Abstract
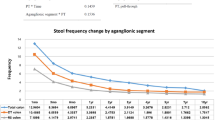
Bowel dysfunction has been proven to be the most typical complication of long-segment Hirschsprung disease (LSHD). Additionally, bowel dysfunction in preschool and early childhood should be properly assessed, because it may result in persistent bowel dysfunction, social issues, and depression in adolescence and adulthood. This study evaluated bowel function during preschool and early childhood in patients with LSHD. A cross-sectional bowel function score (BFS) questionnaire survey was conducted on 270 infants with short-segment Hirschsprung disease (SSHD) and LSHD who underwent pull-through (PT) between January 2014 and December 2019 at the Children’s Hospital of Nanjing Medical University. One hundred ninety patients who consented to the survey were asked to complete the questionnaire and were divided into two groups: the LSHD group (n = 42) and the SSHD group (n = 148). Bowel function outcomes were assessed by using a questionnaire. The total BFS score in the LSHD group was significantly lower than that in the SSHD group (15.0 [14.0, 17.0] vs. 18.0 [16.0, 19.0], p < 0.05) and did not improve with age (p > 0.05). Independent BFS items with lower scores were discovered in LSHD than in SSHD, including the capacity to hold back defecation, feeling/reporting the urge to defecate, frequency, soiling, and accidents (all p < 0.05). After subgroup analysis of follow-up age (3–5 years, 5 ~ 7 years, and > 7 years), there was no difference between the score of ability to hold back defecation over 7 years old and feeling/reporting the urge to defecate over 5 years old (all p > 0.05). The frequency and soiling scores were lower in the LSHD group than in the SSHD group over 5 years of age (all p < 0.05). Fortunately, there was no difference in constipation scores and social problems between the LSHD and SSHD groups in every sub-follow-up group (all p > 0.05).
Conclusion: Overall, bowel function at preschool and early childhood age was poorer in LSHD than in SSHD and did not improve with age. However, the ability to hold back defecation and feeling/reporting the urge to defecate with age in LSHD may be similar to those in SSHD. Simultaneously, the frequency, soiling, and number of accidents were consistently worse in the LSHD group.
Trial registration: This study was retrospectively registered in the ClinicalTrials database.gov (NCT05461924) in August 2022.
What is Known: • Bowel function in SSHD is satisfactory or near-normal, and the general consensus is that the longer the aganglionic segment, the worse the bowel function after surgery. • Bowel functional outcomes of LSHD were not defined, and the limited reports of bowel functional outcomes compared with SSHD were extensively varied. Bowel dysfunction at preschool and early childhood may lead to persistent bowel dysfunction, social problems, and depression in adolescence or adulthood. | |
What is New: • Bowel function in preschool and early childhood in patients with LSHD has not been defined and should be thoroughly assessed in a larger group of patients with precise definitions of incontinence or soiling. • The present study was primarily designed to evaluate bowel function at preschool and early childhood age in LSHD compared with SSHD in a relatively large number of HD cases using BFS. |

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are available from the corresponding authors upon reasonable request.
References
Lu C, Hou G, Liu C (2017) Single-stage transanal endorectal pull-through procedure for correction of Hirschsprung disease in neonates and nonneonates: a multicenter study. J Pediatr Surg 52(7):1102–1107
Fang Y, Bai J, Zhang B (2020) Laparoscopic Soave procedure for long-segment Hirschsprung’s disease - single-center experience. Videosurgery and Other Miniinvasive Techniques 15(1):234–238
Kawaguchi AL, Guner YS, Somme S (2021) Management and outcomes for long-segment Hirschsprung disease: a systematic review from the APSA Outcomes and Evidence Based Practice Committee. J Pediatr Surg 56(9):1513–1523
Kim SH, Cho YH, Kim HY (2021) Assessment of defecation function beyond infantile period for transanal single-stage endorectal pull-through in Hirschsprung disease. Annals of Surgical Treatment and Research 101(4):231–239
Bystrom C, Ostlund S, Hoff N (2021) Evaluation of bowel function, urinary tract function, and quality of life after transanal endorectal pull-through surgery for Hirschsprung’s disease. Eur J Pediatr Surg 31(1):40–48
Verkuijl SJ, Meinds RJ, van der Steeg A (2022) Functional outcomes after surgery for total colonic, long-segment, versus rectosigmoid segment Hirschsprung disease. JOURNAL OF PEDIATRIC GASTROENTEROLOGY AND NUTRITION 74(3):348–354
Stenstrom P, Brautigam M, Borg H (2017) Patient-reported Swedish nationwide outcomes of children and adolescents with total colonic aganglionosis. J Pediatr Surg 52(8):1302–1307
Chung P, Wong K, Tam P (2018) Are all patients with short segment Hirschsprung’s disease equal? A retrospective multicenter study. Pediatr Surg Int 34(1):47–53
Chan K, Lee KH, Wong H (2021) Long-term results of one-stage laparoscopic-assisted endorectal pull-through for rectosigmoid Hirschsprung’s disease in patients aged above 5 years. J Laparoendosc Adv Surg Tech 31(2):225–229
Townley OG, Lindley RM, Cohen MC (2020) Functional outcome, quality of life, and ‘failures’ following pull-through surgery for Hirschsprung’s disease: a review of practice at a single-center. J Pediatr Surg 55(2):273–277
Fosby MV, Stensrud KJ, Bjornland K (2020) Bowel function after transanal endorectal pull-through for Hirschsprung disease - does outcome improve over time? J Pediatr Surg 55(11):2375–2378
Dai Y, Deng Y, Lin Y (2020) Long-term outcomes and quality of life of patients with Hirschsprung disease: a systematic review and meta-analysis. BMC Gastroenterol 20(1):67
Drissi F, Meurette G, Baayen C (2019) Long-term outcome of Hirschsprung disease: impact on quality of life and social condition at adult age. Dis Colon Rectum 62(6):727–732
Meinds RJ, van der Steeg A, Sloots C (2019) Long-term functional outcomes and quality of life in patients with Hirschsprung’s disease. Br J Surg 106(4):499–507
Tran VQ, Mahler T, Dassonville M (2018) Long-term outcomes and quality of life in patients after soave pull-through operation for Hirschsprung’s disease: an observational retrospective study. Eur J Pediatr Surg 28(5):445–454
Kyrklund K, Neuvonen MI, Pakarinen MP (2018) Social morbidity in relation to bowel functional outcomes and quality of life in anorectal malformations and Hirschsprung’s disease. Eur J Pediatr Surg 28(6):522–528
Peng C, Tan SS, Pang W (2021) Rectourethral and rectovesical fistula as serious and rare complications after Hirschsprung disease operation: experience in seven patients. J Pediatr Surg 56(2):263–268
Jiao C, Zhuansun D, He Y (2022) Transanal full-thickness pull-through approach in the treatment of anastomotic leakage after operation for Hirschsprung disease. Pediatr Surg Int 38(9):1263–1271
Oyania F, Ogwal A, Nimanya S (2020) Long term bowel function after repair of anorectal malformations in Uganda. J Pediatr Surg 55(7):1400–1404
van der Steeg H, van Rooij I, Iacobelli BD (2022) Bowel function and associated risk factors at preschool and early childhood age in children with anorectal malformation type rectovestibular fistula: An ARM-Net consortium study. J Pediatr Surg 57(9):89–96
Verkuijl SJ, Jonker JE, Trzpis M (2021) Functional outcomes of surgery for colon cancer: a systematic review and meta-analysis. EJSO 47(5):960–969
Magdeburg J, Glatz N, Post S (2016) Long-term functional outcome of colonic resections: how much does faecal impairment influence quality of life? Colorectal Dis 18(11):O405–O413
Hoel AT, Tofft L, Bjornland K (2021) Reaching adulthood with Hirschsprung’s disease: patient experiences and recommendations for transitional care. J Pediatr Surg 56(2):257–262
Roorda D, Verkuij SJ, Derikx J (2022) Did age at surgery influence outcome in patients with Hirschsprung disease? A nationwide cohort study in the Netherlands. Journal Of Pediatric Gastroentology And Nutrition 75(4):431–437
Sakurai T, Tanaka H, Endo N (2021) Predictive factors for the development of postoperative Hirschsprung-associated enterocolitis in children operated during infancy. Pediatr Surg Int 37(2):275–280
Gunadi M, C.T., Stevie, (2022) Long-term functional outcomes of patients with Hirschsprung disease following pull-through. BMC Pediatr 22(1):246
Yuan Y, Xu M, Yang H (2021) The efficacy of biofeedback therapy for the treatment of fecal incontinence after soave procedure in children for Hirschsprung’s disease. Front Pediatr 9:638120
Kyrklund K, Koivusalo A, Rintala RJ (2012) Evaluation of bowel function and fecal continence in 594 Finnish individuals aged 4 to 26 years. Dis Colon Rectum 55(6):671–676
Wood RJ, Levitt MA (2018) Anorectal malformations. Clin Colon Rectal Surg 31(2):61–70
Choi BJ, Kwon W, Baek SH (2020) Single-port laparoscopic Deloyers procedure for tension-free anastomosis after extended left colectomy or subtotal colectomy: a 6-patient case series. Medicine 99(31):e21421
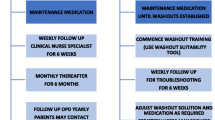
Saadai P, Trappey AF, Goldstein AM (2019) Guidelines for the management of postoperative soiling in children with Hirschsprung disease. Pediatr Surg Int 35(8):829–834
Saad SA, Elseed M, AbouZeid AA (2020) Histopathological perspective of the pulled-through colon in Hirschsprung disease: impact on clinical outcome. J Pediatr Surg 55(9):1829–1833
Brooks LA, Fowler KL, Veras LV (2020) Resection margin histology may predict intermediate-term outcomes in children with rectosigmoid Hirschsprung disease. Pediatr Surg Int 36(8):875–882
Coyle D, O’Donnell AM, Tomuschat C (2019) The extent of the transition zone in Hirschsprung disease. J Pediatr Surg 54(11):2318–2324
Kapur RP, Smith C, Ambartsumyan L (2020) Postoperative pullthrough obstruction in Hirschsprung disease: etiologies and diagnosis. Pediatric Aand Developmental Pathology 23(1):40–59
Langer JC, Rollins MD, Levitt M (2017) Guidelines for the management of postoperative obstructive symptoms in children with Hirschsprung disease. Pediatr Surg Int 33(5):523–526
Ghosh DN, Liu Y, Cass DT (2017) Transition zone pull-through in Hirschsprung’s disease: a tertiary hospital experience. ANZ J Surg 87(10):780–783
Fernandez IM, Sanchez MJ, Martinez CI (2014) Quality of life and long term results in Hirschsprung’s disease]. Cir Pediatr 27(3):117–124
Xiong X, Chen X, Wang G (2015) Long term quality of life in patients with Hirschsprung’s disease who underwent heart-shaped anastomosis during childhood: a twenty-year follow-up in China. J Pediatr Surg 50(12):2044–2047
Funding
This study was funded by the Top of Jiangsu Provincial Health Committee’s Six One Project, China (LGY2020019); Jiangsu Provincial Key Research and Development Program, China (BE2017609); and the General Project of the Nanjing Health Commission (YKK20121).
Author information
Authors and Affiliations
Contributions
Weibing Tang and Weiwei Jiang contributed to the conception and design of the study and were the corresponding authors. Shiwen Pan, Xinyi Hua, and Changgui Lu organized the database and performed statistical analyses. Changgui Lu wrote the first draft of the manuscript. Xinyi Hua, Shiwen Pan, and Changgui Lu contributed equally to the study. All authors contributed to the manuscript revision and read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all the participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lu, C., Pan, S., Hua, X. et al. Bowel function at preschool and early childhood age in children with long-segment Hirschsprung disease. Eur J Pediatr 182, 1251–1259 (2023). https://doi.org/10.1007/s00431-023-04814-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04814-7