi.org/10.1093/oxfordjournals.aje.a010247. (PubMed PMID: 10733041)
Oken E, Huh SY, Taveras EM, Rich-Edwards JW, Gillman MW (2005) Associations of maternal prenatal smoking with child adiposity and blood pressure. Obes Res 13(11):2021–2028. https://doi.org/10.1038/oby.2005.248. (PubMed PMID: 16339135; PubMed Central PMCID:PMC1483219)
Ayer JG, Belousova E, Harmer JA, David C, Marks GB, Celermajer DS (2011) Maternal cigarette smoking is associated with reduced high-density lipoprotein cholesterol in healthy 8-year-old children. Eur Heart J 32(19):2446–53. Epub 20110621. https://doi.org/10.1093/eurheartj/ehr174. (PubMed PMID: 21693475)
Blake KV, Gurrin LC, Evans SF, Beilin LJ, Landau LI, Stanley FJ et al (2000) Maternal cigarette smoking during pregnancy, low birth weight and subsequent blood pressure in early childhood. Early Hum Dev 57(2):137–147. https://doi.org/10.1016/s0378-3782(99)00064-x. (PubMed PMID: 10735460)
Faber T, Kumar A, Mackenbach JP, Millett C, Basu S, Sheikh A et al (2017) Effect of tobacco control policies on perinatal and child health: a systematic review and meta-analysis. Lancet Public Health 2(9):e420-e37. Epub 20170905. https://doi.org/10.1016/s2468-2667(17)30144-5. (PubMed PMID: 28944313; PubMed Central PMCID: PMC5592249)
Kyrklund-Blomberg NB, Cnattingius S (1998) Preterm birth and maternal smoking: risks related to gestational age and onset of delivery. Am J Obstet Gynecol 179(4):1051–1055. https://doi.org/10.1016/s0002-9378(98)70214-5. (PubMed PMID: 9790397)
Doyle LW, Faber B, Callanan C, Morley R (2003) Blood pressure in late adolescence and very low birth weight. Pediatrics 111(2):252–257. https://doi.org/10.1542/peds.111.2.252. (PubMed PMID: 12563047)
Garovic VD, Dechend R, Easterling T, Karumanchi SA, McMurtry Baird S, Magee LA et al (2022) Hypertension in pregnancy: diagnosis, blood pressure goals, and pharmacotherapy: a scientific statement from the American Heart Association. Hypertension 79(2):e21-e41. Epub 20211215. https://doi.org/10.1161/hyp.0000000000000208. (PubMed PMID: 34905954)
Hardy ST, Sakhuja S, Jaeger BC, Urbina EM, Suglia SF, Feig DI et al (2021) Trends in blood pressure and hypertension among US children and adolescents, 1999–2018. JAMA Netw Open 4(4):e213917. Epub 20210401. https://doi.org/10.1001/jamanetworkopen.2021.3917. (PubMed PMID: 33792732; PubMed Central PMCID: PMC8017470)
Ni H, Wu C, Prineas R, Shea S, Liu K, Kronmal R et al (2006) Comparison of Dinamap PRO-100 and mercury sphygmomanometer blood pressure measurements in a population-based study. Am J Hypertens 19(4):353–360. https://doi.org/10.1016/j.amjhyper.2005.10.020. (PubMed PMID: 16580569)
Ostchega Y, Zhang G, Sorlie P, Hughes JP, Reed-Gillette DS, Nwankwo T et al (2012) Blood pressure randomized methodology study comparing automatic oscillometric and mercury sphygmomanometer devices: National Health and Nutrition Examination Survey, 2009–2010. Natl Health Stat Report 59:1–15 (PubMed PMID: 24984529)
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H et al (2019) Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med 16(2):e1002744. Epub 20190211. https://doi.org/10.1371/journal.pmed.1002744. (PubMed PMID: 30742624; PubMed Central PMCID: PMC6370184)
Gillman MW, Cook NR (1995) Blood pressure measurement in childhood epidemiological studies. Circulation 92(4):1049–1057. https://doi.org/10.1161/01.cir.92.4.1049. (PubMed PMID: 7641339)
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN et al (2005) Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 111(5):697–716. https://doi.org/10.1161/01.cir.0000154900.76284.f6. (PubMed PMID: 15699287)
Xie T, Falahi F, Schmidt-Ott T, Vrijkotte TGM, Corpeleijn E, Snieder H (2020) Early determinants of childhood blood pressure at the age of 6 years: the GECKO Drenthe and ABCD study birth cohorts. J Am Heart Assoc 9(22):e018089. Epub 20201110. https://doi.org/10.1161/jaha.120.018089. (PubMed PMID: 33167754; PubMed Central PMCID: PMC7763711)
Brion MJ, Leary SD, Smith GD, Ness AR (2007) Similar associations of parental prenatal smoking suggest child blood pressure is not influenced by intrauterine effects. Hypertension 49(6):1422–8. Epub 20070402. https://doi.org/10.1161/hypertensionaha.106.085316. (PubMed PMID: 17404184)
Leary SD, Brion MJ, Lawlor DA, Smith GD, Ness AR (2013) Lack of emergence of associations between selected maternal exposures and offspring blood pressure at age 15 years. J Epidemiol Community Health 67(4):320–6. Epub 20130115. https://doi.org/10.1136/jech-2012-201784. (PubMed PMID: 23322851)
Yang S, Decker A, Kramer MS (2013) Exposure to parental smoking and child growth and development: a cohort study. BMC Pediatr 13:104. Epub 20130710. doi: https://doi.org/10.1186/1471-2431-13-104. (PubMed PMID: 23842036; PubMed Central PMCID: PMC3717101)
Laura HC, Menezes AB, Noal RB, Hallal PC, Araújo CL (2010) Maternal anthropometric characteristics in pregnancy and blood pressure among adolescents: 1993 live birth cohort, Pelotas, southern Brazil. BMC Public Health 10:434. Epub 20100723. https://doi.org/10.1186/1471-2458-10-434. (PubMed PMID: 20653949; PubMed Central PMCID: PMC2918557)
Tubol IB, Zhukovskiĭ GS, Dorofeeva TG, Il’chenko IN, Perova NV (1989) Epidemiology of arteriosclerosis precursors in schoolchildren 10–13 years of age (data of a prospective study). Kardiologiia 29(3):86–88 (PubMed PMID: 2733346)
Takemura T (2015) Childhood hypertension. Nihon Rinsho 73(11):1893–1896 (PubMed PMID: 26619664)
Groner JA, Huang H, Joshi MS, Eastman N, Nicholson L, Bauer JA (2017) Secondhand smoke exposure and preclinical markers of cardiovascular risk in toddlers. J Pediatr 189:155–61. Epub 20170712. https://doi.org/10.1016/j.jpeds.2017.06.032. (PubMed PMID: 28711174; PubMed Central PMCID: PMC6446918)
Seyedzadeh A, Hashemi F, Soleimani A (2012) Relationship between blood pressure and passive smoking in elementary school children. Iran J Pediatr 22(3):351–6. (PubMed PMID: 23400119; PubMed Central PMCID: PMC3564091)
Crispim PA, Peixoto Mdo R, Jardim PC (2014) Risk factors associated with high blood pressure in two-to five-year-old children. Arq Bras Cardiol 102(1):39–46. Epub 20131122. https://doi.org/10.5935/abc.20130227. (PubMed PMID: 24263779; PubMed Central PMCID: PMC3987386)
Huntington-Moskos L, Turner-Henson A, Rice M (2014) Tobacco exposure, weight status, and elevated blood pressure in adolescents. J Community Health 39(4):653–659. https://doi.org/10.1007/s10900-014-9839-5. (PubMed PMID: 24519179)
Charakida M, Georgiopoulos G, Dangardt F, Chiesa ST, Hughes AD, Rapala A et al (2019) Early vascular damage from smoking and alcohol in teenage years: the ALSPAC study. Eur Heart J 40(4):345–353. https://doi.org/10.1093/eurheartj/ehy524. (PubMed PMID: 30169581; PubMed Central PMCID: PMC6340100)
Hamoen M, Welten M, Nieboer D, Bai G, Heymans MW, Twisk JWR et al (2020) Development of a prediction model to target screening for high blood pressure in children. Prev Med 132:105997. Epub 20200123. https://doi.org/10.1016/j.ypmed.2020.105997. (PubMed PMID: 31981642)
Rauschert S, Melton PE, Burdge G, Craig JM, Godfrey KM, Holbrook JD et al (2019) Maternal smoking during pregnancy induces persistent epigenetic changes into adolescence, independent of postnatal smoke exposure and is associated with cardiometabolic risk. Front Genet 10:770. Epub 20190905. https://doi.org/10.3389/fgene.2019.00770. (PubMed PMID: 31616461; PubMed Central PMCID: PMC6764289)
De Smidt JJA, Odendaal HJ, Nel DG, Nolan H, Du Plessis C, Brink LT et al (2021) The effects of in utero exposure to teratogens on organ size: a prospective paediatric study. J Dev Orig Health Dis 12(5):748–57. Epub 20201117. https://doi.org/10.1017/s2040174420001002. (PubMed PMID: 33198841; PubMed Central PMCID: PMC8536468)
Kok Grouleff M, Wielsøe M, Berthelsen D, Mulvad G, Isidor S, Long M et al (2021) Anthropometric measures and blood pressure of Greenlandic preschool children. Int J Circumpolar Health 80(1):1954382. https://doi.org/10.1080/22423982.2021.1954382. (PubMed PMID: 34291707; PubMed Central PMCID: PMC8300929)
Cajachagua-Torres KN, El Marroun H, Reiss IKM, Santos S, Jaddoe VWV (2022) Foetal tobacco and cannabis exposure, body fat and cardio-metabolic health in childhood. Pediatr Obes 17(3):e12863. Epub 20211021. https://doi.org/10.1111/ijpo.12863. (PubMed PMID: 34674394)
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. All phases of this study were supported by the Government Delegation for the National Plan on Drugs (Spain) grant 2021I009. The funder/sponsor did not participate in the work.
Author information
Authors and Affiliations
Contributions
Nerea Mourino was responsible for the conception and planning, analysis, interpretation, and drafting of the manuscript. Leonor Varela-Lema was also responsible for the conception and planning, analysis, interpretation, and drafting of the manuscript. Jasjit S Ahluwalia provided intellectual contributions, and reviewed and revised the successive versions of the manuscript. Julia Rey-Brandariz provided intellectual contributions, and reviewed and revised the manuscript. Cristina Candal-Pedreira provided intellectual contributions, and reviewed and revised the successive versions of the manuscript. Alberto Ruano-Ravina provided intellectual contributions, and reviewed and revised the successive versions of the manuscript. Andrea Vila-Farinas provided intellectual contributions, and reviewed and revised the successive versions of the manuscript. Andrés Torres provided intellectual contributions, and reviewed and revised the successive versions of the manuscript. Mónica Pérez-Ríos was also responsible for the conception and planning, analysis, interpretation, and drafting of the manuscript. All authors contributed to data analysis and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate.
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Gregorio Milani.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Impact
This study evaluated the effect of maternal tobacco use during pregnancy on diastolic and systolic blood pressure in childhood and adolescence. Smoking during pregnancy might increase SBP during childhood and adolescence. Due to the low level of evidence, solid inferences cannot be drawn about the clinical relevance of these findings.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mourino, N., Varela-Lema, L., Ahluwalia, J.S. et al. Maternal smoking in pregnancy and blood pressure during childhood and adolescence: a meta-analysis. Eur J Pediatr 182, 2119–2132 (2023). https://doi.org/10.1007/s00431-023-04836-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04836-1