Abstract
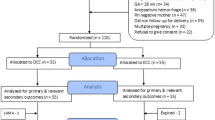
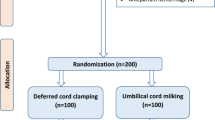
Recommendations for umbilical cord management in intrauterine growth-restricted (IUGR) neonates are lacking. The present randomized controlled trial compared hemodynamic effects of umbilical cord milking (UCM) with delayed cord clamping (DCC) in IUGR neonates > 28 weeks of gestation, not requiring resuscitation. One hundred seventy IUGR neonates were randomly allocated to intact UCM (4 times squeezing of 20 cm intact cord; n = 85) or DCC (cord clamping after 60 s; n = 85) immediately after delivery. The primary outcome variable was superior vena cava (SVC) blood flow at 24 ± 2 h. Secondary outcomes assessed were anterior cerebral artery (ACA) and superior mesenteric artery (SMA) blood flow indices, right ventricular output (RVO), regional cerebral oxygen saturation (CrSO2) and venous hematocrit at 24 ± 2 h, peak total serum bilirubin (TSB), incidences of in-hospital complications, need and duration of respiratory support, and hospital stay. SVC flow was significantly higher in UCM compared to DCC (111.95 ± 33.54 and 99.49 ± 31.96 mL/kg/min, in UCM and DCC groups, respectively; p < 0.05). RVO and ACA/SMA blood flow indices were comparable whereas CrSO2 was significantly higher in UCM group. Incidences of polycythemia and jaundice requiring phototherapy were similar despite significantly higher venous hematocrit and peak TSB in UCM group. The need for non-invasive respiratory support was significantly higher in UCM group though the need and duration of mechanical ventilation and other outcomes were comparable.
Conclusions: UCM significantly increases SVC flow, venous hematocrit, and CrSO2 compared to DCC in IUGR neonates without any difference in other hemodynamic parameters and incidences of polycythemia and jaundice requiring phototherapy; however, the need for non-invasive respiratory support was higher with UCM.
Trial registration: Clinical trial registry of India (CTRI/2021/03/031864).
What is Known: |
• Umbilical cord milking (UCM) increases superior vena cava blood flow (SVC flow) and hematocrit without increasing the risk of symptomatic polycythemia and jaundice requiring phototherapy in preterm neonates compared to delayed cord clamping (DCC). |
• An association between UCM and intraventricular hemorrhage in preterm neonates < 28 weeks of gestation is still being investigated. |
What is New: |
• Placental transfusion by UCM compared to DCC increases SVC flow, regional cerebral oxygenation, and hematocrit without increasing the incidence of symptomatic polycythemia and jaundice requiring phototherapy in intrauterine growth-restricted neonates. |
• UCM also increases the need for non-invasive respiratory support compared to DCC. |

Similar content being viewed by others
Availability of data and material
Deidentified individual participant data (including data dictionaries) will be made available, in addition to study protocols, the statistical analysis plan, and the informed consent form. The data will be made available upon publication to researchers who provide a methodologically sound proposal for use in achieving the goals of the approved proposal. Proposals should be submitted to chaitra.s.angadi@gmail.com.
Code availability
N/A.
Abbreviations
- ACA:
-
Anterior cerebral artery
- CBF:
-
Cerebral blood flow
- CI:
-
Confidence interval
- CPAP:
-
Continuous positive airway pressure
- CrSO2 :
-
Regional cerebral oxygenation saturation
- CTRI:
-
Clinical Trial Registry of India
- DCC:
-
Delayed cord clamping
- DR-CPAP:
-
Delivery room continuous positive airway pressure
- ECC:
-
Early cord clamping
- EDV:
-
End-diastolic velocity
- GA:
-
Gestational age
- IQR:
-
Interquartile range
- IUGR:
-
Intrauterine growth restriction
- IVH:
-
Intraventricular hemorrhage
- MD:
-
Mean difference
- n :
-
Number
- N :
-
Total number in that population
- NEC:
-
Necrotizing enterocolitis
- PSV:
-
Peak systolic velocity
- RCT:
-
Randomized controlled trial
- RI:
-
Resistive index
- RR:
-
Relative risk
- RVO:
-
Right ventricular output
- SD:
-
Standard deviation
- SMA:
-
Superior mesenteric artery
- SVC:
-
Superior vena cava
- TSB:
-
Total serum bilirubin
- UA:
-
Umbilical artery
- VTI:
-
Velocity time integral
References
Aziz K, Lee CHC, Escobedo MB, Hoover AV, Kamath-Rayne BD, Kapadia VS, Magid DJ, Niermeyer S, Schmölzer GM, Szyld E et al (2021) Part 5: Neonatal Resuscitation 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 147(Suppl 1):e2020038505E
Madar J, Roehr CC, Ainsworth S, Ersdal H, Morley C, Rüdiger M, Skåre C, Szczapa T, Te Pas A, Trevisanuto D et al (2021) European Resuscitation Council Guidelines 2021: newborn resuscitation and support of transition of infants at birth. Resuscitation 161:291–326
Rabe H, Gyte GM, Díaz-Rossello JL, Duley L (2019) Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev 9:CD003248
Wang M, Mercer JS, Padbury JF (2018) Delayed cord clamping in infants with suspected intrauterine growth restriction. J Pediatr 201:264–268
Chopra A, Thakur A, Garg P, Kler N, Gujral K (2018) Early versus delayed cord clamping in small for gestational age infants and iron stores at 3 months of age - a randomized controlled trial. BMC Pediatr 18:234
Digal KC, Singh P, Srivastava Y, Chaturvedi J, Tyagi AK, Basu S (2021) Effects of delayed cord clamping in intrauterine growth-restricted neonates: a randomized controlled trial. Eur J Pediatr 180:1701–1710
Brown BE, Shah PS, Afifi JK, Sherlock RL, Adie MA, Monterrosa LA, Crane JM, Ye XY, El-Naggar WI, Neonatal C, Network; Canadian Preterm Birth Network Investigators, (2022) Delayed cord clamping in small for gestational age preterm infants. Am J Obstet Gynecol 226:247.e1-247.e10
Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN (2015) Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics 136:61–69
Mangla MK, Thukral A, Sankar MJ, Agarwal R, Deorari AK, Paul VK (2020) Effect of umbilical cord milking vs delayed cord clamping on venous hematocrit at 48 hours in late preterm and term neonates: a randomized controlled trial. Indian Pediatr 57:1119–1123
Jaiswal P, Upadhyay A, Gothwal S, Singh D, Dubey K, Garg A, Vishnubhatala S (2015) Comparison of two types of intervention to enhance placental redistribution in term infants: randomized control trial. Eur J Pediatr 174:1159–1167
Sura M, Osoti A, Gachuno O, Musoke R, Kagema F, Gwako G, Ondieki D, Ndavi PM, Ogutu O (2021) Effect of umbilical cord milking versus delayed cord clamping on preterm neonates in Kenya: a randomized controlled trial. PLoS ONE 16:e0246109
Katheria A, Reister F, Essers J, Mendler M, Hummler H, Subramaniam A, Carlo W, Tita A, Truong G, Davis-Nelson S et al (2019) Association of umbilical cord milking vs delayed umbilical cord clamping with death or severe intraventricular hemorrhage among preterm infants. JAMA 322:1877–1886
Katheria AC, Szychowski JM, Essers J, Mendler MR, Dempsey EM, Schmölzer GM, Arnell K, Rich WD, Hassen K, Allman P et al (2020) Early cardiac and cerebral hemodynamics with umbilical cord milking compared with delayed cord clamping in infants born preterm. J Pediatr 223:51-56.e1
Montaldo P, Puzone S, Caredda E, Pugliese U, Inserra E, Cirillo G, Gicchino F, Campana G, Ursi D, Galdo F et al (2022) Impact of intrauterine growth restriction on cerebral and renal oxygenation and perfusion during the first 3 days after birth. Sci Rep 12:5067
Papageorghiou AT, Ohuma EO, Altman DG, Todros T, Cheikh Ismail L, Lambert A, Jaffer YA, Bertino E, Gravett MG, Purwar M, International Fetal and Newborn Growth Consortium for the 21st Century (INTERGROWTH-21st) et al (2014) International standards for fetal growth based on serial ultrasound measurements: the Fetal Growth Longitudinal Study of the INTERGROWTH-21st Project. Lancet 384:869–879
Papile LA, Burstein J, Burstein R, Koffler H (1978) Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 92:529–534
Fanaro S (2013) Feeding intolerance in the preterm infant. Early Hum Dev 89(Suppl 2):S13-20
Kliegman RM, Walsh MC (1987) Neonatal necrotizing enterocolitis: pathogenesis, classification, and spectrum of illness. Curr Probl Pediatr 17:213–288. https://doi.org/10.1016/0045-9380(87)90031-4
Evans N, Kluckow M, Simmons M, Osborn D (2002) Which to measure, systemic or organ blood flow? Middle cerebral artery and superior vena cava flow in very preterm infants. Arch Dis Child Fetal Neonatal Ed 87:F181–F184
Yanowitz TD, Yao AC, Pettigrew KD, Werner JC, Oh W (1985) Stonestreet BS (1999) Postnatal hemodynamic changes in very-low-birth weight infants. J Appl Physiol 87:370–380
Kluckow M, Evans N (2000) Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed 82:F182–F187
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia (2004) Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 114:297–316. https://doi.org/10.1542/peds.114.1.297.Erratum.In:Pediatrics114:1138
National Collaborating Centre for Women’s and Children’s Health. Neonatal jaundice: Clinical guideline. 2010. https://www.nice.org.uk/guidance/cg98/evidence/full-guideline-245411821. Last accessed on 13 March, 2023
Turan OM, Turan S, Gungor S, Berg C, Moyano D, Gembruch U, Nicolaides KH, Harman CR, Baschat AA (2008) Progression of Doppler abnormalities in intrauterine growth restriction. Ultrasound Obstet Gynecol 32:160–167
Leipälä JA, Boldt T, Turpeinen U, Vuolteenaho O, Fellman V (2003) Cardiac hypertrophy and altered hemodynamic adaptation in growth-restricted preterm infants. Pediatr Res 53:989–993
Sehgal A, Doctor T, Menahem S (2013) Cardiac function and arterial biophysical properties in small for gestational age infants: postnatal manifestations of fetal programming. J Pediatr 63:1296–1300
Drayton MR, Skidmore R (1987) Vasoactivity of the major intracranial arteries in newborn infants. Arch Dis Child 62:236–240
Sloot SC, de Waal KA, van der Lee JH, van Kaam AH (2010) Central blood flow measurements in stable preterm infants after the transitional period. Arch Dis Child Fetal Neonatal Ed 95:F369–F372
Giussani DA (2016) The fetal brain sparing response to hypoxia: physiological mechanisms. J Physiol 594:1215–1230
Cohen E, Baerts W, van Bel F (2015) Brain-sparing in intrauterine growth restriction: considerations for the neonatologist. Neonatology 108:269–276
Banait N, Suryawanshi P, Malshe N, Nagpal R, Lalwani S (2013) Cardiac blood flow measurements in stable full term small for gestational age neonates. J Clin Diagn Res 7:1651–1654
Farag MM, Thabet MAEH, Abd-Almohsen AM, Ibrahim HIAM (2022) The effect of placental transfusion on hemodynamics in premature newborns: a randomized controlled trial. Eur J Pediatr 181:4121–4133
Finn D, Ryan DH, Pavel A, O’Toole JM, Livingstone V, Boylan GB, Kenny LC, Dempsey EM (2019) Clamping the Umbilical Cord in Premature Deliveries (CUPiD): neuromonitoring in the immediate newborn period in a randomized, controlled trial of preterm infants born at <32 weeks of gestation. J Pediatr 208:121-126.e2
Rabe H, Jewison A, Fernandez Alvarez R, Crook D, Stilton D, Bradley R, Holden D; Brighton Perinatal Study Group (2011) Milking compared with delayed cord clamping to increase placental transfusion in preterm neonates: a randomized controlled trial. Obstet Gynecol 117(2 Pt 1):205–211
Shirk SK, Manolis SA, Lambers DS, Smith KL (2019) Delayed clamping vs milking of umbilical cord in preterm infants: a randomized controlled trial. Am J Obstet Gynecol 220:482.e1-482.e8
Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, Okada T, Takahashi S, Harada K (2008) Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks’ gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 93:F14–F19
Ortiz-Esquinas I, Gómez-Salgado J, Rodriguez-Almagro J, Arias-Arias Á, Ballesta-Castillejos A, Hernández-Martínez A (2020) Umbilical cord milking in infants born at <37 weeks of gestation: a systematic review and meta-analysis. J Clin Med 9:1071
Usher R, Shephard M, Lind J (1963) The blood volume of the newborn infant and placental transfusion. Acta Paediatr (Stockh) 52:497–512
Kumbhat N, Eggleston B, Davis AS, DeMauro SB, Van Meurs KP, Foglia EE, Lakshminrusimha S, Walsh MC, Watterberg KL, Wyckoff MH; Generic Database Subcommittee of the National Institute of Child Health and Human Development Neonatal Research Network et al (2021) Umbilical cord milking vs delayed cord clamping and associations with in-hospital outcomes among extremely premature infants. J Pediatr 232:87–94.e4
Balasubramanian H, Ananthan A, Jain V, Rao SC, Kabra N (2020) Umbilical cord milking in preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 105:572–580
Blank DA, Polglase GR, Kluckow M, Gill AW, Crossley KJ, Moxham A, Rodgers K, Zahra V, Inocencio I, Stenning F et al (2018) Haemodynamic effects of umbilical cord milking in premature sheep during the neonatal transition. Arch Dis Child Fetal Neonatal Ed 103:F539-546
Acknowledgements
We would like to thank all the study participants and their families who consented to join this study.
Author information
Authors and Affiliations
Contributions
Dr. Chaitra recruited patients, collected and analyzed the data, and drafted the initial manuscript; Drs. Singh and Basu supervised data collection and analysis of the data and did critical revision and finalization of the manuscript; Dr. Shrivastava contributed to the study design, echocardiography, data analysis, and interpretation; Drs. Priyadarshi, Chaurasia, and Chaturvedi contributed to the study design, data analysis, and interpretation; and all authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. The study protocol was approved by the Institute’s Ethics Committee of AIIMS Rishikesh, Uttarakhand, India (Ref No. AIIMS/IEC/21/103/dated 12/02/2021).
Consent to participate
Written informed consent was obtained from the parent of each subject before enrolment.
Consent for publication
Written informed consent was obtained from all the parents of the study participants for the publication of their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Angadi, C., Singh, P., Shrivastava, Y. et al. Effects of umbilical cord milking versus delayed cord clamping on systemic blood flow in intrauterine growth-restricted neonates: A randomized controlled trial. Eur J Pediatr 182, 4185–4194 (2023). https://doi.org/10.1007/s00431-023-05105-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05105-x