Abstract
The purpose of this study is to synthesize evidence on risk factors associated with newborn 31-day unplanned hospital readmissions (UHRs). A systematic review was conducted searching CINAHL, EMBASE (Ovid), and MEDLINE from January 1st 2000 to 30th June 2021. Studies examining unplanned readmissions of newborns within 31 days of discharge following the initial hospitalization at the time of their birth were included. Characteristics of the included studies examined variables and statistically significant risk factors were extracted from the inclusion studies. Extracted risk factors could not be pooled statistically due to the heterogeneity of the included studies. Data were synthesized using content analysis and presented in narrative and tabular form. Twenty-eight studies met the eligibility criteria, and 17 significant risk factors were extracted from the included studies. The most frequently cited risk factors associated with newborn readmissions were gestational age, postnatal length of stay, neonatal comorbidity, and feeding methods. The most frequently cited maternal-related risk factors which contributed to newborn readmissions were parity, race/ethnicity, and complications in pregnancy and/or perinatal period.
Conclusion: This systematic review identified a complex and diverse range of risk factors associated with 31-day UHR in newborn. Six of the 17 extracted risk factors were consistently cited by studies. Four factors were maternal (primiparous, mother being Asian, vaginal delivery, maternal complications), and two factors were neonatal (male infant and neonatal comorbidities). Implementation of evidence-based clinical practice guidelines for inpatient care and individualized hospital-to-home transition plans, including transition checklists and discharge readiness assessments, are recommended to reduce newborn UHRs.
What is Known: • Attempts have been made to identify risk factors associated with newborn UHRs; however, the results are inconsistent. | |
What is New: • Six consistently cited risk factors related to newborn 31-day UHRs. Four maternal factors (primiparous, mother being Asian, vaginal delivery, maternal complications) and 2 neonatal factors (male infant and neonatal comorbidities). • The importance of discharge readiness assessment, including newborn clinical fitness for discharge and parental readiness for discharge. Future research is warranted to establish standardised maternal and newborn-related variables which healthcare providers can utilize to identify newborns at greater risk of UHRs and enable comparison of research findings. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Newborn unplanned hospital readmission (UHR) is defined as an unexpected hospital readmission within a specified time period following discharge from the initial hospitalization at the time of birth [1, 2]. Newborn UHRs are widely recognized as indicators of health service delivery quality and contribute to neonatal morbidity and increased healthcare cost [3,4,5]. Some unplanned hospital readmissions may present due to incomplete or inappropriate transitional care at the time of discharge [6]. Others are related to risk factors such as feeding issues or prolonged jaundice that may have been preventable with an individualized hospital-to-home transition plan and improved transitional care [7, 8].
Identifying risk factors associated with UHRs of the newborn can assist in reducing readmission rates through improvements in clinical practice, policy development, and the use of maternal-child healthcare services. While studies have examined causes associated with neonatal morbidity and mortality [9, 10], there is no published review of risk factors associated with UHRs for the newborn. This paper systematically reviewed current literature identifying risk factors associated with newborn 31-day UHRs. The objectives were to review the characteristics of included studies and synthesize the identified risk factors related to newborn UHRs.
Methods
The systematic review followed the 2009 PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) Statement [11].
Data sources and search strategy
An electronic database search was carried out using the CINAHL, EMBASE (Ovid), MEDLINE from 1st January 2000 to 30th June 2021 with key search terms (“Readmission” or rehospitali* or readmission* or readmit* or re-admission*) and (newborn* or new born* or newly born or baby* or babies or premature or prematurity or preterm or pre term or preemie* or premie* or low birth weight or low birthweight (LBW) or very low birthweight (VLBW) or extremely low birth weight (ELBW or infant* or infancy or neonat*) (A complete search strategy is provided in Appendix 1).
Four inclusion criteria for this review were (1) primary research studies, (2) UHRs assessment/measurements within 31 days, (3) study design stated clearly and reported statistical analysis procedure/s, and (4) published in peer-reviewed journals and the English language with full text available. Studies were excluded when mixed adverse outcomes, including complications and emergency department (ED) visits post-hospital discharge or readmission were measured more than once. Conference abstract-only references were also excluded.
Study selection
Two reviewers initially read all titles and abstracts independently to assess potential inclusion. Included full-text articles were then assessed against the inclusion criteria. Disagreements between the reviewers on potential articles for inclusion were resolved through discussion. Reference lists of all included articles were screened to identify additional articles.
Data extraction
Data extraction included study characteristics, examined variables, and statistically significant risk factors. Study characteristics included study setting, population, sample size, the timing of data collection, study design, data source, readmission rate, and statistical analysis test/s used to identify risk factors as per Table 1. All examined variables or confounding factors and statistically significant risk factors were extracted as per Table 2.
Quality assessment
The methodological quality of included studies was assessed independently by two reviewers using a standardised set of predefined criteria in six dimensions (Study participation, Study attrition, Prognostic factor measurement, Outcome measurement, Confounding measurement and account, and Analysis). The evaluation results of each item were rated as Yes/Partly/No/Unsure. The potential bias of each study was evaluated by overall risk “low” or “high” [12, 13].
Data synthesis
Pooling extracted risk factors is not possible due to the heterogeneity of included studies such as diagnosis, examined variables, or follow-up period to identify readmissions. Therefore, content analysis was used to synthesize the extracted risk factors, and the results are presented narratively [11]. Due to the complex and diverse nature of the population and risk factors associated with newborn 31-day UHRs, it was decided on the collation of all available evidence as it is not possible to proceed with meaningful sub-analysis given the limited amount of research evidence available in sub-groups. The overall aim of this review was the identification of commonly cited risk factors and to promote awareness for healthcare providers to be able to recognize newborns at greater risk for UHR.
Results
A total of 6783 records were initially identified, after removing 1771 duplicates, 5012 records remained and were screened through titles and abstracts. Of these, 4979 records were excluded due to irrelevance and 33 relevant references were considered eligible for potential inclusion. A further 4 were excluded as they were conference abstracts only. A total of 29 references were retrieved as full text. Three studies were further excluded for the following reasons: (1) Outcome measures included unplanned ED visits [14, 15] (n = 2); (2) readmissions were measured more than once [16] (n = 1). Two additional articles [17, 18] were identified during a hand search of the reference lists. As a result, 28 studies were included in the systematic review. Figure 1 illustrates the search result and selection process.
Study quality appraisal
Overall, the risk of potential bias for the 28 included studies was low against the six predefined dimensions of potential bias [12, 13]. Key characteristics of included populations were described clearly, samples were represented completely, all independent variables of the study population were measured appropriately, outcome variables of UHR were measured accurately, and statistical analysis tests were appropriate for the study design.
Characteristics of the included studies
Characteristics of the 28 included studies are summarized in Table 1. Eighteen studies were conducted in the United States of America (USA), three from Canada, two from the United Kingdom (UK), and one from Australia, France, India, Lebanon, and Taiwan. Length of time between discharge from initial admission at the time of birth to unplanned readmission varied from 7 to 31 days. Twenty included studies used 28-day or 30-day UHRs. Seven of the 28 studies examined a combination of data from an administrative database and medical records; 13 used medical records only, while the remaining seven used administrative databases.
Twenty-two included studies retrieved data from multiple sites, while 6 from a single center. Samples sizes varied from 58 to 4,667,827 and UHRs rates varied from 0.2 [19] to 39% [20]. The majority of included studies (n = 18) recorded the age of patients using gestational age (GA), while nine studies referred to the newborn without specific GA. The four main types of the population involved in the 28 included studies were health-term newborns (n = 2), all live newborns (n = 9), late-preterm newborns with various health condition focus (n = 5), and newborn with varieties of health issues (n = 12).
The time span for the retrieved data varied from 2 months [21] to 12 years [22]. In particular, six included studies accessed over 10 years of data. Two of the 28 included studies reported risk predictive models of performance. All five of the identified predictive models in the studies demonstrated sub-optimal performance (C-statistic of 0.62, 0.69, and 0.62, respectively) [23, 24].
Examined variables/confounding factors and significant risk factors
Variables or confounding factors differed across the 28 included studies. The number of examined variables for each study ranged from one [20, 22, 25, 26] to twenty-four [27]. Two studies [18, 22] reported inconclusive findings. Seventeen statistically significant risk factors related to newborn UHRs were extracted and grouped under either maternal or newborn-related factors in Table 2.
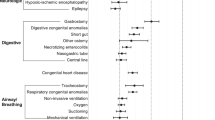
Maternal-related risk factors
Seventeen of the 28 included studies identified maternal variables contributing to 31-day newborn UHRs. The three most frequently cited risk factors were maternal parity, pre-existing or perinatal complications, and race/ethnicity. Nine studies [3, 7, 19, 23, 28, 30, 32, 38, 39] identified the primiparous mother as a significant risk factor for readmission for newborns with an odds ratio (OR) ranging from 1.1 to 5.5. Maternal race/ethnicity was cited in eight differing studies [7, 19, 28, 30, 32, 38,39,40]. Compared with other race/ethnicities, newborns of Asian mothers were more likely to be readmitted following the initial hospitalization at the time of birth (OR = 1.08 to 3.17).
Nine studies reported that mothers with pre-existing or perinatal complications increased the probability of newborn readmission following discharge [3, 7, 19, 21, 27, 30, 32, 35, 39]. The most common pre-existing maternal medical conditions and/or pregnancycomplications that resulted in newborn readmissions included gestational hypertension, gestational diabetes mellitus, placenta previa, placental abruption, and prolonged rupture of membranes. In two studies, newborns whose mothers experienced delivery complications were found to be at high risk of unplanned readmission [3, 30]. One study [27] identified maternal intrapartum chemoprophylaxis for group B streptococcus was associated with newborn readmission (OR = 2.55). Another study [21] cited newborns of mothers who self-rated poor health as more like to be readmitted (OR = 5.17).
In five studies, health care utilization and family resources, including uninsured health care status, unstable family income and inadequate support for the mother following the discharge, were identified as increasing the risk of newborn readmission [3, 21, 31, 39, 40]. Other studies differed, citing mothers who received comprehensive perinatal care as more likely to experience a UHR of their newborn [33, 39].
The geographic location of both the hospital where the birth occurred and the residential address of parents was cited as risk factors by five differing studies [17, 23, 36, 40, 41]. Higher readmission rates were noted for births in non-metropolitan hospitals [22, 36]. When newborns were discharged to residential addresses associated with lower newborn mortality rates, the risk of UHR was decreased by 10% (OR = 0.9) [41]. Two other studies found that health services with protocols requiring longer length of stay for newborns following their birth [17] or health services which provided limited use of intensive phototherapy for jaundice [32] experienced higher rates of readmissions (OR = 1.22–2.31).
The maternal age was cited as a risk factor by five studies [7, 23, 32, 38, 41]. One study [32] suggested that newborns of mothers younger than 20 years were more likely to be readmitted (OR = 1.2). In comparison, three studies [7, 38, 41] identified that newborns of mothers older than 30 or 35 years were at greater risk of readmission. One study [23] also reported increased readmission for healthy term infants with older mothers (OR = 1.02).
Newborn-related risk factors
Eleven significant risk factors pertaining to the newborns were extracted. The most frequently cited risk factors were gestation age, neonatal comorbidity, postnatal length of stay (LOS), and feeding methods.
Gestational age was the most frequently cited significant predictor of unplanned readmission for newborns with OR range from 1.18 to 9.43 [7, 17, 19, 23,24,25, 27, 30,31,32, 34,35,36,37,38, 42]. Generally, infants born before 37 gestational weeks were associated with an increased likelihood of readmission compared with those delivered at 39 to 40 weeks. Three studies specifically cited gestational age of 37 to 38 weeks as a risk factor for unplanned readmission as well [27, 30, 34].
Newborns who either had a medical condition at birth or developed medical conditions following their birth were associated with an increased risk of UHRs [2, 19, 20, 26,27,28, 30, 31, 33, 36, 40]. Medical conditions included jaundice, haemolysis, congenital abnormalities, complex/chronic conditions, sepsis, seizure, cardiac surgery, and myelomeningocele repair of newborns. Two studies cited infants who had a screening bilirubin test associated with jaundice during their hospitalization at the time of birth as significantly associated with increased risk of readmission with OR ranging from 6.66–8.76 [19, 33]. One study [27] indicated that jaundice assessed visually and documented on day two of life was a predictor of newborn readmission (OR = 2.45). Two studies [30, 31] involving newborns with neonatal abstinence syndrome (NAS), a postnatal drug withdrawal syndrome related to opioid exposure, found that newborns with NAS were more likely to be readmitted to the hospital compared to newborns without NAS (OR = 1.21–2.49).
Eleven included studies [2, 7, 22, 23, 30, 32,33,34,35, 38, 39] identified length of hospital stay (LOS) after birth as associated with increased risk of readmission; however, the results were inconsistent. Seven studies found shorter LOS (< 3 days) as associated with a higher risk of readmission for newborns delivered by vaginal or cesarean (OR = 1.2–13.8) [7, 30, 32, 35, 38, 39] or infants born late preterm and term (P < 0.05) [34].
Two studies [23, 33] reported that longer hospital LOS decreased the UHR rate for infants born by cesarean (OR = 0.40–0.78). Newborns who underwent cardiac surgery and stayed longer than 7 days in intensive care units were five times more likely to be readmitted [2]. One study [22], however, reported that longer LOS did not decrease 7-day readmission for late-preterm infants delivered vaginally.
Feeding methods and feeding problems were identified in nine studies [3, 17, 19, 27, 29, 32, 33, 35, 38]. Compared with bottle feeding, exclusive breastfeeding was found to contribute to an increased risk of newborn readmission in six cited studies [3, 29, 32, 33, 35, 38]. One study [19] also found newborns who experienced breastfeeding difficulties during birth hospitalization were more likely to be readmitted (OR = 1.85). One study [17] reported breastfeeding as associated with a lower rate of readmission for newborns (OR = 0.69). While one study [27] found newborns who were totally formula fed in the first 3 days of life were associated with decreased newborn readmission (OR = 0.996).
Gender was examined and reported consistently across seven differing studies. Compared to females, male newborns experienced a higher risk of unplanned readmission after birth [7, 23, 32, 36, 38,39,40].
Three studies [7, 32, 35] referred to newborns delivered as a vaginal or assisted vaginal birth (vacuum/forceps) as a higher risk of readmission compared to caesarean delivery. Two studies cited cesarean delivery mode as a protective factor against readmission [7, 27] (OR = 0.31–0.45).
The birth weight of newborns was also identified as a statistically significant factor in two studies. The measurement of birth weight, however, was inconsistent amongst the studies. One study [17] reported birth weight of less than 2500 g was associated with an increased risk of readmission among newborns (OR = 1.95), while another study [30] found newborns with birthweights in either the 10th or 90th percentile using national percentile ranges were more likely to be readmitted.
Two studies cited newborns’ weight at discharge as risk factors. One study [29] reported newborns with more than a 10% weight loss from birth at the time of discharge as at higher risk of readmission. This compared with one other study [33] which suggested that every 100 g of gained weight at discharge increased the risk of readmission for late-preterm newborns with hyperbilirubinemia.
Discussion
This systematic review synthesized risk factors associated with newborn 31-day unplanned hospital readmissions following discharge from the hospital where the birth occurred. Twenty-eight studies were reviewed, and 17 significant risk factors were extracted. These included six maternal and 11 newborn-related variables. Of the 17 predictors, six were consistently cited. Four factors were maternal (primiparous, mother being Asian, vaginal delivery, maternal complications), and two factors were neonatal (male infant and neonatal comorbidities). The remaining risk factors were inconsistent across the included studies.
Newborns of mothers under 20 or over the age of 35, especially primiparous, were at greater risk of unplanned hospital readmission. This is consistent with evidence on the adverse outcomes of pregnancies conceived at extreme maternal age [43]. Adverse outcomes included preterm births or perinatal deaths as well as pregnancy complications such as gestational diabetes and pregnancy-induced hypertension [44,45,46].
Newborns of Asian mothers were found in this review to have up to a 3 times greater likelihood than other ethnicities of being readmitted. It is noted that almost 90% of the included studies (n = 25) in this review were conducted in western developed countries such as the USA, Canada, UK, Australia, and France with extensive multicultural backgrounds. Mothers of Asian ethnicity experience language and cultural barriers during hospitalization impacting their health literacy and comprehension of discharge information on caring for newborns and themselves [47]. Additionally, where there is inadequate family support for migrants there is often limited uptake of community support services following hospital discharge [48, 49].
Our review also revealed that early-term or late preterm newborns (34 to 38 weeks GA), who are physiologically immature, were often treated the same as a full-term newborn and experienced higher readmission rates [18, 44]. There is a need to implement evidence-based practice guidelines and individualized transitional care plans that include newborn and parental assessment of discharge readiness to prevent UHR.
Readmission rates associated with the LOS for newborns after their birth were inconsistent and varied from 1.3 to 6.6 days across 92 countries [50]. Since the 1970s, there has been a trend toward shortening postnatal hospital stays for mother and newborn [51]. Some studies found reduced LOS and early newborn discharge did not increase the adverse outcomes and/or readmission rate [52,53,54]. In contrast, others reported shorter LOS associated with newborn mortality and neonatal UHR [51, 55]. The heterogeneity of the study population may explain the lack of consensus in the different studies, such as the newborn’s GA or birth weight, mode of delivery and parity, access to maternity care, availability of follow-up services, and/or parental knowledge and competence [56]. The inconsistent results highlight the importance of discharge readiness assessment, including newborn clinical fitness for discharge and parental readiness for discharge. Therefore, the timing of discharge should be decided in conjunction with the families.
This review found that vaginal or assisted vaginal deliveries significantly increased the risk of unplanned newborn readmissions compared with cesarean section. This is opposite to evidence promoting the advantages of vaginal delivery. Compared to newborns delivered by cesarean section, those delivered vaginally were found to have an increased probability of newborn hyperbilirubinemia and jaundice [57, 58], which resulted in an increased risk of newborn readmission. The indicators for either an elective or emergency cesarean procedure are to correct maternal or fetal existing medical conditions or distress. As a result, a higher level of care is required to be provided for both mothers postoperatively and newborns. This often leads to a longer stay in the hospital than mothers who have a vaginal delivery resulting in mothers having a greater length of time to recover and establish routines with their babies [59]. Newborns delivered by cesarean were strongly associated with reduced readmissions for jaundice [7, 32, 35]. More extended hospitalization following cesarean section than vaginal birth allowed mothers and newborns to establish breastfeeding [60], which was a protective factor reducing the risk of newborn UHRs. Newborns delivered by cesarean were also strongly associated with reduced readmissions for jaundice [7, 32, 35]. Additionally, vacuum-assisted deliveries were found to be associated with neonatal bruising and/or cephalohematoma, which increased the risk of newborn readmission [61].
Six included studies cited exclusive breastfeeding as a predictor of newborn readmission, which conflicts with the evidence citing the advantages of breastfeeding. Notably, most studies citing breastfeeding as a risk factor were related to newborn readmissions with jaundice [29, 32, 33, 38]. Mothers who wish to breastfeed their newborns exclusively might encounter many challenges resulting in newborns’ low oral intake and poor weight gain. Challenges include limited professional support, advice, and access to primary care services during the initial period following discharge [62]. Insufficient oral intake of newborns can cause severe hyperbilirubinemia, which also leads to UHRs [33, 63].
This systematic review has certain limitations. Firstly, only English language papers with full-text access were considered. The majority of the included studies were conducted in the North America, Europe, and Australia; therefore, generalization of this review’s results should be made with caution considering the characteristic of the healthcare settings. In addition, a meta-analysis was not performed to synthesize the extracted risk factors due to the heterogeneity in the 28 included studies. The studies’ heterogeneity included newborns’ characters, examined variables, time period associated with UHRs, and outcomes coherence. This systematic review did not restrict newborn’s gestational age and comorbidities, which might contribute to the large variation of UHR rate of 0.2% to 39%.
Conclusion
This systematic review confirms the diverse and complex nature of risk factors associated with newborn 31-day UHRs. Six consistently cited predictors include 4 maternal factors (primiparous, mother being Asian, vaginal delivery, maternal complications) and 2 neonatal factors (male infant and neonatal comorbidities). There is a need to promote healthcare providers’ awareness of risk factors then develop and implement comprehensive individualized hospital-to-home transition plans from the time of admission for the birth through to discharge home to reduce unplanned neonatal readmissions [64]. Transition checklists and discharge readiness assessments are recommended as strategies to reduce newborn UHRs as the quality of hospital-to-home transition of care is positively associated with the caregiver’s perception of readiness for discharge [65]. Transition assessment instruments include “Readiness for hospital discharge scale,” “Quality of discharge teaching scale,” and “Post-discharge coping difficulty scale” [66,67,68,69,70].
Applying identified predictive risk factors assists healthcare providers to recognize newborns at higher risk of readmission and implement preventative strategies, for example, individualized discharge planning [71]. Future research is warranted to establish standardized maternal and newborn-related variables for healthcare providers to identify newborns at higher risk of UHRs. The classification/grouping of newborn physiological conditions, such as GA, delivery mode, birth weight, and Apgar scores, should be clearly defined and standardized in future studies allowing comparisons across healthcare settings.
Availability of data and materials
Not applicable to a systematic review.
Change history
22 February 2023
Open Access funding information has been added in the Funding Note.
Abbreviations
- ELBW:
-
Extremely low birth weight
- GA:
-
Gestational age
- LBW:
-
Low birth weight or low birthweight
- LOS:
-
Length of stay
- NAS:
-
Neonatal abstinence syndrome
- OR:
-
Odds ratio
- UK:
-
United Kingdom
- UHR:
-
Unplanned hospital readmissions
- USA:
-
United States of America
- VLBW:
-
Very low birthweight
References
Edmonson MB, Stoddard JJ, Owens LM (1997) Hospital readmission with feeding-related problems after early postpartum discharge of normal newborns. JAMA 278(4):299–303
Mackie AS, Gauvreau K, Newburger JW et al (2004) Risk factors for readmission after neonatal cardiac surgery. Ann Thorac Surg 78:1972–1978. https://doi.org/10.1016/j.athoracsur.2004.05.047
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M et al (2006) Risk factors for neonatal morbidity and mortality among “healthy”, late preterm newborns. Semin Perinatol 30(2):54–60. https://doi.org/10.1053/j.semperi.2006.02.002
McLaurin KK, Hall CB, Jackson EA et al (2009) Persistence of morbidity and cost differences between late-preterm and term infants during the first year of life. Pediatrics 123(2):653–659. https://doi.org/10.1542/peds.2008-1439
Underwood MA, Danielsen B, Gilbert WM (2007) Cost, causes and rates of rehospitalization of preterm infants. J Perinatol 27(10):614–619. https://doi.org/10.1038/sj.jp.7211801
Goldfield NI, McCullough EC, Hughes JS et al (2008) Identifying potentially preventable readmissions. Health Care Financ Rev 30(1):75–91
Paul IM, Lehman EB, Hollenbeak CS et al (2006) Preventable newborn readmissions since passage of the Newborns’ and Mothers’ Health Protection Act. Pediatrics 118(6):2349–2358. https://doi.org/10.1542/peds.2006-2043
Kripalani S, Theobald CN, Anctil B et al (2014) Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med 65:471–485. https://doi.org/10.1146/annurev-med-022613-090415
Hamilton E, Dyachenko A, Ciampi A et al (2020) Estimating risk of severe neonatal morbidity in preterm births under 32 weeks of gestation. J Matern Fetal Neonatal Med 33(1):73–80. https://doi.org/10.1080/14767058.2018.1487395
Iriondo M, Thio M, Del Río R et al (2020) Prediction of mortality in very low birth weight neonates in Spain. PLoS ONE 15(7):e0235794. https://doi.org/10.1371/journal.pone.023579411
Moher D, Liberati A, Tetzlaff J et al (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Hayden J, Côté P, Bombardier CJ et al (2006) Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med 144(6):427–437. https://doi.org/10.7326/0003-4819-144-6-200603210-00010
Zhou H, Roberts PA, Dhaliwal SS et al (2019) Risk factors associated with paediatric unplanned hospital readmissions: a systematic review. BMJ Open 9(1):e020554. https://doi.org/10.1136/bmjopen-2017-020554
Anderson JG, Rogers EE, Baer RJ et al (2018) Racial and ethnic disparities in preterm infant mortality and severe morbidity: a population-based study. Neonatology 113(1):44–54. https://doi.org/10.1159/000480536
Crowe S, Ridout DA, Knowles R et al (2016) Death and emergency readmission of infants discharged after interventions for congenital heart disease: a national study of 7643 infants to inform service improvement. J Am Heart Assoc. https://doi.org/10.1161/jaha.116.003369
Sánchez Luna M, Fernández-Pérez C, Bernal JL et al (2018) Spanish population-study shows that healthy late preterm infants had worse outcomes one year after discharge than term-born infants. Acta Paediatr. https://doi.org/10.1111/apa.14254
Oddie SJ, Hammal D, Richmond S et al (2005) Early discharge and readmission to hospital in the first month of life in the Northern Region of the UK during 1998: a case cohort study. Arch Dis Child 90(2):119–124. https://doi.org/10.1136/adc.2003.040766
Macdonald EM, Ng R, Yudin MH et al (2015) Postpartum maternal and neonatal hospitalizations among women with HIV: a population-based study. AIDS Res Hum Retroviruses 31(10):967–972. https://doi.org/10.1089/aid.2015.0047
Geiger AM, Petitti DB, Yao JF (2001) Rehospitalisation for neonatal jaundice: risk factors and outcomes. Paediatr Perinat Epidemiol 15(4):352–358. https://doi.org/10.1046/j.1365-3016.2001.00374.x
Cools M, Northam W, Goodnight W et al (2019) Thirty-day medical and surgical readmission following prenatal versus postnatal myelomeningocele repair. Neurosurg Focus 47(4):E14. https://doi.org/10.3171/2019.7.Focus19355
Sword WA, Watt S, Krueger PD et al (2001) Understanding newborn infant readmission: findings of the Ontario Mother and Infant Survey. Can J Public Health 92(3):196–200. https://doi.org/10.1007/bf03404304
Goyal N, Zubizarreta JR, Small DS et al (2013) Length of stay and readmission among late preterm infants: an instrumental variable approach. Hosp Pediatr 3(1):7–15. https://doi.org/10.1542/hpeds.2012-0027
Lee S, O’Sullivan DE, Brenner DR et al (2020) Developing and validating multivariable prediction models for predicting the risk of 7-day neonatal readmission following vaginal and cesarean birth using administrative databases. J Matern Fetal Neonatal Med. https://doi.org/10.1080/14767058.2020.1860933
Reed RA, Morgan AS, Zeitlin J et al (2019) Assessing the risk of early unplanned rehospitalisation in preterm babies: EPIPAGE 2 study. BMC Pediatr 19(1):451. https://doi.org/10.1186/s12887-019-1827-6
Mallick AK, Venkatnarayan K, Thapar RK et al (2019) Morbidity patterns of late preterm babies born small for gestation. Indian J Pediatr 86(7):578–583. https://doi.org/10.1007/s12098-019-02925-4
Yu TC, Nguyen C, Ruiz N et al (2019) Prevalence and burden of illness of treated hemolytic neonatal hyperbilirubinemia in a privately insured population in the United States. BMC Pediatr 19(1):53. https://doi.org/10.1186/s12887-019-1414-x
Hensman AM, Erickson-Owens DA, Sullivan MC et al (2020) Determinants of neonatal readmission in healthy term infants: results from a nested case-control study. Am J Perinatol. https://doi.org/10.1055/s-0040-1702936
Bentz MG, Carmona N, Bhagwat MM et al (2018) Beyond “Asian”: specific East and Southeast Asian races or ethnicities associated with jaundice readmission. Hosp Pediatr 8(5):269–273. https://doi.org/10.1542/hpeds.2017-0234
Flaherman V, Schaefer EW, Kuzniewicz MW et al (2018) Health care utilization in the first month after birth and its relationship to newborn weight loss and method of feeding. Acad Pediatr 18(6):677–684. https://doi.org/10.1016/j.acap.2017.11.005
Harron K, Gilbert R, Cromwell D et al (2017) Newborn length of stay and risk of readmission. Paediatr Perinat Epidemiol 31(3):221–232. https://doi.org/10.1111/ppe.12359
Patrick SW, Burke JF, Biel TJ et al (2015) Risk of hospital readmission among infants with neonatal abstinence syndrome. Hosp Pediatr 5(10):513–519. https://doi.org/10.1542/hpeds.2015-0024
Lain SJ, Roberts CL, Bowen JR et al (2015) Early discharge of infants and risk of readmission for jaundice. Pediatrics 135(2):314–321. https://doi.org/10.1542/peds.2014-2388
Moyer LB, Goyal NK, Meinzen-Derr J et al (2014) Factors associated with readmission in late-preterm infants: a matched case-control study. Hosp Pediatr 4(5):298–304. https://doi.org/10.1542/hpeds.2013-0120
Young PC, Korgenski K, Buchi KF (2013) Early readmission of newborns in a large health care system. Pediatrics 131(5):e1538–e1544. https://doi.org/10.1542/peds.2012-2634
Farhat R, Rajab M (2011) Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. N Am J Med Sci 3(3):146–151. https://doi.org/10.4297/najms.2011.3146
Tseng YH, Chen CW, Huang HL et al (2010) Incidence of and predictors for short-term readmission among preterm low-birthweight infants. Pediatr Int 52(5):711–717. https://doi.org/10.1111/j.1442-200X.2010.03129.x
Tomashek KM, Shapiro-Mendoza CK, Weiss J et al (2006) Early discharge among late preterm and term newborns and risk of neonatal morbidity. Semin Perinatol 30(2):61–68. https://doi.org/10.1053/j.semperi.2006.02.003
Escobar GJ, Gonzales VM, Armstrong MA et al (2002) Rehospitalization for neonatal dehydration: a nested case-control study. Arch Pediatr Adolesc Med 156(2):155–161. https://doi.org/10.1001/archpedi.156.2.155
Danielsen B, Castles AG, Damberg CL et al (2000) Newborn discharge timing and readmissions: California, 1992–1995. Pediatrics 106:31–39. https://doi.org/10.1542/peds.106.1.31
Fein EH, Friedlander S, Lu Y et al (2019) Phototherapy for neonatal unconjugated hyperbilirubinemia: examining outcomes by level of care. Hosp Pediatr 9(2):115–120. https://doi.org/10.1542/hpeds.2018-0136
Kosowan L, Mignone J, Chartier M et al (2019) Maternal social and economic factors and infant morbidity, mortality, and congenital anomaly: are there associations? Fam Community Health 42(1):54–61. https://doi.org/10.1097/fch.0000000000000211
Benitz WE (2015) Hospital stay for healthy term newborn infants. Pediatrics 135(5):948–953. https://doi.org/10.1542/peds.2015-0699
Kean N, Turner J, Flatley C et al (2020) Maternal age potentiates the impact of operative birth on serious neonatal outcomes. J Matern Fetal Neonatal Med 33(4):598–605. https://doi.org/10.1080/14767058.2018.1498478
Pinheiro RL, Areia AL, Mota Pinto A et al (2019) Advanced maternal age: adverse outcomes of pregnancy, a meta-analysis. Acta Med Port 32(3):219–26. https://doi.org/10.20344/amp.11057
Balasch J, Gratacós E (2012) Delayed childbearing: effects on fertility and the outcome of pregnancy. Curr Opin Obstet Gynecol 24(3):187–193. https://doi.org/10.1097/GCO.0b013e3283517908
Londero AP, Rossetti E, Pittini C et al (2019) Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth 19(1):261. https://doi.org/10.1186/s12884-019-2400-x
Vo T, Desai M (2021) Immigrant Southeast and East Asian mothers’ transnational postpartum cultural practices: a meta-ethnography. Womens Health (Lond). https://doi.org/10.1177/17455065211060640
Higginbottom GM, Morgan M, Alexandre M et al (2015) Immigrant women’s experiences of maternity-care services in Canada: a systematic review using a narrative synthesis. Syst Rev. https://doi.org/10.1186/2046-4053-4-13
Heys S, Downe S, Thomson G (2021) ‘I know my place’: a meta-ethnographic synthesis of disadvantaged and vulnerable women’s negative experiences of maternity care in high-income countries. Midwifery. https://doi.org/10.1016/j.midw.2021.103123
Campbell OM, Cegolon L, Macleod D et al (2016) Length of stay after childbirth in 92 countries and associated factors in 30 low- and middle-income countries: compilation of Reported Data and a Cross-sectional Analysis from Nationally Representative Surveys. PLoS Med 13(3):e1001972. https://doi.org/10.1371/journal.pmed.1001972
Jones E, Taylor B, MacArthur C et al (2020) Early postnatal discharge for Infants: a meta-analysis. Pediatrics. https://doi.org/10.1542/peds.2019-3365
Brown S, Bruinsma F, Darcy MA et al (2004) Early discharge: no evidence of adverse outcomes in three consecutive population-based Australian surveys of recent mothers, conducted in 1989, 1994 and 2000. Paediatr Perinat Epidemiol 18(3):202–213. https://doi.org/10.1111/j.1365-3016.2004.00558.x
Teulón González M, Martínez Pillado M, Cuadrado Martín MM et al (2017) Effectiveness of an early discharge program after normal childbirth. Rev Calid Asist 32(1):17–20. https://doi.org/10.1016/j.cali.2016.07.005
Benahmed N, San Miguel L, Devos C et al (2017) Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth 17(1):289. https://doi.org/10.1186/s12884-017-1465-7
Malkin JD, Garber S, Broder MS et al (2000) Infant mortality and early postpartum discharge. Obstet Gynecol 96(2):183–188. https://doi.org/10.1016/s0029-7844(00)00894-2
Darling EK, Babe G, Sorbara C et al (2020) Trends in very early discharge from hospital for newborns under midwifery care in Ontario from 2003 to 2017: a retrospective cohort study. CMAJ Open 8(2):E462–E468. https://doi.org/10.9778/cmajo.20190165
Brits H, Adendorff J, Huisamen D et al (2018) The prevalence of neonatal jaundice and risk factors in healthy term neonates at National District Hospital in Bloemfontein. Afr J Prim Health Care Fam Med 10(1):e1–e6. https://doi.org/10.4102/phcfm.v10i1.1582
Boskabadi H, Rakhshanizadeh F, Zakerihamidi M (2020) Evaluation of maternal risk factors in neonatal hyperbilirubinemia. Arch Iran Med 23(2):128–140
Campbell OM, Cegolon L, Macleod D et al (2016) Length of stay after childbirth in 92 countries and associated factors in 30 low- and middle-income countries: compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLoS Med. https://doi.org/10.1371/journal.pmed.1001972
Salas AA, Salazar J, Burgoa CV et al (2009) Significant weight loss in breastfed term infants readmitted for hyperbilirubinemia. BMC Pediatr 9:82. https://doi.org/10.1186/1471-2431-9-82
Ekéus C, Högberg U, Norman M et al (2014) Vacuum assisted birth and risk for cerebral complications in term newborn infants: a population-based cohort study. BMC Pregnancy Childbirth 14:36. https://doi.org/10.1186/1471-2393-14-36
Oakley LL, Henderson J, Redshaw M et al (2014) The role of support and other factors in early breastfeeding cessation: an analysis of data from a maternity survey in England. BMC Pregnancy Childbirth 14:88. https://doi.org/10.1186/1471-2393-14-88
Muchowski KE (2014) Evaluation and treatment of neonatal hyperbilirubinemia. Am Fam Physician 89(11):873–878
Zhou H, Roberts PA, Della PR (2021) Nurse-caregiver communication of hospital-to-home transition information at a tertiary pediatric hospital in Western Australia: a multi-stage qualitative descriptive study. J Pediatr Nurs 60:83–91. https://doi.org/10.1016/j.pedn.2021.02.017
Glick AF, Farkas JS, Nicholson J et al (2017) Parental management of discharge instructions: a systematic review. Pediatrics. https://doi.org/10.1542/peds.2016-4165
Lerret SM (2009) Discharge readiness: an integrative review focusing on discharge following pediatric hospitalization. J Spec Pediatr Nurs 14(4):245–255. https://doi.org/10.1111/j.1744-6155.2009.00205.x
Lerret SM, Weiss ME (2011) How ready are they? Parents of pediatric solid organ transplant recipients and the transition from hospital to home following transplant. Pediatr Transplant 15(6):606–616. https://doi.org/10.1111/j.1399-3046.2011.01536.x
Lerret SM, Weiss ME, Stendahl G et al (2014) Transition from hospital to home following pediatric solid organ transplant: qualitative findings of parent experience. Pediatr Transplant 18:527–537. https://doi.org/10.1111/petr.12269
Lerret SM, Weiss ME, Stendahl GL et al (2015) Pediatric solid organ transplant recipients: transition to home and chronic illness care. Pediatr Transplant. https://doi.org/10.1111/petr.12397
Weiss ME, Sawin KJ, Gralton K et al (2017) Discharge teaching, readiness for discharge, and post-discharge outcomes in parents of hospitalized children. J Pediatr Nurs 34:58–64. https://doi.org/10.1016/j.pedn.2016.12.021
Zhou H, Della PR, Roberts P et al (2016) Utility of models to predict 28-day or 30-day unplanned hospital readmissions: an updated systematic review. BMJ Open 6(6):e011060. https://doi.org/10.1136/bmjopen-2016-011060
Acknowledgements
We would like to acknowledge Ms Marta Rossignoli, Previous Librarian of Child and Adolescent Health Service, Western Australia, for her assistance in the literature search.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
PRD conceptualized and designed the systematic review, participated in the paper selection, data extraction, critical appraisal, and data analyses, critically reviewed the manuscript, and approved the final manuscript as submitted. HH contributed to paper selection and data extraction, critical appraisal and initial analyses, drafted the initial manuscript, and approved the final manuscript as submitted. PAR contributed to the paper selection and data extraction, critical appraisal and initial analyses, critically reviewed the manuscript, and approved the final manuscript as submitted. PP and EA contributed to critical appraisal, critical review of manuscript, and approved the final manuscript as submitted. HZ conceptualized and designed the systematic review, participated in literature search, paper selection, critical appraisal, and data analyses, drafted the initial manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Consent to participate
Not applicable to a systematic review.
Consent to publication
Not applicable to a systematic review.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Della, P.R., Huang, H., Roberts, P.A. et al. Risk factors associated with 31-day unplanned hospital readmission in newborns: a systematic review. Eur J Pediatr 182, 1469–1482 (2023). https://doi.org/10.1007/s00431-023-04819-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04819-2