Abstract
New technologies enable the creation of digital twin systems (DTS) combining continuous data collection from children’s home and artificial intelligence (AI)-based recommendations to adapt their care in real time. The objective was to assess whether children and adolescents with asthma would be ready to use such DTS. A mixed-method study was conducted with 104 asthma patients aged 8 to 17 years. The potential advantages and disadvantages associated with AI and the use of DTS were collected in semi-structured interviews. Children were then asked whether they would agree to use a DTS for the daily management of their asthma. The strength of their decision was assessed as well as the factors determining their choice. The main advantages of DTS identified by children were the possibility to be (i) supported in managing their asthma (ii) from home and (iii) in real time. Technical issues and the risk of loss of humanity were the main drawbacks reported. Half of the children (56%) were willing to use a DTS for the daily management of their asthma if it was as effective as current care, and up to 93% if it was more effective. Those with the best computer skills were more likely to choose the DTS, while those who placed a high value on the physician–patient relationship were less likely to do so.
Conclusions: The majority of children were ready to use a DTS for the management of their asthma, particularly if it was more effective than current care. The results of this study support the development of DTS for childhood asthma and the evaluation of their effectiveness in clinical trials.
What is Known: • New technologies enable the creation of digital twin systems (DTS) for children with asthma. • Acceptance of these DTSs by children with asthma is unknown. | |
What is New: • Half of the children (56%) were willing to use a DTS for the daily management of their asthma if it was as effective as current care, and up to 93% if it was more effective. •Children identified the ability to be supported from home and in real time as the main benefits of DTS. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
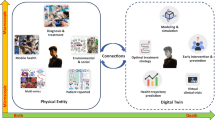
During the twentieth century, the practice of medicine was transformed by the multiplication of data sources allowing physicians to refine their diagnosis and optimise the management of their patients’ disease [1]. The growing amount of data has two consequences in the first half of the twenty-first century: (i) the multiplication of computational models processing patients’ health data to propose a diagnosis, make a prognosis, and/or recommend a treatment rather than another, grouped under the term “artificial intelligence” (AI) [1, 2]; (ii) the possibility of obtaining, using the internet of things (IoT), a comprehensive representation of the patient’s health status in real time, i.e. a live digital replica of the patient, more commonly known as a “digital twin” (DT) [3, 4]. The combination of AI in DTs could lead to digital twin systems (DTS): DTS comprise a physical element—the patient, a digital element—the patient’s DT, and 2-way interactions between the physical and digital elements: sensors transform the patient’s signal into the patient’s DT, and software processes them to act on the patient’s management through recommendations to the physician or automated adaptations [5]. Compared to existing mobile applications, DTS integrate multiple data sources to provide as complete an assessment of the patient as possible, collect most of the data in real time, and automatically adjust management when possible and alert medical teams when not.
Such DTS are particularly interesting in childhood asthma [6]. Despite effective treatments, clear guidelines, and the efforts from physicians, children, and their families, two-thirds of children with asthma continue to experience frequent asthma attacks resulting in decreased quality of life [7]. A personalised, real-time management of childhood asthma could help prevent asthma attacks in children and obtain better asthma control [8]. New connected objects (connected inhalers, connected smartwatches, etc.) and environmental databases (pollutants, pollens, weather conditions) now make it possible to passively and continuously collect objective and quantitative data on essential determinants of asthma control (adherence to controller treatment, environment, etc.). In the near future, this data can be processed by AI techniques to provide real-time recommendations to children, their families, and healthcare professionals.
While these DTS look attractive from a medical point of view, it is essential to collect the point of view of children and their families before developing such systems. In a survey conducted in France in 2020 before the COVID-19 pandemic, 54% of the 295 parents interviewed were ready to use such systems for the management of their child’s asthma, with socially advantaged parents being more willing to use them [9]. However, we are not aware of similar studies in children with asthma, who will be the first to be affected by this new type of management.
The primary objective of this study was to describe the children’s perception of AI and to assess whether they would accept/prefer a DTS for the management of their asthma compared to their current management by a physician only. Secondary objectives were to identify factors associated with a preference for the use of a DTS among the children interviewed, to collect their opinions on the potential advantages and disadvantages of DTS for the management of their asthma, and to investigate the correlation between the children’s and their parents’ responses.
Methods
Study design and population
A mixed-method study was conducted from June 2021 to May 2022 in three departments of paediatric pulmonology in two hospitals in Paris, France. Children and adolescents aged between 8 and 17 years with a physician-diagnosis of asthma were proposed to participate in a semi-structured interview, and their accompanying parents were invited to complete a survey. All participants provided informed consent. The study was approved by the ethics committee CERAPHP.CENTRE (Comité d'éthique de la recherche APHP Centre-2021-03-04).
The study was conducted in two stages. First, children were asked about their perception of AI in the management of their asthma and then about their perception of DTS in the management of their asthma. In both cases, we used a mixed method with a sequential design: qualitative and then quantitative.
Conduct of the semi-structured interviews
Development of the semi-structured interview guide followed the 5-step process presented in the systematic methodologic review by Kallio et al. [10]. Two of the authors (DD and AG) wrote the first version of the topic guide, which was then tested in three ways: internally (between the authors), with experts in the field (a psychologist and a data scientist from the ethics committee), and after reformulation following comments from these experts, with two children (8 and 11 years old) and a teenager (13 years old) with asthma (field testing). The final guide is presented in the supplemental material (Table S1).
All interviews were conducted face-to-face by the same investigator (AG), who had no prior relation with the children included. After introducing herself and obtaining the consent of the child and his/her parents, the investigator started by asking general questions to the child (age, school level, etc.). Then, the first open questions focused on AI: children were asked about their knowledge of AI and their views on how AI could help in the management of asthma in general. A closed question related to the place of AI in medical decisions regarding their health was associated (quantitative data).
At this stage of the interview, children were given an explanation about DTs integrating AI, using a demonstrator of a DTS interface modifying the asthma treatment of the child based on his/her responses to a short questionnaire equivalent to the Global Initiative for Asthma questionnaire (Fig. 1). Following these explanations, open questions were used to collect the children’s views on the potential advantages and disadvantages of using such a DTS for their daily asthma management. Then, the investigator collected quantitative data using closed questions related to their agreement (or not) to use a DTS for the daily management of their asthma. For this question, children were first asked if they would agree to use a DTS (yes or no). Then, in order to estimate their degree of preference for asthma management by the DTS over their current management by the physician only, they were asked to choose between the two types of management in 5 situations: an imaginary scenario of asthma management by the physician limiting the use of emergency treatment to 10 times per year and an imaginary scenario of asthma management by the DTS limiting the use of emergency treatment to 7, 8, 9, 10, or 11 times per year for each situation, respectively. These situations correspond to differences in effectiveness of + 30%, + 20%, + 10%, 0%, and − 10% for DTS-based management compared to physician-based management. The situation in which participants chose DTS over physician management defined their “strength of preference for DTS”, from 0 (refusal of DTS in all cases) to 5 (choice of DTS even when its effectiveness is 10% lower than that of physician management).
Animation created for the study to show children what the interface of the digital twin system might look like (https://scratch.mit.edu/projects/721368471)
Additional questions were asked about potential explanatory variables of their degree of preference for the DTS. The choice of the variables was based on a review of the literature, and included children’s characteristics (age, gender, school level), asthma severity (assessed using the GINA medication step), perceived importance of the physician–patient relationship, perceived knowledge of AI, concerns about data collection and use, and declared computer skills using scoring systems developed in our previous study [9] and presented in the supplementary material (Table S1).
Finally, to ensure that children understood all the questions related to AI and DTS and provided meaningful answers, the last question of the interview asked children to explain the DTS integrating AI. A custom score ranging from 1 (no understanding) to 4 (ability to explain the DTS in details) was used.
Parental survey
In parallel to the interviews with children, accompanying parents were asked to complete a short survey on their characteristics and on their degree of preference for their child’s asthma to be managed by the DTS compared to their current management by the physician.
Statistical analysis
For the qualitative part, a grounded theory approach was used to develop the codebook. Interviews were transcribed verbatim. Two investigators (AG and DD) independently coded the first 12 interviews, and codes were refined until consensus was reached. The subsequent interviews were then coded using the codebook in blocks of 12, and codes were revised after each turn. Although no new code appeared after the 79th interview (thematic saturation achieved), the investigators coded the remaining interviews because 104 dyads needed to be included for the quantitative analysis. Following an inductive approach, the codes were grouped into categories that were themselves grouped into major themes by AG and DD. Themes were reviewed until no new themes could be identified, tested by looking for confirming and disconfirming cases, and finally sent to all the authors for validation. In terms of researcher characteristics and reflexivity, AG is a junior paediatric pulmonologist, and DD is a senior one, both following children with asthma. However, AG had no previous experience of AI and DTS applications in childhood asthma, whereas DD is developing several research projects linked with these topics and anticipated both the potential advantages and risks of DTS for children [5]. Thus, the analyses were conducted by two researchers with different backgrounds, reducing the risk of a biased analysis of the children’s responses. Inter-rater reliability (IRR) was calculated using Cohen’s κ coefficient.
For the quantitative part, categorical variables were reported as proportions and percentage, and continuous variables were summarised by means and standard deviations (SD). The correlation between the degree of acceptance of a DTS by children and their parents (from the same dyad) was assessed by the Spearman coefficient. To identify the potential causal determinants of agreement to use DTS among children and conduct the appropriate statistical analysis, we used a directed acyclic graph (DAG) [11]. DAGs are an increasingly popular approach for identifying confounding variables that require conditioning when estimating causal effects, decreasing the risk of bias due to over adjustment [12]. We designed the DAG using the freely available software DAGitty v3.0 (http://www.dagitty.net/dags.html) [13] and identified potential determinants of DTS acceptance and their links based on a review of the literature (Supplementary material). The resulting DAG is presented in Fig. 2.
From the DAG, the variables needed to estimate the total effect of each determinant were identified using d-separation rules automatically calculated by the DAGitty software. For each determinant, a specific ordinal logistic regression model was used with the corresponding set of adjustment variables.
Analyses were performed with R software (4.1.2), using the MASS package [14].
With 9 predefined potential explanatory variables, and a minimal number of 10 events per variable, 90 interviews needed to be completed to run the ordinal logistic regression model. We estimated that 15% of the parent’s surveys may be incomplete and aimed to include 104 parent–child dyads.
Results
Of the 107 parent–child dyads approached, 104 agreed to participate in the study. Five dyads whose child showed no understanding of the concept of DTS and AI at the end of the study despite the explanations given were excluded from the analysis. Finally, 99 children and their 95 parents (four siblings) were included in the analysis (flow chart in Figure S1). The characteristics of these children and their parents are presented in Tables 1 and S2, respectively. For the qualitative analysis, there were 506 text units coded with 43 different codes. The IRR between the two coders (AG and DD) was κ = 0.98. The mean number of different codes per interview was 5.1.
Children’ views on artificial intelligence for asthma
The level of understanding of artificial intelligence among participants at the beginning of the study was variable. Quotes from four patients reflect this heterogeneity: “I don’t know at all”; “It’s a robot that is intelligent”; “You have something on your phone, you give him a name, and you can ask it some question like -what is the weather- and it’s going to answer you”; “AI is a computer intelligence that can think by itself, it’s not programmed to tell you this and this, it can think by itself”. Older age was associated with higher knowledge of AI, while, surprisingly, higher parental education level was associated with lower knowledge of AI (Table S3).
When asked about their views on how AI could help manage asthma, 52% of children had no idea. For the remainder, the main themes were that AI could help with the daily management of asthma (by improving adherence, monitoring symptoms, adjusting treatments, providing advice, or predicting asthma attacks), with the development of new solutions for asthma management (new devices/treatments), decrease waiting times for appointments and automate the order of asthma treatments (Table 2).
Children's views on the place of artificial intelligence in medical decisions affecting them
When asked to determine the respective positions of their doctor (human intelligence) and an AI for medical decisions concerning them, 61 children (62%) responded that these decisions should rely only on their physician or essentially on their physician assisted sometimes/often by an AI (Fig. 3). Only 3 (3%) supported the idea of medical decisions based on fully autonomous AI.
Children’s views on digital twin systems for the daily management of their asthma
The potential advantages and disadvantages of DTS identified by the children are presented in Table 3 and summarised below. As the number of respondents was 99, only the percentages are reported, as the number of children is almost identical. Older children (13–17 years old) identified more advantages and disadvantages of using a DTS than younger children (8–12 years old, Table S4).
The majority of children (87%) reported the advantages of using a DTS. The possibility of remote management of their asthma was the dominant theme (47%). It included the advantages of fewer travels, fewer medical visits, and fewer missed school days. The second main theme was the assistance provided by the DTS in the daily management of asthma (27%), including automated medication adjustment, support to improve adherence and manage asthma attacks, personalised management based on the child’s actions, and the integration of environmental factors into asthma management. The continuous health monitoring offered by the DTS allowing real-time management with immediate alerts from the physician in case of deterioration was the third theme (26%). In summary, the main benefits of the DTS identified by the children were that they could be supported in the daily management of their asthma (i) from home and (ii) in real time.
Children had more difficulty identifying the disadvantages of using a DTS with only 57% providing an example. The main disadvantage identified was the risk of bugs (53%), whether caused by a programming error (38%) or an external cause (virus, hacking) (17%). Then, the loss of humanity was the second main theme (24%): children shared their difficulties in trusting the embedded AI (15%), some asked for human supervision of all decisions (7%), and others regretted the loss of human contact (6%). Several respondents thought that the DTS would perform worse than their physician (18%), with their physician being better able to deal with symptoms and unexpected events than the embedded AI (15%).
Children’s acceptance of a digital twin system for their daily asthma management
Eighty-five percent of children agreed to use a system equivalent to the DTS presented during the interview. To assess their strength of preference for a DTS over their current physician-based management, we asked them to choose between the usual follow-up by their physician and the follow-up by the DTS (Fig. 4). Seven percent never chose the DTS, even when its hypothetical ability to control asthma was 30% better than that of the physician alone. If the DTS was said to be equally effective as the physician, 56% of participants were willing to use it, and this rate increased to 93% if the DTS was said to be 30% more effective than the physician. Even when the DTS was considered 10% less effective than the physician, 23% of children preferred this new type of care. These results were not different between children (8–12 years old) and adolescents (13–17 years old) (p = 0.6).
Parent’s acceptance of a digital twin system for the daily management of their children's asthma
Parents were more reluctant than their children to use a DTS, with 31% saying they would never choose the DTS. However, 43% were willing to use the DTS if it was as effective as the physician, and up to 69% if the DTS was said to be 30% better than the physician’s usual management (Fig. 4). There was no significant correlation between the children’s and their parents’ responses to this question (Spearman’s rho coefficient = 0.17; p = 0.10).
Analysis of factors associated with children’s acceptance of a digital twin system
In the multivariate analysis, children were more prone to choose the DTS-based management if they had high computer skills and less prone to choose the DTS-based management if they valued the physician–patient relationship (Table 4).
Discussion
The main finding of this study was that half of the children were willing to use a DTS for the daily management of their asthma if it was as effective as current care, and up to 93% if it was more effective. Children reported that the ability to be supported in managing their asthma from home and in real time was the main benefit of the DTS. They also identified risks related to technical problems that might occur, as well as the risk of loss of humanity.
This study supports the idea that children’s views should be taken into account when considering changes in their care at the societal level: discussions were rich, and the advantages and disadvantages of the potential use of DTSs identified by children were similar to those reported by adults regarding the use of AI in medical settings [15]. The understanding of the topic discussed was also good, with only five children unable to simply re-explain the concept of AI and DTS at the end of the interview.
One of the original features of our study is that we compared children’s attitudes towards DTS with those of their parents. We found that parents were less prone to use DTSs than children. However, within the same family, we did not find a correlation between the child’s response and the parents’ response when asked to choose between a DTS and a physician-based management.
There are several hypotheses to explain why children are more prone to use DTS than their parents. A first hypothesis is that children are less aware of the risks associated with the use of a DTS than their parents. A study conducted by UNICEF on the perception of AI by adolescents aged 14–16 [16] showed that the majority of them had little or no understanding of the risks of AI. In our study, when children expressed concerns about DTS, they were similar to those reported by adults [15], but raised less frequently. Acceptance of DTS may be higher among children because they do not perceive their risks as much as adults.
A second hypothesis is that younger people are more used to new technologies and more comfortable with their use, which would explain why they are also more prone to use a DTS. This hypothesis is supported by the results of our study, which identified that a higher level of computer skills predicted a higher strength of preference for the DTS. Being comfortable with the technology might make it easier to see how a DTS like the one presented would work and to not remain in fear of the unknown.
The third hypothesis is that of a profound digital transformation of society. Whereas the previous generation was used to face-to-face consultations, the “digital-native” generation has been raised in an environment of screens, rapid home deliveries, and instant answers from search engines and now virtual assistants. In our study, the main advantages of the DTS identified were that their asthma could be managed (i) from home and (ii) in real time. It is possible that this new generation is ready for a complete paradigm shift in the management of chronic diseases, which would be managed remotely and in real time by connected physicians closer to health engineers than to the image of the family physician.
This change in mentality seems to have been largely reinforced by the COVID-19 pandemic: our team had conducted a similar study [9] among 300 parents of asthmatic children in France between September 2019 and February 2020, during which 45% of them had declared that they would never agree to use a DTS. In our study, only 31% of parents said they would never use a DTS. Between the two studies, there was the COVID-19 pandemic, which forced patients to become familiar with the use of telemonitoring and telecare and spread and established its use among all generations [17, 18].
Nevertheless, the physician–patient relationship remains important for the children and adolescents interviewed. Those who were most attached to this relationship were less likely to choose DTS management. For the majority of respondents, as for the majority of adults [9, 15], AI and DTS remain an additional tool that shall remain under the supervision of their physician.
This study has several limitations. Patients were recruited from two Parisian university hospitals, and the extrinsic validity of our results to the general population of children with asthma remains unknown. In addition, participants were asked about hypothetical scenarios, and it is difficult to say whether their answers would be transposable if they were offered to use a real DTS. Finally, we only proposed a model of DTS that supports remote self-management and did not address the case of DTs with other applications such as personalising patient education.
In conclusion, half of the participating children were ready to use a DTS if it was as effective as usual management by the physician, and this proportion increased to 9 out of 10 children when the DTS was associated with at least 20% better asthma control compared to usual management by the physician. The results of this study support the development of DTS for childhood asthma and open up a new field of research. Future studies will need to determine how best to involve children in the design of DTS, and how to evaluate such systems taking into account both the medical and economic dimensions, as well as the societal and environmental consequences of their implementation.
Availability of data and material
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code availability
Not applicable.
Abbreviations
- AI:
-
Artificial intelligence
- DAG:
-
Directed acyclic graph
- DTS:
-
Digital twin system
- IOT:
-
Internet of things
- IRR:
-
Inter-rater reliability
References
Drummond D (2021) Between competence and warmth: the remaining place of the physician in the era of artificial intelligence. NPJ Digit Med 4:85
Exarchos KP, Beltsiou M, Votti CA, Kostikas K (2020) Artificial intelligence techniques in asthma: a systematic review and critical appraisal of the existing literature. Eur Respir J 56
Popa EO, van Hilten M, Oosterkamp E, Bogaardt M-J (2021) The use of digital twins in healthcare: socio-ethical benefits and socio-ethical risks. Life Sci Soc Policy 17:6
Laubenbacher R, Sluka JP, Glazier JA (2021) Using digital twins in viral infection. Science 371:1105–1106
Drummond D, Coulet A (2022) Technical, Ethical, legal, and societal challenges with digital twin systems for the management of chronic diseases in children and young people. J Med Internet Res 24:e39698
Drummond D (2022) Digital tools for remote monitoring of asthma patients: gadgets or revolution? Rev Mal Respir 39:241–257
Hammer SC et al (2008) Actual asthma control in a paediatric outpatient clinic population: do patients perceive their actual level of control? Pediatr Allergy Immunol 19:626–633
Guilleminault L et al (2017) Personalised medicine in asthma: from curative to preventive medicine. Eur Respir J 26
Abdoul C et al (2021) Parents’ views on artificial intelligence for the daily management of childhood asthma: a survey. J Allergy Clin Immunol Pract 9:1728-1730.e3
Kallio H, Pietilä A-M, Johnson M, Kangasniemi M (2016) Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J Adv Nurs 72:2954–2965
Lederer DJ et al (2019) Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals. Ann Am Thorac Soc 16:22–28
Diemer EW, Hudson JI, Javaras KN (2021) More (adjustment) is not always better: how directed acyclic graphs can help researchers decide which covariates to include in models for the causal relationship between an exposure and an outcome in observational research. Psychother Psychosom 90:289–298
Textor J, van der Zander B, Gilthorpe MS, Liśkiewicz M, Ellison GT (2016) Robust causal inference using directed acyclic graphs: the R package ‘dagitty.’ Int J Epidemiol 45:1887–1894
Ripley B et al (2013) Package ‘mass.’ Cran r 538:113–120
Young AT, Amara D, Bhattacharya A, Wei ML (2021) Patient and general public attitudes towards clinical artificial intelligence: a mixed methods systematic review. The Lancet Digital Health 3:e599–e611
United Nations Children’s Fund (UNICEF) (2021) Adolescent perspectives on artificial intelligence. https://www.unicef.org/globalinsight/sites/unicef.org.globalinsight/files/2021-02/UNICEF_AI_AdolescentPerspectives_20210222.pdf
Karimi M et al (2022) National survey trends in telehealth use in 2021: disparities in utilization and audio vs. video services. 15
Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L (2021) Assessment of patient preferences for telehealth in post–COVID-19 pandemic health care. JAMA Netw Open 4:e2136405
Author information
Authors and Affiliations
Contributions
Apolline Gonsard and David Drummond contributed to the study conception and design. All authors participated in data collection. Apolline Gonsard and David Drummond analysed the results and wrote the first draft of the manuscript. All authors commented on previous versions of the manuscript, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the ethics committee CERAPHP.CENTRE (Comité d'éthique de la recherche APHP Centre—2021–03-04).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gonsard, A., AbouTaam, R., Prévost, B. et al. Children’s views on artificial intelligence and digital twins for the daily management of their asthma: a mixed-method study. Eur J Pediatr 182, 877–888 (2023). https://doi.org/10.1007/s00431-022-04754-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04754-8