Abstract
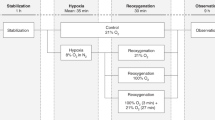
The main purpose of this study was to evaluate the impact of drip versus intermittent feeding on splanchnic oxygenation in preterm infants with intrauterine growth restriction. The second objective was to assess the relationship between fetal splanchnic circulation parameters and splanchnic oxygenation during the first week of life. A single-center, prospective, randomized study with 51 fetuses/infants was conducted. Fetal Doppler measurements including umbilical artery, middle cerebral artery, and superior mesenteric artery (SMA) were recorded in IUGR fetuses. After preterm delivery, the infants were randomly assigned to one of two feeding modalities: drip (3-h continuous) or intermittent (bolus in 10 min). Continuous regional splanchnic saturation (rSO2S) monitoring was carried out during the first week of life, simultaneously with continuous oxygen arterial saturation (SaO2) monitoring, and the infants’ fractional oxygen extractions (FOE) were calculated. These parameters were evaluated as means on a daily basis for the first week of life, as well as pre-prandial and post-prandial measurements on the seventh day. Fetal Doppler flow velocimetry disturbances were present in 72.5% of the study cohort. The drip (26 infants) and intermittent (25 infants) groups were similar in demographic and clinical characteristics, as well as the prevalence of feeding intolerance and necrotizing enterocolitis. During the first week of life, there was no difference in daily mean rSO2S and FOE values between the drip and intermittent groups, whereas unfed infants had mostly lower rSO2S values. Pre-prandial and post-prandial rSO2S values remained stable in both groups. Also, no association was detected between fetal splanchnic circulation parameters and neonatal splanchnic oxygenation. RSO2S values were strongly correlated to gestational age and birth weight. During the whole week, except for the first 2 days, infants with umbilical catheters had significantly lower rSO2S values than infants without.
Conclusion: Our data suggest that the key factor in splanchnic oxygenation is feeding, not the feeding modality. In addition, the umbilical vein catheter had a negative impact on splanchnic oxygenation.
Clinical Trial Registration: The Effect of Neonatal Feeding Modalities on Splanchnic Oxygenation, NCT05513495, https://clinicaltrials.gov/ct2/results cond=&term=NCT05513495&cntry=TR&state=&city=&dist=. Retrospectively registered, date of registration: August 2022.
What is Known: |
• It is known that preterm infants with IUGR are at increased risk of hypoxic-ischemic intestinal damage and impaired splanchnic oxygenation. |
What is New: |
• The key factor in splanchnic oxygenation of preterm infants with IUGR is feeding, not the feeding modality (drip or intermittent). |
• In addition, the umbilical vein catheter had a negative impact on splanchnic oxygenation. |



Similar content being viewed by others
Data availability
Data were recorded in SPSS. The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AREDF:
-
Absent or reversed end-diastolic blood flow
- DOL:
-
Day of life
- FEF:
-
Full enteral feeding
- FI:
-
Feeding intolerance
- FMP:
-
First meconium passage
- FOE:
-
Fractional oxygen extractions
- IUGR:
-
Intrauterine growth restriction
- MCA:
-
Middle cerebral artery
- NEC:
-
Necrotizing enterocolitis
- NICU:
-
Neonatal intensive care unit
- NIRS:
-
Near-infrared spectroscopy
- rSO2S:
-
Regional splanchnic saturation
- SMA:
-
Superior mesenteric artery
- SaO2 :
-
Oxygen arterial saturation
- UA:
-
Umbilical artery
- UAC:
-
Umbilical artery catheters
- UVC:
-
Umbilical vein catheter
- WOL:
-
Week of life
References
Kiserud T, Ebbing C, Kessler J, Rasmussen S (2006) Fetal cardiac output, distribution to the placenta and impact of placental compromise. Ultrasound Obstet Gynecol 28(2):126–136
Stampalija T, Casati D, Monasta L, Sassi R, Rivolta MW, Muggiasca ML et al (2016) Brain sparing effect in growth-restricted fetuses is associated with decreased cardiac acceleration and deceleration capacities: a case-control study. BJOG 123(12):1947–1954
Ebbing C, Rasmussen S, Godfrey KM, Hanson MA, Kiserud T (2009) Redistribution pattern of fetal liver circulation in intrauterine growth restriction. Acta Obstet Gynecol Scand 88(10):1118–1123
Watkins DJ, Besner GE (2013) The role of the intestinal microcirculation in necrotizing enterocolitis. Semin Pediatr Surg 22(2):83–87
Surmeli Onay O, Korkmaz A, Yigit S, Yurdakok M (2020) Hypoxic-ischemic enterocolitis: a proposal of a new terminology for early NEC or NEC-like disease in preterm infants, a single-center prospective observational study. Eur J Pediatr 179(4):561–570
Robel-Tillig E, Vogtmann C, Faber R (2000) Postnatal intestinal disturbances in small-for-gestational-age premature infants after prenatal haemodynamic disturbances. Acta Paediatr 89(3):324–330
Bora R, Mukhopadhyay K, Saxena AK, Jain V, Narang A (2009) Prediction of feed intolerance and necrotizing enterocolitis in neonates with absent end diastolic flow in umbilical artery and the correlation of feed intolerance with postnatal superior mesenteric artery flow. J Matern Fetal Neonatal Med 22(11):1092–1096
Martini S, Corvaglia L (2018) Splanchnic NIRS monitoring in neonatal care: rationale, current applications and future perspectives. J Perinatol 38(5):431–443
Bozzetti V, Paterlini G, De Lorenzo P, Gazzolo D, Valsecchi MG, Tagliabue PE (2016) Impact of continuous vs bolus feeding on splanchnic perfusion in very low birth weight infants: a randomized trial. J Pediatr 176(86–92):e2
Murdoch EM, Sinha AK, Shanmugalingam ST, Smith GC, Kempley ST (2006) Doppler flow velocimetry in the superior mesenteric artery on the first day of life in preterm infants and the risk of neonatal necrotizing enterocolitis. Pediatrics 118(5):1999–2003
Achiron R, Orvieto R, Lipitz S, Yagel S, Rotstein Z (1998) Superior mesenteric artery blood flow velocimetry: cross-sectional Doppler sonographic study in normal fetuses. J Ultrasound Med 17(12):769–773
Kivilevitch Z, Salomon LJ, Yagel S, Achiron R (2011) Bowel circulation in normally grown and growth-restricted fetuses. J Ultrasound Med 30(11):1529–1537
Achiron R, Mazkereth R, Orvieto R, Kuint J, Lipitz S, Rotstein Z (2002) Echogenic bowel in intrauterine growth restriction fetuses: does this jeopardize the gut? Obstet Gynecol 100(1):120–125
Ebbing C, Rasmussen S, Kiserud T (2007) Middle cerebral artery blood flow velocities and pulsatility index and the cerebroplacental pulsatility ratio: longitudinal reference ranges and terms for serial measurements. Ultrasound Obstet Gynecol 30(3):287–296
Bahado-Singh RO, Kovanci E, Jeffres A, Oz U, Deren O, Copel J et al (1999) The Doppler cerebroplacental ratio and perinatal outcome in intrauterine growth restriction. Am J Obstet Gynecol 180(3 Pt 1):750–756
Fenton TR (2003) A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr 3:13
Olsen IE, Groveman SA, Lawson ML, Clark RH, Zemel BS (2010) New intrauterine growth curves based on United States data. Pediatrics 125(2):e214-224
Arnoldi R, Leva E, Macchini F, Di Cesare A, Colnaghi M, Fumagalli M et al (2011) Delayed meconium passage in very low birth weight infants. Eur J Pediatr Surg 21(6):395–398
Moore TA, Wilson ME (2011) Feeding intolerance: a concept analysis. Adv Neonatal Care 11(3):149–154
Walsh MC, Kliegman RM (1986) Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am 33(1):179–201
Papile LA, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 92(4):529–534
Montaldo P, De Leonibus C, Giordano L, De Vivo M, Giliberti P (2015) Cerebral, renal and mesenteric regional oxygen saturation of term infants during transition. J Pediatr Surg 50(8):1273–1277
van der Heide M, Dotinga BM, Stewart RE, Kalteren WS, Hulscher JBF, Reijneveld SA et al (2021) Regional splanchnic oxygen saturation for preterm infants in the first week after birth: reference values. Pediatr Res 90(4):882–887
Bailey SM, Hendricks-Munoz KD, Mally P (2014) Cerebral, renal, and splanchnic tissue oxygen saturation values in healthy term newborns. Am J Perinatol 31(4):339–344
Patel AK, Lazar DA, Burrin DG, Smith EO, Magliaro TJ, Stark AR et al (2014) Abdominal near-infrared spectroscopy measurements are lower in preterm infants at risk for necrotizing enterocolitis. Pediatr Crit Care Med 15(8):735–741
McNeill S, Gatenby JC, McElroy S, Engelhardt B (2011) Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J Perinatol 31(1):51–57
Azhibekov T, Noori S, Soleymani S, Seri I (2014) Transitional cardiovascular physiology and comprehensive hemodynamic monitoring in the neonate: relevance to research and clinical care. Semin Fetal Neonatal Med 19(1):45–53
Ledo A, Aguar M, Nunez-Ramiro A, Saenz P, Vento M (2017) Abdominal near-infrared spectroscopy detects low mesenteric perfusion early in preterm infants with hemodynamic significant ductus arteriosus. Neonatology 112(3):238–245
Bozzetti V, Tagliabue PE (2017) Enteral feeding of intrauterine growth restriction preterm infants: theoretical risks and practical implications. Pediatr Med Chir 39(2):160
Dave V, Brion LP, Campbell DE, Scheiner M, Raab C, Nafday SM (2009) Splanchnic tissue oxygenation, but not brain tissue oxygenation, increases after feeds in stable preterm neonates tolerating full bolus orogastric feeding. J Perinatol 29(3):213–218
Dani C, Pratesi S, Barp J, Bertini G, Gozzini E, Mele L et al (2013) Near-infrared spectroscopy measurements of splanchnic tissue oxygenation during continuous versus intermittent feeding method in preterm infants. J Pediatr Gastroenterol Nutr 56(6):652–656
Corvaglia L, Martini S, Battistini B, Rucci P, Aceti A, Faldella G (2014) Bolus vs. continuous feeding: effects on splanchnic and cerebral tissue oxygenation in healthy preterm infants. Pediatr Res 76(1):81–85
Kuik SJ, van Zoonen A, Bos AF, Van Braeckel K, Hulscher JBF, Kooi EMW (2019) The effect of enteral bolus feeding on regional intestinal oxygen saturation in preterm infants is age-dependent: a longitudinal observational study. BMC Pediatr 19(1):404
Martini S, Aceti A, Beghetti I, Faldella G, Corvaglia L (2018) Feed-related splanchnic oxygenation in preterm infants with abnormal antenatal Doppler developing gut complications. J Pediatr Gastroenterol Nutr 66(5):755–759
Premji SS, Chessell L (2011) Continuous nasogastric milk feeding versus intermittent bolus milk feeding for premature infants less than 1500 grams. Cochrane Database Syst Rev (11):CD001819.
Gillam-Krakauer M, Cochran CM, Slaughter JC, Polavarapu S, McElroy SJ, Hernanz-Schulman M et al (2013) Correlation of abdominal rSO2 with superior mesenteric artery velocities in preterm infants. J Perinatol 33(8):609–612
Arman D, Sancak S, Gursoy T, Topcuoglu S, Karatekin G, Ovali F (2020) The association between NIRS and Doppler ultrasonography in preterm infants with patent ductus arteriosus. J Matern Fetal Neonatal Med 33(7):1245–1252
Velipasaoglu M, Surmeli Onay O, Saglik AC, Aydemir O, Tanir HM, Tekin AN (2022) The relationship of foetal superior mesenteric artery blood flow and the time to first meconium passage in newborns with late-onset foetal growth restriction. J Obstet Gynaecol 1–6
Roll C, Hanssler L (1998) Effect of umbilical arterial catheters on intestinal blood supply. Acta Paediatr 87(9):955–959
Shah JB, Bracero LA, Gewitz MH, Fish BG, Dweck HS (1998) Umbilical artery catheters and blood flow velocities in the superior mesenteric artery: effect of insertion, removal, aspiration, and bolus infusion. J Clin Ultrasound 26(2):73–77
Sulemanji M, Vakili K, Zurakowski D, Tworetzky W, Fishman SJ, Kim HB (2017) Umbilical venous catheter malposition is associated with necrotizing enterocolitis in premature infants. Neonatology 111(4):337–343
Dotinga BM, Mintzer JP, Moore JE, Hulscher JBF, Bos AF, Kooi EMW (2020) Maturation of intestinal oxygenation: a review of mechanisms and clinical implications for preterm neonates. Front Pediatr 8:354
Funding
This study was supported by Eskisehir Osmangazi University Scientific Research Projects Coordination Unit under grant no. 61690618-604.99-E.61140. There has been no involvement in study design, collection of analysis, interpretation of data, writing of the report, and decision to submit the manuscript for publication by Eskisehir Osmangazi University Scientific Research Projects Coordination Unit.
Author information
Authors and Affiliations
Contributions
Dr. Surmeli Onay: conceptualized and designed the study, coordinated and supervised data collection, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. Drs. Velipasaoglu and Tanır: designed the data collection instruments, collected data, carried out the initial analyses, and reviewed and revised the manuscript. Dr. Surmeli Onay and Dr. Velipasaoglu have contributed equally as the first authors of this article. Drs. Tutal, Sarılar, and Cakil Saglık designed the data collection instruments, collected data, and carried out the initial analyses. Mr. Bilgin carried out the statistical analyses, and reviewed and revised the manuscript. Drs. Aydemir, Barsan Kaya, and Tekin coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. Each author has seen and approved the submission of this version of the manuscript and takes full responsibility for the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was performed in line with the Declaration of Helsinki and the Institutional Ethics Committee approved the study (No: 80558721–050.99-E.105607).
Consent to participate
Written informed consent was obtained from all subjects (from all parents or legal guardians).
Consent for publication
All the patient data are anonymized, and parents and legal guardians consented to the publication of the results of the project.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
431_2023_4810_MOESM2_ESM.docx
Supplementary file2 Supplement Figure The course of daily mean regional splanchnic oxygen saturation (rSO2S) measurements in infants with and without umbilical catheters during the first week of life. *p < 0.05 (JPG 99 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Surmeli Onay, O., Velipasaoğlu, M., Tutal, M. et al. The effect of drip versus intermittent feeding on splanchnic oxygenation in preterm infants with intrauterine growth restriction: a prospective randomized trial. Eur J Pediatr 182, 1317–1328 (2023). https://doi.org/10.1007/s00431-023-04810-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04810-x